190 Pharmacoeconomics
Pharmacoeconomics is a branch of health economics that analyzes the economic impact and cost-effectiveness of pharmaceuticals.1 This definition has been broadened to include not only the economic costs but also the quality-of-life or humanistic consequences of drug therapy. Evaluation of therapeutic protocols and guidelines also is included in pharmacoeconomic studies.2 It has been suggested that health economics can help answer two fundamental questions: (1) Is a given therapy (or program) worth using when compared with alternatives? (2) Should a portion of available healthcare resources be allocated to a given therapy or program?3
Since the term was first used in 1986, pharmacoeconomics has evolved in complexity and applicability.2 Although still not required by the U.S. Food and Drug Administration (FDA), clinicians, administrators, and healthcare systems are mandating that economic information be added to the clinical effectiveness information for new therapies before a drug is added to a formulary. The Academy of Managed Care Pharmacy (AMCP) published the Format for Formulary Submissions, Version 3.0 as a template pharmaceutical manufacturers can use when submitting drugs for health system review.4 The goal of these guidelines is to ensure that all new products bring added clinical as well as economic value to the insured population. As such, pharmacoeconomic data can lead to more informed decisions being made about selecting a particular drug for a patient or healthcare system. A recent survey of 540 pharmacy directors revealed that 37% had their staffing budgets reduced in the past 6 months5; 56% had to reduce their drug expenditures by 2% to 5%, and 25% reported reductions of 6% to 10%. This can translate into several million dollars cut from drug budgets. Hospital administrators are increasingly focusing on pharmacy costs. Whereas CEOs of hospitals did not rank drug expenditures in their top 20 concerns for 1996, the repeat survey in 2000 yielded drug expenditures as the seventh most important concern.6 In fact, drug and technology costs were second only to decreased reimbursement, whereas drugs offered the single greatest opportunity for cost savings.
 Economics of Health Care in the Intensive Care Unit
Economics of Health Care in the Intensive Care Unit
One of the catalysts driving the growth of pharmacoeconomics is the staggering cost of health care. In 2009, healthcare spending in the United States increased to a total of $2.6 trillion, and it is projected to be 4.7 trillion in 2019, which would represent 19.3% of the U.S. Gross Domestic Product (GDP).7 Hospital sector spending in the United States increased 86% in 2009 to $761 billion.
U.S. prescription drug expenditures were $300 billion in 2009, representing a 5% increase from 2008.8 Data in nonfederal hospitals for 2008 reveal that drug expenditures increased by 2.1% to $27 billion, and injectable drugs accounted for 71% of these expenditures.8 In 2008, the top 10 therapeutic classes accounted for 73% of hospital drug expenditures, with antineoplastic agents being the highest expenditure at $3.3 billion. The top two individual drugs in 2008 were enoxaparin at $1.1 billion and immune globulin at $868 million.
The cost of drug therapy is complex and comprises multiple components. Table 190-1 summarizes the cost of the drug product versus the cost of complications.9 It is easy to obtain data on acquisition costs of drugs and materials to prepare and administer drugs. Determining the cost of drug failures or adverse drug events is far more challenging, however, and often is not considered. The estimated annual costs of drug-related problems in the United States increased from $77.6 billion in 1995 to $155 billion in 2000.10
| Cost of a Drug | Cost of a Complication |
|---|---|
| Acquisition cost | Increased morbidity cost |
| Associated material preparation and delivery cost | Increased mortality cost |
| Number of doses per day cost | Increased total cost |
| Route of administration cost | Increased length of stay |
| Labor preparation and administration cost | Increased intensity of care |
| Decreased patient satisfaction |
Intensive care units (ICUs) consume significant hospital resources. Quantifying costs attributable to ICU care is complex, since both patients and their costs are constantly being shifted to and from the ICU, and different hospitals use different cost accounting systems. However, the large economic burden of the ICU is out of proportion to the number of ICU beds in the institution. In 2005, 95,000 ICU beds accounted for only 7% of all inpatient beds in the United States yet consumed about 13% of inpatient costs, or $82 billion annually.11 Furthermore, this figure represents 4% of national health expenditures. The cost of an ICU day is estimated to be three to four times the cost of a ward day and has increased 30% from 2000 to 2005.12 One study reported that daily ICU costs averaged $3518 during 2000-2005,12 but a large database of more than 50,000 patients from 252 ICUs revealed a mean ICU cost of $19,725.13 Daily ICU costs were greatest on day 1 (average $7728), decreased on day 2 (average $3872), and stabilized on day 3 and beyond at approximately $4200 in 2009 dollars. Mechanically ventilated patients had the highest ICU costs; use of a ventilator increased average daily cost by $1800 compared to ICU patients who were not receiving mechanical ventilation. Therapeutic interventions that can reduce ICU length of stay by even 1 day can have a significant impact on total hospital costs, particularly in patients requiring mechanical ventilation. Cost saving initiatives are particularly relevant in this setting, since only 83% of hospital costs are covered for Medicare patients with an ICU admission.14 This discrepancy can result in a $5.8 billion loss to hospitals when ICU care is required.
Drug costs in the ICU are difficult to quantify because most hospitals are not sufficiently computerized to track these data. In one academic medical center, 15 drugs accounted for more than 50% of drug costs in the ICU.15 Drug costs in the ICU averaged 38% of the hospital’s total drug costs and increased at a higher rate than non-ICU drug costs over the 4-year period studied (12.4% versus 5.9%). Fiscal year 2002 data revealed an ICU drug cost of $312 per day compared with $112 per day outside of the ICU.
