CHAPTER 5 Peripheral Tears of the TFCC: Arthroscopic Diagnosis and Management
Anatomy and Biomechanics
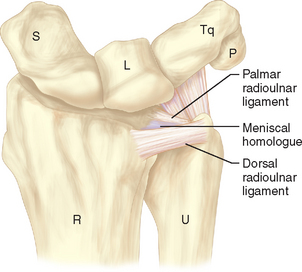
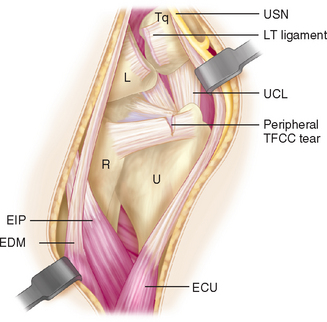
The anatomy of the triangular fibrocartilage complex (TFCC) is primarily composed of the articular disc (or triangular fibrocartilage), a meniscus homologue, dorsal and volar radioulnar ligaments, the extensor carpi ulnaris (ECU) tendon subsheath, and the ulnocarpal ligaments (ulnolunate, ulnotriquetral, and ulnocapitate)—as depicted in Figures 5.1 and 5.2. The triangular fibrocartilage is a meniscus-like structure composed predominantly of type I collagen. Surrounding the periphery of the triangular fibrocartilage is the meniscal homologue, a fibrocartilaginous rim of dense irregular connective tissue that confluences with the dorsal and volar radioulnar ligaments.1
The ligaments and the triangular fibrocartilage form a three-walled structure that supports the distal radioulnar joint and ulnar portion of the carpus. The TFC, with its bordering volar and dorsal radioulnar ligaments, acts as the base of this structure. These ligaments originate as a unit from the fovea of the ulnar head and the very base of the ulnar styloid (Figure 5.3) and diverge distally into dorsal and volar stabilizers for the distal radius as it rotates around the distal ulna to achieve forearm rotation.2 The ulnotriquetral, ulnolunate, and ulnocapitate ligaments form the volar wall of this box, and the dorsal radial triquetral ligament (along with the dorsal fibers of the ECU subsheath) forms the dorsal wall.
The dorsal ECU subsheath has Sharpey fiber connections to the ulnar head at the fovea.2 The ulnar fibers of the ECU subsheath make up the ulnar-sided wall. The ulnotriquetral and ulnolunate ligaments along the volar wall of the TFCC have been shown to extend distally from the volar margin of the triangular fibrocartilage and the volar radioulnar ligament, rather than from the ulna itself.2,3 This confluence of many ligaments on the ulnar aspect of the wrist stabilizes the ulnar carpus to the triangular fibrocartilage as the radius rotates around the ulna.
The blood supply and innervation of the triangular fibrocartilage enters from the periphery.4,5 Thiru et al. evaluated the vascular perforators to the TFCC in a cadaveric study.6 The ulnar artery provides the blood supply to the ulnar portion of the TFCC through dorsal and palmar radiocarpal branches. This ulnar periphery of TFCC has the richest blood supply and the best potential for healing after repair. The dorsal and palmar branches of the anterior interosseous artery supply the more radial periphery and the attachment to the distal radius. The central portion of the TFCC is essentially avascular and is not amenable for repair. Similarly, the radial/central portion has been shown to have essentially no innervation.7 The majority of nerve supply to the TFCC is also peripheral, with contributions from the posterior interosseous nerve, the ulnar nerve, and the dorsal sensory branch of the ulnar nerve (DSBUN).
The volar and dorsal radioulnar ligaments are the primary stabilizers of the distal radioulnar joint (DRUJ) during rotation and translation at the DRUJ. As the forearm supinates from a position of full pronation, the volar radioulnar ligament is under stress and lengthens in a viscoelastic manner to accommodate.8,9 Pronation, from a position of full supination, causes the dorsal radioulnar ligament to be stressed and subsequently lengthen.8,9 A majority of the load from the carpus are directed to the radius (80%), whereas the remainder (20%) is directed to the ulna through the TFCC.10
There continues to be dispute among authors as to the advantages of either arthroscopic or open surgery for tears of the TFCC. Significant DRUJ instability has been demonstrated with complete release of the foveal attachments of the TFCC.11,12 In one study, the DRUJ instability was corrected with an open suture repair of the volar and dorsal radioulnar ligaments through bone tunnels to the fovea or an open version of the arthroscopic repair of the ulnar TFCC to the ECU subsheath.12 Biomechanical testing demonstrated significant improvements in the stability of the DRUJ for both groups. However, it was noted that the weakest aspect of each repair was not the type of repair but the bioabsorbable polydioxanone suture used.
