CHAPTER 64 Peritoneum and peritoneal cavity
The peritoneum is the largest serous membrane in the body, and its arrangements are complex. In males it forms a closed sac, but in females it is open at the lateral ends of the uterine tubes. It consists of a single layer of flat mesothelial cells lying on a layer of loose connective tissue. The mesothelium usually forms a continuous surface, but in some areas may be fenestrated. Neighbouring cells are joined by junctional complexes, but probably permit the passage of macrophages. The submesothelial connective tissue may also contain macrophages, lymphocytes and adipocytes (in some regions). Mesothelial cells may transform into fibroblasts, which may play an important role in the formation of peritoneal adhesions after surgery or inflammation of the peritoneum.
GENERAL ARRANGEMENT OF THE PERITONEUM
In utero, the alimentary tract develops as a single tube suspended in the coelomic cavity by ventral and dorsal mesenteries (see Ch. 73). Ultimately, the ventral mesentery is largely resorbed, although some parts persist in the upper abdomen and form structures such as the falciform ligament. The mesenteries of the intestines in the adult are the remnants of the dorsal mesentery. The migration and subsequent fixation of parts of the gastrointestinal tract produce the so-called ‘retroperitoneal’ segments of bowel (duodenum, ascending colon, descending colon, and rectum), and four separate intraperitoneal bowel loops suspended by mesenteries of variable lengths. These are all covered by visceral peritoneum which is continuous with the parietal peritoneum covering the posterior abdominal wall. The first intraperitoneal loop is formed by the intraperitoneal oesophagus, the stomach and first part of the duodenum. The second loop is made up of the duodenojejunal junction, jejunum, ileum and occasionally the caecum and proximal ascending colon. The third loop contains the transverse colon and the final loop contains the sigmoid colon and occasionally the distal descending colon.
Where the visceral peritoneum encloses or suspends organs within the peritoneal cavity, the peritoneum and related connective tissues are known as the peritoneal ligaments, omenta or mesenteries. All but the greater omentum are composed of two layers of visceral peritoneum separated by variable amounts of connective tissue. The greater omentum is folded back on itself and is therefore made up of four layers of closely applied visceral peritoneum, which are separated by variable amounts of adipose tissue. The mesenteries attach their respective viscera to the posterior abdominal wall: the attachment is referred to as the mesenteric root, and the peritoneum of the mesentery is continuous with that of the posterior abdominal wall in this area (Fig. 64.1).
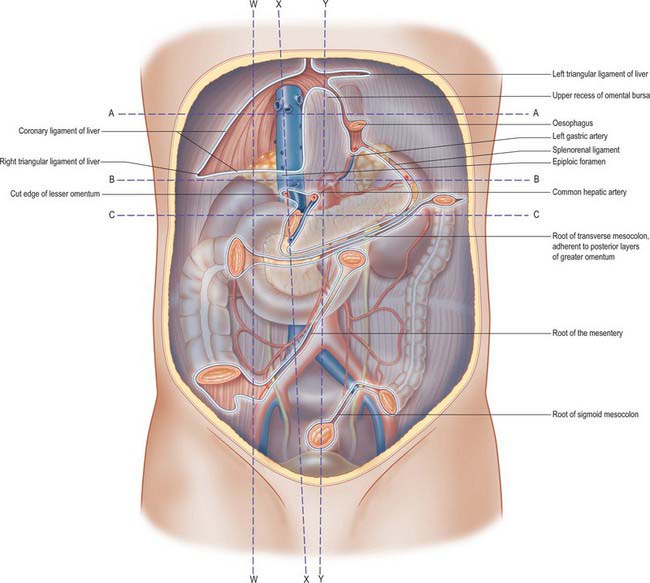
Fig. 64.1 The posterior abdominal wall, showing the lines of peritoneal reflection, after removal of the liver, spleen, stomach, jejunum, ileum, caecum, transverse colon and sigmoid colon. The various sessile (retroperitoneal) organs are seen shining through the posterior parietal peritoneum. Note: the ascending and descending colon, duodenum, kidneys, suprarenals, pancreas and inferior vena cava. Line W–W represents the plane of Fig. 64.2. Line X–X represents the plane of Fig. 64.3. Line Y–Y represents the plane of Fig. 64.4. Line A–A represents the plane of Fig. 64.5A. Line B–B represents the plane of Fig. 64.5B. Line C–C represents the plane of Fig. 64.5C.
