Pelvis and Perineum
ADDITIONAL LEARNING RESOURCES for Chapter 5, Pelvis and Perineum, on STUDENT CONSULT (www.studentconsult.com):
Conceptual overview
General description
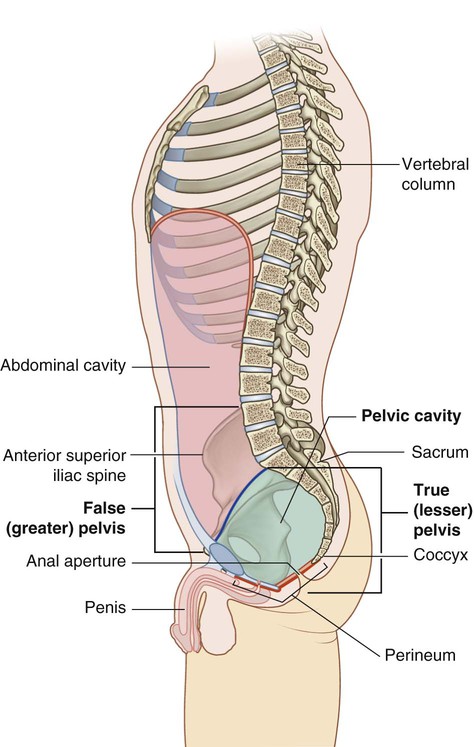
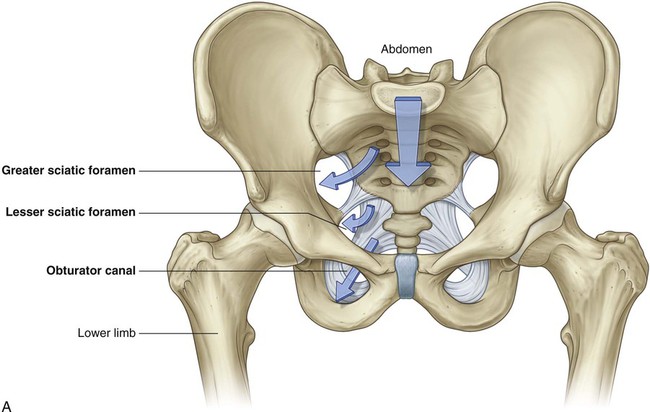
 The superior region related to upper parts of the pelvic bones and lower lumbar vertebrae is the false pelvis (greater pelvis) and is generally considered part of the abdomen (Fig. 5.1).
The superior region related to upper parts of the pelvic bones and lower lumbar vertebrae is the false pelvis (greater pelvis) and is generally considered part of the abdomen (Fig. 5.1).
 The true pelvis (lesser pelvis) is related to the inferior parts of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet.
The true pelvis (lesser pelvis) is related to the inferior parts of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet.
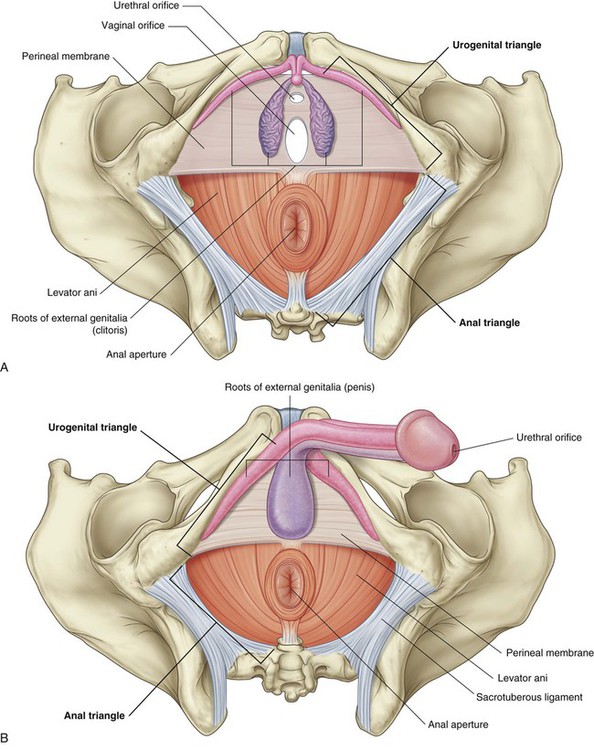
The perineum (Fig. 5.1) is inferior to the floor of the pelvic cavity; its boundaries form the pelvic outlet. The perineum contains the external genitalia and external openings of the genitourinary and gastrointestinal systems.
Functions
Contains and supports the bladder, rectum, anal canal, and reproductive tracts
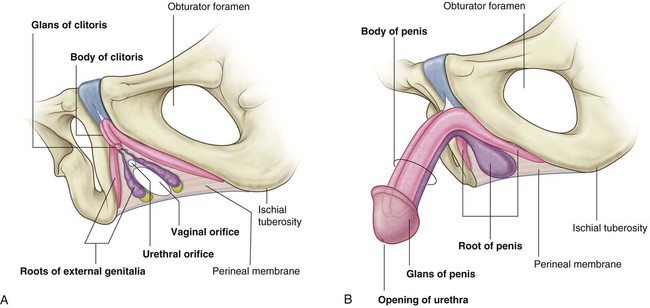
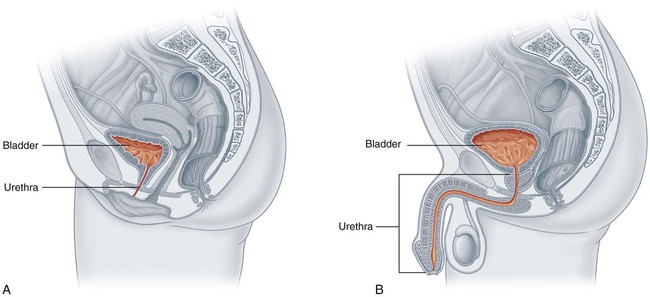
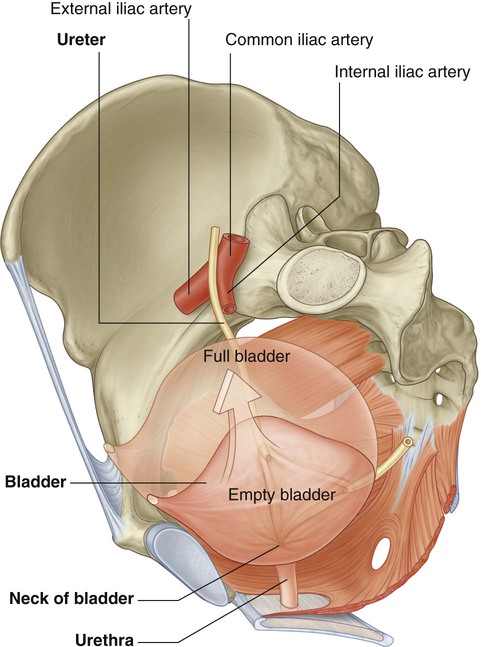
As it fills, the bladder expands superiorly into the abdomen. It is supported by adjacent elements of the pelvic bone and by the pelvic floor. The urethra passes through the pelvic floor to the perineum, where, in women, it opens externally (Fig. 5.2A) and in men it enters the base of the penis (Fig. 5.2B).
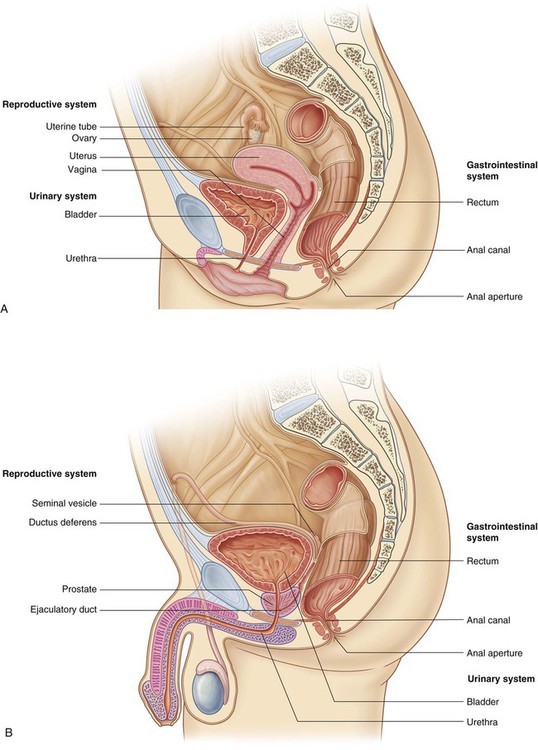
 In women, the vagina penetrates the pelvic floor and connects with the uterus in the pelvic cavity. The uterus is positioned between the rectum and the bladder. A uterine (fallopian) tube extends laterally on each side toward the pelvic wall to open near the ovary.
In women, the vagina penetrates the pelvic floor and connects with the uterus in the pelvic cavity. The uterus is positioned between the rectum and the bladder. A uterine (fallopian) tube extends laterally on each side toward the pelvic wall to open near the ovary.
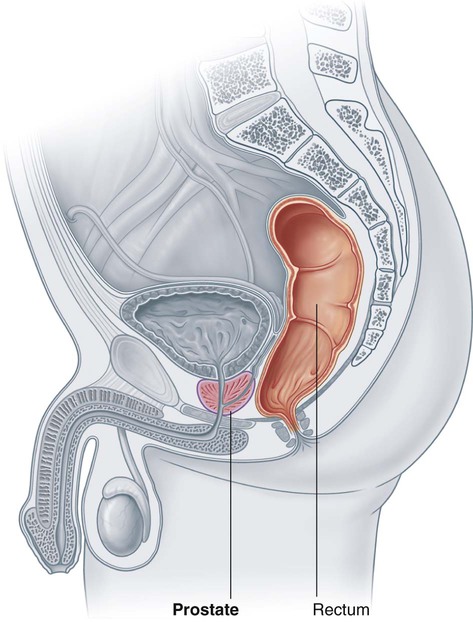
 In men, the pelvic cavity contains the site of connection between the urinary and reproductive tracts. It also contains major glands associated with the reproductive system—the prostate and two seminal vesicles.
In men, the pelvic cavity contains the site of connection between the urinary and reproductive tracts. It also contains major glands associated with the reproductive system—the prostate and two seminal vesicles.
Component parts
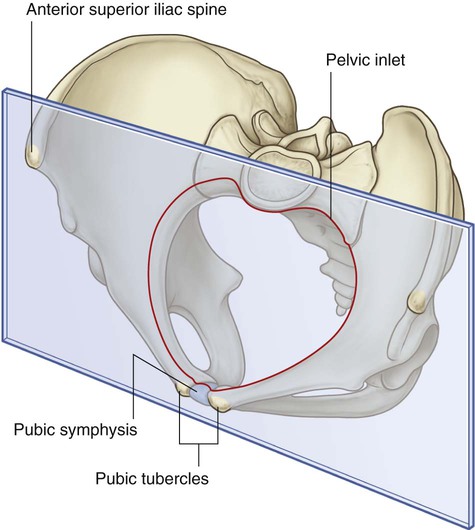
Pelvic inlet
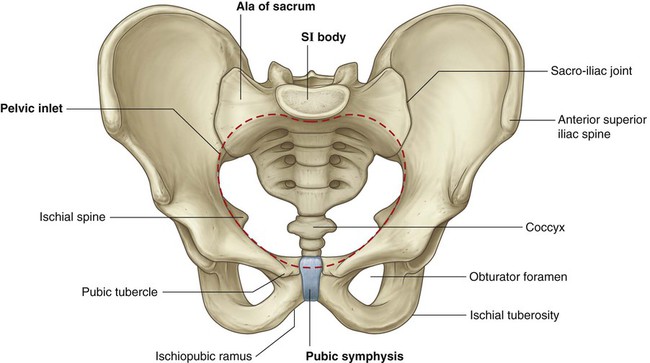
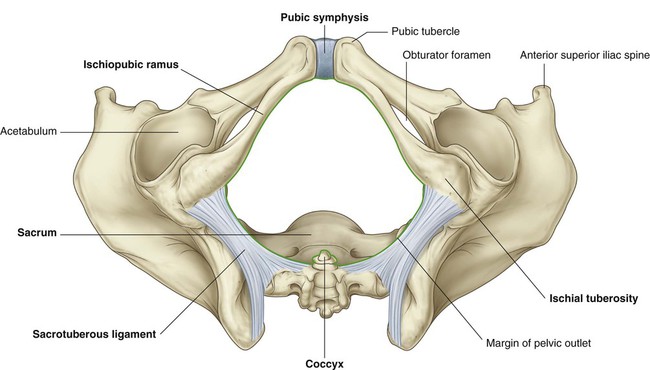
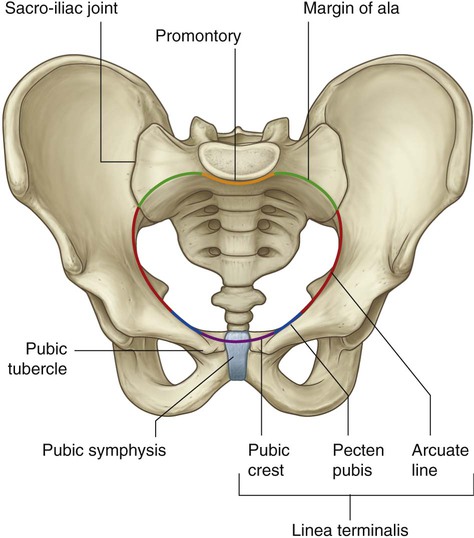
The pelvic inlet is somewhat heart shaped and completely ringed by bone (Fig. 5.4). Posteriorly, the inlet is bordered by the body of vertebra SI, which projects into the inlet as the sacral promontory. On each side of this vertebra, wing-like transverse processes called the alae (wings) contribute to the margin of the pelvic inlet. Laterally, a prominent rim on the pelvic bone continues the boundary of the inlet forward to the pubic symphysis, where the two pelvic bones are joined in the midline.
Structures pass between the pelvic cavity and the abdomen through the pelvic inlet.
Pelvic walls
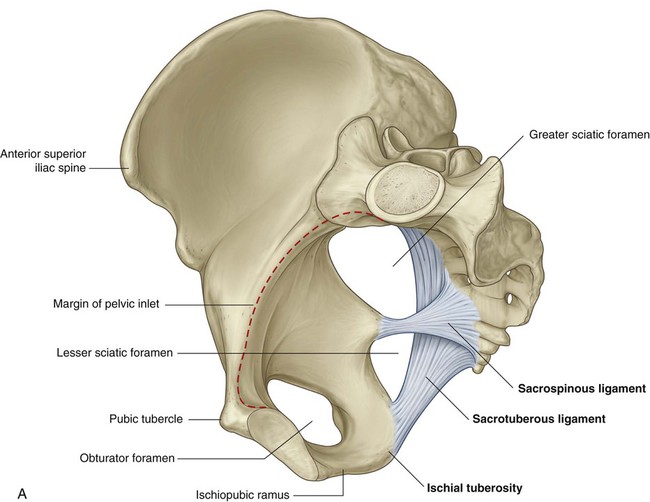
Two ligaments—the sacrospinous and the sacrotuberous ligaments—are important architectural elements of the walls because they link each pelvic bone to the sacrum and coccyx (Fig. 5.5A). These ligaments also convert two notches on the pelvic bones—the greater and lesser sciatic notches—into foramina on the lateral pelvic walls.
