8 Phenol Peeling
Introduction
The distribution of peel patients used for this chapter are seen in Table 8.1. Factors affecting phenol peel depth are shown in Box 8.1. One hundred and fifty-nine full face phenol peels and nine human biopsy studies were used in this study. Results of these efforts were published in Clinics in Plastic Surgery.
| Formula | Number of patients | Age range |
|---|---|---|
| Venner-Kellson | 18 | 29–60 |
| Maschek-Truppman | 7 | 46–63 |
| Finsti | 3 | 55–65 |
| Baker-Gordon w/o croton oil | 1 | 60 |
| Gradé I | 3 | 46–49 |
| Gradé II | 4 | 40–48 |
| Gradé III | 2 | 41–64 |
| Stone II | 24 | 32–72 |
| Combined Gradé II, III | 2 | 47–49 |
| Combined Gradé I, III | 3 | 38–64 |
| Combined Gradé III, Baker-Gordon | 1 | 57 |
| Combined I, II, Baker-Gordon | 1 | 47 |
| Combined Gradé II, Stone II | 3 | 31–52 |
| Stone II-Venner-Kellson | 23 | 42–71 |
| Combined Stone II, Baker-Gordon | 2 | 38–49 |
| Combined Baker-Gordon, Venner-Kellson | 4 | 28–60 |
| Combined Baker-Gordon, Venner-Kellson, TCA | 1 | 71 |
| Combined Baker-Gordon, TCA | 2 | 56–60 |
| Combined Maschek-Truppman, Baker-Gordon | 1 | 58 |
| Combined Venner-Kellson, TCA | 6 | 28–69 |
| Baker-Gordon | 48 | 29–74 |
| Total | 159 |
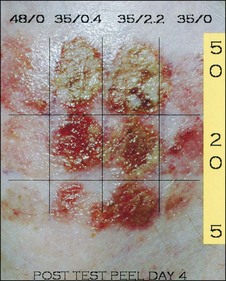
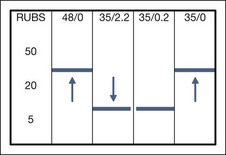
Based on these studies and two new experiments reported below, the author concluded that: (1) rubbing increased the depth of injury (agree with Hetter); (2) the thickness of papillary dermis injury, the degree of fibrosis, and the degree of inflammation were less with 5 rubs and more with 50 rubs (Fig. 8.1); (3) phenol is not all-or-none (agree with Hetter); (4) croton oil increased depth of injury (agree with Hetter); (5) there was little observable difference between 0.4% croton oil and 2.2% croton oil when application techniques were kept constant (disagree with Hetter), and (6) human experimental models have inherent variables.
Based on quantifiably reproducible experimental test peel patch studies on the right cheek and, later, left cheek test peel patches (reported below), using 48% phenol with 0.0% croton oil, 35% phenol with 0.4% croton oil, 35% phenol with 2.2% croton oil, and 35% phenol with 0.0% croton oil (see Fig. 8.1), a lowering of the threshold affect to create injury (Fig. 8.2) to between 5 and 20 rubs can be seen when croton oil is added. This is down from the 20 to 50 rubs required when croton oil is excluded. The early appearance of coagulation is not a true indicator of depth of peel, nor is the immediate density of frost as evidenced by the reported superficial results from 88% USP Phenol which can produce an immediate, dense, white frost. The length of time a given formula is applied, the concentration of phenol and croton oil, the volume of acid, the vigor and abrasiveness of the application and predegreasing procedure, and the occlusive technique all play a vital role in the final result.