PERITONEUM OF THE UPPER ABDOMEN
The abdominal oesophagus, stomach, liver and spleen all lie within a double fold of visceral peritoneum which runs from the posterior to the anterior abdominal wall. This fold has no recognized name, but has been referred to as the mesogastrium by Coakley & Hricak 1999 because it is derived from the fetal mesogastrium. It has a complex attachment to the wall of the abdominal cavity and gives rise to the falciform ligament, coronary ligaments, lesser omentum (gastrohepatic and hepatoduodenal ligaments), greater omentum (including gastrocolic ligament), gastrosplenic ligament, splenorenal ligament, and phrenicocolic ligament (Figs 64.2, 64.3, 64.4).
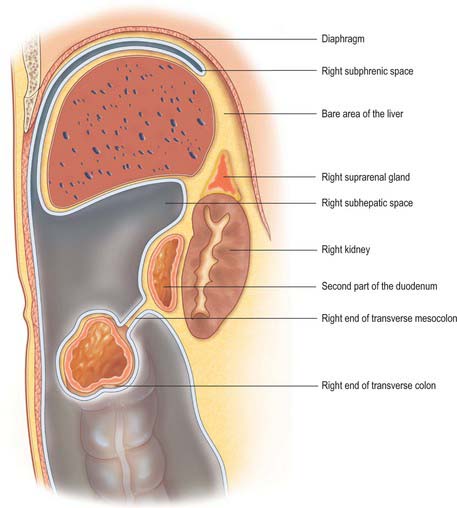
Fig. 64.2 Sagittal section through the abdomen to the right of the epiploic foramen along one line of W–W in Fig. 64.1.
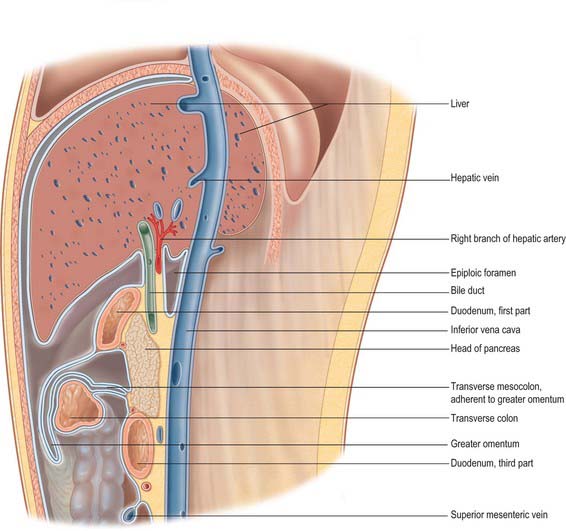
Fig. 64.3 Section through the upper part of the abdominal cavity, along the line X–X in Fig. 64.1. The boundaries of the epiploic foramen are shown and a small recess of the lesser sac is displayed in front of the head of the pancreas. Note that the transverse colon and its mesocolon are adherent to the posterior two layers of the greater omentum.