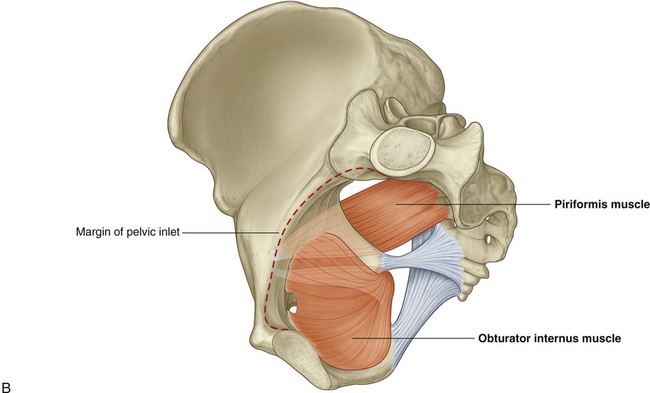
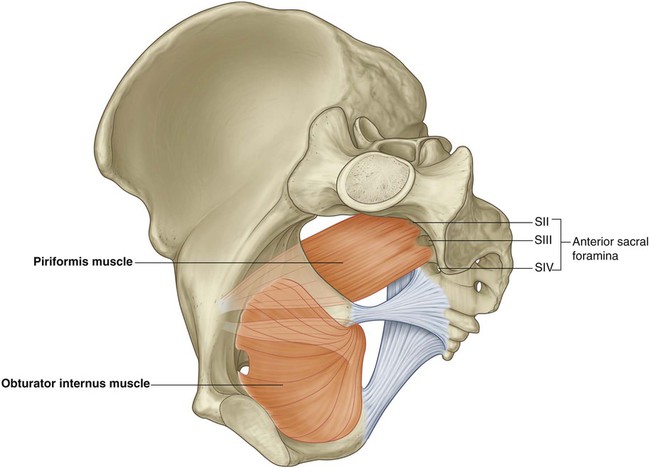
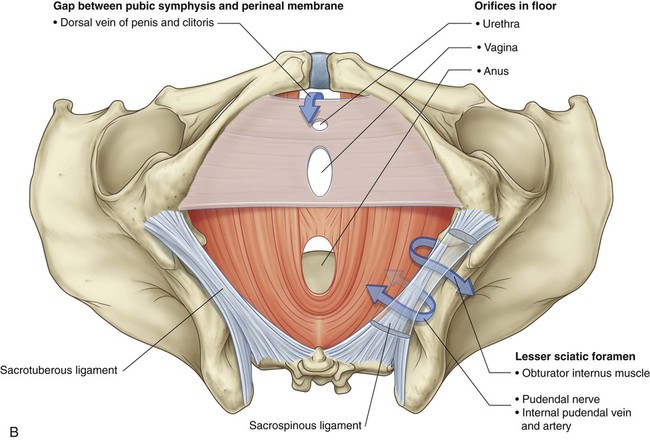
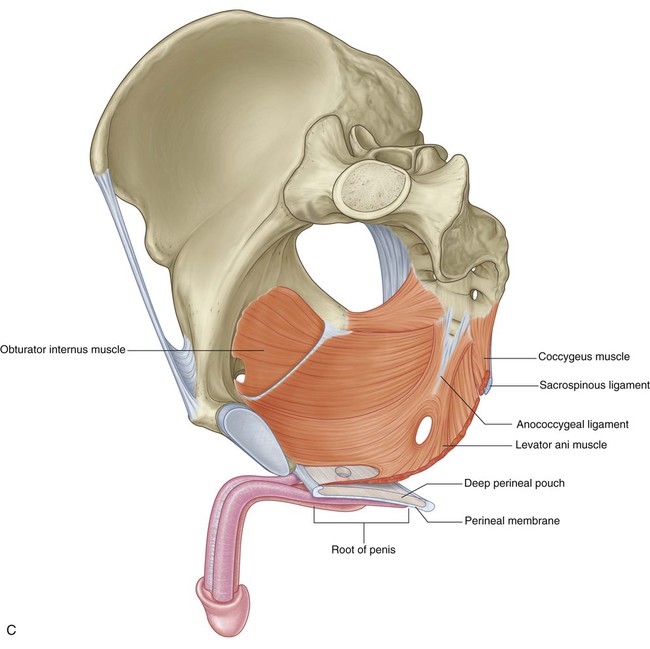
Completing the walls are the obturator internus and piriformis muscles (Fig. 5.5B), which arise in the pelvis and exit through the sciatic foramina to act on the hip joint.
Pelvic floor
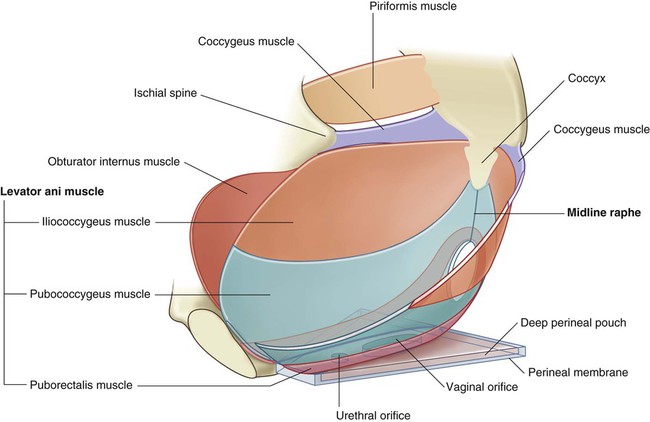
The pelvic floor, which separates the pelvic cavity from the perineum, is formed by muscles and fascia (Fig. 5.7).
The pelvic floor is supported anteriorly by:
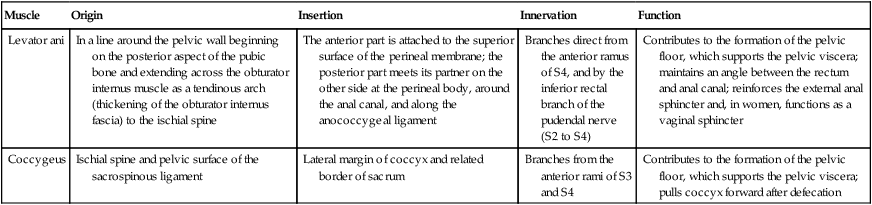
The perineal membrane is a thick, triangular fascial sheet that fills the space between the arms of the pubic arch, and has a free posterior border (Fig. 5.7). The deep perineal pouch is a narrow region superior to the perineal membrane.
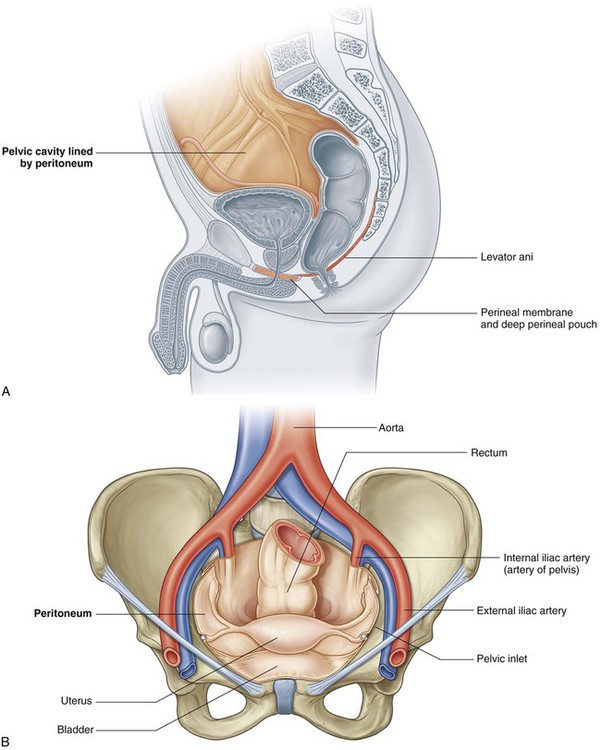
Pelvic cavity
The pelvic cavity is lined by peritoneum continuous with the peritoneum of the abdominal cavity that drapes over the superior aspects of the pelvic viscera, but in most regions, does not reach the pelvic floor (Fig. 5.8A).
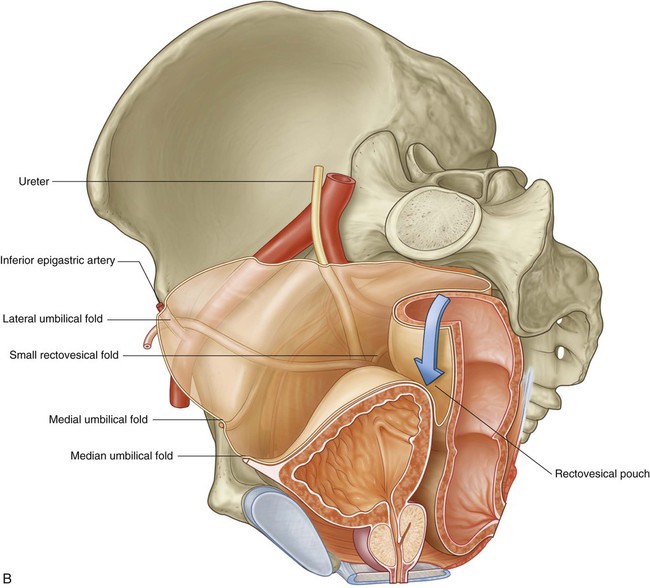
The pelvic viscera are located in the midline of the pelvic cavity. The bladder is anterior and the rectum is posterior. In women, the uterus lies between the bladder and rectum (Fig. 5.8B). Other structures, such as vessels and nerves, lie deep to the peritoneum in association with the pelvic walls and on either side of the pelvic viscera.
Perineum
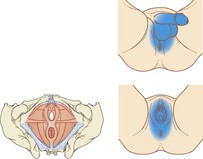
The perineum lies inferior to the pelvic floor between the lower limbs (Fig. 5.9). Its margin is formed by the pelvic outlet. An imaginary line between the ischial tuberosities divides the perineum into two triangular regions.
 Anteriorly, the urogenital triangle contains the roots of the external genitalia and, in women, the openings of the urethra and the vagina (Fig. 5.9A). In men, the distal part of the urethra is enclosed by erectile tissues and opens at the end of the penis (Fig. 5.9B).
Anteriorly, the urogenital triangle contains the roots of the external genitalia and, in women, the openings of the urethra and the vagina (Fig. 5.9A). In men, the distal part of the urethra is enclosed by erectile tissues and opens at the end of the penis (Fig. 5.9B).
Relationship to other regions
Abdomen
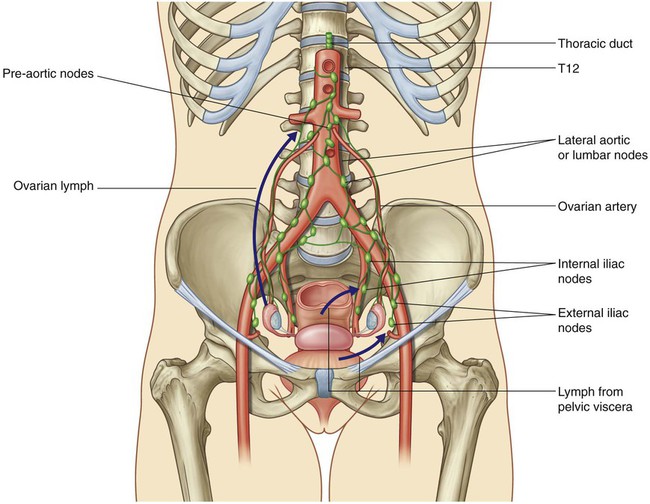
The cavity of the true pelvis is continuous with the abdominal cavity at the pelvic inlet (Fig. 5.10A). All structures passing between the pelvic cavity and abdomen, including major vessels, nerves, and lymphatics, as well as the sigmoid colon and ureters, pass via the inlet. In men, the ductus deferens on each side passes through the anterior abdominal wall and over the inlet to enter the pelvic cavity. In women, ovarian vessels, nerves, and lymphatics pass through the inlet to reach the ovaries, which lie on each side just inferior to the pelvic inlet.
Lower limb
Three apertures in the pelvic wall communicate with the lower limb (Fig. 5.10A):
The lesser sciatic foramen, which lies inferior to the pelvic floor, provides communication between the gluteal region and the perineum (Fig. 5.10B).
The pelvic cavity also communicates directly with the perineum through a small gap between the pubic symphysis and the perineal membrane (Fig. 5.10B).
Key features
The pelvic cavity projects posteriorly
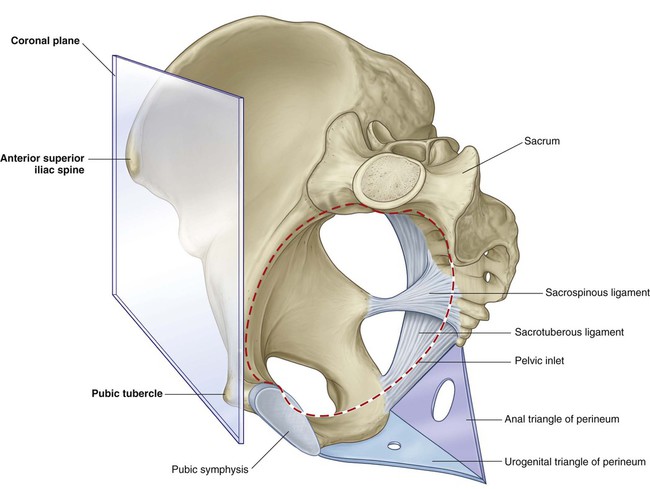
In the anatomical position, the anterior superior iliac spines and the superior edge of the pubic symphysis lie in the same vertical plane (Fig. 5.11). Consequently, the pelvic inlet is angled 50°–60° forward relative to the horizontal plane, and the pelvic cavity projects posteriorly from the abdominal cavity.
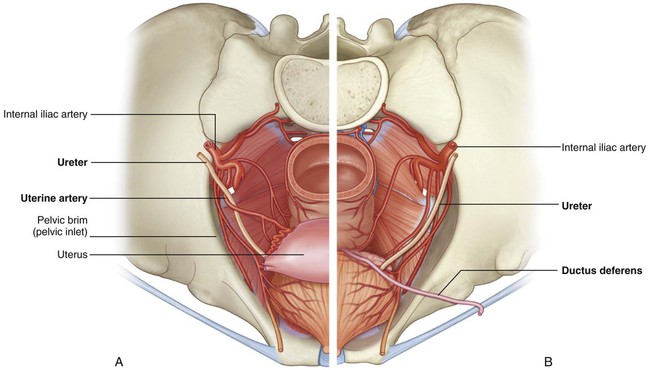
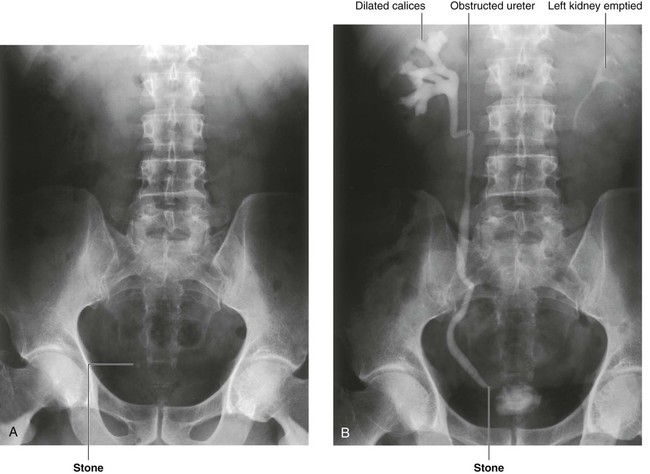
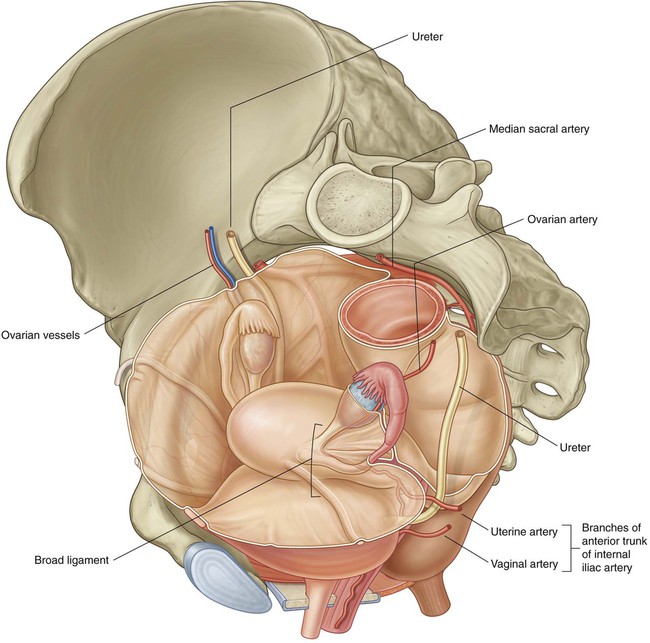
Important structures cross the ureters in the pelvic cavity
An important structure crosses the ureters in the pelvic cavity in both men and women—in women, the uterine artery crosses the ureter lateral to the cervix of the uterus (Fig. 5.12A), and in men, the ductus deferens crosses over the ureter just posterior to the bladder (Fig. 5.12B).
The perineum is innervated by sacral spinal cord segments
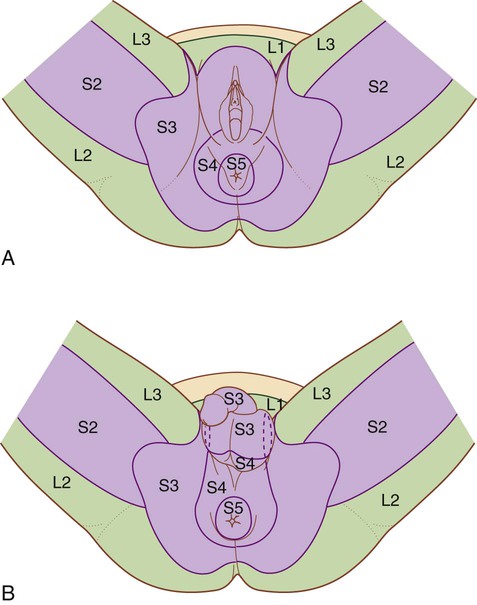
Dermatomes of the perineum in both men and women are from spinal cord levels S3 to S5, except for the anterior regions, which tend to be innervated by spinal cord level L1 by nerves associated with the abdominal wall (Fig. 5.14). Dermatomes of L2 to S2 are predominantly in the lower limb.
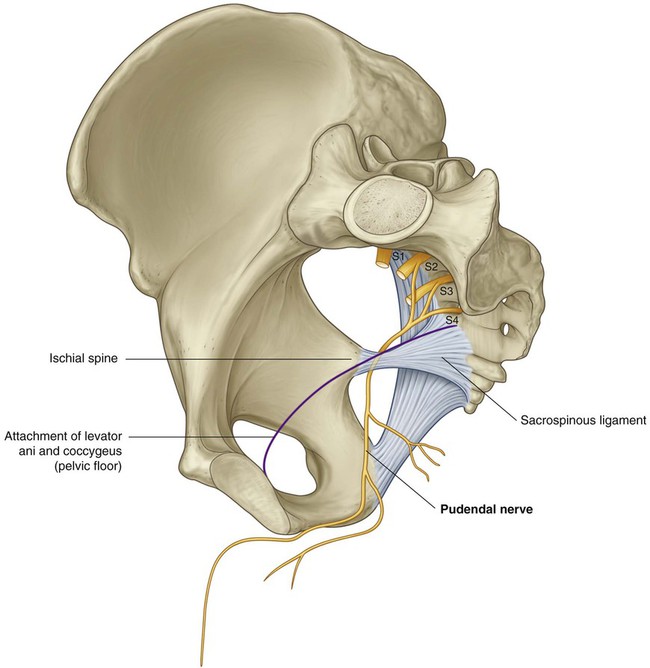
Nerves are related to bone
The pudendal nerve is the major nerve of the perineum and is directly associated with the ischial spine of the pelvis (Fig. 5.15). On each side of the body, these spines and the attached sacrospinous ligaments separate the greater sciatic foramina from the lesser sciatic foramina on the lateral pelvic wall.