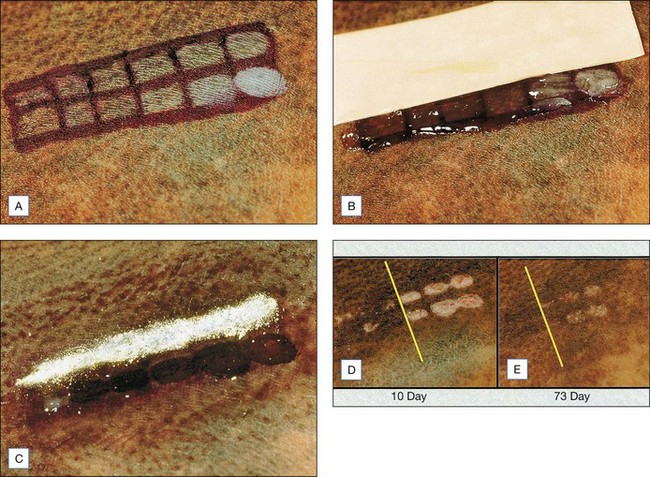
In order to further test the hypothesis that length of application or number of rubs plays a paramount role in peel result, an African-American male, age 37, with a truncal congenital nevus of Becker was tested with one formula: the Stone II (60% phenol, 0.2% croton oil) (Fig. 8.3A–E). Twelve test patches, six in each of two rows, were rubbed with 1, 5, 10, 20, 50, and 100 coats using twice-blotted, semi-dried Q-tips. The top row was covered with tape for 48 hours followed by thymol iodide powder (Delasco Laboratories, Council Bluffs, IA) for 7 days. The bottom row was covered with Aquaphor ointment until healed. A clear threshold between 10 and 20 rubs was seen by day 10 and persisted through to day 73, the last day of the study.
Based on this objective data, it is the author’s conclusion that both the Hetter and Stone techniques can produce excellent results with modified phenol. The student is left with a clear choice. Using the Hetter technique the student will employ several dilutions over multiple facial and neck zones with an ointment occlusion, or will choose one formula with a timed application and a waterproof tape/ powder occlusion. It is a bit like comparing proven facelift techniques. Not one method is good for all students or all patients. See Box 8.2 for key features.
Box 8.2
Key features
Treatment Approach
• Definition of zones
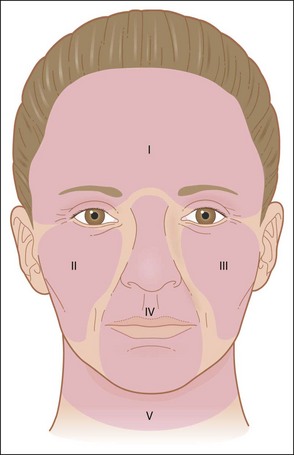
It is a well known fact that a thorough phenol peel should take a minimum of 1 hour to avoid too rapid absorption of phenol. Therefore, the face is divided into zones for the purpose of ensuring that the procedure takes a minimum of 90 minutes to complete (Fig. 8.4).
• Formulae
From 1975 to 1991 the author used Baker-Gordon phenol formula exclusively. From 1992 to the present, while searching for the ‘best formula’, experience was gained with the Venner-Kellson formula, the Maschek-Truppman formula, Gradé formulae I, II, III, the Finsti formula and the Hetter-Heresy formulae. This author soon realized the benefits of the Venner-Kellson formula without recognizing the actual percentage of croton oil until Hetter focused attention on its importance. When the croton oil percentages were calculated, it was clear that croton oil (0.16% in Venner-Kellson and 0.2% in Gradé II) were comparable to the very light Hetter-Heresy formula croton oil concentration (0.105%) and the Hetter-Heresy medium-light formula (0.35%). The major difference was in the phenol concentration of approximately 60% with Venner-Kellson and Gradé II compared with 33% phenol in the Hetter-Heresy medium-light formula. While Hetter was pursuing the optimum peel by reducing croton oil and phenol percentages, the author was modifying application technique and quantifying the number of rubs over time and, finally, time of application as the best way to standardize and teach the procedure. The author became convinced of the importance of application technique when Hetter presented a patient who underwent a coronal forehead lift and simultaneous 35% phenol with 0.0% croton oil peel to the forehead and 35% phenol with 0.4% croton oil peel to the nose, lips, chin and cheeks. Clearly the patient had a lighter peel to the forehead (not ‘no peel’), as stated by Hetter, and deeper peel to the nose and cheeks. One cannot conclude that this deeper peel is due solely to the croton oil as Hetter would have us believe, unless the applications were identical. We simply do not know for how long the Hetter formulae were applied. It is unlikely that forehead skin undermined during a forehead lift would be peeled with the same vigor as unlifted wrinkled cheek skin. The same principal holds when combining facelift with immediate laser resurfacing, or immediate TCA applications. Objective data seen in Figures 8.2 and 8.3 support the hypothesis that depth of peel is modified by application technique. There is little difference between 0.4% and 2.2% croton oil when combined with 35% phenol and used in a controlled fashion with 5, 20 or 50 rubs on human cheek skin. With both formulae, 5 rubs produces least injury and 50 rubs produces most. More work is necessary to relate application times with corresponding injury levels in various skin types.