 Economic Evaluations in Critical Care Medicine
Economic Evaluations in Critical Care Medicine
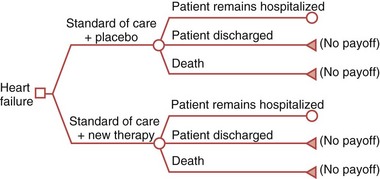
Although any economic analysis could be performed in a critical care environment, some of the more appropriate are cost-effectiveness analysis, cost-benefit analysis, cost minimization analysis, cost utility analysis, and cost of illness.16 Cost-effectiveness evaluation is discussed in greater depth because it is the most commonly performed and the approach recommended by expert bodies.17
In 1996, the Panel on Cost-Effectiveness in Health and Medicine (PCEHM) published seminal work consisting of guidelines for the conduct and reporting of economic analyses.18 This work resulted in some key points to consider when employing a cost-effectiveness evaluation, including use of a reference case for comparison, the importance of transparent methods and logic, and consideration of the perspective being evaluated. The PCEHM recommends that the societal perspective is the most comprehensive and considers workforce and familial aspects of illness. The PCEHM recommends using the following steps when designing a cost-effectiveness analysis:
The American Thoracic Society convened a workshop to address the application of the PCEHM guidelines to a critical care environment.19 A group of experts compiled key considerations for a cost-effectiveness evaluation in the ICU, and details can be reviewed in their report.
Cost utility analysis is a form of cost-effectiveness evaluation that examines the utility or value of an outcome.16 Patient, family member, provider, or societal preferences can value health outcomes. Cost per quality-adjusted life-year can be measured for alternative therapies by assessing the length of time a patient is in a state of health rated on a scale of 0 to 1, where 0 equals death, and 1 equals perfect health.
The American Recovery and Reinvestment Act of 2009 provided considerable funding for comparative effectiveness research and mandated that the Institute of Medicine (IOM) of the National Academy of Sciences recommend initial national priorities for this research.20 Its purpose is to compare the ratio of cost to effectiveness of two interventions used for the same condition.16 These comparisons should be evaluated in the real-world setting and could provide data about which interventions are most effective for patients under specific circumstances.8 It has been estimated that these data could reduce spending by Medicare and Medicaid by $0.1 billion from 2008 to 2012 and $1.3 billion between 2008 and 2017.
 Determining Costs in the Intensive Care Unit
Determining Costs in the Intensive Care Unit
Three approaches frequently are used to assess the economic burden of a disease state: prospective study design, retrospective analysis, and decision modeling.17 A prospective study gives the investigator an opportunity to measure important variables completely and accurately. Retrospective database analysis reviews data that already have been assembled and has the advantage of being much less costly and time consuming than prospective studies with the ability to review many patients easily.
In retrospective studies, the subjects already are assembled and have been de-identified, baseline measurements have been made, and the follow-up period has occurred. The total direct and indirect costs of a condition can be readily assessed. Total direct costs include the value of all goods, services, and other resources consumed in the provision of an intervention or in dealing with the side effects of the intervention or other current or future consequences linked to the intervention.21 Indirect costs are the costs that result from a certain therapy or illness, such as lost wages, workforce replacement, or child care that may be necessary.
Patient billing information and summary estimates of department-level expenditures can be used to estimate costs when hospital administrative data are used. At one extreme, hospital charges can be used as a proxy of costs. This approach may be reasonable in a comparative analysis of interventions, assuming that charges per admission are roughly proportional to economic costs per admission. Another approach is to use the department’s cost-to-charge ratio, which has been shown to perform accurately when evaluating average costs per diagnosis-related group.22
 Cost of Intensive Care Unit–Related Conditions
Cost of Intensive Care Unit–Related Conditions
Evaluation of the economic impact of medical conditions is one of several areas of focus since the 1990s in ongoing efforts to decrease overall healthcare spending and identify high-cost diseases to target therapies. More recently, hospital-acquired conditions have received increased attention. Several of these are so-called never events that are not reimbursed by government payers.23 Representative conditions of the 10 identified areas for 2009 and 2010 include deep venous thrombosis (DVT) or pulmonary embolism (PE) developing after total knee or hip replacements, extreme manifestations of poor glycemic control, and surgical site infections. Recently, a study analyzed the performance of several hundred hospitals for hospital-acquired conditions and their associated additional costs.24 Top conditions and their associated annual costs were decubitus ulcers ($536,900), DVT and PE ($564,000), and infections ($252,600). Preventing these conditions from developing could result, for example, in a 200-bed hospital saving $2 million per year.
Acute Congestive Heart Failure
Among the nearly 5 million Americans with congestive heart failure, the number of hospital discharges has increased by 165% in the past 20 years.25 Acute congestive heart failure is the reason for at least 20% of hospital admissions in patients older than 65 years of age and the most expensive admission diagnosis, with an estimated $39.2 billion spent in the United States during 2010.26 In 1998, the cost per admission of a congestive heart failure patient was $5471, and in 2001, hospitals lost on average $1288 per Medicare patient.27 In fact, one large database study conducted in 2005 revealed 50% of heart failure admissions had costs that exceeded the DRG (diagnosis-related group) payment.28 More recent data reveal that the mean hospital cost per admission was $21,800 in 2009 dollars, and that 75% of admissions with acute heart failure developed this condition as a secondary diagnosis.29 As such, the global burden of acute heart failure may be underestimated from these data, since statistics are generated from patients with a primary diagnosis of heart failure.26
Acute Kidney Injury
Despite considerable information on the clinical effects of acute kidney injury (AKI), there have been only seven studies describing costs associated with this condition.30 There are substantial differences in methods, such as different definitions of the condition and different definitions of costs. As such, comparisons are difficult. The median hospital costs adjusted to 2008 dollars range from $3300 in patients with uncomplicated AKI to $56,095 from the start of renal replacement therapy to hospital discharge.30 One study reported that the median postoperative costs of AKI following coronary artery bypass surgery was $44,800 compared to $21,900 in controls in 2009 dollars.31 Even patients with small increases in serum creatinine postoperatively, namely 1.5 times baseline, had higher postoperative costs ($35,400), whereas patients with the most severe AKI had costs of $62,700 (median value).
