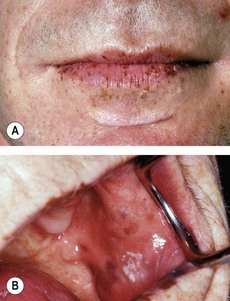
181 Peutz–Jeghers syndrome
Salient features
Advanced-level questions
What are the types of colonic polyp?
• Tubular adenomas: over 60% are in the rectosigmoid colon and may cause bleeding or obstruction. The risk of malignancy correlates with size. The tubular adenoma is removed endoscopically. Follow-up surveillance is by colonoscopy every 2 years.
• Villous adenomas are usually found in the left colon and have a high risk of malignancy. Polyps larger than 2 cm have a 50% risk of malignancy. They may present with hypokalaemia as a result of potassium loss in the stools. They are removed by colonoscopic resection.
• Hyperplastic polyps are benign and rarely undergo malignant change. They are usually detected as an incidental finding at colonoscopy.
What polyposis syndromes do you know?
Familial adenomatous polyposis and variants:
• Familial adenomatous polyposis (FAP) is an autosomal dominant condition with the defect localized to APC on chromosome 5q21 (N Engl J Med 1993;329:1982). There are several thousand polyps in the colon, which start to appear between the ages of 10 and 35 years. The potential malignant change is 100% by the age of 40 years. Hence all relatives should be screened annually from the age of 12 years and all patients should have prophylactic colectomy by the age of 30. A protein assay can diagnose the genetic defect in 87% of such families, and 150 mg sulindac twice daily has been shown to reduce the number and size of the adenomatous polyps in the rectum (N Engl J Med 1993;328:1313). Another promising drug is celecoxib, a cyclooxygenase-2 inhibitor (N Engl J Med 2000;342:1946–52), which significantly reduces the number of colorectal polyps. Calcium supplementation has been shown to reduce the risk of recurrent colorectal adenomas (N Engl J Med 1999;340:101–7).
• Gardner syndrome. This is a variant of FAP in which affected members develop extraintestinal soft tissue tumours (osteomas, lipomas, dermoid tumours) and pigmentation of fundi.
• Turcot syndrome. In this varient, CNS gliomas may also develop. Disruption of any of three genes—APC, hMLH1 or hPMS2—can lead to Turcot syndrome (N Engl J Med 1995;332:839–47).
Other polyposis syndromes
• Familial juvenile polyposis is an autosomal dominant condition occurring in children and teenagers. It causes GI bleeds, abdominal pain, diarrhoea and intussusception. There is an increased incidence of malignant change in the interspersed adenomatous polyps. The affected genes are Smad4 (DPC4), BMPRIA, PTEN.
• Peutz-Jeghers syndrome is an autosomal dominant condition characterized by mucocutaneous melanosis with GI hamartomas. The intestinal polyps may give rise to haematemeis, melaena or rectal bleeding, anaemia or intussusception depending on their location. These polyps are usually found in the ileum and jejunum and they rarely undergo malignant change. However, affected people tend to have an increased incidence of other malignancies, both of GI tract (stomach and duodenum) and other viscera (lung, breasts, pancreas and gonads).
• Cronkhite–Canada syndrome comprises sporadic, colonic, small bowel or gastric polyps associated with ectodermal changes such as hyperpigmentation, nail atrophy and alopecia.
• Cowden’s disease is is an autosomal dominant condition characterized by multiple GI hamartomas with warty papules on the mucosa, and skin malformations. The affected genes are PTEN (MMAC1, DEP1).
• Bannayan–Ruvalcaba–Riley syndrome comprises microcephaly, hamartoatous polyps, fibromatosis, speckled penis and haemangiomas. The affected gene is PTEN.