23
Pemphigus
Chapters 23–25 review the major autoimmune bullous diseases (Table 23.1). Because of the significant overlap in their clinical presentations, histologic examination of lesional skin (see Fig. 1.12B) as well as direct immunofluorescence (DIF) of perilesional skin (Figs. 23.1–23.3) are usually required in order to establish a specific diagnosis. Indirect immunofluorescence (IIF) and/or ELISA of sera provide additional helpful information; for example, the latter can detect anti-desmoglein 3 (Dsg3) versus anti-Dsg1 antibodies.
Table 23.1
Characteristics of major autoimmune bullous diseases.
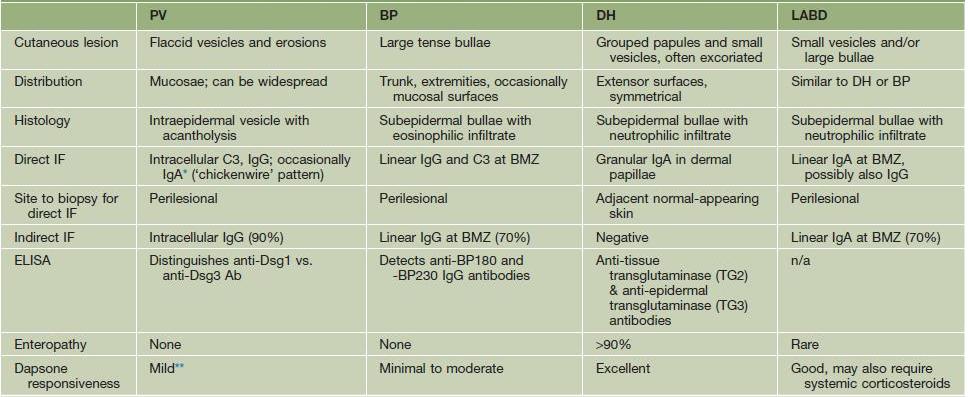
* Referred to as IgA pemphigus.
** Greater response if IgA +/or neutrophils.
Ab, antibody; BP, bullous pemphigoid; DH, dermatitis herpetiformis; ELISA, enzyme-linked immunosorbent assay; LABD, linear IgA bullous disease; n/a, not commercially available; PV, pemphigus vulgaris.
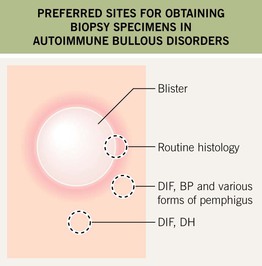
Fig. 23.1 Preferred sites for obtaining biopsy specimens in autoimmune bullous diseases. If the edematous papule or vesicle is small enough, it can be removed in its entirety for routine histology. Otherwise, a biopsy specimen that includes the inflammatory rim as well as the edge of a fresh vesicle or bulla is appropriate. In bullous pemphigoid (BP) and pemphigus vulgaris, a perilesional biopsy is done for direct immunofluorescence (DIF), whereas in dermatitis herpetiformis (DH), nearby normal skin is preferred for DIF.
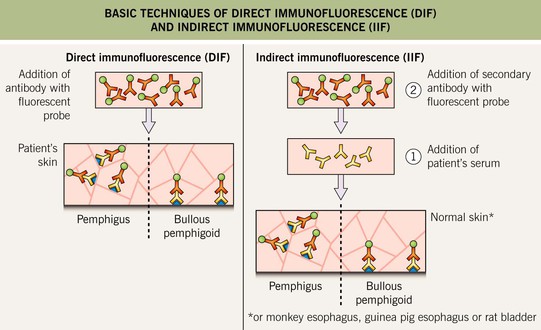
Fig. 23.2 Basic techniques of direct immunofluorescence (DIF) and indirect immunofluorescence (IIF). DIF is performed on skin biopsies to detect tissue-bound immunodeposits (see Fig. 23.1). IIF is performed utilizing patients’ sera to detect circulating autoantibodies that bind epithelial antigens. The preferred substrate for IIF is monkey esophagus for pemphigus vulgaris, guinea pig esophagus for pemphigus foliaceus, and human skin for the pemphigoid group and LABD.
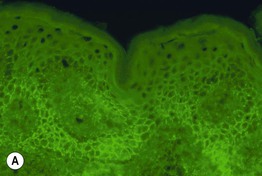
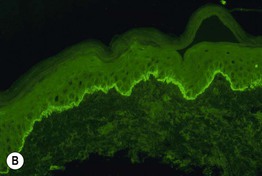
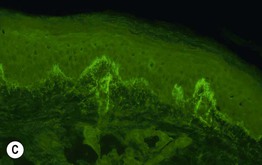
Fig. 23.3 Direct immunofluorescence (DIF) of skin in patients with pemphigus vulgaris (PV), bullous pemphigoid (BP), and dermatitis herpetiformis (DH). A Intercellular deposits of IgG within the lower epidermis in a chickenwire pattern (PV). B Linear deposits of C3 at the basement membrane zone (BP); a similar pattern of IgA deposition is seen in linear IgA bullous dermatosis. C Granular deposits of IgA within the dermal papillae (DH). Courtesy, Christine Ko, MD.
Pemphigus is classically divided into three major groups: (1) pemphigus vulgaris, with pemphigus vegetans representing a rare variant; (2) pemphigus foliaceus, with pemphigus erythematosus representing an unusual localized variant, and fogo selvagem, an endemic form; and (3) paraneoplastic pemphigus. Additional subtypes include the two forms of IgA pemphigus and drug-induced pemphigus.
Pemphigus Vulgaris and Pemphigus Vegetans
• The decrease in cell–cell adhesion leads to the separation of individual keratinocytes from one another (referred to as acantholysis) and the formation of a split within the epidermis or mucosal epithelium, primarily in its lower portion, just above the basal layer (see Fig. 1.12B).
• Clinically, almost all patients with pemphigus vulgaris have painful erosions of the oral mucosa and at least half will have flaccid bullae of the skin plus erosions due to their rupture; lesions can be localized or widespread (Fig. 23.4), and there may be involvement of other mucosal surfaces, e.g. conjunctival, nasal, vaginal.