Infectious Diseases
Healthcare-Acquired Infections
Hospital staffs recognize the importance of preventing infections in patients admitted to their institution. By implementing appropriate procedures and guidelines, hospitals can save on costs associated with these infections. Importantly, the government will not reimburse hospitals if patients develop infections such as catheter-associated urinary tract infections, vascular catheter–associated bloodstream infections, and surgical site infections. The Centers for Disease Control and Prevention (CDC) recently summarized the literature on this topic in a comprehensive published report.32 They estimate that overall annual direct medical costs of 1.7 million healthcare-associated infections ranged from $28.4 to $33.8 billion, depending on the method used for adjusting to 2007 dollars. They furthermore state that prevention can save $5.7 to $6.8 billion for preventing only 20% of infections. The attributable patient costs are separated by infection site and are shown in Table 190-2. A sample from 69 million hospital discharges between 1998 and 2006 revealed 558,000 identified cases, and costs were adjusted to 2006 dollars.33 For patients with invasive surgery, the attributable mean length of stay was 11 days with hospital costs of $32,000 for sepsis and 14 days and $46,400 for pneumonia, respectively. The corresponding values for patients without invasive surgery were 6 days and $12,700 for sepsis and 9.7 days and $22,300 for pneumonia, respectively. Another recent evaluation of costs of nosocomial infections34 reviewed 1.3 million admissions from 55 hospitals; costs were adjusted to 2007 dollars. The 58,000 cases of nosocomial infections had a mean added total hospital cost of $12,200 (95% confidence interval [CI], $4862-$19533). The highest costs were seen in cerebrospinal fluid and respiratory infections.
TABLE 190-2 Average Attributable Costs per Patient of Hospital-Associated Infections by Sites of Infection
| Infection Site | Low Estimate Adjusted to 2007 Dollars Using CPI-U | High Estimate Adjusted to 2007 Dollars Using CPI-U |
|---|---|---|
| Surgical site infection | $11,087 | $29,443 |
| Central line–associated bloodstream infection | $6,461 | $25,849 |
| Ventilator-associated pneumonia | $14,806 | $27,520 |
| Catheter-associated urinary tract infection | $749 | $832 |
| Clostridium difficile–associated disease | $5,682 | $8,090 |
CPI-U, consumer price index for all urban consumers.
Ventilator-associated pneumonia (VAP) is a frequent complication of mechanical ventilation in critically ill patients and is associated with a 20% to 54% ICU mortality rate.35,36 Studies published through 2004 estimated that the cost of VAP ranges from $5365 to $10,062 per patient. One study determined the attributable cost of VAP in a nonteaching U.S. medical center.37 Compared with noninfected mechanically ventilated patients, patients with VAP had a higher incidence of bacteremia (36% versus 22%), longer ICU length of stay (26 versus 4 days), and greater mortality rate (50% versus 34%). Hospital costs for VAP patients were significantly higher ($70,568 versus $21,620), with a higher proportion of total costs being room, nursing, pharmacy, and respiratory therapy expenses. The cost differences for patients developing early-onset compared to late-onset VAP were $36,822 versus $60,562. The attributable cost of VAP when adjusted for a wide variety of factors was $11,897 (95% CI, $5265-$26,214). Approaches that provide even a small clinical effect can have a significant economic benefit.35,36
Additional recent studies have quantified costs of bloodstream infections, colitis due to Clostridium difficile infection, catheter-related infections, and severe sepsis.38–41 A study of catheter-associated bloodstream infections in a medical and surgical ICU at a nonteaching hospital revealed an incidence of 4%, with an attributable total hospital cost of $14,200 in 2009 dollars.38 The catheter-related infections were associated with an attributable ICU length of stay of 2.4 days. Infections caused by C. difficile are a common cause of diarrhea in hospitalized patients, and many of these patients are in ICUs. A review of the literature reveals that the incremental costs in 2008 dollars ranged from $2800 to $4800 for primary infection and $13,600 to $18,000 for recurrent disease.39 The hospital records of 1.3 million patients revealed 22% of patients had a bloodstream infection.40 Incremental costs of these patients in 2006 dollars averaged $19,400. When infections occurring after hospital day 7 were excluded, costs were estimated at $20,600.
Severe Sepsis
The incidence of severe sepsis in the United States is estimated to be 751,000 cases per year, and the mortality rate is estimated to be 28.6%, which increases to 38.4% in patients older than 85 years. The average cost per case of severe sepsis in 2009 dollars is $31,100. The estimated annual 2009 cost in the United States is $23.5 billion.41
One cautionary note is that the costs of healthcare-associated infections may be overstated due to shortcomings in assessing costs and related outcomes. The authors suggest complete economic evaluations that include changes to all costs and health benefits be performed. Readers are referred to the primary article for more detail on this topic.42
Venous Thromboembolism
Approximately 1 million patients develop venous thromboembolism in the United States, with an annual cost estimated at $3 to $4 billion.43 Some estimates of the financial consequences of hospitalized patients developing a DVT or PE add $8000 to $14,000 to the bill of general medical ward patients.44 For patients developing both conditions, additional costs rise to $28,000 per patient. For patients with recurrent disease or readmitted within 1 year, DVT and PE add $11,800 and $14,700, respectively. Hospital stays can be doubled. The Centers for Medicare and Medicaid Services (CMS) in the United States does not reimburse hospitals for the additional costs associated with the development of a DVT or PE. This puts extreme pressures on hospitals to initiate prevention measures, especially in high-risk patients.
Delirium
Annual costs of delirium on the healthcare system are estimated to be between $38 and $152 billion.45 Some of these costs can be attributed to inpatient care. Delirium has a significant correlation with increased ICU and hospital length of stay.46 Milbrandt and colleagues were the first to assess the costs of delirium in mechanically ventilated patients.47 They reported that ICU costs are increased by approximately $10,900 and hospital costs by $17,000 in 2009 dollars for patients who experienced at least one episode of delirium, compared to patients who did not develop delirium. Optimizing approaches to detection of delirium and finding the best strategies to treat this condition could alleviate the economic burden.