Patient Presentation
Upon physical examination, acute TFCC injuries present with ulnar-sided wrist swelling. Point tenderness occurs when palpating the ulnar side of the wrist in the ballotable region between the ulnar styloid and the triquetrum. Forearm rotation with the wrist maintained in ulnar deviation may also elicit pain or a wrist click. The TFCC compression test is positive if axial loading of the ulnar side of the hand with ulnar deviation of the wrist results in significant pain. Similarly, de Araujo et al.13 described an ulnar impaction test that elicits pain by wrist hyperextension and ulnar deviation with axial compression. Although radiographs may not directly diagnose soft-tissue pathology in cases of suspected TFCC tears without carpal or distal radioulnar joint instability, indirect information can be obtained from the ulnar variance, the distal radioulnar joint congruency, and the presence or absence of a prior ulnar styloid or distal radius fracture.
Magnetic resonance imaging (MRI) with intra-articular gadolinium has become the imaging modality of choice for the diagnosis of soft-tissue injuries, and TFCC injuries are no exception (Figures 5.4 and 5.5). Although an MRI arthrogram may be both sensitive and specific in diagnosing a tear,14 at this point it has not been shown to be accurate in assessing tear size. In one study, Fulcher and Poehling felt that MRI understaged some TFCC pathology and overstaged others.15 Pederzini et al. performed arthrography, MRI, and arthroscopy on 11 patients with TFCC injuries.16 Although these authors found 100% specificities with sensitivities of 80 and 82% for arthrography and MRI (respectively), arthroscopic visualization of a TFCC tear continues to be the gold standard for definitive diagnosis.
Classification of TFCC Injuries
Anatomic, clinical, and biomechanical investigations have led to a classification of the triangular fibrocartilage complex injuries. Originally proposed by Palmer,17 this classification helps differentiate between traumatic and degenerative lesions. Repairable peripheral tears are generally classified as either type 1B or type 1C tears. Type 1B lesions are peripheral tears that occur as the ulnar side of the TFCC complex is avulsed from its capsule ulnar ligamentous attachments. These injuries are amenable to arthroscopic repair of the TFCC if there is no associated ulnar styloid fracture and no associated DRUJ instability. The type 1C injury involves rupture along the volar attachment of the TFCC or tears of the ulnocarpal ligaments. Type 1C tears may be amenable to repair if the ligamentous injury is vertically oriented. Arthroscopic repair of transverse or horizontally oriented tears of the ulnocarpal ligaments has not yet been described to our knowledge.
TFCC tears can be subdivided further by their time course from injury to treatment (Table 5.1).18 Tears are classified as acute when treated within three months from the time of injury. Arthroscopic repairs of acute tears can result in the recovery of up to 85% of the contralateral grip strength and range of motion.18 Acute injuries have a better prognosis than subacute injuries and chronic injuries.19 Subacute tears are treated from three months to one year after injury. Although subacute tears are still amenable to direct repair, in general they tend to regain less strength and range of motion than patients with repair of acute injuries.19 Chronic tears (more than one year) are repairable, but the results are inconsistent—presumably due to contraction of TFCC ligaments and degeneration of the torn fibrocartilage margins. Chronic injuries frequently require ulnar shortening osteotomy with or without TFCC debridement to decrease the load distributed to the ulna via the TFCC.
| Class 1: Traumatic |
Indications
Whereas repair of the peripheral triangular fibrocartilage attempts to recreate the original anatomy with direct suture of a rent in the fibrocartilage or its peripheral attachment, arthroscopic repairs involve imbrication of the peripheral-most aspect of the TFCC to the neighboring wrist capsule. This imbrication restores the tautness and trampoline effect of the TFCC and thus improves the stability of the TFCC as well as the patient’s symptoms, but does not precisely replicate the pre-injury anatomy. If DRUJ instability exists, only an open and direct reattachment of the foveal origin of the volar and dorsal radioulnar ligaments can reliably and completely restore stability.20 However, patients frequently present with acute or subacute peripheral TFCC tears in the setting of a stable DRUJ. These patients are amenable to arthroscopic repair.