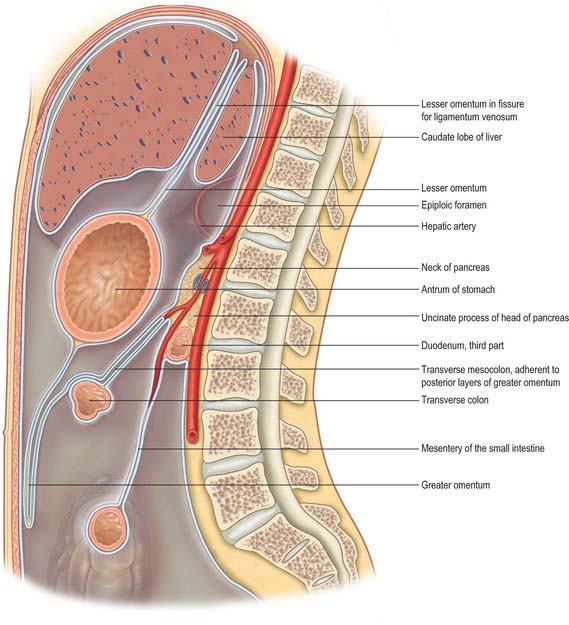
Fig. 64.4 Sagittal section through the abdomen, approximately in the median plane. Compare with Fig. 64.1. The section cuts the posterior abdominal wall along the line Y–Y in Fig. 64.1. The peritoneum is shown in blue except along its cut edges, which are left white.
The falciform ligament
The falciform ligament is a thin anteroposterior peritoneal fold which connects the liver to the posterior aspect of the anterior abdominal wall just to the right of the midline. It extends inferiorly to the level of the umbilicus, and is widest between the liver and umbilicus. The ligament narrows superiorly as the distance between the liver and anterior abdominal wall reduces and narrows to just a centimetre or so in height over the superior surface of the liver. Its two peritoneal layers divide to enclose the liver and are continuous with the visceral peritoneum that is adherent to the surface of the liver. Superiorly, they are reflected onto the inferior surface of the diaphragm and are continuous with the parietal peritoneum over the right dome. At the posterior limit, or apex, of the falciform ligament, the two layers are also reflected vertically left and right, and are continuous with the anterior layers of the left triangular ligament and the superior layer of the coronary ligament of the liver. The inferior aspect of the falciform ligament forms a free border where the two peritoneal layers become continuous with each other as they fold over to enclose the ligamentum teres. Because the peritoneum of the falciform ligament is continuous with that covering the posterior abdominal wall and the periumbilical anterior abdominal wall, blood arising from retroperitoneal haemorrhage (commonly acute haemorrhagic pancreatitis) may track between the folds of peritoneum and appear as haemorrhagic discolouration around the umbilicus (Cullen’s sign). Inflammatory change from the pancreas may spread via the gastrohepatic ligament (lesser omentum) and then via the falciform ligament to the umbilicus.
The peritoneal connections of the liver
The liver is almost completely covered in visceral peritoneum, and only the ‘bare area’ is in direct contact with the right dome of the diaphragm. Peritoneal folds, the ligaments of the liver, run from the liver to the surrounding viscera and to the abdominal wall and diaphragm (Fig. 64.5); they are described in detail in Chapter 68.
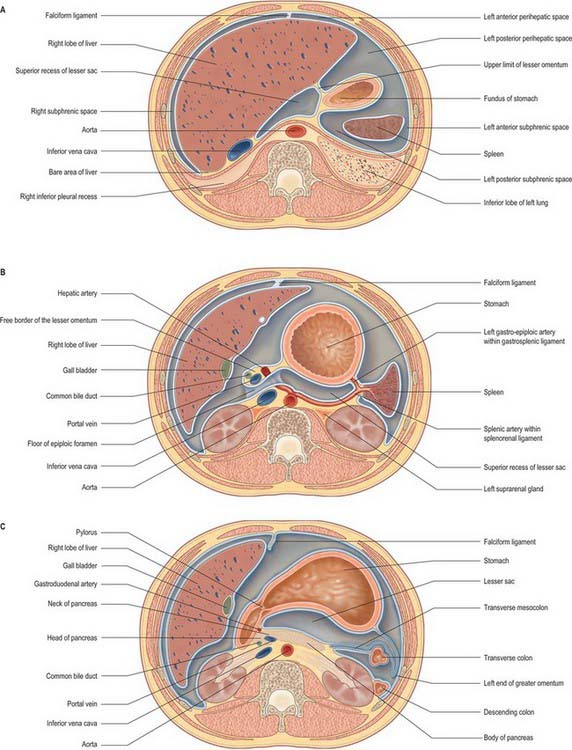
Fig. 64.5 Transverse sections through the abdomen. A, At the level of the line A–A in Fig. 64.1. The line passes through the bare area of the liver at the superior end of the lesser omentum. The parts of the left subphrenic space are clearly seen although they are continuous with each other. B, At the level of line B–B in Fig. 64.1, viewed from below. The peritoneal cavity is shown by a blue ‘wash’; the peritoneum and its cut edges in pale blue. C, Transverse section through the abdomen at the level of the line C–C in Fig. 64.1, viewed from below. Colours as in Fig. 64.1.