Miscellaneous Conditions
There are some additional diseases for which the burden of illness had been estimated. Approximately 74.5 million patients in the United States have hypertension, and the estimated cost associated with this condition in 2010 was $76.6 billion.26 Approximately 1% of these patients present to emergency departments with acute hypertension.48 One study evaluated a claims database of patients hospitalized with hypertension as a secondary diagnosis.49 For the 123,000 admissions with acute hypertension, 13% of total hospital costs were a result of hypertension, which represents $2734 in 2005 dollars. This cost ($3540) was highest for patients with a primary diagnosis of ischemic heart disease. Of interest, the cost attributable to hypertension was still $2254 for patients without ischemic heart disease or cerebrovascular disease, thus documenting the need for cost-effective therapies in these patients. Stroke has a major economic impact, with a prevalence of 6.4 million Americans affected and 795,000 new or recurrent patients per year.50 The estimated total and indirect medical costs for 2010 were $78 billion.26 Costs obtained from a database of 8 million admissions for spontaneous intracranial hemorrhage from 1000 hospitals stated that hospital charges increased 61% from 2003 to 2005.50 The mean hospital charge was $43,200 per patient (adjusted for 2005 dollars), and the aggregate charges in 2005 were $2.9 billion. Finally, a review of 71 studies from 1996-2006 that included the cost of stroke revealed a mean hospital cost of $17,250 ($468-$65,250).51
 Cost of Pharmacotherapy in Critical Care
Cost of Pharmacotherapy in Critical Care
Antimicrobials
Appropriateness of Therapy and Resistance
Antimicrobials are commonly used in the ICU to prevent and treat a wide range of infections.52 The acquisition cost of an antimicrobial is only one component of the cost associated with use of these agents. In fact, one study revealed that the acquisition cost of gentamicin represented only 33% of the total antimicrobial costs for this drug.53
Additional cost drivers associated with antimicrobial use include the treatment of resistant organisms. Methicillin-resistant Staphylococcus aureus (MRSA) is increasingly prevalent in ICUs. A review of the literature pertaining to the cost impact of these bacteria revealed three studies.54 Direct medical costs of MRSA from a database of over 1 million patients with community-acquired infections was $49,300 (adjusted for 2009 dollars). Another study of nosocomial bloodstream infections showed the costs of treating resistant organisms were threefold higher than the costs for treating sensitive organisms. In a study of 188 ICU patients treated for MRSA, the costs (from 2002-2004 data) of initially inappropriate antibiotic therapy was $10,000 greater than the cost of appropriate therapy.55 The cost difference is thought to be the result of 4 extra days of stay in the ICU required by the patients who received inappropriate therapy. Economic analysis of gram-negative bacterial resistance in the ICU also was reviewed.56 One study reported that patients with infections caused by antibiotic-resistant Enterobacteriaceae stayed 4 more days in the ICU and had $58,300 more in hospital charges (2009 dollars) than patients with infections caused by drug-sensitive organisms. When patients with resistant Pseudomonas aeruginosa infections were compared to patients with drug-sensitive infections, ICU length of stay increased from 1 to 6 days, and charges in 2009 dollars were $13,000 to $32,900 higher. An additional study of healthcare-associated infections caused by resistant gram-negative bacteria reported that the mean hospital cost was $151,500 (range $152-$1,056,000) in 2008 dollars.57 A univariate analysis of hospital costs showed that the median total cost for patients with infections caused by resistant bacteria was $38,000 higher than for patients with infections caused by susceptible bacteria.
Several studies have evaluated strategies and protocols to minimize the development of resistance to antibiotics and optimize management of septic patients in the ICU to reduce the incidence of resistance and cost of therapy. For example, an educational protocol for nurses and respiratory therapists was developed.58 This program resulted in a 57% decrease in VAP, with an estimated cost savings in the following 12 months of $425,000. Using a before-and-after study design, Shorr et al. described the economics of a broad-based sepsis protocol based on the Surviving Sepsis Campaign recommendations at their 1200-bed institution.59,60 The estimated development cost was $5000. The average per-patient total hospital costs in 2005 dollars was approximately $6000, or a total cost difference of $573,000 for the 120 patients studied, despite a higher survival rate in the protocol group. The cost difference was driven by a 35% reduction in ICU costs and a 30% reduction in ward costs following the use of the protocol. A decision analysis was performed to estimate the costs of implementing early goal-directed therapy for severe sepsis and septic shock.61 Using 2005 dollars, the authors estimated startup costs of $13,000 for the ICU-based strategy, $30,000 for the emergency department (ED)-based strategy, and an annual outlay of $100,113. The estimated annual total cost savings of this protocol for 91 patients was $789,000. In contrast, implementing the early goal-directed therapy for sepsis at one hospital resulted in a mean increase in 2004 total hospital cost of $8800, an increased ICU length of stay, and higher pharmacy costs, largely driven by a lower mortality rate in protocol patients.62 Further analysis revealed that implementation of this protocol resulted in a cost per quality-adjusted life-year gain of $16,000. This amount is considerably lower than $50,000, a value often used as a threshold for a therapy to be considered cost-effective in medical care.63 Additionally, protocols that focus on appropriate antimicrobial usage have been shown to have favorable clinical and economic benefits.64 Antimicrobial stewardship programs include tailoring antimicrobials to the cultured organism following broad-spectrum initial coverage, formulary restriction, guidelines and clinical pathways, decision support systems, and intravenous-to-oral conversion programs. They have demonstrated a 22% to 36% decrease in antimicrobial usage and annual cost savings of $200,000 to $900,000 in addition to reduced mortality and shorter lengths of stay.64 Whether shorter courses of antibiotics or procalcitonin testing to guide the duration of antibiotic therapy will reduce ICU or hospital costs while maintaining effectiveness remains to be documented.65,66
Drotrecogin Alfa (Activated)
A cost-effectiveness analysis of drotrecogin alfa (activated) was conducted in conjunction with a clinical trial of the safety and efficacy of this recombinant protein as an adjuvant treatment for severe sepsis.67 The acquisition cost of a course of drotrecogin alfa (activated) for a 70-kg patient is approximately $7000. Despite the fact that there were more survivors among patients treated with drotrecogin alfa (activated) compared with placebo, there were no significant differences in costs per patient or resource use, excluding the cost of the drug. The cost per survivor was estimated to be $160,000. Long-term costs and outcomes were modeled, assuming that survivors lived an average of 12.2 years, with utility adjusted to 8.4 quality-adjusted life-years. The cost-effectiveness was $33,000 per life-year saved and the cost per quality-adjusted life-year was $48,800. The cost per quality-adjusted life-year in patients with an APACHE II score greater than 25 was $27,400. Reimbursement for 71 patients with severe sepsis treated with drotrecogin alfa was assessed,68 and the total treatment cost between December 2001 and December 2003 was $6.3 million, whereas reimbursement was $4.3 million, representing a loss of nearly $2 million, or $28,000 per patient.