The specific indications for arthroscopic repair of periphery tears of the TFCC continue to evolve. If clinical assessment and diagnostic studies suggest a TFCC tear, a wrist arthroscopy is warranted for adolescent or adult patients assuming a few key prerequisites (presented in Table 5.2). The type of peripheral tear also plays a role in the indications for repair. Horizontal, oblique, and vertical tears of the periphery of the TFCC can be addressed. However, distal transverse tears involving the volar ulnocarpal ligaments (within the type 1C category) are not amenable to arthroscopic repair at this point. More proximal split tears can be repaired and these ligaments can be imbricated to augment lunotriquetral instability, as has been demonstrated by Moskal et al.21
Table 5.2 Prerequisites for Arthroscopic Repair of Peripheral TFCC Tears
Contraindications
Contraindications to arthroscopic repair begin with DRUJ instability. If the DRUJ is unstable due to fracture or complete disruption of the distal radioulnar ligaments, fracture repair and open repair of the origin of the distal radioulnar ligaments should be considered. In chronic cases of symptomatic DRUJ instability, reconstruction of the ligamentous stabilizers of this joint is warranted. Similarly, in chronic Essex-Lopresti injuries and cases of interosseous instability TFCC repair is unlikely to alter the axial stability (or lack thereof) of the forearm.
An arthritic radiocarpal joint is certainly a reason to reconsider the outcome of an isolated arthroscopic TFCC repair. If the arthritis remains untreated, the return of the trampoline effect of the TFCC will unlikely change a patient’s entire wrist pathology. Last, cases of ulnar positive variance—where the ulna abuts the ulnar carpus with the TFCC sandwiched between—demand ulnar shortening osteotomy (either alone or in concert with arthroscopic TFCC repair).19 A final relative contraindication exists for cases in which the TFCC tear is irreducible, either due to its large size or contracture (Figure 5.6). TFCC tears that cannot be adequately reapproximated or reduced should undergo debridement to a smooth rim.
Surgical Technique
Arthroscopic Repair: Step-by-step Technique
In regard to this section, see Table 5.3. After a general anesthetic, the affected extremity is positioned on a hand table to allow full access to the hand, wrist, and elbow. Diagnosis commences with a physical exam of the radiocarpal joint and the distal radioulnar joint under anesthesia. In isolated peripheral tears of the TFCC, the examination under anesthesia may have no dramatic positive findings other than catching or grind with ulnar-sided compression and simultaneous forearm rotation. However, previously undiagnosed scapholunate or lunotriquetral instability can often be elicited in an anesthetized patient. A nonsterile upper arm tourniquet is placed with plenty of clearance for free elbow flexion after surgical prep and application of the impervious sterile drapes. The traction tower is assembled at this time, with 10 to 15 pounds of traction applied through finger traps on the index through small fingers. It is also possible to apply the finger traps to just the ulnar three digits for more pronounced traction on the ulnar side of the wrist, although this arrangement does make diagnostic arthroscopy of the radial side of the wrist more difficult.
Table 5.3 Preoperative Planning for Arthroscopic Repair of Peripheral TFCC Tears
| Anesthesia |
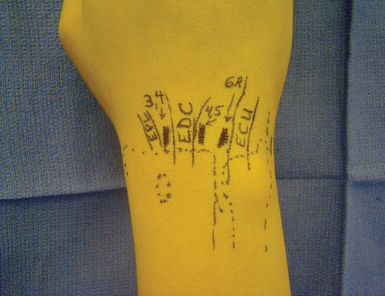
Next, the placement of the arthroscopic portals should be planned (Figure 5.7). Landmarks such as Lister’s tubercle, the DRUJ, the ulnar styloid, and the potential path of the dorsal sensory branch of the ulnar nerve are outlined. The 3-/,4 portal is placed between the extensor pollicis longus (EPL) tendon and the extensor digitorum communis (EDC) tendons, one centimeter distal to Lister’s tubercle between the scaphoid and the lunate. The 4-/,5 portal is positioned also 1 cm distal to Lister’s tubercle, but between the EDC and the EDQ tendons. If desired, a 6-R portal can be marked at the same axial level but just radial to the ECU. The point of outflow can also be designated at the 6-U position just ulnar or volar to the ECU tendon. Midcarpal portals should also be outlined, but will not be used specifically for the TFCC repair.