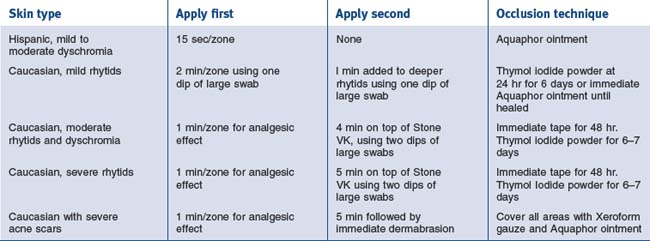
Shown in Boxes 8.3 and 8.4 are the two formulae currently used by the author and, in Table 8.2, the use of Stone VK and Stone II formulae.
The Stone VK formula and the Stone II formula were standardized by Delasco Laboratories and made available to the medical profession. Both formulae were modified from the original Venner-Kellson and Gradé II formulae (Boxes 8.5 and 8.6).
• Set up and procedure
(Table 8.3 shows medication used before, during, and after the peel.)
| Medications | Dosage |
|---|---|
| Preoperative medications | |
| Meperidine HCl/Pethidine (Demerol) 50 mg | 1 tab PO 1 hr prepeel |
| Diazepam (Valium) 10 mg | 1 tab PO 1 hr prepeel |
| Valacyclovir (Valtrex) 500 mg | 1 tab PO bid for 10 days starting 2 days before peel |
| Methylprednisolone (Medrol) dose pack | Take as directed starting day of peel |
| Dicloxacillin 500 mg | Take 1 tab PO bid for 5 days |
| Intraoperative medications | |
| Morphine sulfate 2 mg | IV at start of peel, repeat ×1 prn |
| Postoperative medications | |
| Meperidine HCl/Demerol 50 mg | PO on arrival home and at bed around 6 p.m. |
| Diazepam 10 mg | PO on arrival home and at bed around 6 p.m. |
| Meperidine HCl/Demerol 50 mg | PO 9 p.m. night of peel |
| Flurazepam (Dalmane) 30 mg | PO 9 p.m. night of peel |
| Meperidine HCl/Demerol 50 mg | PO midnight night of peel |
| Flurazepam 30 mg | PO midnight night of peel |
| Valacyclovir 500 mg | PO bid for 10 days starting 2 days prepeel |
| Dicloxacillin 500 mg | PO bid for 5 days |
| Methylprednisolone dose pack | Take as directed, starting night of peel |
| Hydroxyzine (Atarax) 25 mg | PO bid for itching prn |
| Meperidine HCl/Demerol 50 mg | PO prn pain (usually not necessary) |
| Betamethasone diproprionate (Diprolene cream) 0.05% Resume hydroquinone 4% retin-A 0.1% at 3–4 weeks PRN hyperpigmentation | tid for 1 wk starting at day 10 (to reduce redness) |
Alcohol ×3 – with 4″ × 4″ gauze pad rubbed with moderate vigor
Acetone ×3 – with 4″ × 4″ gauze pad rubbed with moderate vigor.