The right triangular ligament is a short V-shaped fold formed by the approximation of the two layers of the coronary ligament at its right lateral end, and is continuous with the peritoneum of the right posterolateral abdominal wall. The coronary ligament is reflected inferiorly and is directly continuous with the peritoneum over the upper pole of the right kidney. This fold is sometimes referred to as the hepatorenal ligament. The recess formed between the peritoneum of the inferior surface of the liver, the hepatorenal ligament and the peritoneum over the right kidney is known as the hepatorenal pouch (of Morison). In the supine position this is the most dependent part of the peritoneal cavity in the upper abdomen, and is a common site of pathological fluid accumulation.
The peritoneum is reflected inferolaterally from the posterior layer of the left triangular ligament onto the posterior abdominal wall above the oesophageal opening of the diaphragm. It lines the inferior surface of the left dome of the diaphragm and continues backwards onto the posterior abdominal wall. Inferiorly, it is reflected behind the spleen onto the most lateral part of the mesentery of the transverse colon and the splenic flexure. It continues down lateral to the descending colon into the pelvis, and forms the left paracolic ‘gutter’. Medially, the peritoneum covering the left upper posterior abdominal wall is reflected anteriorly to form the left layer of the upper end of the lesser omentum, the peritoneum over the left aspect of the abdominal oesophagus and the left layer of the splenorenal ligament.
The greater omentum
The greater omentum is the largest peritoneal fold and hangs inferiorly from the greater curvature of the stomach. It is a double sheet: each sheet consists of two layers of peritoneum separated by a scant amount of connective tissue. The two sheets are folded back on themselves and are firmly adherent to each other. The anterior sheet descends from the greater curvature of the stomach and first part of the duodenum. The most anterior layer is continuous with the visceral peritoneum over the anterior surface of the stomach and duodenum and the posterior layer is continuous with the peritoneum over the posterior wall of the stomach and pylorus. The anterior sheet descends a variable distance into the peritoneal cavity and then turns sharply on itself to ascend as the posterior sheet. The posterior sheet passes anterior to the transverse colon and transverse mesocolon. It is attached to the posterior abdominal wall above the origin of the small intestinal mesentery and anterior to the head and body of the pancreas. The anterior layer of the posterior sheet is continuous with the peritoneum of the posterior wall of the lesser sac. The posterior layer is reflected sharply inferiorly and is continuous with the anterior layer of the transverse mesocolon. The posterior sheet is adherent to the transverse mesocolon at its root and is often known as the gastrocolic ligament, which is the supracolic part of the greater omentum. In early fetal life the greater omentum and transverse mesocolon are separate structures, and this arrangement sometimes persists. During surgical mobilization of the transverse colon, the plane between the transverse mesocolon and greater omentum can be entered opposite the taenia omentalis, and the greater omentum can be separated entirely from the transverse colon and mesocolon if required. Access into the lesser sac can be obtained via this approach if the upper part of the posterior sheet of the greater omentum is then divided. This gives a relatively bloodless plane of entry for surgical access to the posterior wall of the stomach and to the anterior surface of the pancreas. The greater omentum is continuous with the gastrosplenic ligament on the left, and on the right it extends to the start of the duodenum. A fold of peritoneum, the hepatocolic ligament, may run from either the inferior surface of the right lobe of the liver or the first part of the duodenum to the right side of the greater omentum or hepatic flexure of the colon.