A #15 blade is used to create a 5- to 7-mm vertical skin incision at the planned location for the 3-/,4 portal. Blunt dissection with a fine hemostat (Jacobson) or a tenotomy scissors is carried down to the wrist capsule. The wrist capsule should be palpated and balloted with this instrument to ensure accurate placement of this radiocarpal portal in the proximal to distal axis. Once a soft spot in the capsule is confirmed, the tips of the fine hemostat or tenotomy scissors are gently driven into the radiocarpal joint, with the utmost care taken to avoid iatrogenic chondral injury. It is reasonable to check the traction across the wrist prior to entering the joint, as the initial level of traction often changes as the wrist is manipulated throughout the case. Once the joint has been entered, the tips of the instrument are spread to expand the size of the aperture to allow placement of the blunt arthroscopic trocar followed by the arthroscope itself. Most hand surgeons are comfortable with this technique, which relies on a knowledge of the anatomy, palpation of anatomic landmarks, and a tactile sense of the joint capsule.
Alternatively, a fluoroscopic-guided technique has been advocated and utilized by some wrist arthroscopists.22,23 Although this technique may seem burdensome at first, it can prevent iatrogenic chondral injury in a reliable fashion. A small or mini fluoroscopy unit is required, such as a XiScan (XiTec, East Windsor, CT). The fluoroscopy unit is positioned with the arm parallel rather than perpendicular to the floor. It is brought in directly from the end of the hand table at the height of the wrist joint. With a minimal adjustment, the fluoroscopy unit can be directed at the wrist joint in such a way that it avoids the vertical steel rod of the wrist arthroscopy tower. Under direct fluoroscopic control, 18-gauge needles can then be placed easily and atraumatically into the radiocarpal joint (marking the 3-/,4, 4-/,5 or 6-R, and 6-U portals). The small fluoroscopy unit is simply pulled from the field and the formal portals are made using the 18-gauge needles as guides to portal placement and direction.
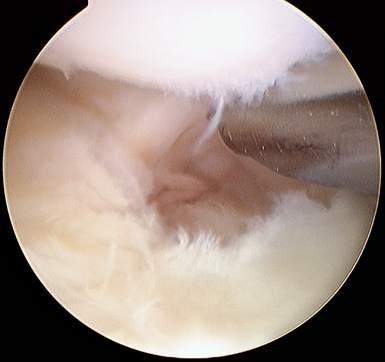
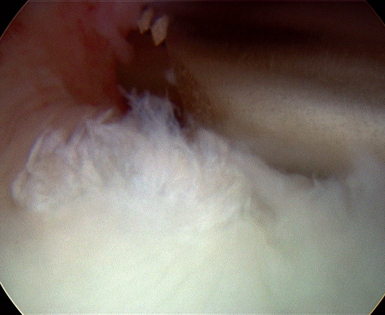
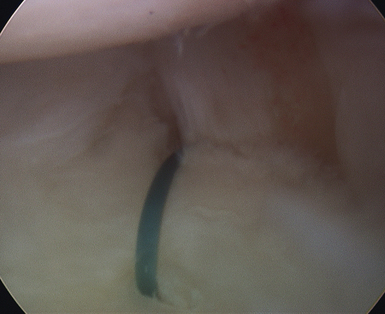
Using a small arthroscopic probe, the diagnosis of peripheral detachment is made by the trampoline test of the TFCC as described by Hermansdorfer and Kleinman.24 A normal TFCC is taut when indented with the probe, as shown in Figure 5.8. With release of indentation pressure the probe will be felt to “bounce” off the robust intact TFCC, similar to rebounding off a trampoline. If the TFCC is redundant or easily deformed when pressed by the arthroscopic probe, the diagnosis of a TFCC injury can be made. Careful arthroscopic inspection is required to differentiate radial-sided (type 1D), central (type 1A), and peripheral (ulnar type 1B or distal type 1C) lesions. One easy intra-articular landmark for TFCC tears is the ulnar head.
