Chapter 20 Percutaneous Sacroplasty
Sacral insufficiency fractures, which are commonly associated with osteoporosis, rheumatoid arthritis, and radiation therapy–related cancer bony metastasis, can be treated with percutaneous sacroplasty under fluoroscopic and CT guidance; procedure is the same in the vertebrae as in the sacrum [1]. Pain caused by sacral insufficiency fractures can be relieved immediately with percutaneous sacroplasty, and patients can be allowed to ambulate immediately after the procedure.
The possible mechanisms for the pain relief experienced after sacroplasty are as follows:
 Stabilization and fixation of the sacral fracture site, which achieves mechanical augmentation and stabilization
Stabilization and fixation of the sacral fracture site, which achieves mechanical augmentation and stabilizationIndications
Procedure
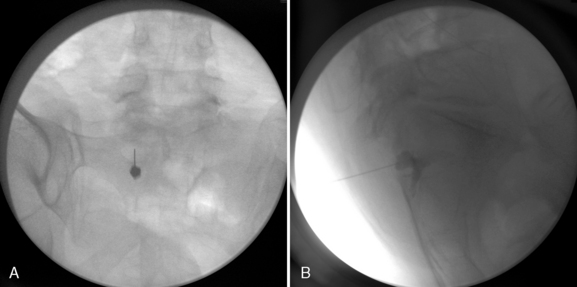
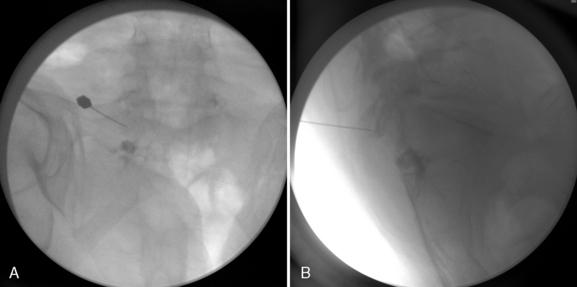
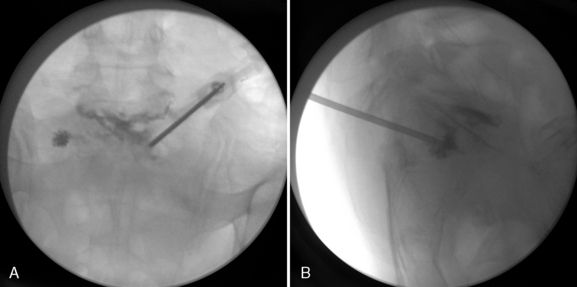
Figure 20–1 (A) Placement of block needle on the left S1 foramen. (B) Injection of contrast medium under fluoroscopy.
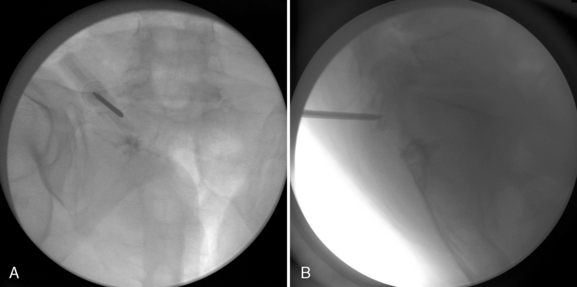
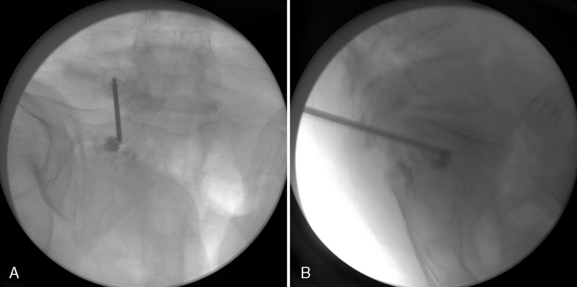
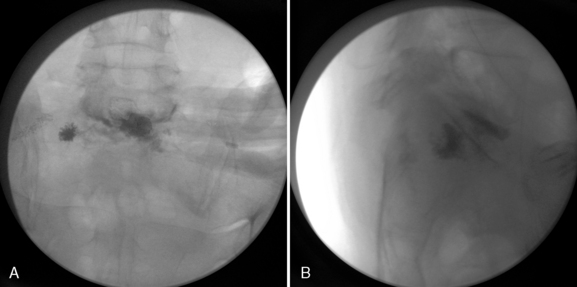
Figure 20–3 Insertion of an 11-gauge, 10-cm vertebral needle to the pre-anesthetized targeted periosteum as Fig. 20-2 and identified on AP fluoroscopic view (A) and lateral view (B).