Sedatives
Although there are many publications on appropriate sedation pharmacotherapy, it is surprising that only a few studies have evaluated the costs associated with treating agitation.69 In addition to sedative drug acquisition costs, there are costs associated with oversedation, such as prolonged time on the ventilator, and costs of undersedation, such as development of ischemic heart disease, respiratory depression and ileus associated with excessive opioid use, and ineffective treatment of delirium. The economic literature on ICU sedation consists mainly of studies comparing drug acquisition costs between treatments.69 Two recent studies have evaluated the cost of care associated with various sedatives. One was a decision analysis of a randomized clinical trial of lorazepam versus propofol in adult mechanically ventilated patients, using a daily sedative interruption method.70 The findings revealed that propofol was cost-effective in 91% of the simulations and resulted in an average total hospital cost saving of $6378 in 2007 dollars and an increase in 3.7 ventilator-free days. Despite the higher cost of propofol, it saved total hospital costs, mainly by reducing time on the ventilator. Finally, a cost minimization analysis was conducted of a randomized clinical trial of dexmedetomidine versus midazolam in adult mechanically ventilated patients.71 Despite an $1100 higher median acquisition cost for dexmedetomidine compared to midazolam, the total ICU cost in the patients randomized to dexmedetomidine was nearly $10,000 less in 2007 dollars. This cost difference was driven mainly by lower ICU and mechanical ventilator costs. We need studies that capture all costs from study patients, including costs of adverse drug reactions, healthcare provider time using time-motion studies, nursing satisfaction, and a variety of cost-effectiveness ratios.69
Thromboprophylaxis and Treatment of Deep Venous Thrombosis
In the past, several studies have shown the cost-effectiveness of low-molecular-weight heparins such as enoxaparin compared to unfractionated heparin.72 More recent economic studies have evaluated the newer agent, fondaparinux. One study used a decision model that evaluated a cohort of 1000 hypothetical patients with DVT treated with either enoxaparin or fondaparinux.73 Despite biasing the model against fondaparinux, there was a 40% reduction in total costs with use of the newer agent, with drug acquisition costs being the major driver. An incremental cost analysis of a randomized clinical trial of fondaparinux versus enoxaparin for total knee replacement revealed a $1081 total cost savings per venous thrombotic event avoided by using fondaparinux.72 Also, in medical patients, low-molecular-weight heparins saved $89 per patient in 2004 dollars compared to unfractionated heparin, despite the higher acquisition costs associated with the low-molecular-weight heparin formulations.72 The data appear to favor low-molecular-weight heparins from both a clinical and economic perspective, compared to unfractionated heparin.
Miscellaneous Conditions
Intensive insulin therapy to maintain tight glycemic control is an important topic for ICUs and can be associated with clinical benefit as long as hypoglycemia can be avoided.74 The recently published NICE-SUGAR study reported a higher mortality rate in patients randomized to an intensive glucose control group versus conventional therapy.75 The intensive glucose control group had a higher incidence of hypoglycemia.
One study evaluated costs (in 2004 dollars) in 800 medical/surgical ICU patients in each cohort, using a before-and-after method of tight glucose control compared to usual care.74 There was a 14% reduction in ICU days following the protocol and a decrease in total hospital costs of $1500 per patient, which translated to a total annualized decrease of $1.3 million. An economic analysis of a randomized clinical trial in surgical ICU patients revealed total ICU costs were 25% lower for patients randomized to intensive insulin therapy.76 Protocol patients had fewer days requiring mechanical ventilation and a shorter ICU stay. These economic studies apply to the patient population studied. Any economic advantage of intense glucose control should be balanced by the documented effects on mortality.
Although not traditionally considered a drug, blood transfusion also has a variety of components beyond the acquisition cost of blood that add to the total cost of a transfusion. A recent activity-based cost analysis from four hospitals evaluated transfusion-related processes, usage factors, and direct and indirect costs to determine the total transfusion cost.77 Whereas the average acquisition cost of a unit of red blood cells ranged from $150 to $250, the average total cost per red blood cell unit was $760 (range $522-$1183). Annual costs from the four hospitals in 2007 ranged from $1.6 million to $6 million.
 Cost of Adverse Drug Events
Cost of Adverse Drug Events
Adverse drug event (ADE) detection can be challenging, but it is important because the attributable costs can be substantial.78,79 Cullen et al.80 performed the first comparison of patients experiencing an ADE in the ICU to patients experiencing ADEs in general care units. This study had several notable findings: (1) the rate of ADEs was nearly doubled in the ICU compared to a general care unit, because critically ill patients received twice the number of medications; (2) the severity of ADEs was greater in the ICU compared to general care units; and (3) the costs after an ADE occurred were higher in the ICU compared to general care units, although the difference was not statistically significant. The additional costs post ADE in the ICU were approximately $9000 compared to the general care unit after adjusting to 2010 values. Another evaluation in the surgical ICU reported about a 2-day increase in length of stay for patients experiencing an ADE compared to those not having an ADE.81
The intravenous route of administration is commonly used for ICU patients. Intravenous administration of drugs can increase the risk and/or severity of ADEs, since the drug immediately enters into the bloodstream, allowing for maximal absorption and relatively quick onset. A study was conducted in three ICUs at an academic institution and two ICUs in a nonacademic institution to evaluate the cost and length of stay associated with intravenous administration–related ADEs.82 Interestingly, the nonacademic institutions did not demonstrate a difference in the cost or length of stay associated with ADEs compared to controls. The academic institutions had $6691 greater costs (2010 values) and a length of stay 4.8 days longer compared to controls.
Considering the cost of a specific ADE, such as heparin-induced thrombocytopenia (HIT), will provide clinicians a further appreciation for the impact of unintended drug responses. A matched case-control study designed to evaluate the financial impact of HIT reported additional costs ranging between $15,500 and $20,300 (2010 values) and about a 15-day longer length of stay.83 Although only 22 cases were evaluated, the substantial cost associated with HIT seems apparent. Another evaluation of HIT showed that the cost for patients exposed to unfractionated heparin was significantly greater (by $61,000) compared to HIT in patients exposed to low-molecular-weight heparins.84 Prevention programs aimed at immediate detection and management of HIT could provide institutional cost savings.