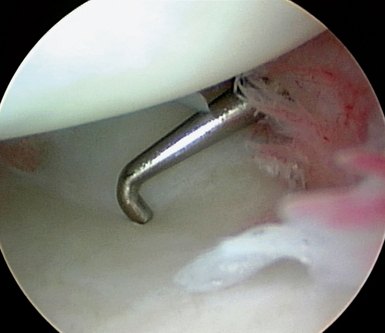
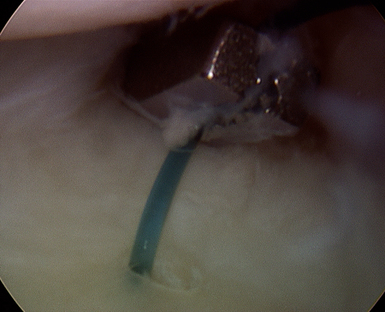
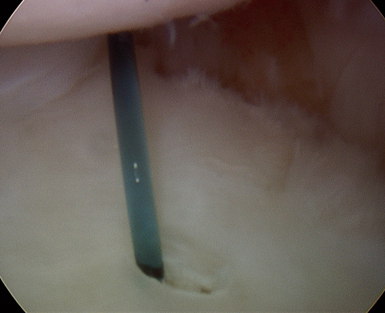
Once a peripheral lesion is identified, it must be debrided to clean edges. A full-radius 2.5-mm shaver is the ideal tool for this debridement, but occasionally a small biter may be necessary to debride larger flaps of torn or redundant tissue (Figures 5.9 and 5.10). An adequate debridement allows for complete assessment of the tear and provides a stimulus for a fibrin clot to form at the repair site. This fibrin clot will incite an appropriate repair response at the biological level. At this point, the size of the tear can be assessed with an arthroscopic probe (by knowing the length of the probe hook, one can measure the intra-articular extent of the TFCC tear). Tears greater than 5 mm in length will typically require at least two sutures to appropriately maintain the TFCC in a reduced position.
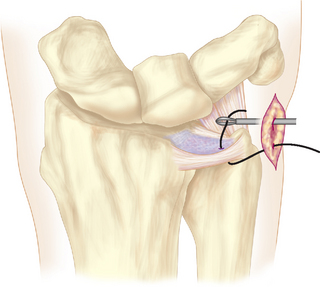
Our preferred repair method of ulnar-sided TFCC injuries is an outside-in technique. Prior to beginning the repair, the surgeon should decide if the repair suture will be horizontally or vertically oriented. A horizontal mattress-type suture is very effective in drawing a peripherally torn edge of the triangular fibrocartilage out toward the ulnar wrist capsule to reestablish the trampoline effect. Similarly, multiple vertically oriented sutures can be effective in coapting the edges of a peripheral tear. Either technique begins with puncturing the ulnar wrist capsule and TFCC using an 18-gauge needle after localization of the stitch with the finer 25-gauge needle to avoid iatrogenic trauma caused by multiple passes with the larger-bore needle. The needle should pass just inferior (for horizontal tears) or radial (for vertical tears) to the torn edge of the TFCC. The repair suture is then threaded into an 18-gauge needle and inserted into the wrist joint via the ulnar-sided 6-U incision under arthroscopic control (Figure 5.11).
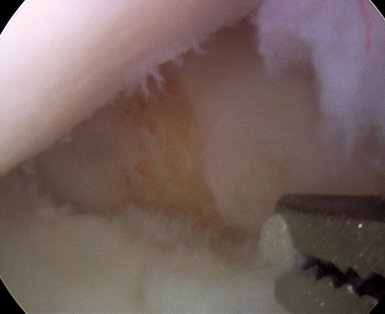
There are different suture retrieval techniques that work well. The intra-articular suture can be grasped using a small arthroscopic grasping forceps or wire suture grasper. With either instrument, a separate intra-articular puncture is required to retrieve the suture (Figures 5.12 and 5.13). The tissue bridge between the just-inserted suture grasper and the 18-gauge needle is the area over which the repair will be tied down. Although all of this work can be done through the small ulnar-sided incision, it is not necessary. The needles and suture must be passed such that the best possible repair is obtained.