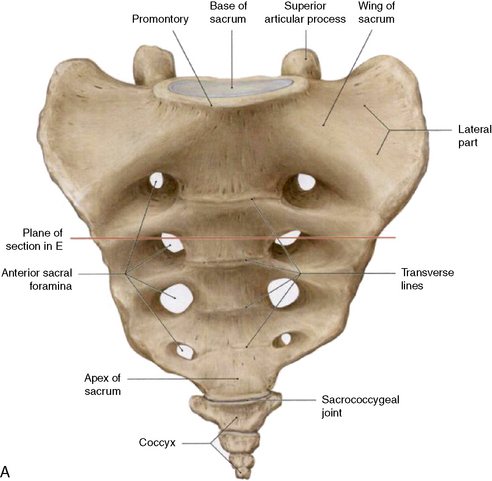
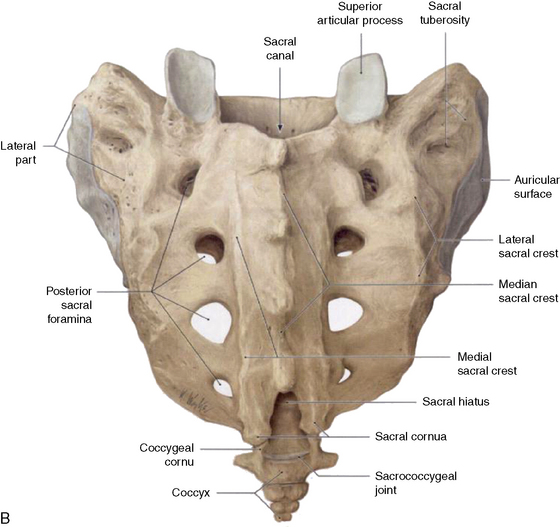
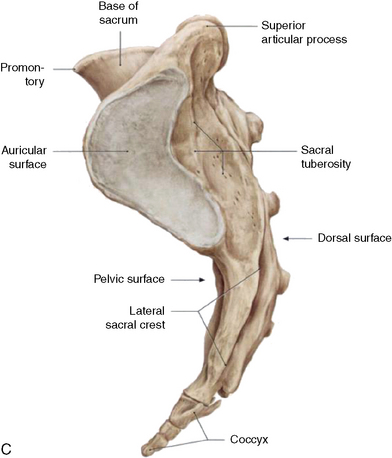
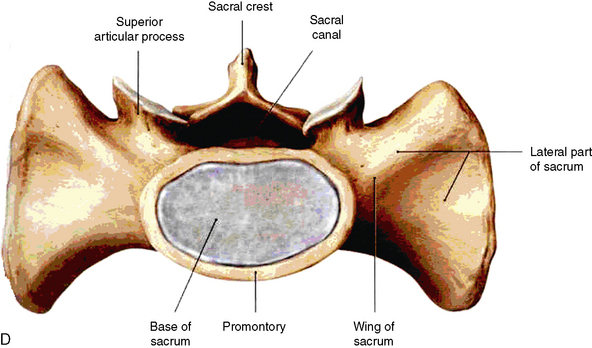
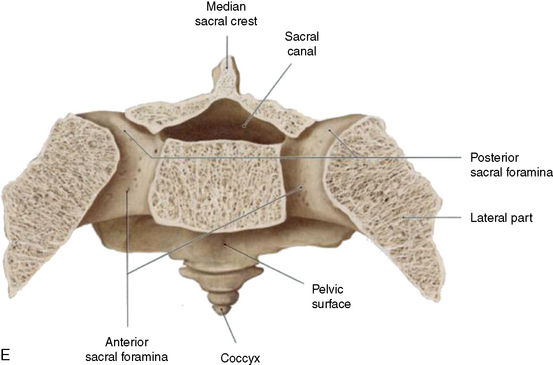
Related anatomy and physiology
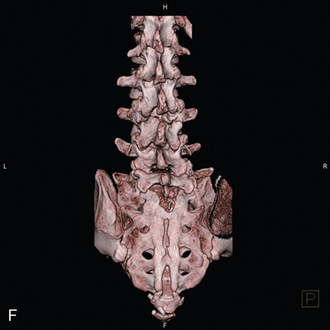
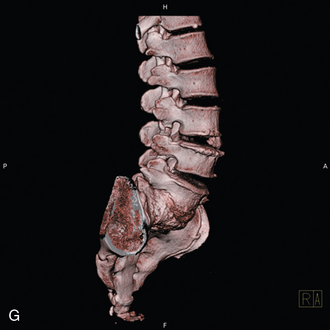
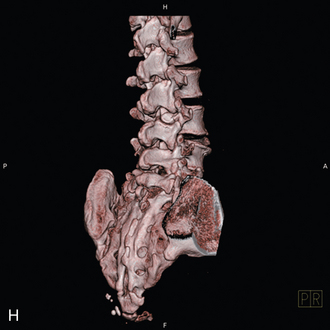
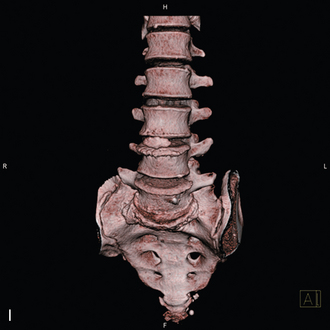
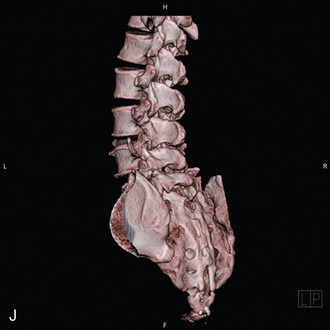
Figure 20-9 illustrates the anatomy and physiology related to sacroplasty.