The pudendal nerve leaves the pelvic cavity through the greater sciatic foramen and then immediately enters the perineum inferiorly to the pelvic floor by passing around the ischial spine and through the lesser sciatic foramen (Fig. 5.15). The ischial spine can be palpated transvaginally in women and is the landmark for administering a pudendal nerve block.
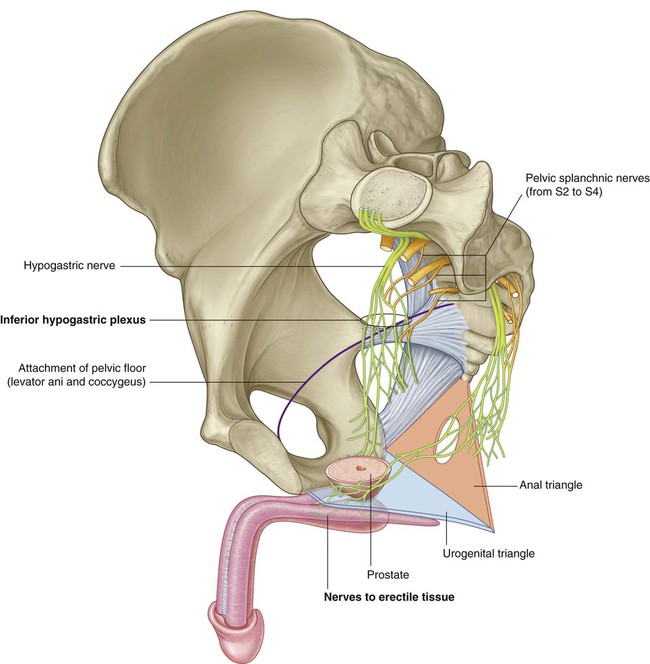
Parasympathetic innervation from spinal cord levels S2 to S4 controls erection
The parasympathetic innervation from spinal cord levels S2 to S4 controls genital erection in both women and men (Fig. 5.16). On each side, preganglionic parasympathetic nerves leave the anterior rami of the sacral spinal nerves and enter the inferior hypogastric plexus (pelvic plexus) on the lateral pelvic wall.
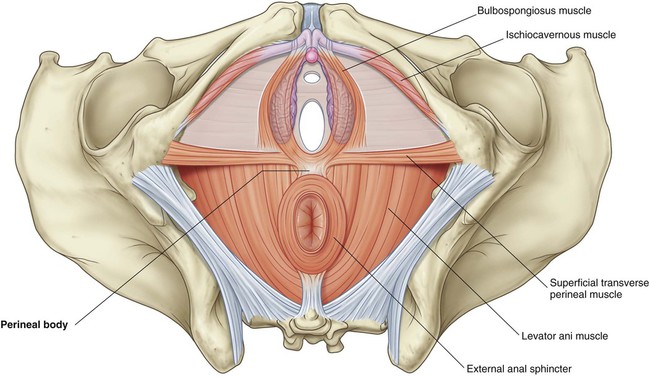
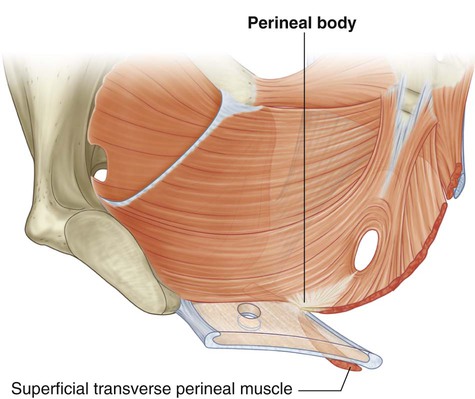
Muscles and fascia of the pelvic floor and perineum intersect at the perineal body
Structures of the pelvic floor intersect with structures in the perineum at the perineal body (Fig. 5.17). This poorly defined fibromuscular node lies at the center of the perineum, approximately midway between the two ischial tuberosities. Converging at the perineal body are:
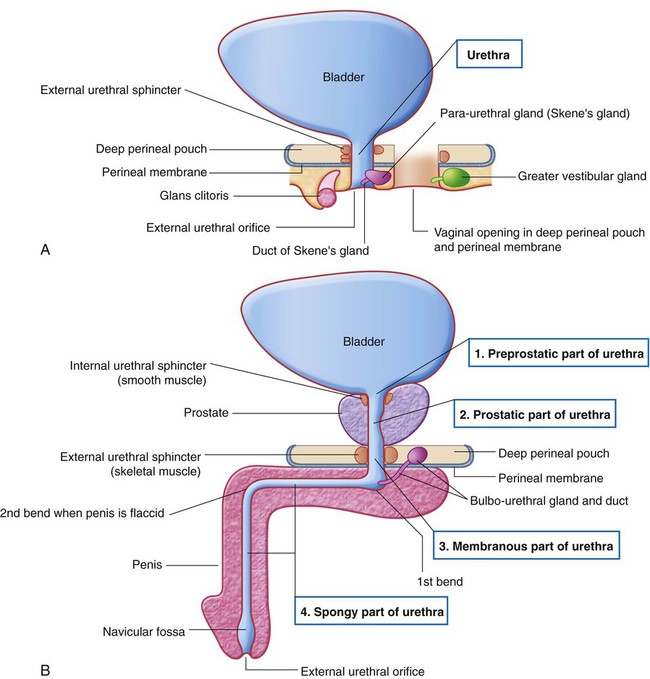
The course of the urethra is different in men and women
In women, the urethra is short and passes inferiorly from the bladder through the pelvic floor and opens directly into the perineum (Fig. 5.18A).
In men the urethra passes through the prostate before coursing through the deep perineal pouch and perineal membrane and then becomes enclosed within the erectile tissues of the penis before opening at the end of the penis (Fig. 5.18B). The penile part of the male urethra has two angles:
Regional anatomy
 the terminal openings of the gastrointestinal and urinary systems,
the terminal openings of the gastrointestinal and urinary systems,
Pelvis
Bones
Pelvic bone
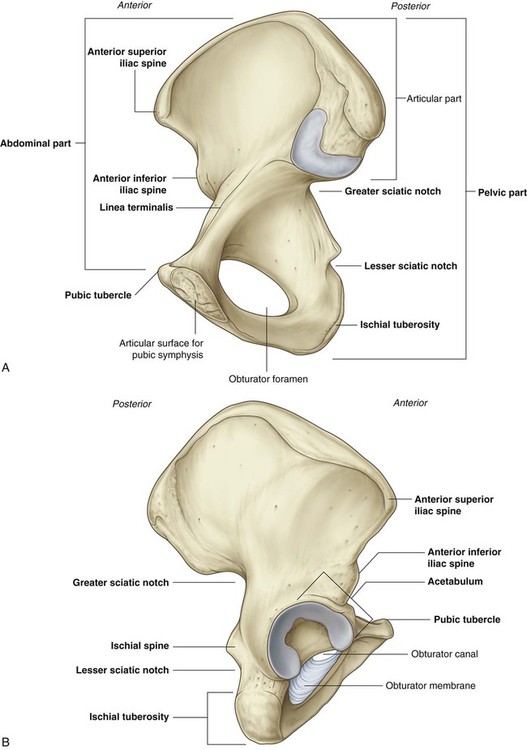
The pelvic bone is irregular in shape and has two major parts separated by an oblique line on the medial surface of the bone (Fig. 5.19A):
 The pelvic bone above this line represents the lateral wall of the false pelvis, which is part of the abdominal cavity.
The pelvic bone above this line represents the lateral wall of the false pelvis, which is part of the abdominal cavity.
 The pelvic bone below this line represents the lateral wall of the true pelvis, which contains the pelvic cavity.
The pelvic bone below this line represents the lateral wall of the true pelvis, which contains the pelvic cavity.
The lateral surface of the pelvic bone has a large articular socket, the acetabulum, which, together with the head of the femur, forms the hip joint (Fig. 5.19B).
The posterior margin of the bone is marked by two notches separated by the ischial spine:
The posterior margin terminates inferiorly as the large ischial tuberosity.
Components of the pelvic bone
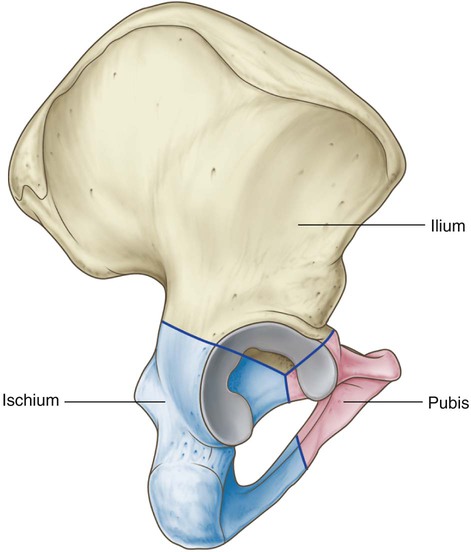
Each pelvic bone is formed by three elements: the ilium, pubis, and ischium. At birth, these bones are connected by cartilage in the area of the acetabulum; later, at between 16 and 18 years of age, they fuse into a single bone (Fig. 5.20).
Of the three components of the pelvic bone, the ilium is the most superior in position.
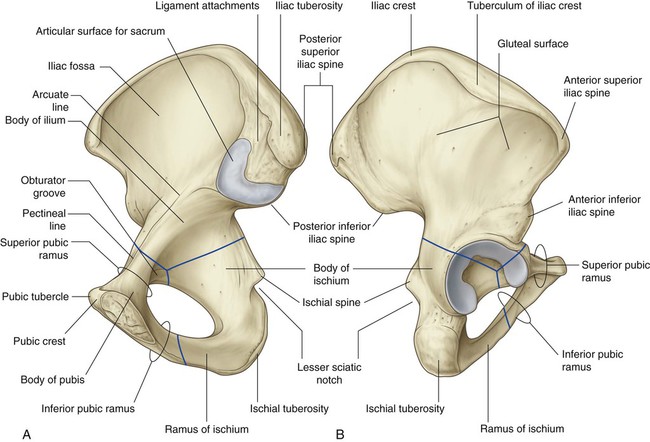
The ilium is separated into upper and lower parts by a ridge on the medial surface (Fig. 5.21A).
 Posteriorly, the ridge is sharp and lies immediately superior to the surface of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened area for the attachment of the strong ligaments that support the sacro-iliac joint (Fig. 5.21).
Posteriorly, the ridge is sharp and lies immediately superior to the surface of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened area for the attachment of the strong ligaments that support the sacro-iliac joint (Fig. 5.21).
 Anteriorly, the ridge separating the upper and lower parts of the ilium is rounded and termed the arcuate line.
Anteriorly, the ridge separating the upper and lower parts of the ilium is rounded and termed the arcuate line.
The arcuate line forms part of the linea terminalis and the pelvic brim.
The upper part of the ilium expands to form a flat, fan-shaped “wing,” which provides bony support for the lower abdomen, or false pelvis. This part of the ilium provides attachment for muscles functionally associated with the lower limb. The anteromedial surface of the wing is concave and forms the iliac fossa. The external (gluteal) surface of the wing is marked by lines and roughenings and is related to the gluteal region of the lower limb (Fig. 5.21B).
The anterior and inferior part of the pelvic bone is the pubis (Fig. 5.21). It has a body and two arms (rami).
 The body is flattened dorsoventrally and articulates with the body of the pubic bone on the other side at the pubic symphysis. The body has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle.
The body is flattened dorsoventrally and articulates with the body of the pubic bone on the other side at the pubic symphysis. The body has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle.
 The superior pubic ramus projects posterolaterally from the body and joins with the ilium and ischium at its base, which is positioned toward the acetabulum. The sharp superior margin of this triangular surface is termed the pecten pubis (pectineal line), which forms part of the linea terminalis of the pelvic bone and the pelvic inlet. Anteriorly, this line is continuous with the pubic crest, which also is part of the linea terminalis and pelvic inlet. The superior pubic ramus is marked on its inferior surface by the obturator groove, which forms the upper margin of the obturator canal.
The superior pubic ramus projects posterolaterally from the body and joins with the ilium and ischium at its base, which is positioned toward the acetabulum. The sharp superior margin of this triangular surface is termed the pecten pubis (pectineal line), which forms part of the linea terminalis of the pelvic bone and the pelvic inlet. Anteriorly, this line is continuous with the pubic crest, which also is part of the linea terminalis and pelvic inlet. The superior pubic ramus is marked on its inferior surface by the obturator groove, which forms the upper margin of the obturator canal.
 The inferior ramus projects laterally and inferiorly to join with the ramus of the ischium.
The inferior ramus projects laterally and inferiorly to join with the ramus of the ischium.
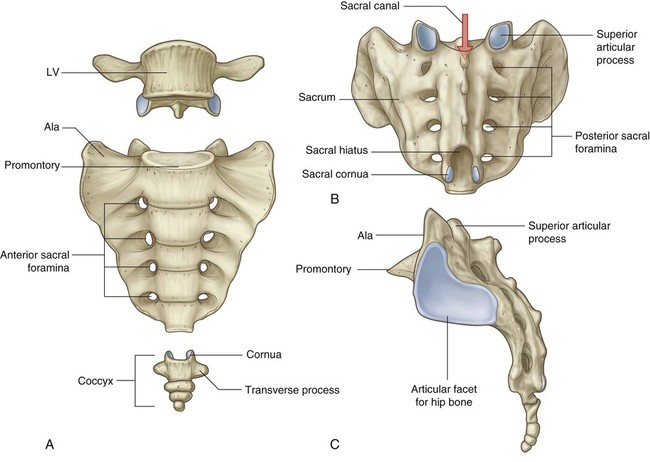
Sacrum
The sacrum, which has the appearance of an inverted triangle, is formed by the fusion of the five sacral vertebrae (Fig. 5.22). The base of the sacrum articulates with vertebra LV, and its apex articulates with the coccyx. Each of the lateral surfaces of the bone bears a large L-shaped facet for articulation with the ilium of the pelvic bone. Posterior to the facet is a large roughened area for the attachment of ligaments that support the sacro-iliac joint. The superior surface of the sacrum is characterized by the superior aspect of the body of vertebra SI and is flanked on each side by an expanded wing-like transverse process termed the ala. The anterior edge of the vertebral body projects forward as the promontory. The anterior surface of the sacrum is concave; the posterior surface is convex. Because the transverse processes of adjacent sacral vertebrae fuse lateral to the position of the intervertebral foramina and lateral to the bifurcation of spinal nerves into posterior and anterior rami, the posterior and anterior rami of spinal nerves S1 to S4 emerge from the sacrum through separate foramina. There are four pairs of anterior sacral foramina on the anterior surface of the sacrum for anterior rami, and four pairs of posterior sacral foramina on the posterior surface for the posterior rami. The sacral canal is a continuation of the vertebral canal that terminates as the sacral hiatus.
Coccyx
The small terminal part of the vertebral column is the coccyx, which consists of four fused coccygeal vertebrae (Fig. 5.22) and, like the sacrum, has the shape of an inverted triangle. The base of the coccyx is directed superiorly. The superior surface bears a facet for articulation with the sacrum and two horns, or cornua, one on each side, that project upward to articulate or fuse with similar downward-projecting cornua from the sacrum. These processes are modified superior and inferior articular processes that are present on other vertebrae. Each lateral surface of the coccyx has a small rudimentary transverse process, extending from the first coccygeal vertebra. Vertebral arches are absent from coccygeal vertebrae; therefore no bony vertebral canal is present in the coccyx.
Joints
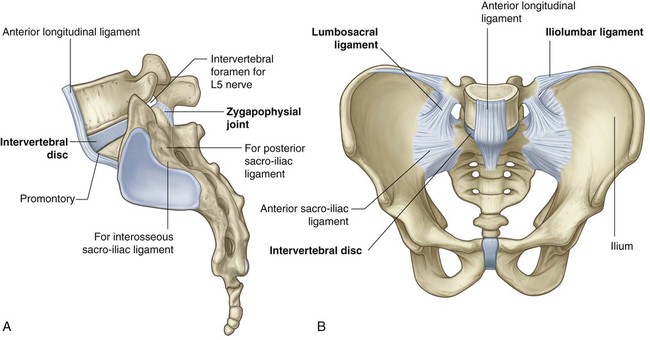
Lumbosacral joints
 the two zygapophysial joints, which occur between adjacent inferior and superior articular processes, and
the two zygapophysial joints, which occur between adjacent inferior and superior articular processes, and
 an intervertebral disc that joins the bodies of vertebrae LV and SI (Fig. 5.23A).
an intervertebral disc that joins the bodies of vertebrae LV and SI (Fig. 5.23A).