Stone VK Peel Technique
• Stone II peel technique
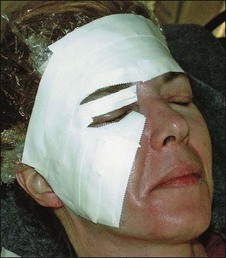
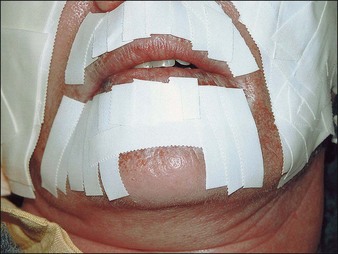
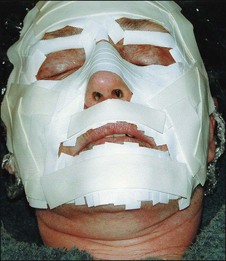
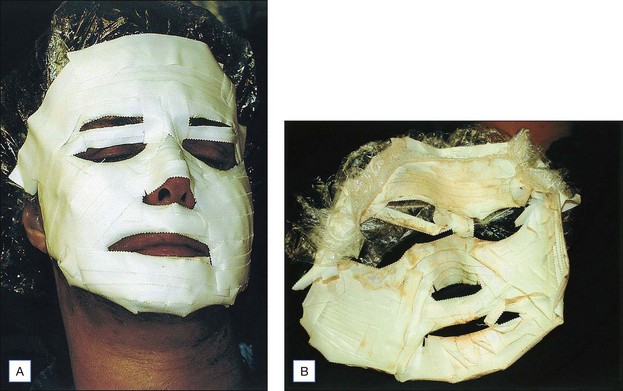
Keep painting over entire area during allotted time (4 minutes for moderate lines, up to 5 minutes for severe lines; use no more than two dips into emulsion, one fresh swab per dipping. Gently sponge away the oily surface with 4″ × 4″ gauze. Apply tape using many overlapping pieces of  and 1″ waterproof tape. Leave brows untapped, and go over pretarsal skin leaving 1–2 cm of untapped skin adjacent to lashes (Fig. 8.6).
and 1″ waterproof tape. Leave brows untapped, and go over pretarsal skin leaving 1–2 cm of untapped skin adjacent to lashes (Fig. 8.6).
Box 8.7
Pearls
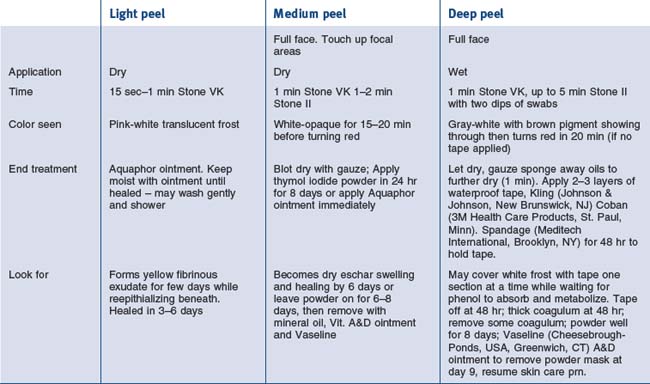
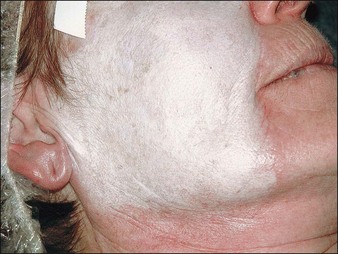
By using this timed approach, what to look for with the frost as it changes appearance will be seen in Table 8.4. You will see pink translucent frost at around 15 seconds (Fig. 8.10) and opaque white (Fig. 8.11) at 4 minutes. After 5 minutes the gray tone will slowly seep through and flecks of brown pigment will begin to show (Fig. 8.12). This is a good end point for a deep peel (a must around the lips and chin with deep rhytids).
• Tape mask for 48 hours
At the completion of the procedure, when the patient meets discharge criteria, they are sent home with the medicine schedule listed in Table 8.3. Based on the fact that the peel process produces pain for 6 hours, the phenol peels are performed at 4 p.m. The patient is usually in their own bed by between 6 p.m. and 7 p.m., which means they have to be made comfortable until about midnight, at which time they take the next set of medications and usually fall asleep for the remainder of the night. They wake up swollen, but pain free. Patients and family are tutored on what to expect by seeing photos and videos of the procedure.
