CHAPTER 33 Periareolar V-T Parachute Mastopexy
Key Points
Historical Background
The term ‘periareolar scar’ refers solely to the site of the scar, but omits any mention of the technique used on the neighboring tissue. This idea is not new, since already in 1952 Gillet1 described a ptosis correction technique involving implantation of nylon mesh around the nipple by suspending it from a narrow cloth band looped around the clavicle. But the author also states that it is difficult to perform a satisfactory cutaneous resection using this method and terminates with a Biesenberger T scar2 in cases where extensive cutaneous resection is required. A number of authors have also used this circular approach, which involves solely an intra- or periareolar incision without insertion of a foreign body. For example Andrews3 advocates an L-shaped resection in the lower outer quadrant secondary to complete dissection of the dermis. This cleavage, which reduces the vascular network of both the skin and breast tissue, explains why the resection in such cases is inevitably of limited scope. For mastopexy, Andrews dissects and plicates the lower extremity of the breast. Following resection of a small strip of skin around the initial intra-areolar incision, the incision is closed in such a way that the cutaneous envelope wraps itself back around the reshaped breast. However, this method is indicated solely in the presence of minor hypertrophy or ptosis and good skin elasticity, and follow-up of the results shown in the illustrations has been unduly brief (1, 2, and 3 months). Benelli4 de-epithelializes a far larger periareolar area, remodeling the adjacent region using glandular flaps, thus incurring a risk of devascularization if resection and dissection are unduly extensive. However, in such settings it is essential to achieve breast projection since periareolar techniques tend to diminish it (assuming of course that shaping the gland alone has a lasting effect). If this (or any other) periareolar technique is performed inadequately or on fatty breasts, a flattened, donut-like appearance is obtained. What should be performed instead is a periareolar circle using robust, non-resorbable sutures, since this is the only type of material that can conserve the incongruence between the two areolar circles and thus avoid excessive areolar enlargement. Felicio5 shifts the site of the resection to the periphery of the breast, with a view to conserving a central pedicle, and likewise uses non-resorbable sutures to maintain the size of the areola. This technique yields the most satisfactory result in younger patients whose skin exhibits good elasticity, and for resections amounting to an average of 300 g per breast (although exceptions to this rule are altogether possible). However, such procedures may be associated with unsatisfactory breast projection, suboptimal scar quality, and areolar enlargement, as well as a risk of areolar necrosis in cases where extensive and multiple resections are performed in the various quadrants.
Other authors have attempted to remedy the main shortcoming (i.e. deficient breast projection) by inserting a net between the skin and breast tissue with a view to creating and maintaining a conical shape. Bustos6 partially encircles the breast with silicone mesh, but only partially, so as to allow for expansion during pregnancy. However, Sampaio Goes7–9 has achieved the most impressive cosmetic and reconstructive surgery results in remodeling the breast following lumpectomy, via the most promising technique of all. This involves the use of resorbable netting, then taking maximum advantage of dermal spreading, and finally the deployment of partially resorbable netting.
The V-T Parachute Technique Principles
This technique aims to combine the advantages of the methods described above with a new approach to resection that is closely related to breast remodeling and avoids the use of a foreign body. Instead of interposing netting, I perform extensive de-epithelialization with a view to achieving the vascular efficiency afforded by the dermis and advocated by Lalardrie (this is also the most innovative feature of his dermal vault technique10).
