100
Pemphigus vulgaris
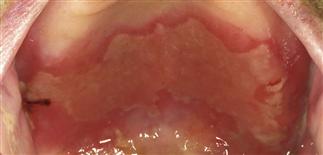
Oral erosions usually precede appearance of skin blisters by several weeks.

Flaccid blisters rupture easily because the roof consists of only a thin portion of upper epidermis and is very fragile. Healing is with brown hyperpigmentation, but without scarring.
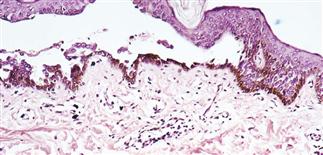
Skin biopsy shows intraepidermal bullae or acantholysis (separation of the epidermal cells) and mild to moderate infiltrate of eosinophils.

Mean age of onset is 60 years, and intraepidermal blistering involving the skin and mucous membranes is common.
DESCRIPTION
Rare, potentially life-threatening, autoimmune, intraepidermal blistering disease involving skin and mucous membranes. Often presents with only oral involvement.
HISTORY
• Mean age of onset 60 years; men and women affected equally. • Incidence estimated at 0.5–3.2/1 000 000; highest in people of Ashkenazi Jewish descent. • Oral erosions usually precede onset of skin blisters by weeks to months. • Most patients describe skin tenderness or irritation.
PHYSICAL FINDINGS
• Bullae vary from 1–3 cm in diameter. Initially localized but eventually become generalized if untreated. Bullae rupture easily because the vesicle roof is very fragile, consisting of a thin portion of upper epidermis. • Applying pressure to small intact bullae causes the fluid to dissect laterally (Asboe–Hansen sign). Traction pressure on intact skin causes bullae formation (Nikolsky sign). • Erosions heal without scarring. • Painful oral erosions occur in 50–70% of patients and are typically the initial presentation. • Skin biopsy with immunofluorescence recommended for all blistering diseases. Shows an intraepidermal bullae or separation of epidermal cells and an infiltrate of eosinophils. • Direct immunofluorescence performed on two biopsies: one from the edge of a fresh lesion, a second from an adjacent normal area showing IgG and often complement C3 in the intercellular substance areas of the epidermis. • Indirect immunofluorescence confirms circulating serum IgG antibodies in 80–90% of patients with active disease. These antibodies are directed against desmoglein-3, an intracellular keratinocyte adhesion molecule. Level of antibody reflects disease activity.
TREATMENT
• Consider dermatology referral for suspected cases, as both diagnosis and management require specialist training. • Prednisone with an immunosuppressive adjuvant agent such as azathioprine or cyclophosphamide is standard treatment. Goal of treatment is to arrest blister formation. Starting dosages of prednisone typically vary between 40 and 120 mg q.d., and are subsequently tapered to establish a minimum dose that controls most disease activity. • Cyclophosphamide (1.5–2.5 mg/kg q.d.) or azathioprine (1.0–2.5 mg/kg q.d.) is initiated with or after starting corticosteroids. • A negative direct immunofluorescence finding is a good indicator of remission. • IVIG should be used in patients with severe pemphigus where conventional therapy is contraindicated or the disease has been refractory to conventional forms of treatment. Treatment with IVIG results in a gradual decline in pemphigus autoantibodies.







