Chapter 23 Percutaneous Endoscopic Cervical Discectomy and Stabilization
Percutaneous endoscopic cervical discectomy (PECD) is a relatively new surgical method for treating soft cervical disc herniations [1–7]. The goal of the procedure is decompression of the spinal nerve root by percutaneous removal of the herniated mass under local anesthesia. A holmium:yttrium-aluminum-garnet (Ho:YAG) laser is generally used to ablate and shrink the herniated disc [1–7].
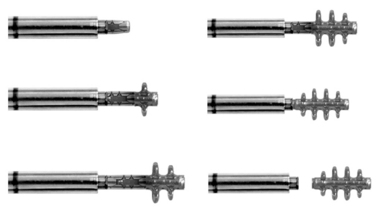
The WSH cervical endoscopy set (Karl Storz, Tuttlingen, Germany) consists of a high-resolution endoscope, illumination, and two irrigation channels [7]. The working channel allows passage of a side-firing Ho:YAG laser and microforceps. The excellent visualization via the endoscope permits the surgeon to selectively remove a portion of the herniated nucleus pulposus. After the anular anchorage has been loosened by the side-firing laser, the herniated fragment can be removed easily with the microforceps. With circumferential rotation of the working cannula and the endoscope, the side-firing laser can also ablate the thickened ligamentum flavum, remnant bone fragment, and shoulder osteophyte.
The major advantages of PECD and PECD stabilization (PECDS) with the B-Twin spacer are as follows [8–12]:
 Minimal insult to anterior anulus, anterior longitudinal ligament, longus colli muscle, and anterior vertebral body
Minimal insult to anterior anulus, anterior longitudinal ligament, longus colli muscle, and anterior vertebral bodyIndications and contraindications
The indication for PECD or PECDS (Box 23.1) is a soft cervical disc herniation that shows no response to conservative treatment for 6 weeks.
Preoperative preparation
The primary patient complaint is cervical radiculopathy or neck pain.
Imaging diagnosis consists of the following modalities and findings:
Instrumentation
Equipment
The following instruments and modalities are required in the operating room for PECD/PECDS:
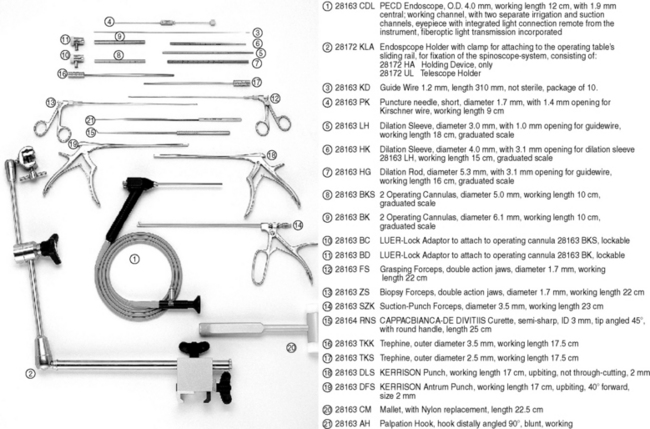
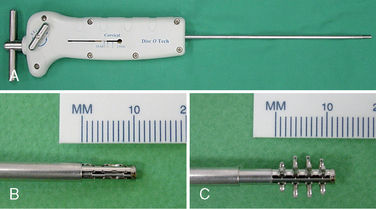
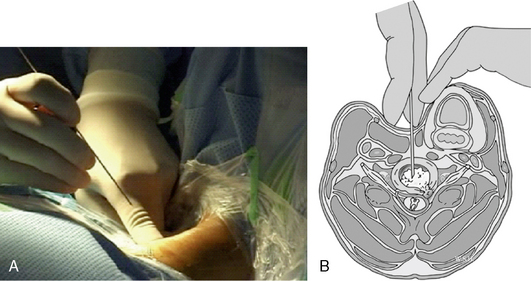
Figure 23–1 A set of percutaneous endoscopic cervical discectomy (PECD) instruments. (Karl Storz, Germany)
Anesthesia and Other Medications
 To decrease the risk of infection, preoperative antibiotics (usually 1.0 g of cefazolin) should be given the day before operation. Preoperative sedatives are recommended.
To decrease the risk of infection, preoperative antibiotics (usually 1.0 g of cefazolin) should be given the day before operation. Preoperative sedatives are recommended.Procedure
Discectomy
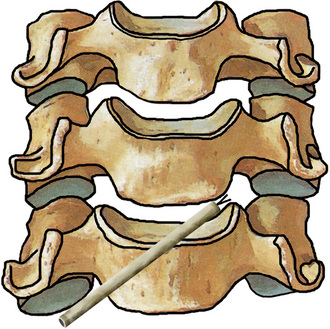
The foraminal cervical disc herniation is better approached from the opposite side—that is, for a left foraminal herniation, a right-sided skin entry is more suitable, and vice versa (Fig. 23-6). The midline herniation can be better approached from the right side by a right-handed surgeon, and from the left side by a left-handed surgeon.