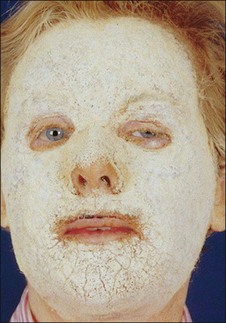
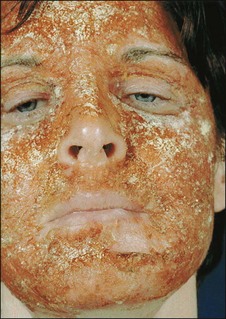
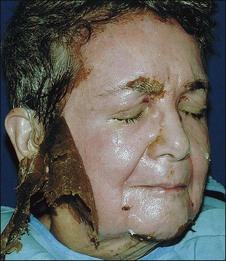
Figure 8.13 shows a typical mask at 48 hours, just prior to removal, and the mask after removal. At this point, there should be abundant wet, yellow exudate (Fig. 8.14). The more the better! Exposed lids, nose and any area where the tape has loosened will show darker, dry eschar (Fig. 8.15). These areas actually will be less deep, heal faster and probably not be a problem in the patient with mild to moderate rhytids. In the patient with severe rhytids, effort is made to keep the tape more adherent with Kling and Spandage, especially around the lips. It is difficult to keep tape adherent in these areas and in the author’s opinion this explains the sometimes less than dramatic results around the lips. But here again, we are not trying to equal the Baker-Gordon result; rather, we welcome a kinder, gentler peel with less hypopigmentation. Better to be underdone than over.
• After tape mask removal
The exudate excess is gently removed with swabs and gauze but no attempt is made to remove all. Thymol iodide powder is applied with large rectal swabs in a rolling fashion. The patient is supplied with powder and swabs to use at home with four to five reapplications recommended daily. The compulsive patient will look like Figure 8.16 with a good opaque yellow mask at day 6. The less compulsive will look like Figure 8.17 with a brown dry eschar beginning to crack, revealing pink underlying new epithelium.
After 7 days of powder – nine days after the peel itself – all areas should be epithelialized. That night the patient starts compresses of warm face towel (wrung out wet, warm towel), moistened liberally with mineral oil, 20 minutes on, 20 minutes off. In the interim, Vaseline and/or vitamin A&D ointment is frosted over the entire mask, using tongue blades supplied to the patient. This is done during the 20 minutes that the skin is not being treated with a compress. This process is done for approximately 3 hours prior to going to sleep with the last layer of ointment. Some patients are good at this and come to the office the next morning all ‘peeled’ and pink. Others are more squeamish and wish to have the mask peeled off by the doctor (Fig. 8.18). This is fun for the doctor and painless for the patient since all is epithelialized.
At this point, patients may shower and shampoo freely and wash the face with gentle products. The author’s favorites are LaRoche-Posay Gentle Dermo Cleanser and Biomedic Gentle Healing Ointment (LaRoche-Posay, France) as moisturizer of choice. Other gentle cleansers and moisturizers may be substituted. Some patients will be more inflamed or red and will be given a course of betamethasone diproprionate (Diprolene Cream 0.05%, Schering Corp., NJ) three times a day for up to 1 week. This is applied before the moisturizer because sometimes it burns a little. By 2 weeks post peel SkinTech SPF 30 (www.skintech.com.au) with titanium dioxide can be used to mask the red. Other products with same function are permissible. Make-up can go over the SPF. By 14 to 21 days the patient is fully epithelialized, comfortable with camouflage make-up, and can return to relatively normal activity. Patients having light peels will reach this stage at between 7 and 12 days.
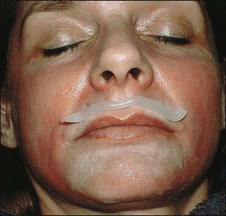
• Touch up
For those patients at three months or later who have persistent perioral or periorbital lines, a repeat peel is done using the same approach. No tape or powder are used during the touch ups. Aquaphor ointment (Fig. 8.19) or vitamin A&D ointment is frosted on the peeled surface immediately. This procedure takes about 10 minutes on the presedated patient. No IVs, EKG (ECG), or other monitors are used because of the small areas involved. There is very little pain with this second Stone VK touch up peel. Rarely, the Stone II is used for touch ups. The patient is obviously not charged for this procedure.