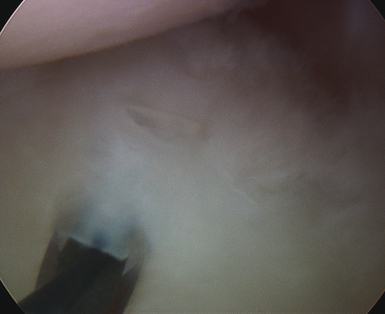
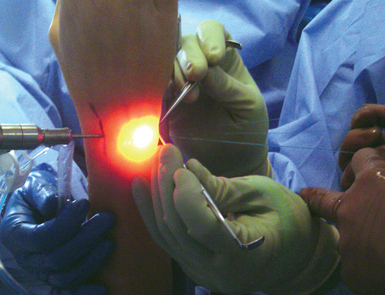
Frequently, one limb of the suture may need to be passed more dorsal (at the 6-R position, for example). In these circumstances, the overlying subcutaneous tissues can be undermined off the dorsal capsule—and with the DSBUN safely retracted, the sutures can still be retrieved into the ulnar-sided 6-U portal incision and tied under direct visualization. Certainly, when tying the repair sutures it is imperative that the DSBUN or an extensor tendon is not trapped under the tie. Tension is then placed on the sutures to ensure that there is reestablishment of TFCC tension and obliteration of any gapping between the articular disc and peripheral capsular tissue (Figure 5.14). In some cases, to establish a tension-free reduction of the torn edges the hand may be taken out of the traction device and the sutures tied with the wrist in slight ulnar deviation and forearm in neutral rotation. However, in a majority of cases the torn edges have not contracted and the suture can be tied with the wrist remaining in the traction tower (Figures 5.15 and 5.16). Two or three sutures are passed and tied using these techniques.
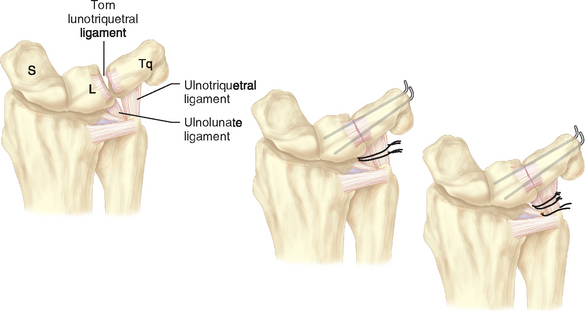
In cases of coincidental lunotriquetral ligament injury or longitudinal injury to the ulnolunate and lunotriquetral ligaments, the repair of these structures follows. Two 0.045-inch Kirschner wires can then be driven across the lunotriquetral articulation to stabilize the joint after reduction of the lunate using a percutaneously placed Kirschner wire (0.045 inch). The palmar ulnolunate and ulnotriquetral ligaments are then lassoed by sutures passed through the 6-U portal to augment the pinning of the lunotriquetral interval (Figure 5.17). Great care is to be taken to avoid inadvertent injury to the ulnar neurovascular bundle lying just volar to the ulnar wrist capsule and ulnocarpal ligaments. If necessary, the ulnar nerve and artery can be identified through the ulnar-sided 6-U incision and safely retracted. The sutures are tied over the capsule after the 6-U portal is enlarged, to bring all sutures out through this portal so that they can be tied under direct vision while protecting the dorsal sensory branch of the ulnar nerve. The pins are left in place for six weeks while the wrist is immobilized following the combined repair of the TFCC and the lunotriquetral ligament.
If there has been prior surgery involving the ulnar radiocarpal joint or DRUJ, scar tissue formation can make arthroscopy extremely difficult. With an open exposure of the TFCC using an approach between the fifth and sixth compartments (Figure 5.2), the same technique can be applied to repair peripheral tears of the TFCC. As previously mentioned, when clinically significant instability of the DRUJ exists open reattachment of the distal radioulnar ligaments to the ulnar fovea or open reconstruction should be considered.
Results
To evaluate the efficacy of arthroscopic repair of the TFCC, functional outcome was determined after arthroscopic repair of 22 wrists.25 Average follow-up was 36 months, with a range from 26 to 48 months. There was a significant relief of pain and increase in work and sports activities (p < 0.01). Postoperative range of motion averaged 86% +/− 9% of the contralateral side and grip strength averaged 82% +/− 20% of the contralateral side. There were significant correlations between the delay from injury to surgical repair and the final total range of motion and grip strength, with repairs of acute tears having better outcomes. Arthroscopic repair of peripheral TFCC tears results in significant relief of pain and increased function during work or sports.
