10 Percutaneous Coronary Interventions of Chronic Total Occlusions
PCI Strategy
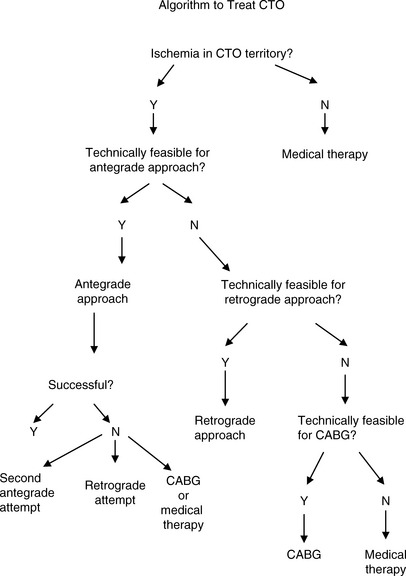
Prior to intervention, a formal strategy (“game plan”) should be devised (Fig. 10-1). By developing a game plan, overextending an already difficult procedure and increasing the risk of complications may be minimized. This plan must start with a decision as to whether the CTO is producing symptoms and/or ischemia, and if so, whether revascularization is actually required (as opposed to medical therapy). If revascularization is chosen, it must be decided whether the patient would be better served with CABG or PCI, as CTOs typically occur in patients with multivessel disease. If PCI is chosen, the next decision is whether the complexity is within the operator’s technical expertise or should be referred to a CTO super-specialist.
Favorable characteristics for the antegrade approach are shown in Figure 10-2 and listed in Table 10-1. Any combination of unfavorable characteristics significantly decreases the chance of success.
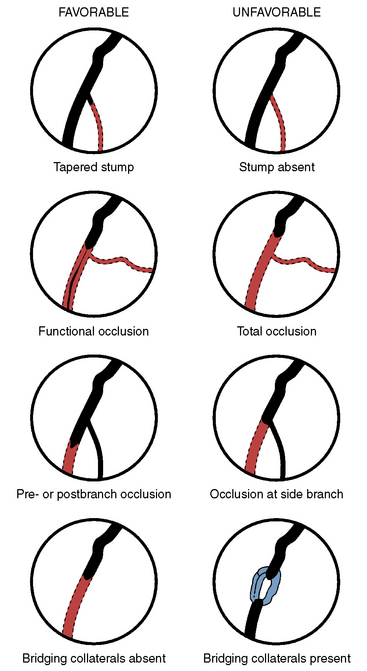
Figure 10-2 Morphology of total coronary occlusion: favorable and unfavorable morphology for procedural success.
(Modified from Safian RD, Freed M, Grines C, eds. The manual of interventional cardiology, 3 rd ed. Birmingham, MI: Physicians’ Press, 2001, p. 295.)
Table 10-1 Favorable and Unfavorable Characteristics for Antegrade Success for Chronic Total Occlusions
| Favorable |
Technical Considerations for CTO PCI
Angiography
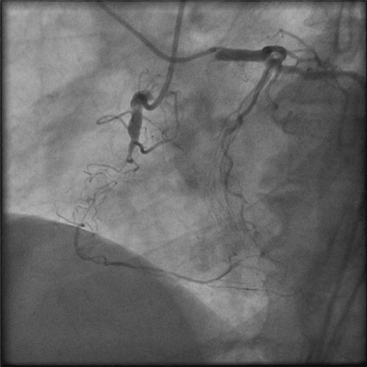
Excellent vessel opacification and knowledge of the occluded segment length and course are important factors for PCI success. Visualization of retrograde collateral filling of the target vessel is often essential. Bilateral coronary angiography is an invaluable aid in many CTO cases (Fig. 10-3). Using the antegrade approach, opacification through the target vessel may be insufficient to visualize the CTO and the course of the potentially recanalized channel. The contralateral vessel injection may allow for visualization of the vessel segment distal to the CTO. Administration of intravenous nitroglycerin may further improve visualization.