PERITONEUM OF THE LOWER ABDOMEN
Transverse mesocolon
The mesentery of the transverse colon is a broad fold of visceral peritoneum reflected anteriorly from the posterior abdominal wall and suspends the transverse colon in the peritoneal cavity. The root of the transverse mesocolon lies along an oblique line passing from the anterior aspect of the second part of the duodenum, over the head and neck of the pancreas, above the duodenojejunal junction and over the upper pole of the left kidney to the splenic flexure (Fig. 64.1). It varies considerably in length but is shortest at either end. It contains the middle colic vessels and their branches together with branches of the superior mesenteric plexus, lymphatics and regional lymph nodes. Its two layers pass to the posterior surface of the transverse colon, where they separate to cover the colon. The upper layer of peritoneum is reflected from the posterior abdominal wall immediately anteriorly and inferiorly and becomes continuous with the posterior layer of the greater omentum to which it is adherent. The lower layer of peritoneum of the transverse mesocolon is continuous with the peritoneum of the posterior abdominal wall. Lateral extensions of the transverse mesocolon produce two shelf-like folds on the right and left sides of the abdominal cavity. On the right the duodenocolic ligament extends from the transverse mesocolon at the hepatic flexure to the second part of the duodenum. On the left the phrenicocolic ligament extends from the transverse mesocolon at the splenic flexure to the diaphragm at the level of the eleventh rib. The root of the transverse mesocolon is closely related to the upper limit of the root of the mesentery of the small intestine near the uncinate process of the pancreas.
Mesentery of the small intestine
The mesentery of the small intestine is arranged as a complex fan formed from two layers of peritoneum (anterosuperior and posteroinferior) separated by connective tissue and vessels. The root of the mesentery lies along a line running diagonally from the duodenojejunal flexure on the left side of the second lumbar vertebral body to the right sacroiliac joint (Fig. 64.1). The root crosses over the third part of the duodenum, aorta, inferior vena cava, right ureter and right psoas major. The average length of the root of the mesentery is 15 cm in adults; while along its intestinal attachment is the same length as the small intestine (approximately 5 m), and consequently the mesentery is usually thrown into multiple folds along its intestinal border. The average depth of the mesentery from the root to the intestinal border is 20 cm, but this varies along the length of the small intestine: it is shortest at the jejunum and terminal ileum and longest in the region of the mid ileum. Its two peritoneal layers contain the jejunum, ileum, jejunal and ileal branches of the superior mesenteric vessels, branches of the superior mesenteric plexus, lacteals and regional lymph nodes. Because of the length and mobility of the mesentery, identification of the proximal and distal ends of a loop of small intestine may be difficult through small surgical incisions. Tracing the continuity of the right peritoneal layer of the mesentery onto the posterior abdominal wall above the root towards the ascending colon, and the continuity of the left layer towards the descending and sigmoid colon, may be useful in helping to orientate an individual loop of ileum. The mesentery of the small intestine is sometimes joined to the transverse mesocolon at the duodenojejunal junction by a peritoneal band. Occasionally the fourth part of the duodenum possesses a very short mesentery which is continuous with the upper end of the root of the small bowel mesentery. Pronounced bands of peritoneum may extend to the posterior abdominal wall at the terminal ileum. The root of the mesentery of the small intestine is continuous with the peritoneum surrounding the appendix and caecum in the right iliac fossa.