The lumbosacral joints are reinforced by strong iliolumbar and lumbosacral ligaments that extend from the expanded transverse processes of vertebra LV to the ilium and the sacrum, respectively (Fig. 5.23B).
Sacro-iliac joints
The sacro-iliac joints transmit forces from the lower limbs to the vertebral column. They are synovial joints between the L-shaped articular facets on the lateral surfaces of the sacrum and similar facets on the iliac parts of the pelvic bones (Fig. 5.24A). The joint surfaces have an irregular contour and interlock to resist movement. The joints often become fibrous with age and may become completely ossified.
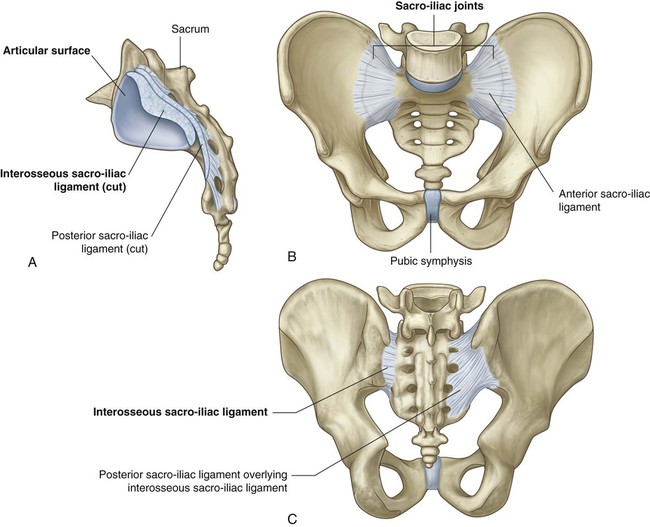
Each sacro-iliac joint is stabilized by three ligaments:
 the anterior sacro-iliac ligament, which is a thickening of the fibrous membrane of the joint capsule and runs anteriorly and inferiorly to the joint (Fig. 5.24B);
the anterior sacro-iliac ligament, which is a thickening of the fibrous membrane of the joint capsule and runs anteriorly and inferiorly to the joint (Fig. 5.24B);
 the interosseous sacro-iliac ligament, which is the largest, strongest ligament of the three, and is positioned immediately posterosuperior to the joint and attaches to adjacent expansive roughened areas on the ilium and sacrum, thereby filling the gap between the two bones (Fig. 5.24A,C); and
the interosseous sacro-iliac ligament, which is the largest, strongest ligament of the three, and is positioned immediately posterosuperior to the joint and attaches to adjacent expansive roughened areas on the ilium and sacrum, thereby filling the gap between the two bones (Fig. 5.24A,C); and
 the posterior sacro-iliac ligament, which covers the interosseous sacro-iliac ligament (Fig. 5.24C).
the posterior sacro-iliac ligament, which covers the interosseous sacro-iliac ligament (Fig. 5.24C).
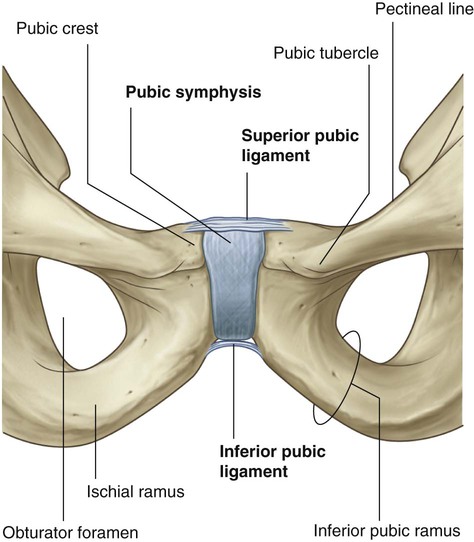
Pubic symphysis joint
The pubic symphysis lies anteriorly between the adjacent surfaces of the pubic bones (Fig. 5.25). Each of the joint’s surfaces is covered by hyaline cartilage and is linked across the midline to adjacent surfaces by fibrocartilage. The joint is surrounded by interwoven layers of collagen fibers and the two major ligaments associated with it are:
Orientation
In the anatomical position, the pelvis is oriented so that the front edge of the top of the pubic symphysis and the anterior superior iliac spines lie in the same vertical plane (Fig. 5.26). As a consequence, the pelvic inlet, which marks the entrance to the pelvic cavity, is tilted to face anteriorly, and the bodies of the pubic bones and the pubic arch are positioned in a nearly horizontal plane facing the ground.
Differences between men and women
 The pelvic inlet in women is circular (Fig. 5.27A) compared with the heart-shaped pelvic inlet (Fig. 5.27B) in men. The more circular shape is partly caused by the less distinct promontory and broader alae in women.
The pelvic inlet in women is circular (Fig. 5.27A) compared with the heart-shaped pelvic inlet (Fig. 5.27B) in men. The more circular shape is partly caused by the less distinct promontory and broader alae in women.
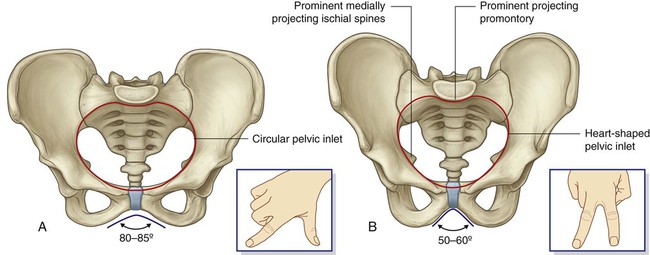
 The angle formed by the two arms of the pubic arch is larger in women (80°–85°) than it is in men (50°–60°).
The angle formed by the two arms of the pubic arch is larger in women (80°–85°) than it is in men (50°–60°).
 The ischial spines generally do not project as far medially into the pelvic cavity in women as they do in men.
The ischial spines generally do not project as far medially into the pelvic cavity in women as they do in men.
True pelvis
Pelvic inlet
The pelvic inlet is the circular opening between the abdominal cavity and the pelvic cavity through which structures traverse between the abdomen and pelvic cavity. It is completely surrounded by bones and joints (Fig. 5.28). The promontory of the sacrum protrudes into the inlet, forming its posterior margin in the midline. On either side of the promontory, the margin is formed by the alae of the sacrum. The margin of the pelvic inlet then crosses the sacro-iliac joint and continues along the linea terminalis (i.e., the arcuate line, the pecten pubis or pectineal line, and the pubic crest) to the pubic symphysis.
Pelvic wall
Ligaments of the pelvic wall
The sacrospinous and sacrotuberous ligaments (Fig. 5.29A) are major components of the lateral pelvic walls that help define the apertures between the pelvic cavity and adjacent regions through which structures pass.
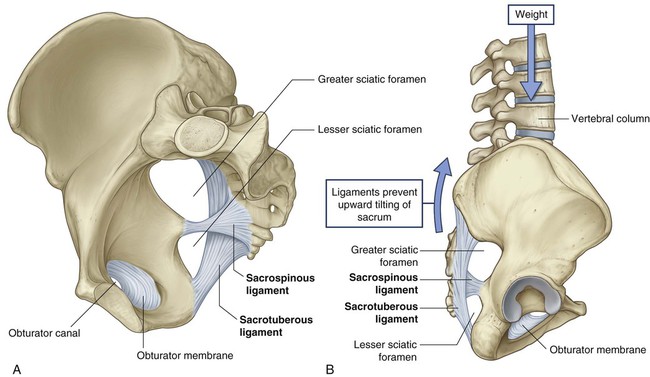
 The smaller of the two, the sacrospinous ligament, is triangular, with its apex attached to the ischial spine and its base attached to the related margins of the sacrum and the coccyx.
The smaller of the two, the sacrospinous ligament, is triangular, with its apex attached to the ischial spine and its base attached to the related margins of the sacrum and the coccyx.
 The sacrotuberous ligament is also triangular and is superficial to the sacrospinous ligament. Its base has a broad attachment that extends from the posterior superior iliac spine of the pelvic bone, along the dorsal aspect and the lateral margin of the sacrum, and onto the dorsolateral surface of the coccyx. Laterally, the apex of the ligament is attached to the medial margin of the ischial tuberosity.
The sacrotuberous ligament is also triangular and is superficial to the sacrospinous ligament. Its base has a broad attachment that extends from the posterior superior iliac spine of the pelvic bone, along the dorsal aspect and the lateral margin of the sacrum, and onto the dorsolateral surface of the coccyx. Laterally, the apex of the ligament is attached to the medial margin of the ischial tuberosity.
These ligaments stabilize the sacrum on the pelvic bones by resisting the upward tilting of the inferior aspect of the sacrum (Fig. 5.29B). They also convert the greater and lesser sciatic notches of the pelvic bone into foramina (Fig. 5.29A,B).
Muscles of the pelvic wall
The obturator internus is a flat, fan-shaped muscle that originates from the deep surface of the obturator membrane and from associated regions of the pelvic bone that surround the obturator foramen (Fig. 5.30 and Table 5.1).
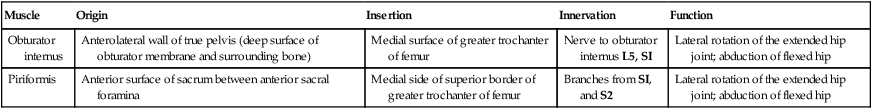
Table 5.1
| Muscle | Origin | Insertion | Innervation | Function |
| Obturator internus | Anterolateral wall of true pelvis (deep surface of obturator membrane and surrounding bone) | Medial surface of greater trochanter of femur | Nerve to obturator internus L5, SI | Lateral rotation of the extended hip joint; abduction of flexed hip |
| Piriformis | Anterior surface of sacrum between anterior sacral foramina | Medial side of superior border of greater trochanter of femur | Branches from SI, and S2 | Lateral rotation of the extended hip joint; abduction of flexed hip |
The obturator internus forms a large part of the anterolateral wall of the pelvic cavity.
The piriformis is triangular and originates in the bridges of bone between the four anterior sacral foramina. It passes laterally through the greater sciatic foramen, crosses the posterosuperior aspect of the hip joint, and inserts on the greater trochanter of the femur above the insertion of the obturator internus muscle (Fig. 5.30 and Table 5.1).
Apertures in the pelvic wall
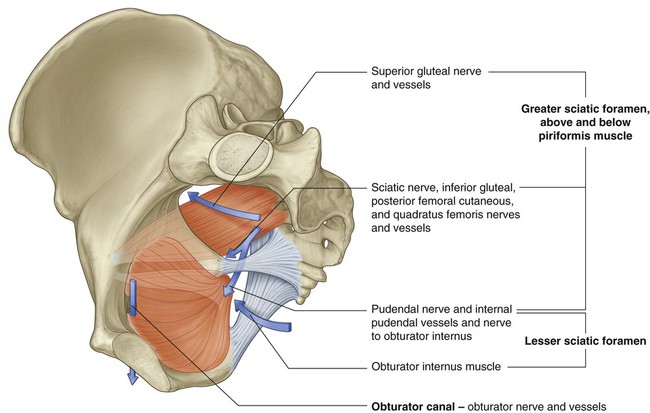
The greater sciatic foramen is a major route of communication between the pelvic cavity and the lower limb (Fig. 5.31). It is formed by the greater sciatic notch in the pelvic bone, the sacrotuberous and the sacrospinous ligaments, and the spine of the ischium.
The piriformis muscle passes through the greater sciatic foramen, dividing it into two parts.
 The superior gluteal nerves and vessels pass through the foramen above the piriformis.
The superior gluteal nerves and vessels pass through the foramen above the piriformis.
 Passing through the foramen below the piriformis are the inferior gluteal nerves and vessels, the sciatic nerve, the pudendal nerve, the internal pudendal vessels, the posterior femoral cutaneous nerves, and the nerves to the obturator internus and quadratus femoris muscles.
Passing through the foramen below the piriformis are the inferior gluteal nerves and vessels, the sciatic nerve, the pudendal nerve, the internal pudendal vessels, the posterior femoral cutaneous nerves, and the nerves to the obturator internus and quadratus femoris muscles.
Pelvic outlet
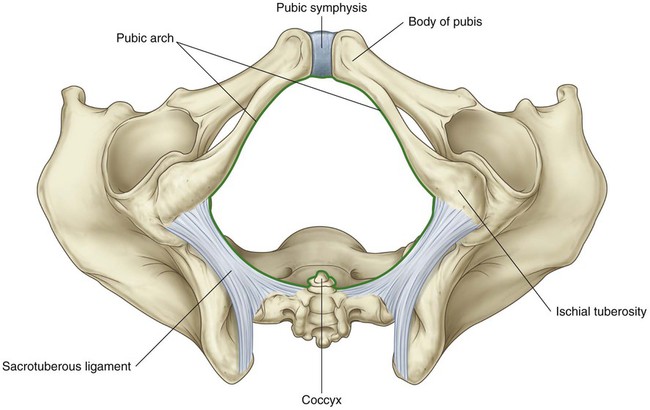
The pelvic outlet is diamond shaped, with the anterior part of the diamond defined predominantly by bone and the posterior part mainly by ligaments (Fig. 5.32). In the midline anteriorly, the boundary of the pelvic outlet is the pubic symphysis. Extending laterally and posteriorly, the boundary on each side is the inferior border of the body of the pubis, the inferior ramus of the pubis, the ramus of the ischium, and the ischial tuberosity. Together, the elements on both sides form the pubic arch.
The area enclosed by the boundaries of the pelvic outlet and below the pelvic floor is the perineum.
Pelvic floor
The pelvic diaphragm
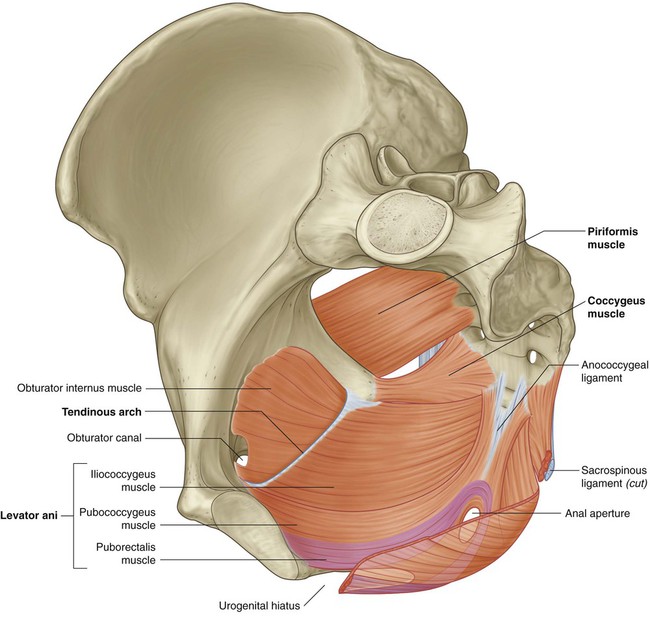
The pelvic diaphragm is the muscular part of the pelvic floor. Shaped like a bowl or funnel and attached superiorly to the pelvic walls, it consists of the levator ani and the coccygeus muscles (Fig. 5.34 and Table 5.2).
Table 5.2
Muscles of the pelvic diaphragm
| Muscle | Origin | Insertion | Innervation | Function |
| Levator ani | In a line around the pelvic wall beginning on the posterior aspect of the pubic bone and extending across the obturator internus muscle as a tendinous arch (thickening of the obturator internus fascia) to the ischial spine | The anterior part is attached to the superior surface of the perineal membrane; the posterior part meets its partner on the other side at the perineal body, around the anal canal, and along the anococcygeal ligament | Branches direct from the anterior ramus of S4, and by the inferior rectal branch of the pudendal nerve (S2 to S4) | Contributes to the formation of the pelvic floor, which supports the pelvic viscera; maintains an angle between the rectum and anal canal; reinforces the external anal sphincter and, in women, functions as a vaginal sphincter |
| Coccygeus | Ischial spine and pelvic surface of the sacrospinous ligament | Lateral margin of coccyx and related border of sacrum | Branches from the anterior rami of S3 and S4 | Contributes to the formation of the pelvic floor, which supports the pelvic viscera; pulls coccyx forward after defecation |
 the greater sciatic foramen is situated above the level of the pelvic floor and is a route of communication between the pelvic cavity and the gluteal region of the lower limb; and
the greater sciatic foramen is situated above the level of the pelvic floor and is a route of communication between the pelvic cavity and the gluteal region of the lower limb; and
 the lesser sciatic foramen is situated below the pelvic floor, providing a route of communication between the gluteal region of the lower limb and the perineum.
the lesser sciatic foramen is situated below the pelvic floor, providing a route of communication between the gluteal region of the lower limb and the perineum.
 the posterior aspect of the body of the pubic bone,
the posterior aspect of the body of the pubic bone,
 a linear thickening called the tendinous arch, in the fascia covering the obturator internus muscle, and
a linear thickening called the tendinous arch, in the fascia covering the obturator internus muscle, and
At the midline, the muscles blend together posterior to the vagina in women and around the anal aperture in both sexes. Posterior to the anal aperture, the muscles come together as a ligament or raphe called the anococcygeal ligament (anococcygeal body) and attaches to the coccyx. Anteriorly, the muscles are separated by a U-shaped defect or gap termed the urogenital hiatus. The margins of this hiatus merge with the walls of the associated viscera and with muscles in the deep perineal pouch below. The hiatus allows the urethra (in both men and women), and the vagina (in women), to pass through the pelvic diaphragm (Fig. 5.34).