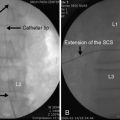
 In the anteroposterior fluoroscopic view, the tip of the cannula should lie in the midline for a midline disc herniation, and the cannula tip should be facing the affected foramen for a foraminal disc herniation.
In the anteroposterior fluoroscopic view, the tip of the cannula should lie in the midline for a midline disc herniation, and the cannula tip should be facing the affected foramen for a foraminal disc herniation.Percutaneous Cervical Stabilization Using the Cervical B-Twin Expandable Holder
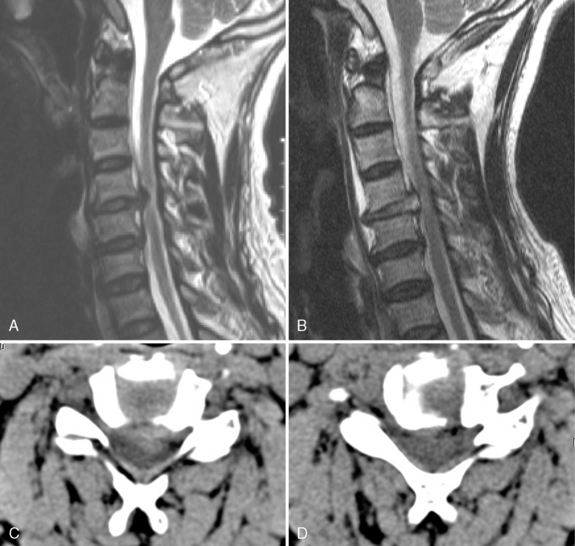
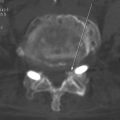
Figure 23–16 Case Study 23.1: (A) Preoperative sagittal magnetic resonance (MR) image shows noncontained disc herniation at C4-C5. (B) Sagittal MR image obtained 5 weeks after the procedure showed no instability. (C) Preoperative axial computed tomography (CT) demonstrates soft disc herniation. (D) Postoperative axial CT scan demonstrates complete removal of the disc herniation.
Postprocedural management
 The patient is observed for 3 hours and permitted to go home within 24 hours unless there is a complication. The patient does not need bed rest for more than 1 night.
The patient is observed for 3 hours and permitted to go home within 24 hours unless there is a complication. The patient does not need bed rest for more than 1 night. Mild physical therapy may be helpful for fast recovery within 2 weeks postoperatively if cervicobrachialgia does not disappear completely.
Mild physical therapy may be helpful for fast recovery within 2 weeks postoperatively if cervicobrachialgia does not disappear completely. If pain and discomfort remain, complementary epidural injection of steroids with lidocaine may be performed so that no further open procedure is necessary. The logic is to complement the therapeutic approaches of mechanical decompression and PECD with the reduction of inflammatory components by steroids.
If pain and discomfort remain, complementary epidural injection of steroids with lidocaine may be performed so that no further open procedure is necessary. The logic is to complement the therapeutic approaches of mechanical decompression and PECD with the reduction of inflammatory components by steroids. Rehabilitation exercises for neck muscle strengthening and improvement of range of motion are recommended twice a week for 3 months after 4 to 6 weeks postoperatively.
Rehabilitation exercises for neck muscle strengthening and improvement of range of motion are recommended twice a week for 3 months after 4 to 6 weeks postoperatively.CASE STUDY 23.1
A 61-year-old man suffered from cervical myelopathy. Preoperative magnetic resonance imaging showed noncontained disc herniation at the C4-C5 level, and computed tomography demonstrated soft disc herniation. Because the patient was concerned about the risks of general anesthesia, he underwent percutaneous endoscopic cervical discectomy. Five weeks after the procedure, magnetic resonance imaging showed no instability, and computed tomography demonstrated complete removal of the disc herniation (Fig. 23-16).
CASE STUDY 23.2
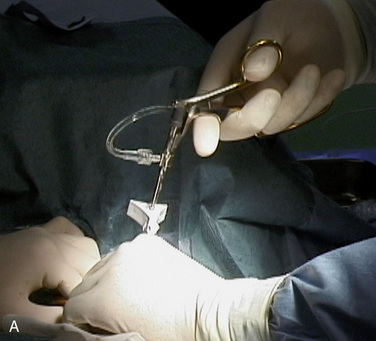
A 43-year-old man with C5-C6 instability suffered from neck pain and right shoulder pain. Preoperative magnetic resonance imaging showed C5-C6 instability with disc herniation, and computed tomography confirmed soft disc herniation. Percutaneous endoscopic cervical discectomy and stabilization were performed and immediate stability was obtained (Fig. 23-17)
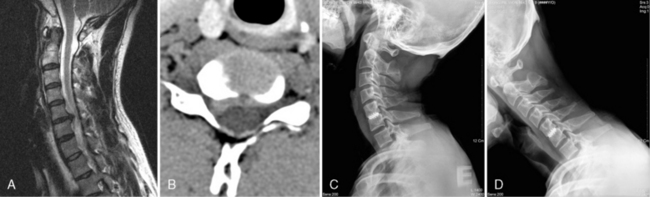
Figure 23–17 Case Study 23.2: (A) Preoperative magnetic resonance image shows C5-C6 instability with disc herniation. (B) Preoperative computed tomography scan demonstrates soft disc herniation at right side. Postoperative lateral radiographs in extension (C) and flexion views (D) show proper position of cage and immediate stability.