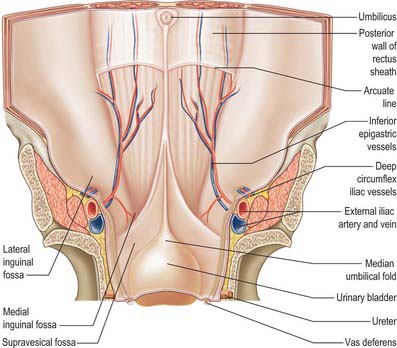
PERITONEUM OF THE LOWER ANTERIOR ABDOMINAL WALL
The peritoneum of the lower anterior abdominal wall is raised into five ridges which diverge as they descend from the umbilicus. These are the median and right and left lateral and medial umbilical folds (Fig. 64.6). The median umbilical fold extends from the umbilicus to the apex of the bladder and contains the urachus or its remnant (Ch. 78). The obliterated umbilical artery lies under the medial umbilical fold which ascends from the pelvis to the umbilicus. The supravesical fossa lies between the medial and median umbilical folds on either side of the midline. The lateral umbilical fold covers the inferior epigastric artery and vein below their entry into the rectus sheath, and is separated from the medial umbilical fold by the medial inguinal fossa. The lateral inguinal fossa lies lateral to the lateral umbilical fold, and covers the deep inguinal ring. The femoral fossa lies inferomedial to the lateral inguinal fossa, from which it is separated by the medial end of the inguinal ligament. It overlies the femoral ring (see Ch. 61).
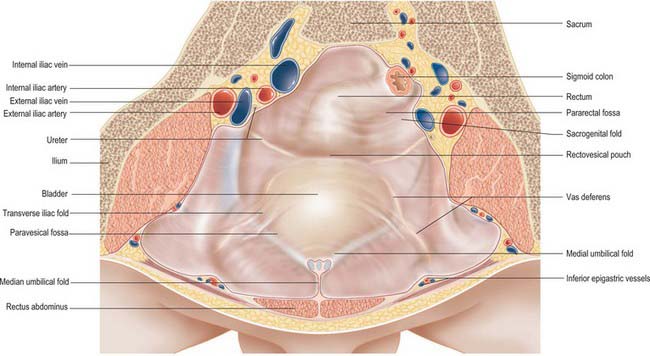
PERITONEUM OF THE PELVIS
Peritoneum of the male pelvis
In males, the peritoneum of the left lower abdominal wall is reflected from the junction of the sigmoid colon and anterolateral surface of the rectum to line the brim and upper inner surface of the true pelvis (Fig. 64.7). The peritoneum passes down into the true pelvis, lying over the anterior surface of the rectum, which then becomes an extraperitoneal organ. Laterally, the peritoneum is reflected to the pelvic side walls to form the right and left pararectal fossae: these vary in size according to the degree of distension of the rectum. The peritoneum is reflected anteriorly from the anterior surface of the rectum over the upper poles of the seminal vesicles and onto the posterior surface of the bladder, producing the rectovesical pouch. Anteriorly the rectovesical pouch is limited laterally by peritoneal folds, the sacrogenital folds, which extend from the sides of the bladder posteriorly to the anterior aspect of the sacrum. The peritoneum covers the superior surface of the bladder, and forms a paravesical fossa on each side limited laterally by a ridge of peritoneum which contains the ductus deferens. The size of the paravesical fossae depends on the volume of urine in the bladder. When the bladder is empty, a variable transverse vesical fold divides each fossa into two. The anterior ends of the sacrogenital folds may sometimes be joined by a ridge separating a middle fossa from the main rectovesical pouch. Between the paravesical and pararectal fossae the ureters and internal iliac vessels may cause slight elevations in the peritoneum. From the apex of the bladder the peritoneum extends superiorly along the posterior surface of the lower anterior abdominal wall to the umbilicus. When the bladder distends, the peritoneum is lifted from the lower anterior abdominal wall so that part of the anterior surface of the bladder is in direct contact with the posterior surface of the lower median area of the anterior abdominal wall. This relationship means that a well-distended bladder can be entered by direct puncture through the lower anterior abdominal wall without entering the peritoneal cavity (suprapubic puncture).