 The pubococcygeus originates from the body of the pubis and courses posteriorly to attach along the midline as far back as the coccyx. This part of the muscle is further subdivided on the basis of association with structures in the midline into the puboprostaticus (levator prostatae), the pubovaginalis, and the puboanalis muscles.
The pubococcygeus originates from the body of the pubis and courses posteriorly to attach along the midline as far back as the coccyx. This part of the muscle is further subdivided on the basis of association with structures in the midline into the puboprostaticus (levator prostatae), the pubovaginalis, and the puboanalis muscles.
 A second major collection of muscle fibers, the puborectalis portion of the levator ani muscles, originates, in association with the pubococcygeus muscle, from the pubis and passes inferiorly on each side to form a sling around the terminal part of the gastrointestinal tract. This muscular sling maintains an angle or flexure, called the perineal flexure, at the anorectal junction. This angle functions as part of the mechanism that keeps the end of the gastrointestinal system closed.
A second major collection of muscle fibers, the puborectalis portion of the levator ani muscles, originates, in association with the pubococcygeus muscle, from the pubis and passes inferiorly on each side to form a sling around the terminal part of the gastrointestinal tract. This muscular sling maintains an angle or flexure, called the perineal flexure, at the anorectal junction. This angle functions as part of the mechanism that keeps the end of the gastrointestinal system closed.
 The final part of the levator ani muscle is the iliococcygeus. This part of the muscle originates from the fascia that covers the obturator internus muscle. It joins the same muscle on the other side in the midline to form a ligament or raphe that extends from the anal aperture to the coccyx.
The final part of the levator ani muscle is the iliococcygeus. This part of the muscle originates from the fascia that covers the obturator internus muscle. It joins the same muscle on the other side in the midline to form a ligament or raphe that extends from the anal aperture to the coccyx.
The two coccygeus muscles, one on each side, are triangular and overlie the sacrospinous ligaments; together they complete the posterior part of the pelvic diaphragm (Fig. 5.34 and Table 5.2). They are attached, by their apices, to the tips of the ischial spines and, by their bases, to the lateral margins of the coccyx and adjacent margins of the sacrum.
The perineal membrane and deep perineal pouch
The perineal membrane is a thick fascial, triangular structure attached to the bony framework of the pubic arch (Fig. 5.35A). It is oriented in the horizontal plane and has a free posterior margin. Anteriorly, there is a small gap (blue arrow in Fig. 5.35A) between the membrane and the inferior pubic ligament (a ligament associated with the pubic symphysis).
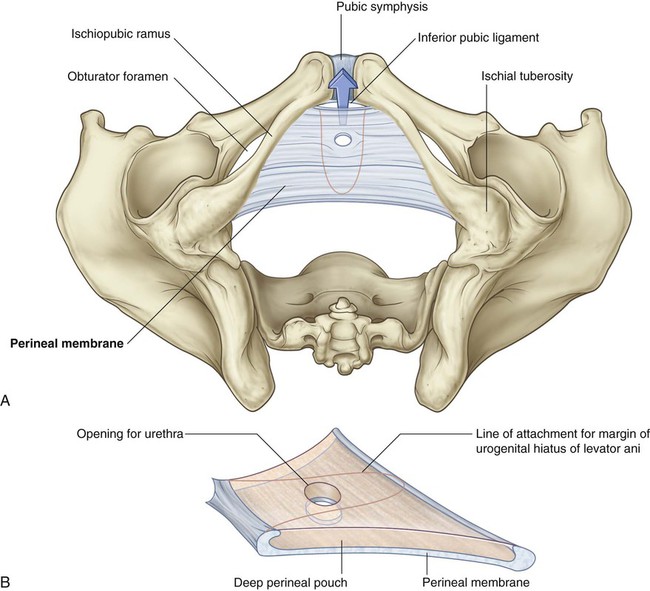
Perineal membrane and deep perineal pouch. C. Medial view.
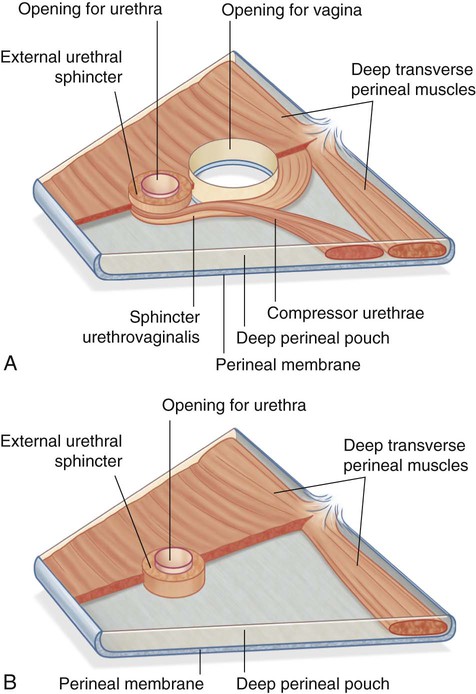
The perineal membrane is related above to a thin space called the deep perineal pouch (deep perineal space) (Fig. 5.35B), which contains a layer of skeletal muscle and various neurovascular elements.
The perineal membrane and adjacent pubic arch provide attachment for the roots of the external genitalia and the muscles associated with them (Fig. 5.35C).
Within the deep perineal pouch, a sheet of skeletal muscle functions as a sphincter, mainly for the urethra, and as a stabilizer of the posterior edge of the perineal membrane (Fig. 5.36 and Table 5.3).
Table 5.3
Muscles within the deep perineal pouch
| Muscle | Origin | Insertion | Innervation | Function |
| External urethral sphincter | From the inferior ramus of the pubis on each side and adjacent walls of the deep perineal pouch | Surrounds membranous part of urethra | Perineal branches of the pudendal nerve (S2 to S4) | Compresses the membranous urethra; relaxes during micturition |
| Deep transverse perineal | Medial aspect of ischial ramus | Perineal body | Perineal branches of the pudendal nerve (S2 to S4) | Stabilizes the position of the perineal body |
| Compressor urethrae (in women only) | Ischiopubic ramus on each side | Blends with partner on other side anterior to the urethra | Perineal branches of the pudendal nerve (S2 to S4) | Functions as an accessory sphincter of the urethra |
| Sphincter urethrovaginalis (in women only) | Perineal body | Passes forward lateral to the vagina to blend with partner on other side anterior to the urethra | Perineal branches of the pudendal nerve (S2 to S4) | Functions as an accessory sphincter of the urethra (also may facilitate closing the vagina) |
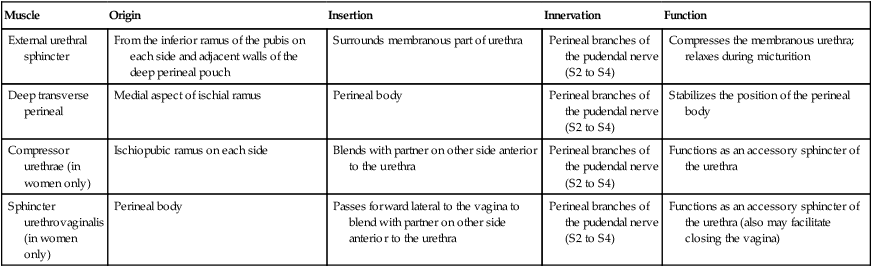
 Anteriorly, a group of muscle fibers surround the urethra and collectively form the external urethral sphincter.
Anteriorly, a group of muscle fibers surround the urethra and collectively form the external urethral sphincter.
 Two additional groups of muscle fibers are associated with the urethra and vagina in women. One group forms the sphincter urethrovaginalis, which surrounds the urethra and vagina as a unit. The second group forms the compressor urethrae, on each side, which originate from the ischiopubic rami and meet anterior to the urethra. Together with the external urethral sphincter, the sphincter urethrovaginalis and compressor urethrae facilitate closing of the urethra.
Two additional groups of muscle fibers are associated with the urethra and vagina in women. One group forms the sphincter urethrovaginalis, which surrounds the urethra and vagina as a unit. The second group forms the compressor urethrae, on each side, which originate from the ischiopubic rami and meet anterior to the urethra. Together with the external urethral sphincter, the sphincter urethrovaginalis and compressor urethrae facilitate closing of the urethra.
 In both men and women, a deep transverse perineal muscle on each side parallels the free margin of the perineal membrane and joins with its partner at the midline. These muscles are thought to stabilize the position of the perineal body, which is a midline structure along the posterior edge of the perineal membrane.
In both men and women, a deep transverse perineal muscle on each side parallels the free margin of the perineal membrane and joins with its partner at the midline. These muscles are thought to stabilize the position of the perineal body, which is a midline structure along the posterior edge of the perineal membrane.
Perineal body
The perineal body is an ill-defined but important connective tissue structure into which muscles of the pelvic floor and the perineum attach (Fig. 5.37). It is positioned in the midline along the posterior border of the perineal membrane, to which it attaches. The posterior end of the urogenital hiatus in the levator ani muscles is also connected to it.
Viscera
Gastrointestinal system
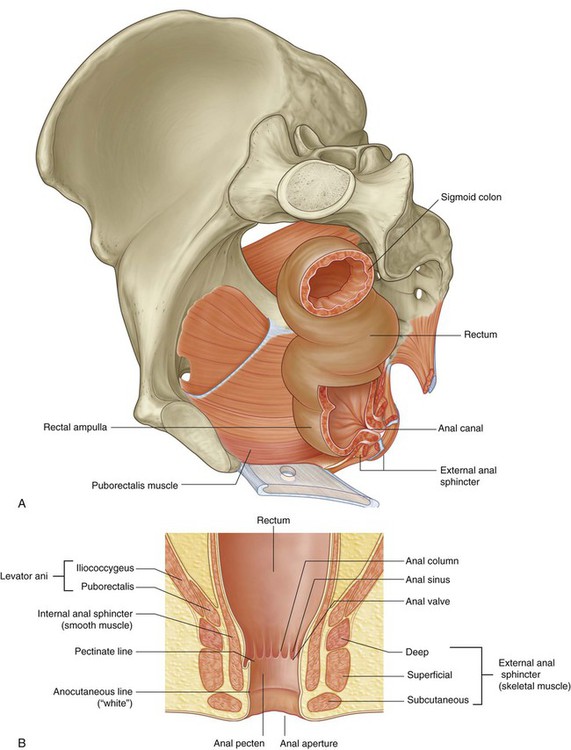
Pelvic parts of the gastrointestinal system consist mainly of the rectum and the anal canal, although the terminal part of the sigmoid colon is also in the pelvic cavity (Fig. 5.38).
Anal canal
The lining of the anal canal bears a number of characteristic structural features that reflect the approximate position of the anococcygeal membrane in the fetus (which closes the terminal end of the developing gastrointestinal system in the fetus) and the transition from gastrointestinal mucosa to skin in the adult (Fig. 5.38B).
 The upper part of the anal canal is lined by mucosa similar to that lining the rectum and is distinguished by a number of longitudinally oriented folds known as anal columns, which are united inferiorly by crescentic folds termed anal valves. Superior to each valve is a depression termed an anal sinus. The anal valves together form a circle around the anal canal at a location known as the pectinate line, which marks the approximate position of the anal membrane in the fetus.
The upper part of the anal canal is lined by mucosa similar to that lining the rectum and is distinguished by a number of longitudinally oriented folds known as anal columns, which are united inferiorly by crescentic folds termed anal valves. Superior to each valve is a depression termed an anal sinus. The anal valves together form a circle around the anal canal at a location known as the pectinate line, which marks the approximate position of the anal membrane in the fetus.
 Inferior to the pectinate line is a transition zone known as the anal pecten, which is lined by nonkeratinized stratified squamous epithelium. The anal pecten ends inferiorly at the anocutaneous line (“white line”), or where the lining of the anal canal becomes true skin.
Inferior to the pectinate line is a transition zone known as the anal pecten, which is lined by nonkeratinized stratified squamous epithelium. The anal pecten ends inferiorly at the anocutaneous line (“white line”), or where the lining of the anal canal becomes true skin.
Urinary system
The pelvic parts of the urinary system consist of the terminal parts of the ureters, the bladder, and the proximal part of the urethra (Fig. 5.39).
Bladder
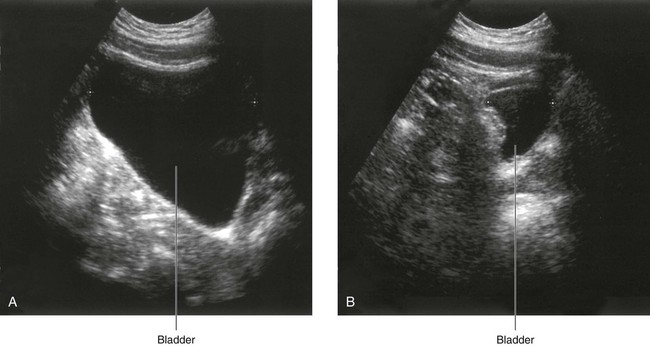
The bladder is the most anterior element of the pelvic viscera. Although it is entirely situated in the pelvic cavity when empty, it expands superiorly into the abdominal cavity when full (Fig. 5.39).
The empty bladder is shaped like a three-sided pyramid that has tipped over to lie on one of its margins (Fig. 5.40A). It has an apex, a base, a superior surface, and two inferolateral surfaces.
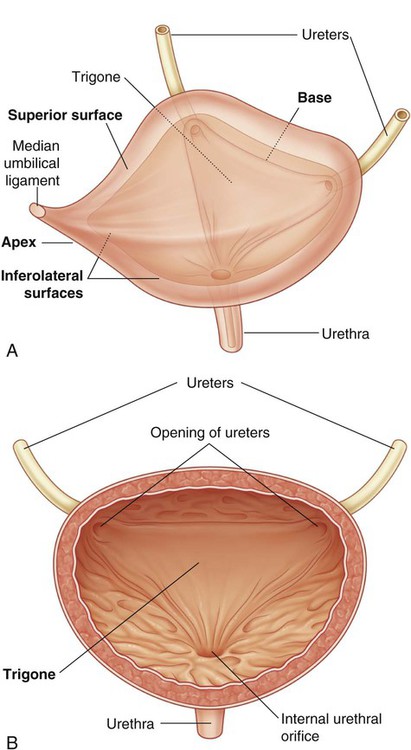
 The apex of the bladder is directed toward the top of the pubic symphysis; a structure known as the median umbilical ligament (a remnant of the embryological urachus that contributes to the formation of the bladder) continues from it superiorly up the anterior abdominal wall to the umbilicus.
The apex of the bladder is directed toward the top of the pubic symphysis; a structure known as the median umbilical ligament (a remnant of the embryological urachus that contributes to the formation of the bladder) continues from it superiorly up the anterior abdominal wall to the umbilicus.
 The base of the bladder is shaped like an inverted triangle and faces posteroinferiorly. The two ureters enter the bladder at each of the upper corners of the base, and the urethra drains inferiorly from the lower corner of the base. Inside, the mucosal lining on the base of the bladder is smooth and firmly attached to the underlying smooth muscle coat of the wall—unlike elsewhere in the bladder where the mucosa is folded and loosely attached to the wall. The smooth triangular area between the openings of the ureters and urethra on the inside of the bladder is known as the trigone (Fig. 5.40B).
The base of the bladder is shaped like an inverted triangle and faces posteroinferiorly. The two ureters enter the bladder at each of the upper corners of the base, and the urethra drains inferiorly from the lower corner of the base. Inside, the mucosal lining on the base of the bladder is smooth and firmly attached to the underlying smooth muscle coat of the wall—unlike elsewhere in the bladder where the mucosa is folded and loosely attached to the wall. The smooth triangular area between the openings of the ureters and urethra on the inside of the bladder is known as the trigone (Fig. 5.40B).
 The inferolateral surfaces of the bladder are cradled between the levator ani muscles of the pelvic diaphragm and the adjacent obturator internus muscles above the attachment of the pelvic diaphragm. The superior surface is slightly domed when the bladder is empty; it balloons upward as the bladder fills.
The inferolateral surfaces of the bladder are cradled between the levator ani muscles of the pelvic diaphragm and the adjacent obturator internus muscles above the attachment of the pelvic diaphragm. The superior surface is slightly domed when the bladder is empty; it balloons upward as the bladder fills.
 In women, these fibromuscular bands are termed pubovesical ligaments (Fig. 5.41A). Together with the perineal membrane and associated muscles, the levator ani muscles, and the pubic bones, these ligaments help support the bladder.
In women, these fibromuscular bands are termed pubovesical ligaments (Fig. 5.41A). Together with the perineal membrane and associated muscles, the levator ani muscles, and the pubic bones, these ligaments help support the bladder.
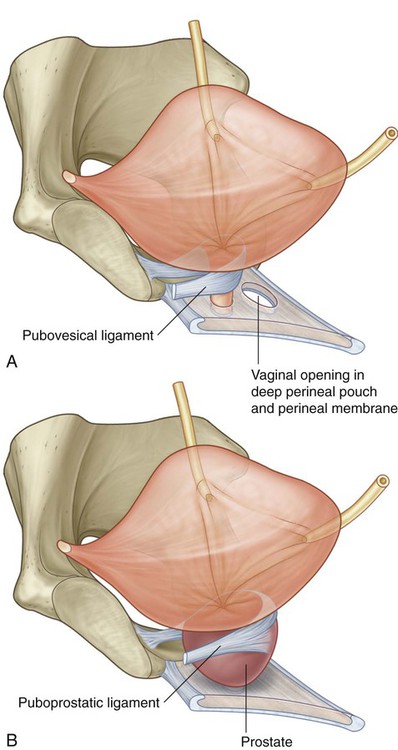
 In men, the paired fibromuscular bands are known as puboprostatic ligaments because they blend with the fibrous capsule of the prostate, which surrounds the neck of the bladder and adjacent part of the urethra (Fig. 5.41B).