1 Benjamin M, Evans EJ, Pemberton DJ. Histological studies on the triangular fibrocartilage complex of the wrist. J Anat. 1990;172:59-67.
2 Nakamura T, Takayama S, Horiuchi Y, Yabe Y. Origins and insertions of the triangular fibrocartilage complex: A histological study. J Hand Surg [Br]. 2001;26(5):446-454.
3 Nakamura T, Yabe Y. Histological anatomy of the triangular fibrocartilage complex of the human wrist. Ann Anat. 2000;182(6):567-572.
4 Chidgey LK, Dell PC, Bittar ES, Spanier SS. Histologic anatomy of the triangular fibrocartilage. J Hand Surg [Am]. 1991;16(6):1084-1100.
5 Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: Its clinical significance. J Hand Surg [Am]. 1991;16(6):1101-1105.
6 Thiru RG, Ferlic DC, Clayton ML, McClure DC. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg [Am]. 1986;11(2):258-263.
7 Gupta R, Nelson SD, Baker J, Jones NF, Meals RA. The innervation of the triangular fibrocartilage complex: Nitric acid maceration rediscovered. Plast Reconstr Surg. 2001;107(1):135-139.
8 DiTano O, Trumble TE, Tencer AF. Biomechanical function of the distal radioulnar and ulnocarpal wrist ligaments. J Hand Surg [Am]. 2003;28(4):622-627.
9 Nakamura T, Makita A. The proximal ligamentous component of the triangular fibrocartilage complex. J Hand Surg [Br]. 2000;25(5):479-486.
10 Trumble T, Glisson RR, Seaber AV, Urbaniak JR. Forearm force transmission after surgical treatment of distal radioulnar joint disorders. J Hand Surg [Am]. 1987;12(2):196-202.
11 Haugstvedt JR, Berger RA, Nakamura T, Neale P, Berglund L, An KN. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg [Am]. 2006;31(3):445-451.
12 Ruch DS, Anderson SR, Ritter MR. Biomechanical comparison of transosseous and capsular repair of peripheral triangular fibrocartilage tears. Arthroscopy. 2003;19(4):391-396.
13 de Araujo W, Poehling GG, Kuzma GR. New Tuohy needle technique for triangular fibrocartilage complex repair: Preliminary studies. Arthroscopy. 1996;12(6):699-703.
14 Zanetti M, Bram J, Hodler J. Triangular fibrocartilage and intercarpal ligaments of the wrist: Does MR arthrography improve standard MRI? J Magn Reson Imaging. 1997;7(3):590-594.
15 Fulcher SM, Poehling GG. The role of operative arthroscopy for the diagnosis and treatment of lesions about the distal ulna. Hand Clin. 1998;14(2):285-296.
16 Pederzini L, Luchetti R, Soragni O, Alfarano M, Montagna G, Cerofolini E, et al. Evaluation of the triangular fibrocartilage complex tears by arthroscopy, arthrography, and magnetic resonance imaging. Arthroscopy. 1992;8(2):191-197.
17 Palmer AK. Triangular fibrocartilage complex lesions: A classification. J Hand Surg [Am]. 1989;14(4):594-606.
18 Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: Management by early arthroscopic repairs. J Hand Surg. 1997;22A:57-65.
19 Trumble TE, Gilbert M, Vedder N. Ulnar shortening combined with arthroscopic repairs in the delayed management of triangular fibrocartilage complex tears. J Hand Surg [Am]. 1997;22(5):807-813.
20 Nakamura T, Nakao Y, Ikegami H, Sato K, Takayama S. Open repair of the ulnar disruption of the triangular fibrocartilage complex with double three-dimensional mattress suturing technique. Tech Hand Up Extrem Surg. 2004;8(2):116-123.
21 Moskal MJ, Savoie FHIII, Field LD. Arthroscopic capsulodesis of the lunotriquetral joint. Clin Sports Med. 2001;20(1):141-153. ix, x.
22 Slade JFIII, Geissler WB, Gutow AP, Merrell GA. Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. J Bone Joint Surg Am. 2003;85(4):20-32.
23 Slade JFIII, Dodds SD. Minimally invasive management of scaphoid nonunions. Clin Orthop Relat Res. 2006;445:108-119.
24 Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am. 1991;16(2):340-346.
25 Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy. 1996;12(5):588-597.