Antegrade Approach
Guide and Support Catheters
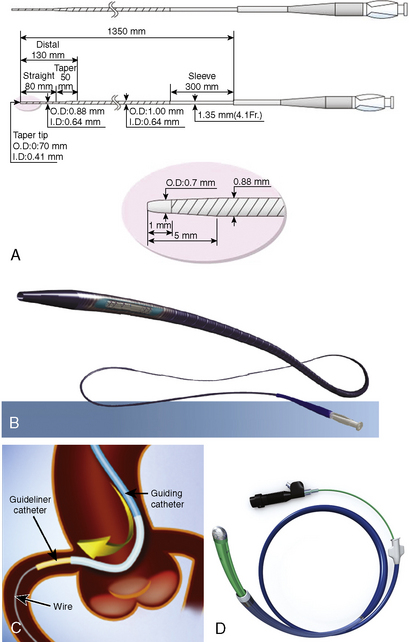
A guide catheter with good backup is extremely important. The diameter of the guide remains an operator choice. In general, the greater the backup required and the amount of hardware to be introduced into the vessel, the larger should be the catheter diameter. Although stand-alone guidewire passage across a CTO may be effective, support for wire passage is usually required. Support for guidewire passage can be obtained with end-hole microcatheter, e.g., Corsair (Fig. 10-5B) or small-diameter (1.25–1.5 mm) over-the-wire (OTW) balloon catheter and will increase the chance for wire passage through the total obstruction. Wire passage through a CTO into the true lumen increases the success rate to nearly that of a non-CTO, that is, > 90%–95%. Although passage of the wire distally through the true lumen is another major key for success, subintimal wire passage can still be effective.
CTO Guidewires
Wire choice is another key element to treatment success. There is a very large portfolio of available wires. In general, guidewires may be classified as hydrophilic and non-hydrophilic; Table 10-2 lists a few examples of each. Each wire has its own unique combination of flexibility, trackability, torque transmission (or steerability), lubricity (or hydrophilicity), shaft support, wire tip load or strength, wire tip prolapsibility, radiovisibility, ability to shape and retain tip configuration, tip taper and thickness, and tactile feedback. The operator should become familiar with the properties of each wire that might be applied to a lesion so that a wire plan can be developed.
Table 10-2 Examples of Equipment for Recanalization of Chronic Total Occlusion Using the Antegrade Approach
| Category | Example | Rationale for Use |
|---|---|---|
| Guiding catheter | Left: Amplatz, XB (Cordis), EBU (Medtronic), Voda (BSC) Right: Amplatz |
Increased backup support |
| Guidewires | Hydrophilic wires: Fielder, Fielder XT (Asahi), Pilot 50 (Abbott) | Passage through microchannel |
| Increased tip load: Miracle Bros 3-12 (Asahi), Confianza Pro (Asahi) | Passage through “hard” proximal cap | |
| OTW balloon | 1.25–1.5 balloon diameter (multiple companies) | Increase wire force to proximal capPredilation after crossing CTO |
| Microcatheter | Corsair (Asahi), FineCross (Terumo, Tokyo, Japan) | Provide increased wire force to proximal cap |
| Tornus | Enlarge lumen when balloon cannot pass lesion | |
| Guide extender | GuideLiner (Vascular Solutions) | Increase backup support in tortuous, calcific, or difficult to CROSS lesions and vessels |
| Rotational atherectomy | Rotablator (Boston Scientific Corp.) | Enlarge lumen in undilatable lesion |
Treatment After Wire Passage
Usually a balloon catheter can cross a CTO after wire passage. Balloon dilatation can then prepare the vessel for stenting. Occasionally a balloon cannot cross or, even rarer, the balloon crosses but the lesion is undilatable. When a balloon catheter cannot cross a lesion, a particularly useful device is the Tornus (Asahi Intec, Tokyo, JP; Fig. 10-5A), which acts somewhat like a screw to enlarge the channel. If that maneuver is ineffective, or if the amount of calcification is large, consideration of rotational atherectomy should be given if a Rotablator wire can pass through the total occlusion. The operator is sometimes faced with the decision of removing a non-Rotablator wire for a Rotablator wire; this may be necessary but the operator should appreciate that the life line, that is, the previously passed guidewire, has been lost during this interval.
Selected Devices and Techniques to Recanalize the CTO
Double (or Triple Wire) Parallel Wire Technique
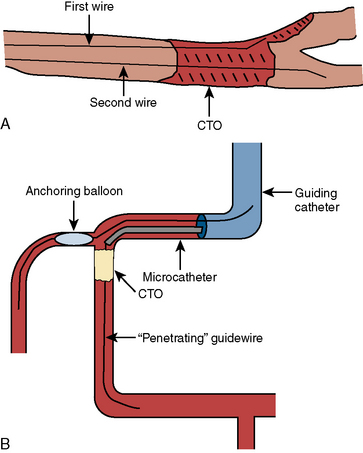
It is common that a guidewire passes subintimally during an attempted CTO crossing. One approach is to maintain the wire in place and use a second wire with an OTW balloon catheter to attempt to traverse the true lumen using the first wire as a marker of the subintimal space (Fig. 10-4A). A variant of this technique, known as the see-saw technique, utilizes an OTW catheter for wires, manipulating one wire and then the other, alternating their position between dissection plane and true lumen until one wire is able to cross the CTO intraluminally.