Peritoneum of the female pelvis
In females the peritoneum covers the upper rectum as it does in the male, but it descends further over the anterior surface of the rectum. The lateral limit of the pararectal and paravesical fossae is the peritoneum covering the round ligament of the uterus. The rectovesical pouch is occupied by the uterus and vagina. The peritoneum from the rectum is thus reflected anteriorly onto the posterior surface of the posterior fornix of the vagina and the uterus, producing the recto-uterine pouch (of Douglas). The peritoneum covers the fundus of the uterus to its anterior (vesical) surface as far as the junction of the body and cervix, from which it is reflected forwards to the upper surface of the bladder, forming a shallow vesico-uterine pouch. Peritoneum is reflected from the bladder to the posterior surface of the anterior abdominal wall as it is in males. Marginal recto-uterine folds correspond to the sacrogenital folds in males and pass back to the sacrum from the sides of the cervix, lateral to the rectum. Peritoneum is reflected from the anterior and posterior uterine surfaces to the lateral pelvic walls as the broad ligament of the uterus (see Fig. 77.18). This consists of anteroinferior and posterosuperior layers which are continuous at the upper border of the ligament. The broad ligament extends from the sides of the uterus to the lateral pelvic walls, and contains the uterine tubes in its free superior margins and the ovaries attached to its posterior layer. Below, it is continuous with the lateral pelvic parietal peritoneum. Between the ridges formed by the obliterated umbilical arteries and the ureter, the peritoneum forms a shallow depression on the lateral pelvic wall, the ovarian fossa, which lies behind the lateral attachment of the broad ligament. The ovary usually rests in the fossa in nulliparous females.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Parietal and visceral peritoneum develop from the somatopleural and splanchnopleural layers respectively of lateral plate mesoderm (see Ch. 73). Parietal peritoneum is therefore supplied by somatic blood vessels of the abdominal and pelvic walls and its lymphatics join those in the body wall and drain to parietal lymph nodes. Visceral peritoneum is best considered as an integral part of the viscera which it overlies; it derives its blood supply from the viscera, and its lymphatics join the visceral vessels to drain to the regional lymph nodes.
INNERVATION
The visceral peritoneum and viscera are not affected by these stimuli because the visceral afferent innervation provides a much more limited sensation of discomfort. When stimulated, the sensation of pain is of a less severe nature and is referred to the area of abdominal wall according to the region of the intestinal tract affected. Discomfort from structures derived from the foregut is felt in the region of the epigastrium, from midgut structures in the region of the umbilicus, and from hindgut structures in the suprapubic region: none of these sensations shows significant lateralization. However, stretch of the visceral peritoneum is a potent cause of certain sensations and responses. Various neural elements in the visceral walls, mesenteries and overlying peritoneum mediate poorly localized sensations of discomfort when stimulated by stretch, and may also elicit profound reflex autonomic reactions involving vasomotor and cardiac changes. This is of considerable clinical relevance. The effects of division of the parietal peritoneum may be rendered painless by local or regional local anaesthesia. In marked contrast, the direct central connections of the visceral afferents, particularly via the vagus, mean that stretching the visceral peritoneum may have profound effects, and may produce acute haemodynamic instability despite high spinal anaesthesia. Ischaemia of the underlying viscera causes poorly localized abdominal pain, probably due to the spasms of visceral smooth muscle.
GENERAL ARRANGEMENT OF THE PERITONEAL CAVITY
SUPRAMESOCOLIC COMPARTMENT
Lesser sac (omental bursa)
Epiploic foramen (of Winslow)
The epiploic foramen (foramen of Winslow, aditus to the lesser sac), is a short, vertical slit, usually 3 cm in height in adults, in the upper part of the right border of the lesser sac. It leads into the greater sac. The hepatoduodenal ligament, which is formed by the thickened right edge of the lesser omentum extending from the flexure between the first and second parts of the duodenum, forms the anterior margin of the foramen. The anterior border contains the common bile duct (on the right), portal vein (posteriorly) and hepatic artery (on the left) between its two layers. Superiorly the peritoneum of the posterior layer of the hepatoduodenal ligament runs over the caudate lobe of the liver which forms the roof of the epiploic foramen. This layer of peritoneum is then reflected onto the inferior vena cava which forms the posterior margin of the epiploic foramen. At the upper border of the first part of the duodenum the peritoneum runs forwards from the inferior vena cava, above the head of the pancreas, and is continuous with the posterior layer of the lesser omentum, forming the floor of the epiploic foramen. A narrow passage, the vestibule of the lesser sac, may be found to the left of the foramen between the caudate process and the first part of the duodenum. To the right, the rim of the foramen is continuous with the peritoneum of the greater sac. The roof is continuous with the peritoneum on the inferior surface of the right hepatic lobe. The anterior and posterior walls of the foramen are normally apposed.
