101
Pemphigus foliaceus

Pemphigus foliaceus is an autoimmune, intraepidermal blistering disease characterized by crusted patches and erosions.
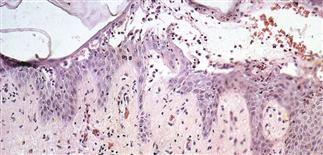
Skin biopsy shows intraepidermal bullae or acantholysis (separation of epidermal cells) in upper epidermis and mild to moderate eosinophil infiltration.
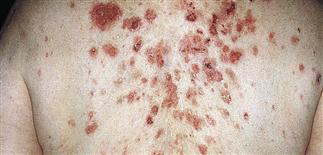
Disease begins gradually on the face in a ‘butterfly’ distribution, or first appears on scalp, chest, or upper back as localized or broad areas of erythema, scaling, crusting, or occasionally bullae.

Vesicle roof is so thin that it ruptures. Serum leaks out and desiccates, forming localized or broad areas of crust. Intact thin-walled blisters are sometimes seen near the edge of erosions.
DESCRIPTION
Autoimmune, superficial, intraepidermal blistering disease characterized by crusted plaques and erosions.
HISTORY
• Age of onset varies more widely than in pemphigus vulgaris. • No racial prevalence. • Pain, burning more often reported than itching. • Sun, heat may worsen signs and symptoms. • May be localized for years or progress rapidly and become generalized, evolving into an exfoliative erythroderma; may be fatal if untreated. • Increased incidence of thymoma, myasthenia gravis, other autoimmune disease. • Fogo selvagem is Portuguese for ‘wild fire.’ It is an endemic form of pemphigus foliaceus found in certain rural areas of Brazil and Colombia. • Pemphigus erythematosus (Senear–Usher syndrome) may be a combination of localized (face and other seborrheic areas) pemphigus foliaceus and systemic lupus erythematosus. Many of these patients have a positive antinuclear antibody, but few have any other signs or symptoms of systemic lupus. • Pemphigus foliaceus has been reported in approximately 5% of patients taking D-penicillamine or captopril. Most cases are mild and may resolve once the drug is stopped.
PHYSICAL FINDINGS
• Early pemphigus foliaceus may resemble seborrheic dermatitis or other papulosquamous diseases. Lesions appear in a ‘seborrheic’ distribution on face, scalp, chest, or upper back. • Disease begins as localized or broad continuous areas of erythema, scaling, crusting, or occasionally bullae. • Vesicle roof so thin that it ruptures. Serum leaks out and desiccates, forming localized or broad areas of crust. Intact thin-walled blisters sometimes seen near the edge of erosions. Intact blisters not usually seen but are sometimes near the edge of the erosions. • Upper portion of the epidermis can be dislodged with lateral finger pressure. • Skin biopsy with immunofluorescence recommended for all blistering diseases. Shows an intraepidermal bullae or acantholysis (separation of epidermal cells) in upper epidermis and mild to moderate infiltration of eosinophils. • Direct immunofluorescence performed on two biopsies: one from the edge of a fresh lesion, the second from an adjacent normal area. IgG and complement C3 are found in the intercellular substance areas of the epidermis. • Indirect immunofluorescence on serum confirms circulating IgG antibodies in approximately 75% of patients with active disease. Antibodies are directed against desmoglein-1, an intracellular keratinocyte adhesion molecule. Level of antibody reflects disease activity. Antibodies of pemphigus vulgaris can be distinguished from those of pemphigus foliaceus by testing on two tissue substrates.
TREATMENT
• Early localized disease may be managed with group I–III topical steroids. • Active widespread disease is treated like pemphigus vulgaris. Sun protection may be helpful.