Anchoring Technique
In some lesions where the proximal cap is hard, advancing the guidewire pushes the guide catheter out of the vessel (even with an excellent backup guide). A technique known as anchoring may be applied (Fig. 10-4B). A small angioplasty balloon is passed to a side branch proximal to the CTO and the balloon inflated. This maneuver will anchor the guide catheter in the coronary ostium. The force along the guidewire will be transmitted more effectively to the CTO and thus increases the chance of puncturing the cap or creating a subintimal wire dissection. The balloon may also be inflated proximal to the CTO, which will allow increased force transmission by the wire.
Mother-Child or Guide-in-Guide Approach
The mother-child technique utilizes one small-diameter guide catheter within a larger guide with passage of the smaller guide into the coronary near the occlusion. There is also a commercially available guide extender, the GuideLiner (Vascular Solutions), which may accomplish the same purpose (Fig. 10-5C). This technique allows for more efficient force transmission of the wire through the microcatheter or the OTW balloon catheter to the proximal CTO end, increasing the chance of puncturing the proximal cap.
Other Devices
The Crosser (FlowCardia, Sunnyvale, CA) is a mechanically driven catheter that uses vibrational energy to aid in crossing the CTO (Fig. 10-5D). The CrossBoss (Bridgepoint Medical, Plymouth, MN), a manually applied catheter with a slightly bulbous tip, has been utilized to cross a CTO intraluminally. It may also be used to traverse the subintimal space and, with the use of the Stingray balloon catheter and guidewire, allow guidewire lumen re-entry. Both the Crosser and CrossBoss have been utilized without a guidewire to cross the CTO.
Use of the Subintimal Space to Recanalize the CTO
Common problems associated with the antegrade approach to CTO are listed in Table 10-3.
Table 10-3 Commonly Encountered Problems With the Antegrade Approach and Potential Solutions
| Issue | Potential Solution |
|---|---|
| Cannot cross proximal cap |
Approaches to PCI for Total Occlusion of Saphenous Vein Grafts (SVGs)
Complications
A common misconception is that one cannot make a CTO worse. This is not true. In fact, as with every PCI, complications occur, the most dreaded being a free flowing (Type III) coronary perforation. The risk of each maneuver in producing a perforation must be considered, and the medical team should be prepared to manage the consequences should it occur. The general management principles for coronary perforation of a CTO are similar to other coronary perforations and are discussed elsewhere in this text (Chapter 4). Distal embolization, collateral closure, and rarely guidewire entrapment may also complicate the procedure. Because of the technical complexity, large contrast and radiation doses may be used, increasing the risk of contrast-induced nephropathy and radiation dermatitis. The operator must be aware of these doses during the procedure in order to minimize the risk of these complications.
Key Points for CTO PCI
• Develop a game plan prior to procedure, including limits of procedure for contrast, radiation, and time on cath lab table, and the technical approach, including guide catheter, wire, and stepwise strategy.
• Use bilateral coronary angiography in most cases to identify CTO characteristics, particularly length and presumed course.
• Consider stopping if myocardial staining of the myocardium or small contained perforation occurs.
• Stop if Type II or III perforation occurs, and treat perforation as described for management of complications. Employ anticoagulation reversal, balloon tamponade, and covered stent if necessary.
• If procedure is not successful, consider second attempt if other technical approaches may be used with a reasonable chance of success.
Godino C., Sharp A.S.P., Carlino M., et al. Crossing CTOs—the tips, tricks, and specialist kit that can mean the difference between success and failure. Catheter Cardiovasc Interv. 2009;74:1019–1046.
Morino Y., Abe M., Morimoto T. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–221.
Saito S. Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc Interv. 2008;71:8–19.
Stone G.W., Kandzari D.E., Mehran R., et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: Part I. Circulation. 2005;112:2364–2372.
Stone G.W., Kandzari D.E., Mehran R., et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: Part II. Circulation. 2005;112:2530–2537.
Sumutsuji S., Inoue K., Ochiai M., et al. Fundamental wire technique and current standard strategy of percutaneous intervention for chronic total occlusion with histopathological insights. JACC Cardiovasc Interv. 2011;4:941–951.