INFRAMESOCOLIC COMPARTMENT
RECESSES OF THE PERITONEAL CAVITY
Duodenal recesses
Several folds of peritoneum may exist around the fourth part of the duodenum and the duodenojejunal junction forming a number of named recesses (Fig. 64.8).
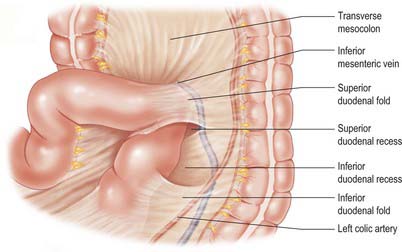
Fig. 64.8 The superior and inferior duodenal recesses. The transverse colon and jejunum have been displaced.
Superior duodenal recess
The superior duodenal recess is occasionally present, usually in association with an inferior duodenal recess. It lies to the left of the end of the fourth part of the duodenum, opposite the second lumbar vertebra, and behind a crescentic superior duodenal fold (duodenojejunal fold). The fold has a semilunar free lower edge which merges to the left with the peritoneum anterior to the left kidney. The inferior mesenteric vein is directly behind the junction of the left (lateral) end of this fold and the posterior parietal peritoneum. The recess varies in size but is commonly 2 cm deep, admitting a fingertip. It opens downwards, its orifice being in the angle formed by the left renal vein as it passes across the abdominal aorta.
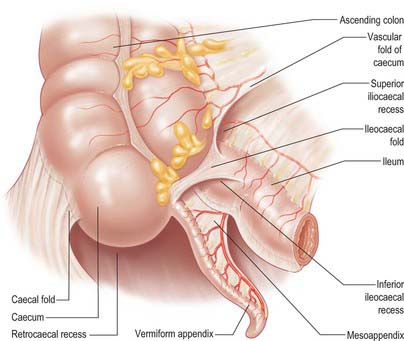
Caecal recesses
Several folds of peritoneum may exist around the caecum and form recesses (Fig. 64.9). Paracaecal recesses are common sites for abscess formation following acute appendicitis.
CLINICAL MANAGEMENT OF FLUID COLLECTIONS IN THE PERITONEAL CAVITY
Fluid collections caused by inflammatory processes are often much more viscid because they contain pus, fibrin or blood and are usually associated with peritoneal inflammation which results in, at least transient, peritoneal adhesions. These factors mean that collections may become localized if the flow of fluid is restricted by the partial compartmentalization of the peritoneum. Once collected in a particular ‘space’, this fluid often becomes further confined by ongoing inflammation and may even form a truly walled-off cavity over time. Any of the spaces of the peritoneum may develop a collection, but the subphrenic, subhepatic and pelvic spaces are the commonest since they are most well defined by the fixed peritoneal folds and organs forming their boundaries. These spaces are also the most dependent spaces within the peritoneum in the supine position and consequently any initially free fluid tends to gravitate to them.
Coakley FV, Hricak H. Imaging of peritoneal and mesenteric disease: key concepts for the clinical radiologist. Clin Radiol. 1999;54:563-574.
Healy JC, Reznek RH. The anterior abdominal wall and peritoneum. In: Butler P, Mitchell A, Ellis H. Applied Radiological Anatomy. Cambridge: Cambridge University Press; 1999:189-200.
Meyers M. Dynamic Radiology of the Abdomen. In Normal and Pathologic Anatomy. New York: Springer; 1994.