In men, the paired fibromuscular bands are known as puboprostatic ligaments because they blend with the fibrous capsule of the prostate, which surrounds the neck of the bladder and adjacent part of the urethra (Fig. 5.41B).
Urethra
In women, the urethra is short, being about 4 cm long. It travels a slightly curved course as it passes inferiorly through the pelvic floor into the perineum, where it passes through the deep perineal pouch and perineal membrane before opening in the vestibule that lies between the labia minora (Fig. 5.44A).
In men, the urethra is long, about 20 cm, and bends twice along its course (Fig. 5.44B). Beginning at the base of the bladder and passing inferiorly through the prostate, it passes through the deep perineal pouch and perineal membrane and immediately enters the root of the penis. As the urethra exits the deep perineal pouch, it bends forward to course anteriorly in the root of the penis. When the penis is flaccid, the urethra makes another bend, this time inferiorly, when passing from the root to the body of the penis. During erection, the bend between the root and body of the penis disappears.
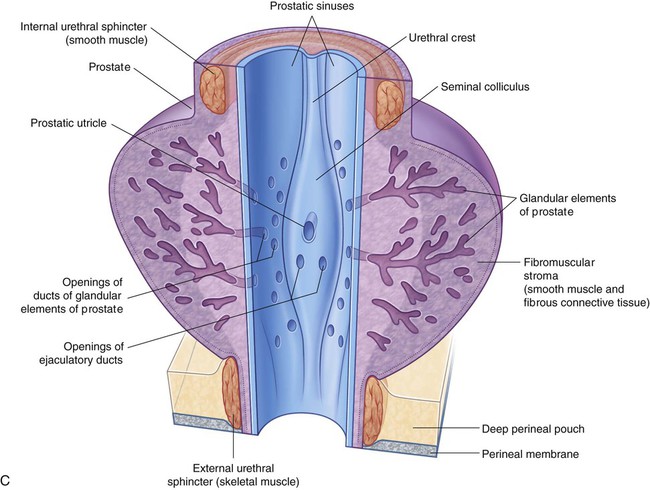
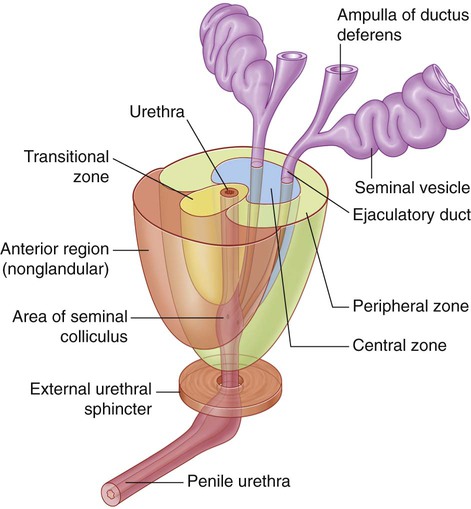
The urethra in men is divided into preprostatic, prostatic, membranous, and spongy parts.
The prostatic part of the urethra (Fig. 5.44C) is 3 to 4 cm long and is surrounded by the prostate. In this region, the lumen of the urethra is marked by a longitudinal midline fold of mucosa (the urethral crest). The depression on each side of the crest is the prostatic sinus; the ducts of the prostate empty into these two sinuses.
The spongy urethra is surrounded by erectile tissue (the corpus spongiosum) of the penis. It is enlarged to form a bulb at the base of the penis and again at the end of the penis to form the navicular fossa (Fig. 5.44B). The two bulbo-urethral glands in the deep perineal pouch are part of the male reproductive system and open into the bulb of the spongy urethra. The external urethral orifice is the sagittal slit at the end of the penis.
Reproductive system
In men
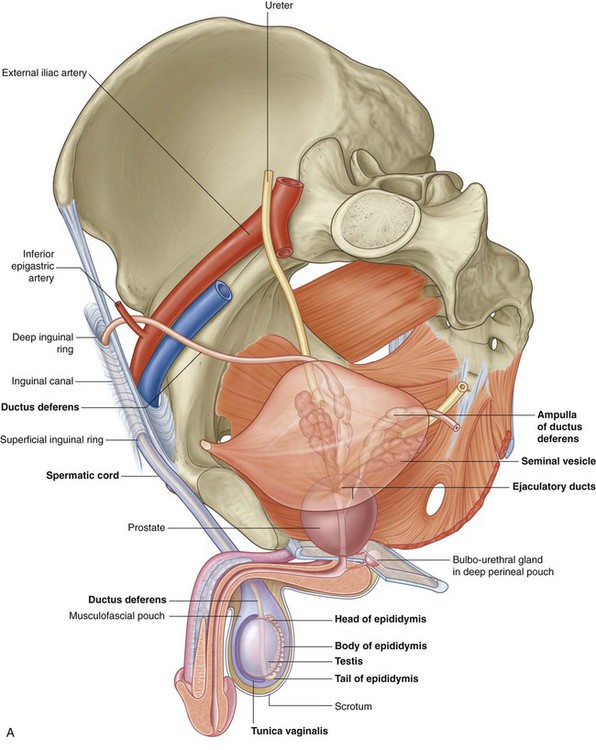
The reproductive system in men has components in the abdomen, pelvis, and perineum (Fig. 5.46A). The major components are a testis, epididymis, ductus deferens, and ejaculatory duct on each side, and the urethra and penis in the midline. In addition, three types of accessory glands are associated with the system:
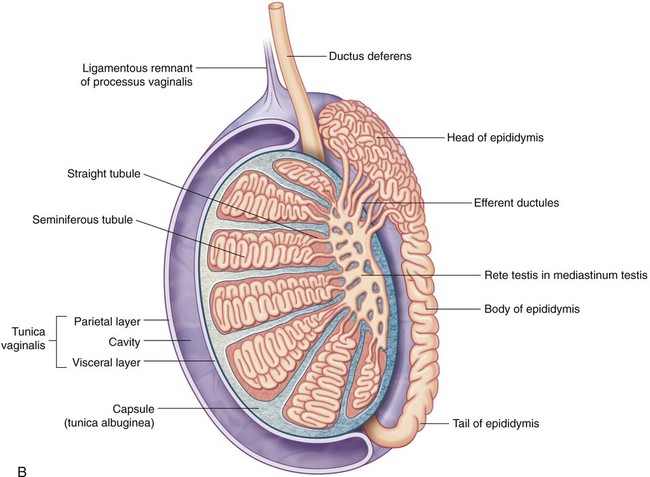
Each testis (Fig. 5.46B) is composed of seminiferous tubules and interstitial tissue surrounded by a thick connective tissue capsule (the tunica albuginea). Spermatozoa are produced by the seminiferous tubules. The 400 to 600 highly coiled seminiferous tubules are modified at each end to become straight tubules, which connect to a collecting chamber (the rete testis) in a thick, vertically oriented linear wedge of connective tissue (the mediastinum testis), projecting from the capsule into the posterior aspect of the gonad. Approximately 12 to 20 efferent ductules originate from the upper end of the rete testis, penetrate the capsule, and connect with the epididymis.
The epididymis courses along the posterolateral side of the testis (Fig. 5.46B). It has two distinct components:
 the efferent ductules, which form an enlarged coiled mass that sits on the posterior superior pole of the testis and forms the head of the epididymis; and
the efferent ductules, which form an enlarged coiled mass that sits on the posterior superior pole of the testis and forms the head of the epididymis; and
 the true epididymis, which is a single, long coiled duct into which the efferent ductules all drain, and which continues inferiorly along the posterolateral margin of the testis as the body of the epididymis and enlarges to form the tail of the epididymis at the inferior pole of the testis.
the true epididymis, which is a single, long coiled duct into which the efferent ductules all drain, and which continues inferiorly along the posterolateral margin of the testis as the body of the epididymis and enlarges to form the tail of the epididymis at the inferior pole of the testis.
The ductus deferens is a long muscular duct that transports spermatozoa from the tail of the epididymis in the scrotum to the ejaculatory duct in the pelvic cavity (Fig. 5.46A). It ascends in the scrotum as a component of the spermatic cord and passes through the inguinal canal in the anterior abdominal wall.
Each seminal vesicle is an accessory gland of the male reproductive system that develops as a blind-ended tubular outgrowth from the ductus deferens (Fig. 5.46A). The tube is coiled with numerous pocket-like outgrowths and is encapsulated by connective tissue to form an elongate structure situated between the bladder and rectum. The gland is immediately lateral to and follows the course of the ductus deferens at the base of the bladder.
The duct of the seminal vesicle joins the ductus deferens to form the ejaculatory duct (Fig. 5.47). Secretions from the seminal vesicle contribute significantly to the volume of the ejaculate (semen).
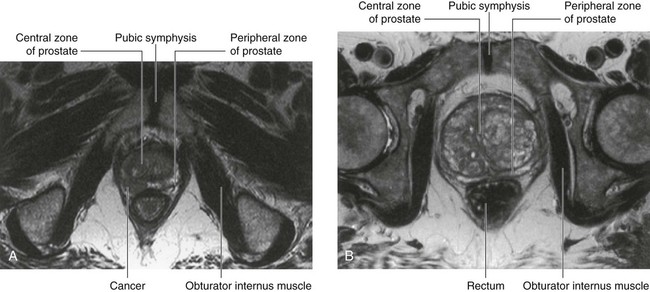
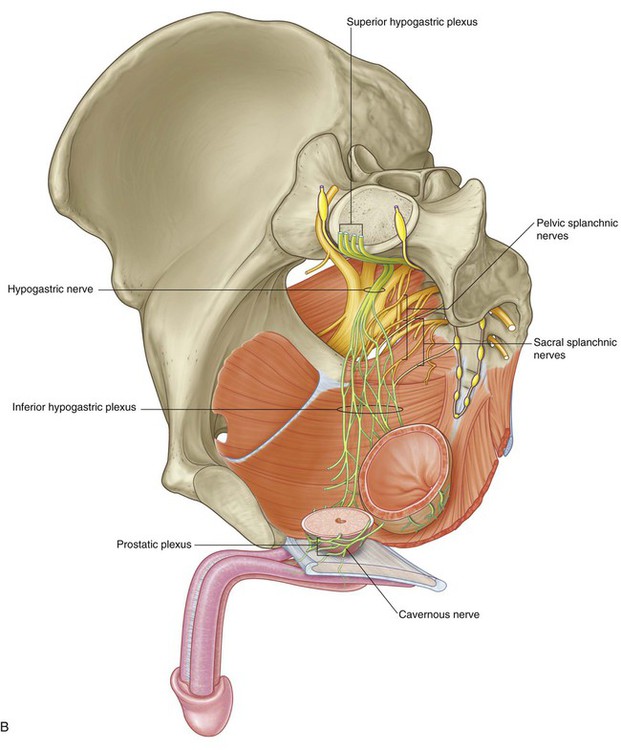
The prostate is an unpaired accessory structure of the male reproductive system that surrounds the urethra in the pelvic cavity (Figs. 5.46A and 5.47). It lies immediately inferior to the bladder, posterior to the pubic symphysis, and anterior to the rectum.
The prostate develops as 30 to 40 individual complex glands, which grow from the urethral epithelium into the surrounding wall of the urethra. Collectively, these glands enlarge the wall of the urethra into what is known as the prostate; however, the individual glands retain their own ducts, which empty independently into the prostatic sinuses on the posterior aspect of the urethral lumen (see Fig. 5.44C).
The bulbo-urethral glands (see Fig. 5.46A), one on each side, are small, pea-shaped mucous glands situated within the deep perineal pouch. They are lateral to the membranous part of the urethra. The duct from each gland passes inferomedially through the perineal membrane, to open into the bulb of the spongy urethra at the root of the penis.
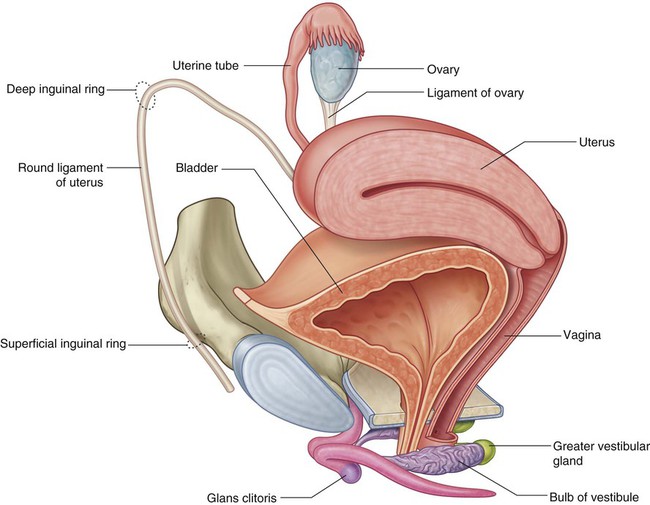
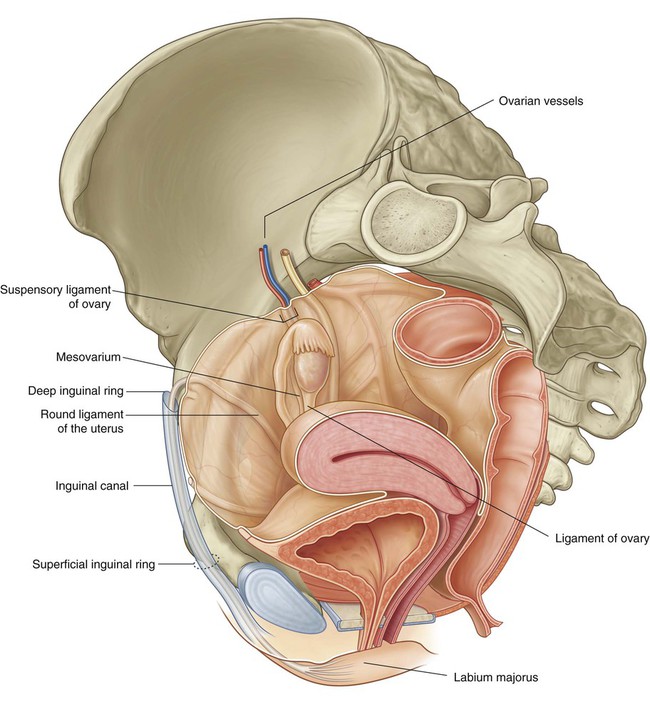
In women
Like the testes in men, the ovaries develop high on the posterior abdominal wall and then descend before birth, bringing with them their vessels, lymphatics, and nerves. Unlike the testes, the ovaries do not migrate through the inguinal canal into the perineum, but stop short and assume a position on the lateral wall of the pelvic cavity (Fig. 5.50).
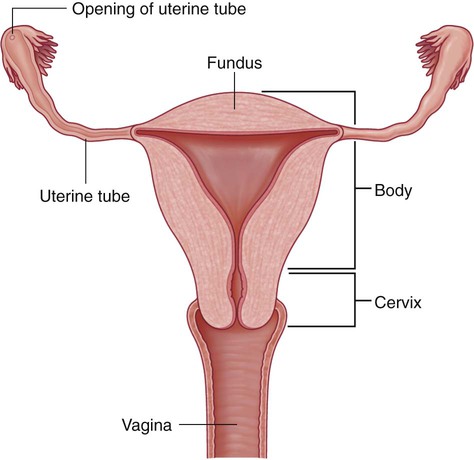
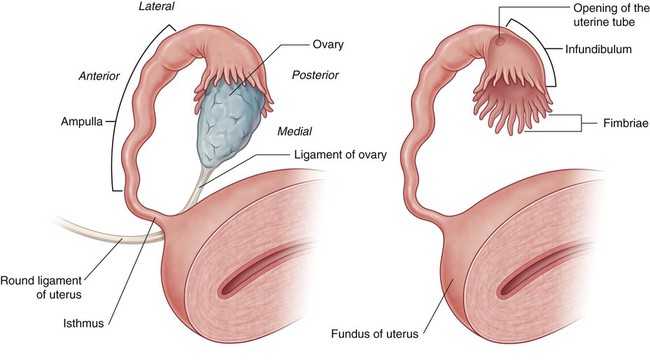
The uterus is a thick-walled muscular organ in the midline between the bladder and rectum (see Fig. 5.50). It consists of a body and a cervix, and inferiorly it joins the vagina (Fig. 5.52). Superiorly, uterine tubes project laterally from the uterus and open into the peritoneal cavity immediately adjacent to the ovaries.
The body of the uterus is flattened anteroposteriorly and, above the level of origin of the uterine tubes (Fig. 5.52), has a rounded superior end (fundus of the uterus). The cavity of the body of the uterus is a narrow slit, when viewed laterally, and is shaped like an inverted triangle, when viewed anteriorly. Each of the superior corners of the cavity is continuous with the lumen of a uterine tube; the inferior corner is continuous with the central canal of the cervix.
The uterine tubes extend from each side of the superior end of the body of the uterus to the lateral pelvic wall and are enclosed within the upper margins of the mesosalpinx portions of the broad ligaments (see p. 483). Because the ovaries are suspended from the posterior aspect of the broad ligaments, the uterine tubes pass superiorly over, and terminate laterally to, the ovaries.