Caveats
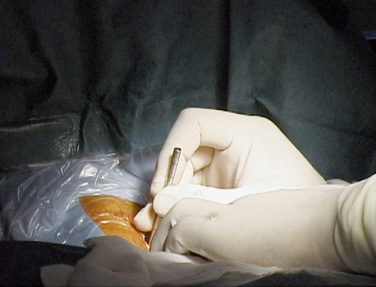
 The surgical anatomy of the neck is quite suitable for an anterior percutaneous approach. Because the prevertebral content is very mobile owing to compartmentalization of the neck by the deep fascia, the visceral axis (thyroid, trachea, pharynx, larynx, and esophagus) can easily be displaced to the opposite side with one or two fingers.
The surgical anatomy of the neck is quite suitable for an anterior percutaneous approach. Because the prevertebral content is very mobile owing to compartmentalization of the neck by the deep fascia, the visceral axis (thyroid, trachea, pharynx, larynx, and esophagus) can easily be displaced to the opposite side with one or two fingers. The surgeon should recognize and manually feel the pulsation of the carotid artery so as to insert the needle and cannula away from the carotid artery. The surgeon should confirm the position of a needle or a cannula on the anteroposterior fluoroscopic view to prevent penetration of the vertebral artery. The fingertips of the operator or the assistant should touch the anterior surface of the vertebral body to avoid perforating the trachea or esophagus.
The surgeon should recognize and manually feel the pulsation of the carotid artery so as to insert the needle and cannula away from the carotid artery. The surgeon should confirm the position of a needle or a cannula on the anteroposterior fluoroscopic view to prevent penetration of the vertebral artery. The fingertips of the operator or the assistant should touch the anterior surface of the vertebral body to avoid perforating the trachea or esophagus.1. Lee SH, Gastambide D. Perkutane endoskopische diskotomie der halswirbelsaule. In: Pfeil J, Siebert W, Janousek A, et al, editors. Minimal-Invasive Verfahren in Der Orthopadie und Traumatologie. New York: Springer; 2000:41-61.
2. Chiu JC, Clifford TJ, Greenspan M, et al. Percutaneous microdecompressive endoscopic cervical discectomy with laser thermodiskoplasty. Mt Sinai J Med. 2000;67:278-282.
3. Lee SH. Percutaneous cervical discectomy with forceps and endoscopic Ho:YAG laser. In: Gerber BE, Knight M, Siebert WE, editors. Lasers in the Musculoskeletal System. New York: Springer; 2001:292-302.
4. Lee SH, Kim SK, Lee SC, et al. Long-term clinical outcomes of percutaneous endoscopic cervical discectomy with Ho-YAG laser. J Korean Soc Laser Med Surg. 2003;7:31-38.
5. Ahn Y, Lee SH, Lee SC, et al. Factors predicting excellent outcome of percutaneous cervical discectomy: Analysis of 111 consecutive cases. Neuroradiology. 2004;46:378-384.
6. Ahn Y, Lee SH, Chung SE, et al. Percutaneous endoscopic cervical discectomy for discogenic cervical headache due to soft disc herniation. Neuroradiology. 2005;25:924-930.
7. Ahn Y, Lee SH, Shin SW. Percutaneous endoscopic cervical discectomy: Clinical outcome and radiographic changes. Photomed Laser Surg. 2005;23:362-368.
8. Ahn Y, Lee SH. Percutaneous endoscopic cervical fusion with expandable holder: Case report of initial technique. J Minim Invasive Spinal Tech. 2002;2:8-9.
9. Lee SH, Choi BK, Choi S. Update on percutaneous cervical stabilization. J Minim Invasive Tech. 2004;4:22-23.
10. Lee SH, Ahn Y. Percutaneous endoscopic cervical diskectomy and stabilization. In: Kim D, Fessler R, Regan J, editors. Endoscopic Spine Surgery and Instrumentation. New York: Thieme; 2005:59-65.
11. Lee SH, Choi BK, Choi WC, Choi SM. Percutaneous cervical stabilization. In: Savitz MH, Chiu JC, Rauschning W, et al, editors. The Practice of Minimally Invasive Spinal Technique. 2005 ed. New City, NY: AAMISS Press; 2005:540-542.
12. Choi WC, Lee SH, Ahn Y, et al. Percutaneous cervical stabilization using the WSH cervical B-Twin. Joint Dis Relat Surg. 2005;16:82-87.