Results, Comments, and Philosophy
This chapter was designed to be a primer for modified phenol face peeling. The formulae and methods were standardized to meet this author’s clinical needs. The method works. Once the basics are in place, you can modify the method to suit your needs. Controlling the peel process to achieve the desired end result is key. This author found that the original Venner-Kellson formula, modified and made available by Delasco, meets all of the requirements for a safe, effective, reproducible peel, and useful for a variety of skin conditions by changing the length of time of application. Changing the method of occlusion is done mainly for expediency since it does not affect the depth of peel as much as the uniformity or evenness of result. The Hispanic patient shown in Figure 8.20 demonstrated a uniform improvement using a 15-second application of the Stone VK. She was treated with Aquaphor ointment through the healing process. One year prior to the Stone VK she had a resorcinol peel (also available from Delasco as the Stone Resorcinol peel formula). This is a topic for another discussion but suffice it to say that resorcinol is the preferred blending peel for neck, chest, arms, and hands.
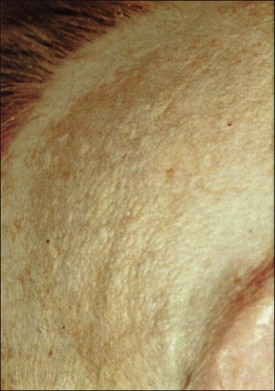
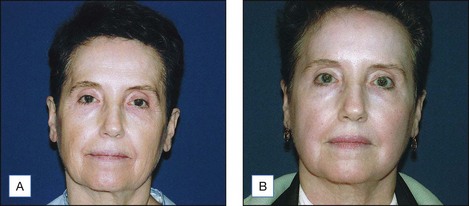
The patient shown in Figure 8.21 is a Caucasian with Fitzpatrick II skin type who was treated with a 5-minute Stone II peel followed by thymol iodide powder at 24 hours until healed at 1 week (see Fig. 8.21D). This was before it was realized that the Stone VK was definitely less painful to apply than the Stone II. The same result could have been expected with a 5-minute Stone VK.
The patient shown in Figure 8.22, a Caucasian with Fitzpatrick skin type III, was treated with a 1-minute Stone II peel followed by waterproof tape occlusion for 48 hours and 3-day blending resorcinol peel to neck. (The face was treated with Aquaphor ointment after tape removal, as was the neck after the 3rd day of five coats of resorcinol – one every 5 minutes for five coats on three consecutive days.) The resorcinol is put on like glycolic acid, one even coat every 5 minutes for five coats and repeated 3 days in a row. On the 3rd day after the five coats of resorcinol have dried, either thymol iodide powder is applied to form a crust or Aquaphor ointment is applied throughout healing. Either occlusion method works well.
Figure 8.23 shows a Caucasian, 60-year-old female of Fitzpatrick II skin type and with moderate rhytids who was treated with a 5-minute Stone VK peel followed by a 2-minute Stone II, with tape and powder occlusion. Her neck was not treated with resorcinol but easily could have been. She was seen at 12 months post peel (see Figure 8.23B).
The patient shown in Figure 8.24, a fifty-five-year-old Caucasian with red hair, Fitzpatrick I skin type, and looking older than her stated age, responded well to a 13-minute Stone VK peel and a 1-minute Stone II peel followed by tape and powder. Note that after 6 months she still had a ruddy complexion and some persistent perioral lines (Fig. 8.24B). Her neck was not treated (now she would have a 3-day resorcinol peel). The patient has not been seen in follow up beyond 6 months but it is assumed she would be lighter.