Each uterine tube has an expanded trumpet-shaped end (the infundibulum), which curves around the superolateral pole of the related ovary (Fig. 5.53). The margin of the infundibulum is rimmed with small finger-like projections termed fimbriae. The lumen of the uterine tube opens into the peritoneal cavity at the narrowed end of the infundibulum. Medial to the infundibulum, the tube expands to form the ampulla and then narrows to form the isthmus, before joining with the body of the uterus.
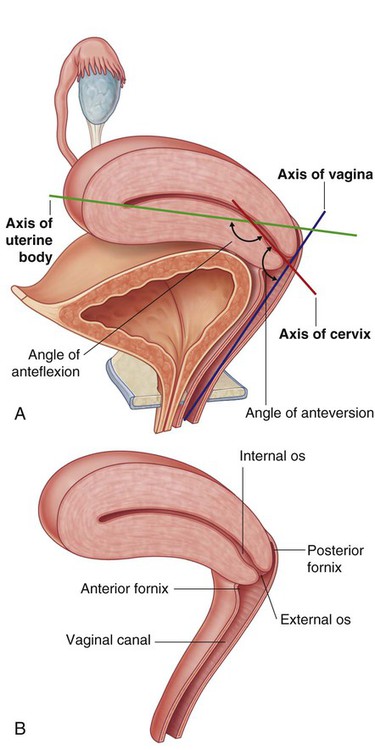
The cervix forms the inferior part of the uterus and is shaped like a short, broad cylinder with a narrow central channel. The body of the uterus normally arches forward (anteflexed on the cervix) over the superior surface of the emptied bladder (Fig. 5.54A). In addition, the cervix is angled forward (anteverted) on the vagina so that the inferior end of the cervix projects into the upper anterior aspect of the vagina. Because the end of the cervix is dome shaped, it bulges into the vagina, and a gutter, or fornix, is formed around the margin of the cervix where it joins the vaginal wall (Fig. 5.54B). The tubular central canal of the cervix opens, below, as the external os, into the vaginal cavity and, above, as the internal os, into the uterine cavity.
The vagina is the copulatory organ in women. It is a distensible fibromuscular tube that extends from the perineum through the pelvic floor and into the pelvic cavity (Fig. 5.56A). The internal end of the canal is enlarged to form a region called the vaginal vault.
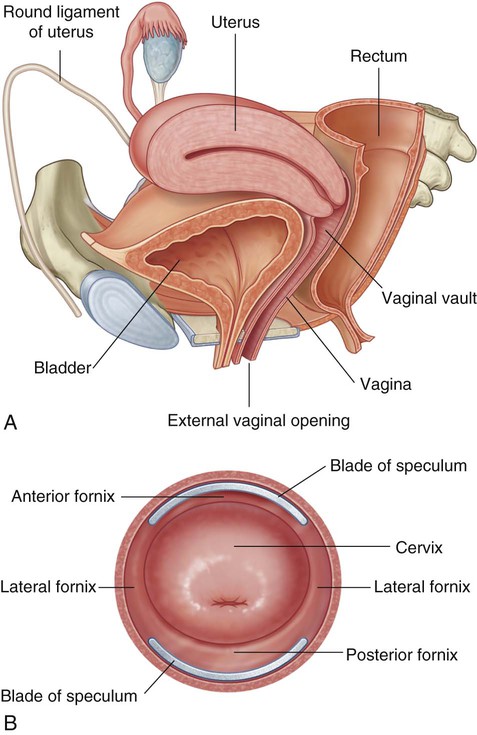
Posteriorly, the vagina is related principally to the rectum.
The vaginal fornix is the recess formed between the margin of the cervix and the vaginal wall. Based on position, the fornix is subdivided into a posterior fornix, an anterior fornix, and two lateral fornices (Fig. 5.56A and see Fig. 5.54).
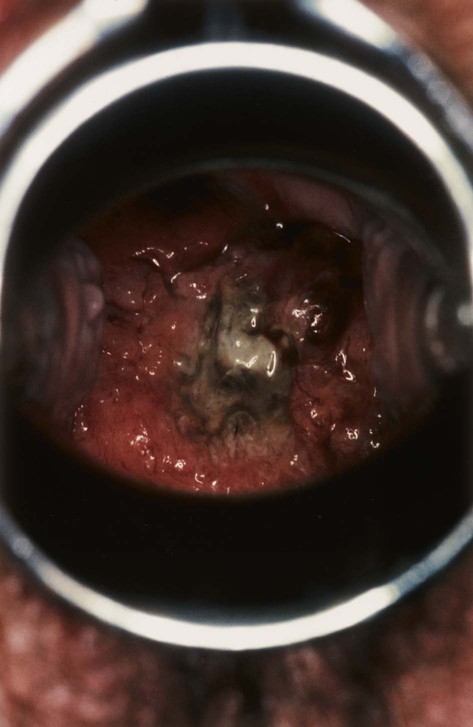
The vaginal canal is normally collapsed so that the anterior wall is in contact with the posterior wall. By using a speculum to open the vaginal canal, a physician can see the domed inferior end of the cervix, the vaginal fornices, and the external os of the cervical canal in a patient (Fig. 5.56B).
Fascia
In women
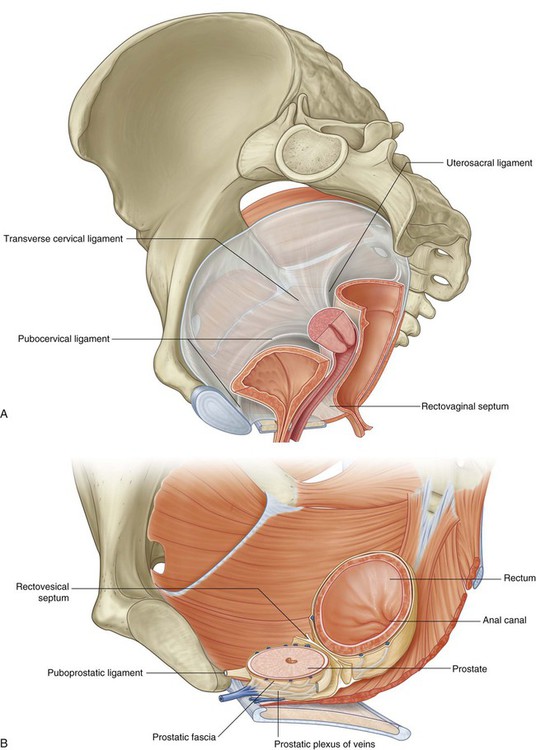
In women, a rectovaginal septum separates the posterior surface of the vagina from the rectum (Fig. 5.57A). Condensations of fascia form ligaments that extend from the cervix to the anterior (pubocervical ligament), lateral (transverse cervical or cardinal ligament), and posterior (uterosacral ligament) pelvic walls (Fig. 5.57A). These ligaments, together with the perineal membrane, the levator ani muscles, and the perineal body, are thought to stabilize the uterus in the pelvic cavity. The most important of these ligaments are the transverse cervical or cardinal ligaments, which extend laterally from each side of the cervix and vaginal vault to the related pelvic wall.
In men
In men, a condensation of fascia around the anterior and lateral region of the prostate (prostatic fascia) contains and surrounds the prostatic plexus of veins and is continuous posteriorly with the rectovesical septum, which separates the posterior surface of the prostate and base of the bladder from the rectum (Fig. 5.57B).
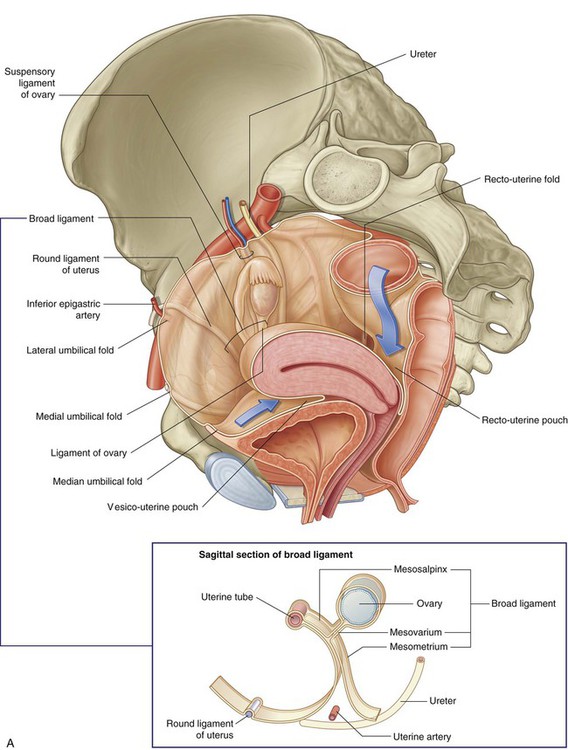
Peritoneum
Anteriorly, median and medial umbilical folds of peritoneum cover the embryological remnants of the urachus and umbilical arteries, respectively (Fig. 5.58). These folds ascend out of the pelvis and onto the anterior abdominal wall. Posteriorly, peritoneum drapes over the anterior and lateral aspects of the upper third of the rectum, but only the anterior surface of the middle third of the rectum is covered by peritoneum; the lower third of the rectum is not covered at all.
In women
In women, the uterus lies between the bladder and rectum, and the uterine tubes extend from the superior aspect of the uterus to the lateral pelvic walls (Fig. 5.58A). As a consequence, a shallow vesico-uterine pouch occurs anteriorly, between the bladder and uterus, and a deep recto-uterine pouch (pouch of Douglas) occurs posteriorly, between the uterus and rectum. In addition, a large fold of peritoneum (the broad ligament), with a uterine tube enclosed in its superior margin and an ovary attached posteriorly, is located on each side of the uterus and extends to the lateral pelvic walls.
Broad ligament
The broad ligament is a sheet-like fold of peritoneum, oriented in the coronal plane that runs from the lateral pelvic wall to the uterus, and encloses the uterine tube in its superior margin and suspends the ovary from its posterior aspect (Fig. 5.58A). The uterine arteries cross the ureters at the base of the broad ligaments, and the ligament of the ovary and round ligament of the uterus are enclosed within the parts of the broad ligament related to the ovary and uterus, respectively. The broad ligament has three parts:
 the mesometrium, the largest part of the broad ligament, which extends from the lateral pelvic walls to the body of the uterus;
the mesometrium, the largest part of the broad ligament, which extends from the lateral pelvic walls to the body of the uterus;
 the mesosalpinx, the most superior part of the broad ligament, which suspends the uterine tube in the pelvic cavity; and
the mesosalpinx, the most superior part of the broad ligament, which suspends the uterine tube in the pelvic cavity; and
 the mesovarium, a posterior extension of the broad ligament, which attaches to the ovary.
the mesovarium, a posterior extension of the broad ligament, which attaches to the ovary.
The inferior pole of the ovary is attached to a fibromuscular band of tissue (the ligament of the ovary), which courses medially in the margin of the mesovarium to the uterus and then continues anterolaterally as the round ligament of the uterus (Fig. 5.58A). The round ligament of the uterus passes over the pelvic inlet to reach the deep inguinal ring and then courses through the inguinal canal to end in connective tissue related to the labium majus in the perineum. Both the ligament of the ovary and the round ligament of the uterus are remnants of the gubernaculum, which attaches the gonad to the labioscrotal swellings in the embryo.
Nerves
Somatic plexuses
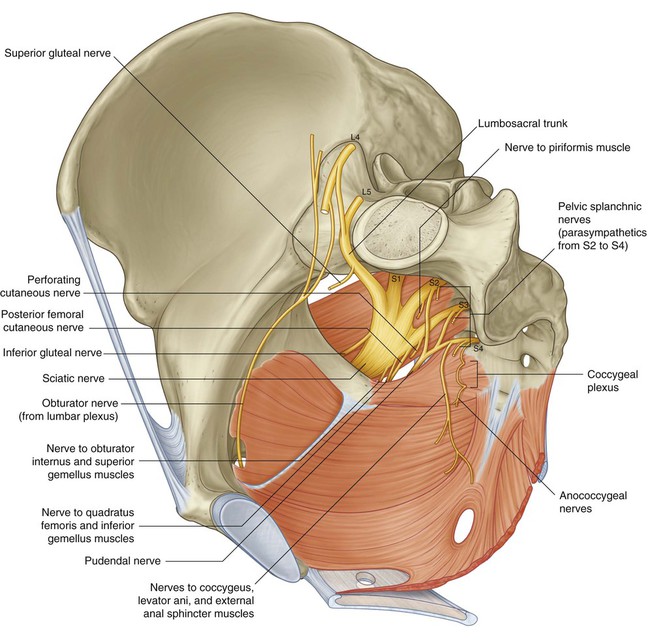
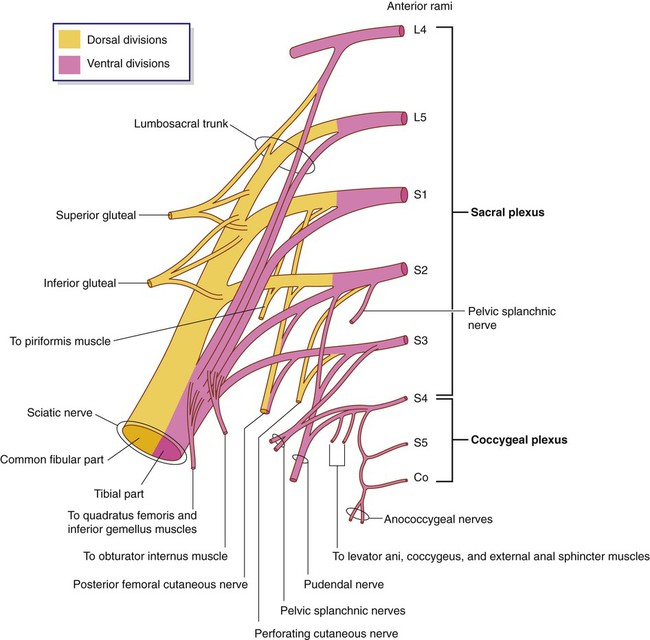
Sacral and coccygeal plexuses
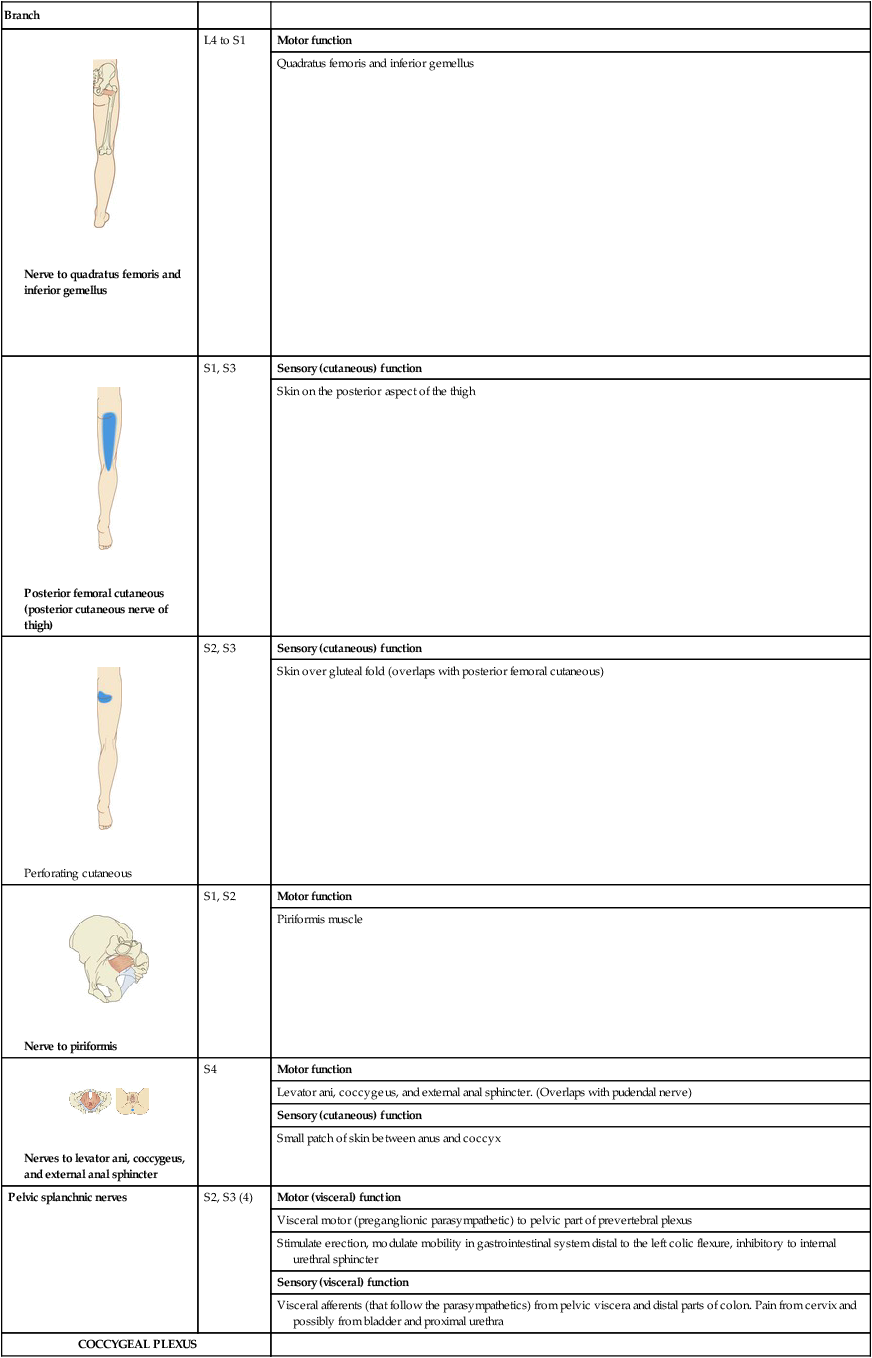
The sacral and coccygeal plexuses are situated on the posterolateral wall of the pelvic cavity and generally occur in the plane between the muscles and blood vessels. They are formed by the ventral rami of S1 to Co, with a significant contribution from L4 and L5, which enter the pelvis from the lumbar plexus (Fig. 5.59). Nerves from these mainly somatic plexuses contribute to the innervation of the lower limb and muscles of the pelvis and perineum. Cutaneous branches supply skin over the medial side of the foot, the posterior aspect of the lower limb, and most of the perineum.