Fig. 23.4 Pemphigus vulgaris. A, B Almost all patients develop painful erosions of the oral mucosa, with the most common locations being the buccal and palatine mucosae; note the sloughing of the mucosa in (B). C The flaccid vesicles are fragile and rupture easily, leading to erosions. D Extensive involvement is associated with significant fluid loss and risk of secondary infection and bacteremia. A, Courtesy, Masayuki Amagai, MD; B, C, Courtesy, Louis Fragola, Jr., MD; D, Courtesy, Department of Dermatology, Hamamatsu University School of Medicine.
• Additional clinical clues include the development of hemorrhagic crusts of the vermilion lips (Table 23.2) and a positive Nikolsky sign in areas of active disease – the epidermis can be easily moved laterally with rubbing (due to reduction in intercellular adhesion).
• In pemphigus vegetans, vegetative and papillomatous plaques and nodules develop at sites of erosions (Fig. 23.5); lesions favor major body folds and pustules can also be seen.

Fig. 23.5 Pemphigus vegetans. Multiple vegetating masses arising within eroded areas. Post-inflammatory hyperpigmentation is seen at previous sites of involvement. Courtesy, Masayuki Amagai, MD.
• DIF of perilesional skin demonstrates immunostaining of the cell surface of keratinocytes within the epidermis or mucosa in almost all patients, and the staining may be more predominant in the lower portion of the epithelium (see Fig. 23.3A); IIF and ELISA of sera is positive in more than 90% of patients (see Fig. 23.2).
Pemphigus Foliaceus, Pemphigus Erythematosus, and Fogo Selvagem
• Clinically, the more superficial and fragile nature of the blisters leads to a predominance of erosions with scale-crust rather than bullae (Fig. 23.6); the scale is said to resemble corn-flakes cereal; mucosal involvement is absent.



Fig. 23.6 Pemphigus foliaceus. A Scale-crusts overlying widespread erosions. B When the disease becomes severe, there is coalescence of lesions; note the large erosions. C The scales have been likened to cornflakes cereal. A, Courtesy, Masayuki Amagai, MD.
• While lesions favor the scalp, face, and upper trunk, they can become widespread, even leading to an exfoliative erythroderma, or they can be localized to the face (pemphigus erythematosus; Fig. 23.7).

Fig. 23.7 Pemphigus erythematosus. Erythematous plaques with scale-crust on the nose and cheeks. Initially this disorder was thought to be a combination of pemphigus vulgaris plus lupus erythematosus, but now it is classified as a localized variant of pemphigus foliaceus. Courtesy, Ronald P. Rapini, MD.
• Fogo selvagem is an endemic form of pemphigus foliaceus seen primarily in rural areas of Brazil and is thought to be related to an immune reaction to antigens introduced by insect bites.
• Rx: topical or oral CS, occasionally dapsone; if severe, steroid-sparing agents.
Paraneoplastic Pemphigus
• Cutaneous lesions are variable and they can resemble lichen planus, erythema multiforme, or bullous pemphigoid as well as pemphigus; severe, recalcitrant oral stomatitis is a characteristic feature and conjunctival involvement is common (Fig. 23.8).

Fig. 23.8 Paraneoplastic pemphigus. Hemorrhagic crusts extend from the nasal and oral mucosae onto the cutaneous and vermilion lips. The chin lesion resembles pemphigus vulgaris. Courtesy, Masayuki Amagai, MD.
• Bronchiolitis obliterans is a serious internal manifestation.
IgA Pemphigus
• Clinically, lesions arise within inflamed or normal skin and assume a figurate arrangement (Fig. 23.9); the most common sites are the axillae and groin.

Fig. 23.9 IgA pemphigus – subcorneal pustular dermatosis type. Annular configuration of pink-brown patches and thin plaques with erosions and scale-crust; in the vesiculopustule, the pustular contents have settled into a dependent location (half pustular/half clear). Courtesy, Masayuki Amagai, MD.
• By DIF, there is immunostaining of the cell surface of keratinocytes within the epidermis, as in pemphigus vulgaris, but the immunodeposits are IgA rather than IgG.