Another example of costly ADEs is opioid-related events.85 A matched case-control study identified 741 patients experiencing an opioid-related ADE during a 6-year period; these subjects were compared to 10,116 controls. The results were reported according to surgery type. The costs attributable to ADEs ranged from $636 to $990 (2010 values). The ADEs were associated with about a half-day increase in length of stay compared to controls. The patient population selected for this study was surgical patients, but we can imagine the financial impact in critically ill patients that receive high doses and prolonged courses of opioids.
 Economic Impact of Critical Care Pharmacists
Economic Impact of Critical Care Pharmacists
There have been several studies documenting the clinical and economic impact of pharmacists involved with several areas of patient care, including the ED and ICU.86–88 For the ICU pharmacist, the literature up to 2003 documented reductions in medication errors, adverse drug events, and reduced rates of VAP.86 The economic outcomes in 2010 dollars range from annual savings of $34,000 in cost avoidance to $355,000 in reductions of adverse drug events. Using large Medicare databases, more recent studies have compared outcomes from ICUs that have clinical pharmacists to those without clinical pharmacists.89,90 In patients with infections, institutions with a clinical pharmacist reported lower mortality rates in the ICU, shorter ICU lengths of stay, lower drug charges, and lower Medicare billing charges. In ICU patients with nosocomial-acquired infections from 272 hospitals, the Medicare charges per patient in hospitals with clinical pharmacists was approximately $12,000 less, resulting in over $132 million in reduced total charges for 25,000 patients. In 141,000 patients with thromboembolic or infarction-related events, the presence of an ICU pharmacist was associated with a 37% lower mortality rate and a 15% shorter ICU length of stay.90 Average Medicare charges per patient were $3400 lower, resulting in over $215 million in total charges in 2005 dollars. Although these two studies do not prove causal effects, it appears that the presence of a clinical pharmacist is associated with substantial cost savings in patients with common conditions seen in ICU patients.
Key Points
Drummond MF, Sculpfer MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. New York: Oxford University Press; 2005.
, Format for formulary submissions (FMCP), Version 3.0. Academy of Managed Care Pharmacy and evidence-based and value-based formulary guidelines. Available at. http://www.amcp.org/amcp.ark?p=0F6E1295. Accessed March 18, 2010
Dasta J, Kim SR, McLaughlin TP, Mody S, Piech CT. Incremental daily cost of mechanical ventilation in patients receiving treatment in an intensive care unit. Crit Care Med. 2005;33:1266-1271.
Dasta JF, Kane-Gill SL, Pencina M, Shehabi Y, Bokesch P, Riker R. A cost-minimization analysis of dexmedetomidine compared to midazolam for long-term sedation in the intensive care unit. Crit Care Med. 2010;38:497-503.
Dobesh P. Economic burden of venous thromboembolism in hospitalized patients. Pharmacotherapy. 2009;29:943-953.
Eber MR, Laxminarayan R, Perencevich EN, Malani A. Clinical and economic outcomes attributable to healthcare-associated sepsis and pneumonia. Arch Intern Med. 2010;170:347-353.
Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix and costs. Crit Care Med. 2010;38:65-71.
Zilberberg MD. Understanding cost-effectiveness in the ICU. Semin Respir Crit Care Med. 2010;31:13-18.
This article reviews methods for evaluating healthcare costs as they apply to the ICU environment.
Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson A, Leape LL. Preventable adverse drug events in hospitalized patients: a comparative study of intensive care units and general care units. Crit Care Med. 1997;25:1289-1297.
Weber RJ, Kane SL, Oriolo VA, et al. Impact of intensive care unit (ICU) drug use on hospital cost: a descriptive analysis, with recommendations for optimizing ICU pharmacotherapy. Crit Care Med. 2003;31:S17-S24.
1 Pittoni GM, Scatto A. Economics and outcome in the intensive care unit. Curr Opin Anesthesiol. 2009;22:232-236.
2 Mauskopf JA. Why study pharmacoeconomics? Expert. Rev Pharmacoecon Outcomes Res. 2001;1:1-3.
3 Coughlin MT, Angus DC. Economic evaluation of new therapies in critical illness. Crit Care Med. 2003;31:S7-16.
4 Format for Formulary Submissions (FMCP), Version 3.0. Academy of Managed Care Pharmacy. Available at. http://www.amcp.org/amcp.ark?p=0F6E1295. Accessed March 18, 2010
5 Available at: http://www.ashp.org/economy-survey Accessed March 19, 2010
6 Rubino M, Hoffman JM, Koesterer LJ, et al. ASHP guidelines on medication costs management strategies for hospitals and health systems. Am J Health Syst Pharm. 2008;65:1368-1384.
7 Highlights—national health expenditures, 2010. National health care expenditures projections: 2010-2019. Available at. http://www.cms.hhs.gov/NationalHealthExpendData/downloads/NHE_Extended_Projections.pdf. Accessed March 19, 2010
8 Hoffman JM, Doloresco F, Vermeulen LC, et al. Projecting future drug expenditures—2010. Am J Health Syst Pharm. 2010;67:919-928.
9 Dasta J, Kane-Gill S. Pharmacoeconomics of sedation in the ICU. Crit Care Clin. 2009;25:571-583.
10 Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: Updating the cost-of-illness model. J Am Pharm Assoc. 2001;41:192-199.
11 Halpern NA, Pastores SM. Critical care medicine in the united states 2000-2005: An analysis of bed numbers, occupancy rates, payer mix and costs. Crit Care Med. 2010;38:65-71.
12 Halpern NA. Can the costs of critical care be controlled? Curr Opin Crit Care. 2009;15:591-596.
13 Dasta J, Kim SR, McLaughlin TP, Mody S, Piech CT. Incremental daily cost of mechanical ventilation in patients receiving treatment in an intensive care unit. Crit Care Med. 2005;33:1266-1271.
14 Cooper LM, Linde-Zwirble WT. Medicare intensive care unit use: Analysis of incidence, cost, and payment. Crit Care Med. 2004;32:2247-2253.
15 Weber RJ, Kane SL, Oriolo VA, et al. Impact of intensive care unit (ICU) drug use on hospital cost: A descriptive analysis, with recommendations for optimizing ICU pharmacotherapy. Crit Care Med. 2003;31:S17-S24.