Operative Technique
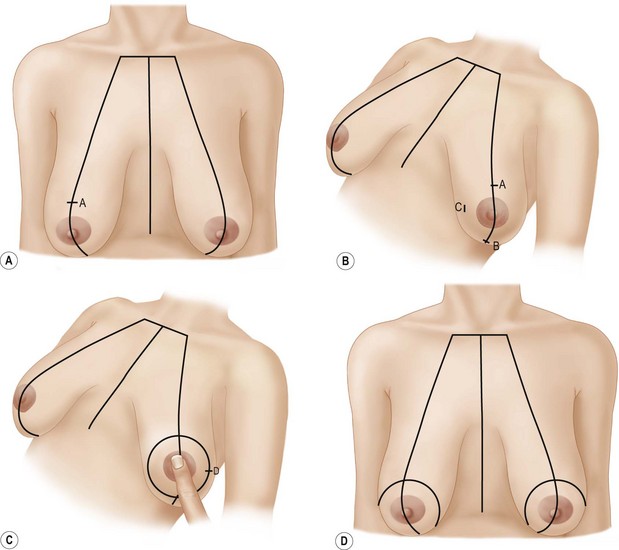
Markings
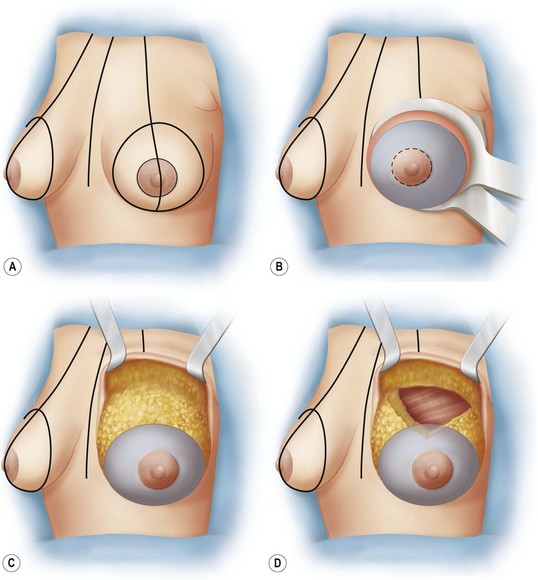
Surgical Procedure
The operation is performed under general anesthesia and with the patient in a sitting position with her arms hanging down at her sides (Fig. 33.2A). The final marking is realized by reducing the diameter of the areola to 4 cm. This line is marked using a 4 cm Dufourmentel ring while an assistant spreads the areolar region slightly. All skin between the two circles is de-epithelialized using a mammostat (Fig. 33.2B). The skin is then fully incised along the periphery of the de-epithelialized region and is dissected from the breast up to its periphery just under the subcutaneous plane at the level of the crests of Duret, as is done for a subcutaneous mastectomy (Fig. 33.2C). The breast mass should not be penetrated, nor should the dissection be more superficial than the fatty subcutaneous level. Pre-incision infiltration of cold saline containing a minute amount of adrenaline (no more than 1 mg per 500 ml of saline) will facilitate the skin dissection. Breast resection (when necessary) is performed in a V shape that straddles the upper quadrants, through the whole thickness of the breast tissue down to the perimysium of the pectoralis major (Fig. 33.2D). If the resection extends to slightly behind the de-epithelialized region, the breast dermis is dissected here as well in order to maintain the continuity of the dermal crown. The point of the V should not reach the lower edge of the pectoralis, or the nipple (taking account of the ptosis), so as to avoid injuring the pedicle (which arises at the fifth intercostal space together with the nipple nerve) and preserve nipple sensitivity. It is all the more important to proceed in this manner since the other option for preserving nipple–areola sensitivity arising in the dermal and subcutaneous network is interrupted by the peripheral cutaneous incision.
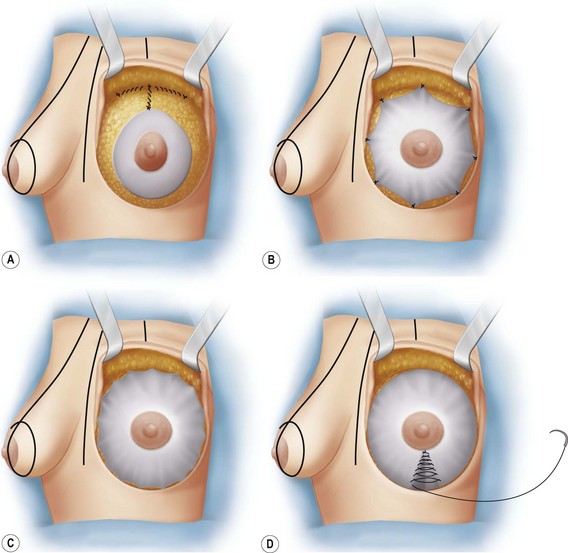
The breast is shaped by converting the V into a T, as follows: The central gap is filled and the nipple is raised by taking two symmetrical sutures on the lateral margins of the breast resection and anchoring these sutures to the same site as the pectoralis major muscle (Fig. 33.3A). In doing this, the distance between the suprasternal notch and nipple should be noted down so that the procedure can be replicated for the other breast. Five or six additional sutures are realized to reinforce the fixation of the horizontal element of the T at the muscular level.
The dermis is then spread as far as possible across the surface of the breast and is fixed to the entire periphery of the breast via eight tacking sutures (Fig. 33.3B) and one continuous suture using a long-term resorbable suture (Fig. 33.3C). As much of the dermis as possible should be sutured to the muscular wall and not to the breast itself, although this of course depends on the size of the de-epithelialized region. If the entirety of the dermis can be sutured to the wall (as is the case with tuberous breasts) at the periphery of the breast, a parachute-like form is obtained – hence the name of the technique. This spreading can be completed by performing a dermal tuck in the lower segment of the breast (Fig. 33.3D), which also enhances breast projection.