Caveat
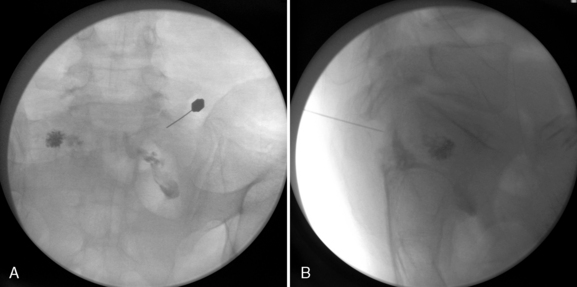
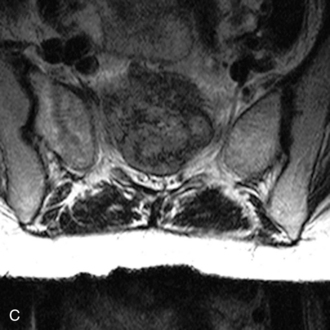
CASE STUDY 20.1
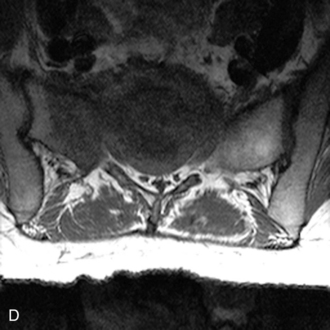
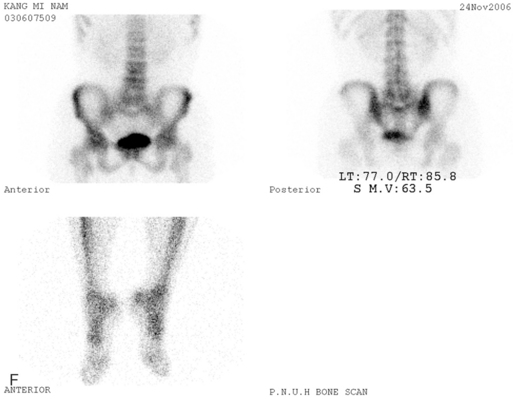
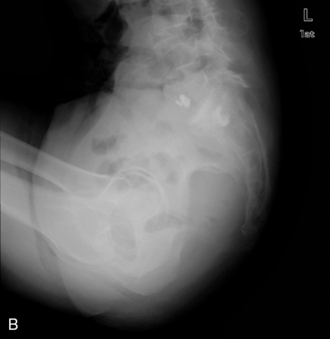
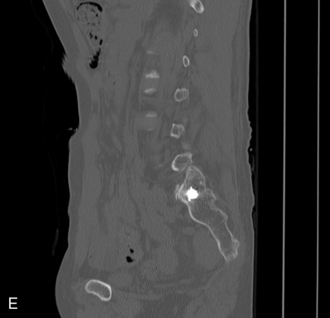
A 38-year-old woman with breast cancer was suffering from intractable low back pain, especially in weight-bearing positions. There were tumor infiltrations on the L5 vertebra and both sacral alae of the S1 and S2 vertebrae as seen in preoperative magnetic resonance imaging and bone scan (Fig. 20-10). It was determined that sacroplasty would be performed and there was no cement leakage into the L5-S1 intervertebral space during the procedure (Fig. 20-11). Two hours after completion of the sacroplasty, the patient experienced pain relief when standing and sitting, and was discharged.