16 Zilberberg MD. Understanding cost-effectiveness in the ICU. Semin Respir Crit Care Med. 2010;31:13-18.
17 Drummond MF, Sculpfer MJ, Torrance GW, O’Brien BJ, Stoddart GL. methods for the economic evaluation of health care programmes. New York: Oxford University Press; 2005.
18 Weinstein MC, Siegel JE, Gold MR, et al. Panel on cost-effectiveness in health and medicine: Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1253-1258.
19 Angus DC, Rubenfeld GD, Roberts MS, et al. Understanding costs and cost-effectiveness in critical care: Report from the Second American Thoracic Society Workshop on Outcomes Research. Am J Respir Crit Care Med. 2002;165:540.
20 VanLare JM, Conway PH, Sox HC. Five next steps for a new national program for comparative-effectiveness research. New Engl J Med. 2010;362:970-973.
21 Kahn J. Understanding economic outcomes in critical care. Curr Opin Crit Care. 2006;12:399-404.
22 Swartz M, Young DW, Siegrist R. The ratio of costs to charges: How good a basis for estimating costs? Inquiry. 1995;32:476-481.
23 Straube B, Blum JD. The policy on paying for treating hospital-acquired conditions: CMS officials respond. Health Aff. 2009;28:1494-1497.
24 Http://www.hmc-benchmarks.com. Accessed March 20, 2010
25 Ng T, Singh A, Dasta JF, et al. Contemporary issues in the pharmacologic management of acute heart failure. Crit Care Clin. 2006;22:199-219.
26 American Heart Association. 2010 Heart and stroke statistical update. Available at. http://www.americanheart.org/. Accessed March 20, 2010
27 Peacock WF. Clinical and economic impact of nesiritide. Am J Health Syst Pharm. 2003;60(Suppl 4):S21-S26.
28 Hauptman PJ, Swindle J, Burroughs TE, Schnitzler MA. Resource utilization in patients with heart failure: insights from a contemporary national hospital database. Am Heart J. 2008;155:978-985.
29 Ng T, Dasta JF, Feldman DF, et al. Differences in patients with a primary vs secondary discharge diagnosis of heart failure from a database of 2.5 million admissions: Implications for health care policy reform. Conges Heart Fail. 2008;14:202-210.
30 Dasta JF, Kane-Gill SL. Economic impact of acute kidney failure. In: Jorres A, Ronco C, Kellum J, editors. Management of acute kidney problems. New York: Springer Publications; 2009:75-80.
31 Dasta JF, Kane-Gill S, Durtschi AJ, Pathak D, Kellum J. Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol Dial Transplant. 2008;23:1970-1974.
32 The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. Available at. http://www.cdc.gov/ncidod/dhqp/pdf/Scott_CostPaper.pdf.
33 Eber MR, Laxminarayan R, Perencevich EN, et al. Clinical and economic outcomes attributable to health care-associated sepsis and pneumonia. Arch Intern Med. 2010;170:347-353.
34 Kilgore ML, Ghosh K, Beavers CM, et al. The costs of nosocomial infections. Med Care. 2008;46:101-104.
35 Shorr AF, Wunderink RG. Dollars and sense in the intensive care unit: The costs of ventilator-associated pneumonia. Crit Care Med. 2003;31:1582-1583.
36 Safdar N, Dezfulian C, Collard HR. Clinical and economic consequences of ventilator-associated pneumonia: A systematic review. Crit Care Med. 2005;33:2184-2193.
37 Warren DK, Shukla SJ, Olsen MA, et al. Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in suburban medical center. Crit Care Med. 2003;31:1312-1317.
38 Warren DK, Quadir WW, Hollenbeak CS, et al. Attributable cost of catheter-associated bloodstream infections among intensive care patients in a nonteaching hospital. Crit Care Med. 2006;34:2084-2089.
39 Ghantoji SS, Sail K, Lairson DR, et al. Economic healthcare costs of Clostridium difficile infection: a systematic review. J Hosp Infect. 2010;74:309-318.
40 Kilgore M, Brossette S. Cost of bloodstream infections. Am J Infect Control. 2008;36:S172.e1-S172.e3.
41 Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the US. Analysis of the incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303-1310.
42 Graves N, Harbarth S, Beyersmann J, et al. Estimating the cost of health care-associated infections: mind your p’s and q’s. Clin Infect Dis. 2010;50:1017-1021.
43 Dobesh PP. Economic burden of venous thromboembolism in hospitalized patients. Pharmacotherapy. 2009;29:943-953.
44 Chan CM, Shorr AF. Venous thromboembolic disease in the intensive care unit. Semin Respir Crit Care Med. 2010;31:39-46.
45 Leslie DL, Marcantonio ER, Zhang Y, et al. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168:27-32.
46 Ely EW, Gautm S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27:1892-1900.
47 Milbrandt EB, Deppen S, Harrison PL, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004;32:955-962.
48 Katz JN, Gore JM, Amin A, et al. Practice patterns, outcomes, and end-organ dysfunction for patients with acute severe hypertension: results from the Studying the Treatment of Acute Hypertension Registry. Am Heart J. 2009;158:599-606.
49 Wang G, Zhang Z, Ayala C. Hospitalization costs associated with hypertension as a secondary diagnosis among insured patients aged 18-64 years. Am J Hypertens. 2009;23:275-281.
50 Andaluz N, Zuccarello M. Recent trends in the treatment of spontaneous intracerebral hemorrhage: analysis of a nationwide inpatient database. J Neurosurg. 2009;110:403-409.
51 Luengo-Fernandez R, Gray AM, Rothwell PM. Costs of stroke using patient-level data. Stroke. 2009;40:e18-e23.
52 Kuster SP, Ruef C, Ledesrgerber B, et al. Quantitative antibiotic use in hospitals: comparison of measurements, literature review, and recommendations for a standard of reporting. Infection. 2008;36:549-559.
53 van Zanten ARH, Engelfriet PM, van Dillen K, et al. Importance of nondrug costs of intravenous antibiotic therapy. Crit Care. 2003;7:R184-R190.