Hemostasis is then checked and a suction drain is inserted in the subcutaneous space.
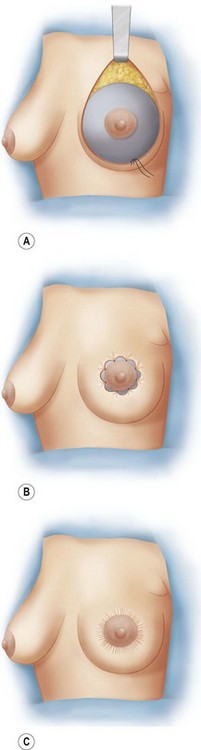
In performing the skin closure, the difference in size between the two areolae is corrected. It is essential that non-resorbable sutures be used here so as to avoid undue postoperative areolar enlargement. I originally performed the suturing as follows: a continuous suture using Gore-Tex® 4-0 suture material and a straight needle was realized in the peripheral dermis 2 or 3 mm beyond the incision (Fig. 33.4A). After eight interrupted sutures are taken in order to distribute the excess skin evenly (Fig. 33.4B), the purse is gathered (Fig. 33.4C). However, I have since modified the technique in such a way that I perform a star-shaped suture by radiating the Gore-Tex suture out from one circle to the other and of course spreading the excess skin evenly across the breast with the aid of the eight markings on the areola and the peripheral dermis. I then gather and close the incision via a continuous superficial intradermal suture using resorbable suture material (Biosyn 4 or 5-0).
Indications
Breast Reduction
The V-T parachute technique only yields good breast reduction results in the presence of moderate hypertrophy (resection of 400 g or less), good skin quality, and a normal or straight breast base (see Fig. 33.4).
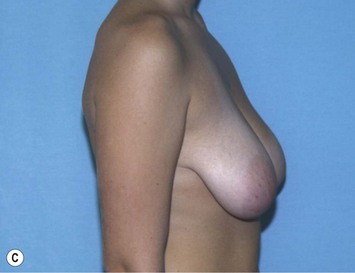
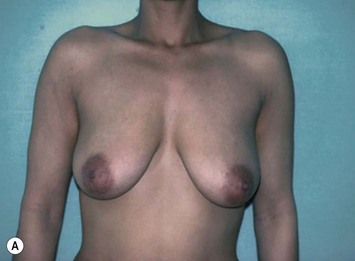
Ptosis
The indication for ptosis is based on the same preoperative criteria as those indicated above, namely the presence of normal or straight breast bases and conical breasts with a low areola (Fig. 33.6).
Asymmetry
In cases of asymmetry where one breast is regarded as normal or requires augmentation (Fig. 33.7), the V-T parachute technique is preferable to the inverted T since the scar is less obtrusive by virtue of its being unilateral. Often in such cases, the technique is performed only partially via a limited resection or without any resection at all; or the skin is not spread all the way across the breast.
Tuberous Breasts
Tuberous breasts are an exceedingly good (and probably the optimal) indication for the V-T parachute technique since these patients meet all of the criteria for a satisfactory outcome, namely a straight breast base, excessive areolar projection and good quality skin (see Fig. 33.8).
Pitfalls and How to Correct
1 Gillet G. Suspension mammaire par prothèse sous-cutanée. Presse Med. 1952;60(62):1325-1326.
2 Gillies H, McIndoe AH. The technique of mammaplasty in conditions of hypertrophy of the breast. Surg Gynec Obstet. 1939;68:658-665.
3 Andrews JM, Yshizuki MA, Martins D, Ramos R. An areolar approach to reduction mammaplasty. Br J Plast Surg. 1975;28:166-170.
4 Benelli L. Technique personnelle de plastie mammaire péri-aréolaire: le ‘round-block.’. Cah Chir. 1991;1(77):15-25.
5 Felicio Y. Periareolar reduction mammaplasty. Plast Reconstr Surg. 1991;88(5):789-799.
6 Bustos RA. Periareolar mammaplasty with silicone supporting lamina. Plast Reconstr Surg. 1992;89(4):646-657.
7 Sampaio Goes JC. Periareolar mammoplasty, double-skin technique. Glande Dis. 1991;4:111-127.
8 Sampaio Goes JC. Periareolar mammaplasty: double-skin technique with application of polyglactine 910 mesh. Rev Soc Bras Cir Plast. 1992;7(1–3):1-9.
9 Sampaio Goes JC. Periareolar mammaplasty: double-skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996;97(5):959-968.
10 Lalardrie JP, Mitz V. Plastie mammaire de réduction par la technique de la voûte dermique. J Chir. 1974;108:57-68.