The patient shown in Figure 8.25A and B, a 65-year-old Caucasian has a Fitzpatrick II skin type showing moderate to severe rhytids and actinic keratosis and was treated with a 2-minute Stone VK peel and 4-minute Stone II peel, followed by tape and powder. Her forehead after a 1-minute Stone VK peel is seen in Figure 8.25C. Her forehead after a 4-minute Stone II peel on top of a 2-minute Stone VK peel shows how the peel is carried well into hairline, brows, and upper lids as part of a zone I peel (Fig. 8.25D). Also note the shower cap before it is taped in place. Figure 8.25E and F shows frontal and lateral views at 3 months. Note her neck was not peeled. At 3 months there is no hypopigmentation but at 2 years post peel (Fig. 8.25G) she is more hypopigmented. She also let her hair dye grow out, actually making her appear older. She needed a perioral touch up, seen after a 2-minute Stone VK peel at 3 days in Figure 8.25H. Note the vitamin A&D ointment occlusion technique, feathering at edges with new epithelium, and thicker adherent coagulum over heavier rhytids. She is seen at 9-days showing increased redness from herpes simplex super infection in Figure 8.25I (when the patient discovered she was using Flagyl given by her pharmacist rather than Famvir), and at 5 weeks in Figure 8.25J with resultant prolonged but temporary redness. (The actual real-time touch up peel can be seen on the DVD). This patient would benefit from a resorcinol neck peel, facelift, make-up and hair styling.
Figure 8.26 show a sixty-five year old Caucasian Fitzpatrick II skin type. Her forehead is white, on account of being hidden by her hair for a long period, while the lower face shows freckles and moderate to severe rhytids, hyperpigmentation, and sagging. She was treated with one minute Stone VK peel and five minute Stone II peel followed by tape and powder. She is seen in the second photograph 2 years and 9 months after the chemical peel and 2 years 6 months after blepharoplasty and facelift, wearing only eyelid make-up and lipstick. Note her original pallor has been restored, not a waxy porcelain mask of hypopigmentation. This patient also participated in the right and left cheek test peel patch studies which left no tell tale signs. This is the expected result from peel followed by facial surgery.
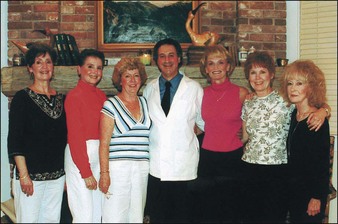
Figures 8.27 and 8.28 show groups of happy patients in various stages of their peels. They became supportive of one another, and patient advocates for my practice. Figure 8.28 shows what the modified phenol face peel can do for your patients: expect a group of very satisfied people who will be proud to share their experiences with other new patients.
Baker TJ. Chemical face peeling and rhytidectomy: a continued approach for facial rejuvenation. Plastic Reconstructive Surgery. 1962;29:199.
Hetter G. An examination of the phenol-croton oil peel: Part 1. Dissecting the formula. Plastic Reconstructive Surgery. 2000;105:227-239.
Hetter G. An examination of the phenol-croton oil peel: Part II. The lay peelers and their croton oil formulas. Plastic Reconstructive Surgery. 2000;105:240-248.
Hetter G. An examination of the phenol-croton oil peel: Part III. The plastic surgeon’s role. Plastic Reconstructive Surgery. 2000;105:752-763.
Hetter G. An examination of the phenol-croton oil peel: Part IV. Face peel results with different concentrations of phenol and croton oil. Plastic Reconstructive Surgery. 2000;105:1061-1083.
MacKee GM, Karp FL. Treatment of post acne scars with phenol. British Journal of Dermatology. 1952;64:456.
Marmelzat WL. Bits of history, bits of mystery: a historical view of chemical rejuvenation of the face. In: Kotler R, editor. Chemical rejuvenation of the face. St Louis: Mosby Yearbook, 1992.
Stone P. The use of modified phenol for chemical face peeling. Clinics in Plastic Surgery. 1998;25(1):21-44.
Stone P, Lefer L. Modified phenol chemical face peels: recognizing the role of application technique. Clinics in Plastic Surgery. 2001;28(1):13-36.
Truppman ES, Ellenby JD. Major electrocardiographic changes during chemical face peeling. Plastic Reconstructive Surgery. 1979;63:44.