54 Shorr AF. Epidemiology and economic impact of methicillin-resistant Staphylococcus aureus. Pharmacoeconomics. 2007;25:751-768.
55 Shorr AF, Micek ST, Kollef M. Inappropriate therapy for methicillin-resistant Staphylococcus aureus: resource utilization and cost implications. Crit Care Med. 2008;36:2335-2340.
56 Shorr AF. Review of studies of the impact on gram-negative bacterial resistance on outcomes in the intensive care unit. Crit Care Med. 2009;37:1463-1469.
57 Mauldin PD, Salgado GD, Hansen IS, et al. Attributable hospital cost and length of stay associated with health care-associated infections caused by antibiotic-resistant gram-negative bacteria. Antimicrob Agents Chemother. 2010;54:109-115.
58 Kollef MH, Micek ST. Using protocols to improve patient outcomes in the intensive care unit: focus on mechanical ventilation and sepsis. Semin Respir Crit Care Med. 2010;31:19-30.
59 Shorr AF, Micek ST, Jackson WL. Economic implications of an evidence-based sepsis protocol: can we improve outcomes and lower costs? Crit Care Med. 2007;35:1257-1262.
60 Dellinger RP, Carlet JM, Masur H, et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858-873.
61 Huang DT, Clermont G, Dremsizov TT, et al. Implementation of early goal-directed therapy for severe sepsis and septic shock: a decision analysis. Crit Care Med. 2007;35:2090-2100.
62 Talmor D, Greenberg D, Howell MD, et al. The costs and cost-effectiveness of an integrated sepsis treatment protocol. Crit Care Med. 2008;36:1168-1174.
63 Grosse SD. Assessing cost-effectiveness in healthcare: history of the $50,000 per QALY threshold. Expert Rev Pharmacoecon Outcomes Res. 2008;8:165-178.
64 Njoku JC, Hermsen ED. Antimicrobial stewardship in the intensive care unit: a focus on potential pitfalls. J Pharm Pract. 2010;23:50-60.
65 Pugh RJ, Cook RPD, Dempsey G. Short course antibiotic therapy for gram-negative hospital-acquired pneumonia in the critically ill. J Hosp Infect. 2010;74:337-343.
66 Bouadma l, Luyt C, Tubach F, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomized controlled trial. Lancet. 2010;375:463-474.
67 Angus DC, Linde-Zwirble WT, Clermont G, et al. Cost-effectiveness of drotrecogin alfa (activated) in the treatment of severe sepsis. Crit Care Med. 2003;31:1-54.
68 Smith BS, Schroeder WS, Tataronis GR. Hospital reimbursement for adult patients with severe sepsis treated with drotrecogin alfa (activated). Hosp Pharm. 2005;40:146-153.
69 Dasta JF, Kane-Gill S. Pharmacoeconomics of sedation in the ICU. Crit Care Clin. 2009;25:571-583.
70 Cox CE, Reed SD, Govert JA, et al. Economic evaluation of propofol and lorazepam for critically ill patients undergoing mechanical ventilation. Crit Care Med. 2008;36:706-714.
71 Dasta JF, Kane-Gill SL, Pencina M, et al. A cost-minimization analysis of dexmedetomidine compared to midazolam for long-term sedation in the intensive care unit. Crit Care Med. 2010;38:497-503.
72 Shorr AF. The pharmacoeconomics of deep vein thrombosis treatment. Am J Med. 2007;120:S35-S41.
73 Shorr AF, Jackson WL, Moores LK, et al. Minimizing costs for treating deep vein thrombosis: the role for fondaparinux. J Thromb Thrombolysis. 2007;23:229-236.
74 Krinsley JS, Jones RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest. 2006;129:644-650.
75 The NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283-1297.
76 Van den Berghe G, Wouters PJ, Kesteloot K, et al. Analysis of healthcare resource utilization with intensive insulin therapy in critically ill patients. Crit Care Med. 2006;34:612-616.
77 Shander A, Hofmann A, Ozawa S, et al. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010;50:753-765.
78 Kane-Gill SL, Devlin JW. Adverse drug event reporting in the intensive care unit: a survey of current practices. Ann Pharmacother. 2006;40:1267-1273.
79 Stockwell D, Kane-Gill SL. Developing a patient safety surveillance system to prevent adverse drug events in the ICU. Crit Care Med. 2010;38:S117-S125.
80 Cullen DJ, Sweitzer BJ, Bates DW, et al. Preventable adverse drug events in hospitalized patients: a comparative study of intensive care units and general care units. Crit Care Med. 1997;25:1289-1297.
81 Vargas E, Terleira A, Hernando F, et al. Effect of adverse drug reactions on length of stay in surgical intensive care units. Crit Care Med. 2003;31:694-698.
82 Nuckols TK, Paddock SM, Bower AG, et al. Costs of intravenous adverse drug events in academic and nonacademic intensive care units. Med Care. 2008;46:17-24.
83 Smythe MA, Koerber JM, Fitzgerald M, Matson JC. The financial impact of heparin-induced thrombocytopenia. Chest. 2008;134:568-573.
84 Baroletti S, Piovella C, Fanikos J, et al. Heparin-induced thrombocytopenia: clinical and economic outcomes. Thromb Haemost. 2008;100:1130-1135.
85 Oderda GM, Said Q, Evans RS, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother. 2007;41:400-407.
86 Kane SL, Weber RJ, Dasta JF. The impact of critical care pharmacists on enhancing outcomes. Intensive Care Med. 2003;29:691-698.
87 De Rijdt T, Willems L, Simoens S. Economic effects of clinical pharmacy interventions: a literature review. Am J Health Syst Pharm. 2008;65:1161-1172.
88 Cohen V, Jellinek SP, Hatch A, et al. Effect of clinical pharmacists on care in the emergency department: a systematic review. Am J Health Syst Pharm. 2009;66:1353-1361.
89 MacLaren R, Bond CA, Martin SJ, et al. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infections. Crit Care Med. 2008;36:3184-3189.
90 MacLaren R, Bond CA. Effects of pharmacist participation in intensive care units on clinical and economic outcomes of critically ill patients with thromboembolism or infarction-related events. Pharmacotherapy. 2009;29:761-768.