The sacral plexus on each side is formed by the anterior rami of S1 to S4, and the lumbosacral trunk (L4 and L5) (Fig. 5.60). The plexus is formed in relation to the anterior surface of the piriformis muscle, which is part of the posterolateral pelvic wall. Sacral contributions to the plexus pass out of the anterior sacral foramina and course laterally and inferiorly on the pelvic wall. The lumbosacral trunk, consisting of part of the anterior ramus of L4 and all of the anterior ramus of L5, courses vertically into the pelvic cavity from the abdomen by passing immediately anterior to the sacro-iliac joint.
Gray rami communicantes from ganglia of the sympathetic trunk connect with each of the anterior rami and carry postganglionic sympathetic fibers destined for the periphery to the somatic nerves (Fig. 5.61). In addition, special visceral nerves (pelvic splanchnic nerves) originating from S2 to S4 deliver preganglionic parasympathetic fibers to the pelvic part of the prevertebral plexus (Figs. 5.59 and 5.60).
Each anterior ramus has ventral and dorsal divisions that combine with similar divisions from other levels to form terminal nerves (Fig. 5.60). The anterior ramus of S4 has only a ventral division.
Branches of the sacral plexus include the sciatic nerve and gluteal nerves, which are major nerves of the lower limb, and the pudendal nerve, which is the nerve of the perineum (Table 5.4). Numerous smaller branches supply the pelvic wall, floor, and lower limb.
Table 5.4
Branches of the sacral and coccygeal plexuses (spinal segments in parentheses do not consistently participate)
| Branch | ||
| SACRAL PLEXUS | ||
| Sciatic | Spinal segments | Motor function |
 Tibial part |
L4 to S3 | All muscles in the posterior or hamstring compartment of the thigh (including the hamstring part of the adductor magnus) except for the short head of the biceps |
| All muscles in the posterior compartment of the leg | ||
| All muscles in the sole of the foot | ||
| Sensory (cutaneous) function | ||
| Skin on posterolateral and lateral surfaces of foot and sole of foot | ||
 Common fibular part |
L4 to S2 | Motor function |
| Short head of biceps in the posterior compartment of the thigh | ||
| All muscles in the anterior and lateral compartments of the leg | ||
| Extensor digitorum brevis in the foot (also contributes to the supply of the first dorsal interosseous muscle) | ||
| Sensory (cutaneous) function | ||
| Skin on the anterolateral surface of the leg and dorsal surface of the foot | ||
 Pudendal |
S2 to S4 | Motor function |
| Skeletal muscles in the perineum including the external urethral and anal sphincters and levator ani (overlaps in supply of the levator ani and external sphincter with branches directly from ventral division of S4) | ||
| Sensory (cutaneous) function | ||
| Most skin of the perineum. Penis and clitoris | ||
 Superior gluteal |
L4 to S1 | Motor function |
| Gluteus medius, gluteus minimus, and tensor fasciae latae | ||
 Inferior gluteal |
L5 to S2 | Motor function |
| Gluteus maximus | ||
 Nerve to obturator internus and superior gemellus |
L5 to S2 | Motor function |
| Obturator internus and superior gemellus | ||
 Nerve to quadratus femoris and inferior gemellus |
L4 to S1 | Motor function |
| Quadratus femoris and inferior gemellus | ||
 Posterior femoral cutaneous (posterior cutaneous nerve of thigh) |
S1, S3 | Sensory (cutaneous) function |
| Skin on the posterior aspect of the thigh | ||
 Perforating cutaneous |
S2, S3 | Sensory (cutaneous) function |
| Skin over gluteal fold (overlaps with posterior femoral cutaneous) | ||
 Nerve to piriformis |
S1, S2 | Motor function |
| Piriformis muscle | ||
 Nerves to levator ani, coccygeus, and external anal sphincter |
S4 | Motor function |
| Levator ani, coccygeus, and external anal sphincter. (Overlaps with pudendal nerve) | ||
| Sensory (cutaneous) function | ||
| Small patch of skin between anus and coccyx | ||
| Pelvic splanchnic nerves | S2, S3 (4) | Motor (visceral) function |
| Visceral motor (preganglionic parasympathetic) to pelvic part of prevertebral plexus | ||
| Stimulate erection, modulate mobility in gastrointestinal system distal to the left colic flexure, inhibitory to internal urethral sphincter | ||
| Sensory (visceral) function | ||
| Visceral afferents (that follow the parasympathetics) from pelvic viscera and distal parts of colon. Pain from cervix and possibly from bladder and proximal urethra | ||
| COCCYGEAL PLEXUS | ||
 Anococcygeal nerves |
S4 to Co | Sensory (cutaneous) function |
| Perianal skin | ||
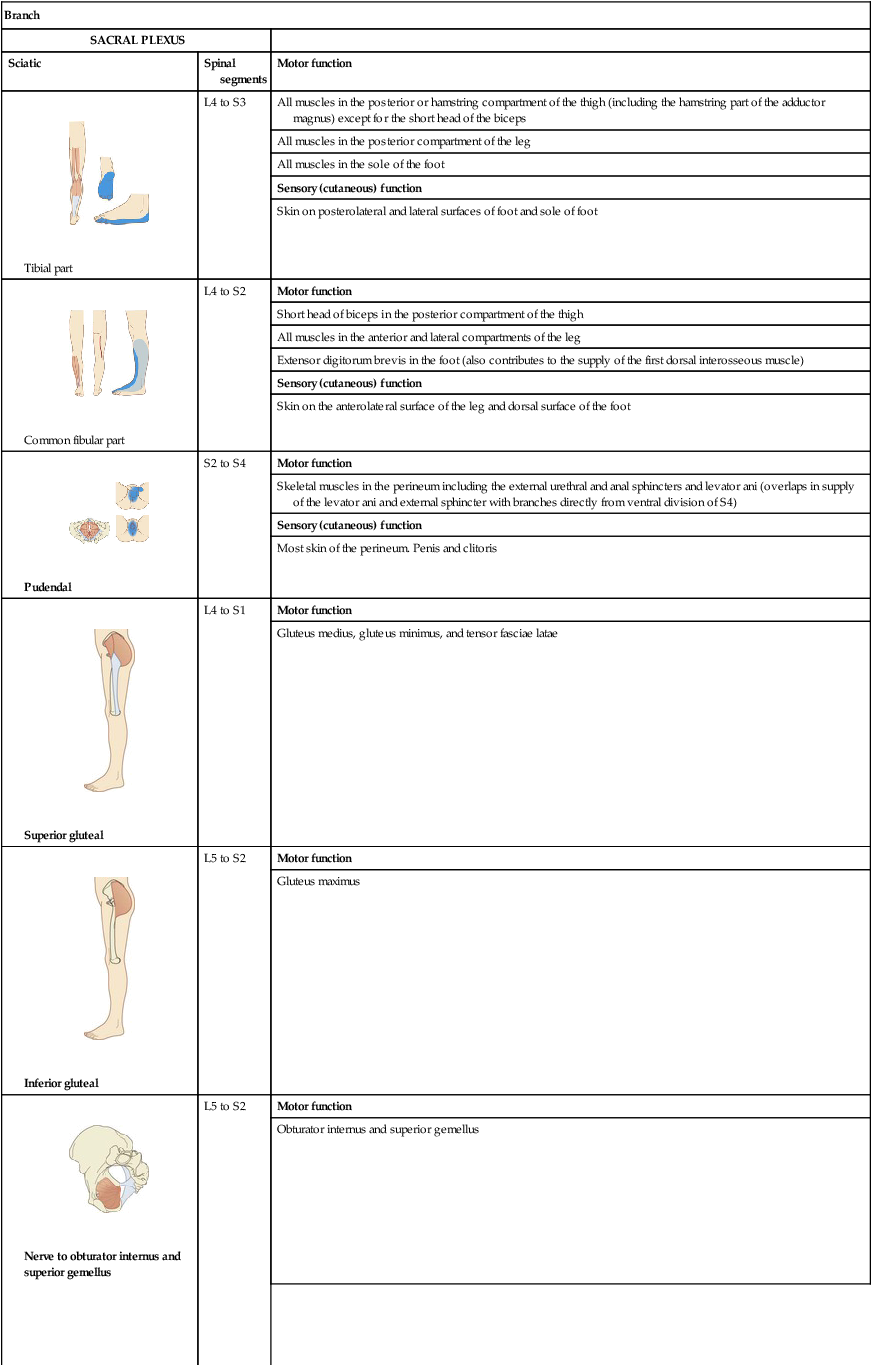
The sciatic nerve is the largest nerve of the body and carries contributions from L4 to S3 (Figs. 5.59 and 5.60). It:
 forms on the anterior surface of the piriformis muscle and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis;
forms on the anterior surface of the piriformis muscle and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis;
 passes through the gluteal region into the thigh, where it divides into its two major branches, the common fibular nerve (common peroneal nerve) and the tibial nerve—dorsal divisions of L4, L5, S1, and S2 are carried in the common fibular part of the nerve and the ventral divisions of L4, L5, S1, S2, and S3 are carried in the tibial part;
passes through the gluteal region into the thigh, where it divides into its two major branches, the common fibular nerve (common peroneal nerve) and the tibial nerve—dorsal divisions of L4, L5, S1, and S2 are carried in the common fibular part of the nerve and the ventral divisions of L4, L5, S1, S2, and S3 are carried in the tibial part;
 innervates muscles in the posterior compartment of the thigh and muscles in the leg and foot; and
innervates muscles in the posterior compartment of the thigh and muscles in the leg and foot; and
 carries sensory fibers from the skin of the foot and lateral leg.
carries sensory fibers from the skin of the foot and lateral leg.
The pudendal nerve forms anteriorly to the lower part of the piriformis muscle from ventral divisions of S2 to S4 (Figs. 5.59 and 5.60). It:
 leaves the pelvic cavity through the greater sciatic foramen, inferior to the piriformis muscle, and enters the gluteal region;
leaves the pelvic cavity through the greater sciatic foramen, inferior to the piriformis muscle, and enters the gluteal region;
 courses into the perineum by immediately passing around the sacrospinous ligament, where the ligament joins the ischial spine, and through the lesser sciatic foramen (this course takes the nerve out of the pelvic cavity, around the peripheral attachment of the pelvic floor, and into the perineum);
courses into the perineum by immediately passing around the sacrospinous ligament, where the ligament joins the ischial spine, and through the lesser sciatic foramen (this course takes the nerve out of the pelvic cavity, around the peripheral attachment of the pelvic floor, and into the perineum);
 is accompanied throughout its course by the internal pudendal vessels; and
is accompanied throughout its course by the internal pudendal vessels; and
 innervates skin and skeletal muscles of the perineum, including the external anal and external urethral sphincters.
innervates skin and skeletal muscles of the perineum, including the external anal and external urethral sphincters.
Other branches of the sacral plexus.
Other branches of the sacral plexus include:
 motor branches to muscles of the gluteal region, pelvic wall, and pelvic floor (superior and inferior gluteal nerves, nerve to obturator internus and superior gemellus, nerve to quadratus femoris and inferior gemellus, nerve to piriformis, nerves to levator ani); and
motor branches to muscles of the gluteal region, pelvic wall, and pelvic floor (superior and inferior gluteal nerves, nerve to obturator internus and superior gemellus, nerve to quadratus femoris and inferior gemellus, nerve to piriformis, nerves to levator ani); and
 sensory nerves to skin over the inferior gluteal region and posterior aspects of the thigh and upper leg (perforating cutaneous nerve and posterior cutaneous nerve of the thigh) (Figs. 5.59 and 5.60).
sensory nerves to skin over the inferior gluteal region and posterior aspects of the thigh and upper leg (perforating cutaneous nerve and posterior cutaneous nerve of the thigh) (Figs. 5.59 and 5.60).
Both superior and inferior gluteal nerves are accompanied by corresponding arteries.
The small coccygeal plexus has a minor contribution from S4 and is formed mainly by the anterior rami of S5 and Co, which originate inferiorly to the pelvic floor. They penetrate the coccygeus muscle to enter the pelvic cavity and join with the anterior ramus of S4 to form a single trunk, from which small anococcygeal nerves originate (Table 5.4). These nerves penetrate the muscle and the overlying sacrospinous and sacrotuberous ligaments and pass superficially to innervate skin in the anal triangle of the perineum.
Visceral plexuses
Paravertebral sympathetic chain
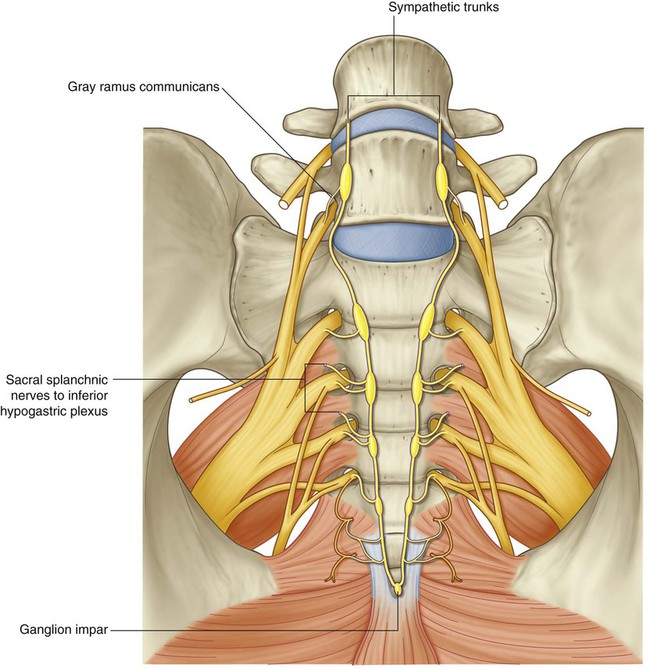
The paravertebral part of the visceral nervous system is represented in the pelvis by the inferior ends of the sympathetic trunks (Fig. 5.62A). Each trunk enters the pelvic cavity from the abdomen by passing over the ala of the sacrum medially to the lumbosacral trunks and posteriorly to the iliac vessels. The trunks course inferiorly along the anterior surface of the sacrum, where they are positioned medially to the anterior sacral foramina. Four ganglia occur along each trunk. Anteriorly to the coccyx, the two trunks join to form a single small terminal ganglion (the ganglion impar).
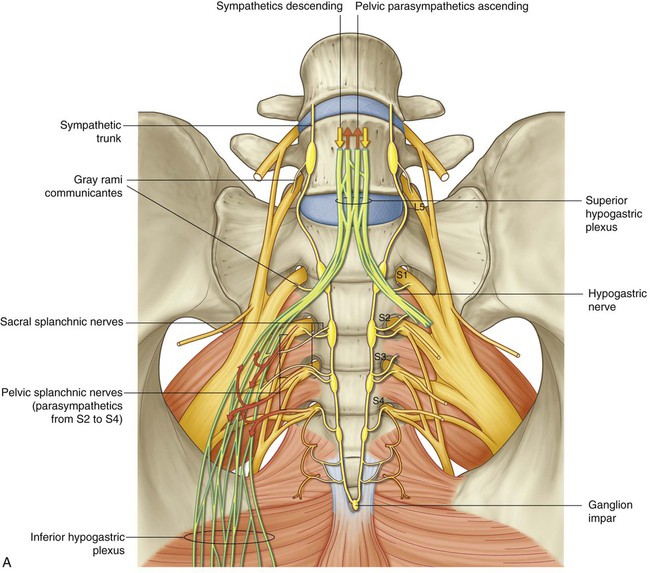
In addition to gray rami communicantes, other branches (the sacral splanchnic nerves) join and contribute to the pelvic part of the prevertebral plexus associated with innervating pelvic viscera (Fig. 5.62A).
Pelvic extensions of the prevertebral plexus
The pelvic parts of the prevertebral plexus carry sympathetic, parasympathetic, and visceral afferent fibers (Fig. 5.62A). Pelvic parts of the plexus are associated with innervating pelvic viscera and erectile tissues of the perineum.
The prevertebral plexus enters the pelvis as two hypogastric nerves, one on each side, that cross the pelvic inlet medially to the internal iliac vessels (Fig. 5.62A). The hypogastric nerves are formed by the separation of the fibers in the superior hypogastric plexus, into right and left bundles. The superior hypogastric plexus is situated anterior to vertebra LV between the promontory of the sacrum and the bifurcation of the aorta.
When the hypogastric nerves are joined by pelvic splanchnic nerves carrying preganglionic parasympathetic fibers from S2 to S4, the pelvic plexuses (inferior hypogastric plexuses) are formed (Fig. 5.62). The inferior hypogastric plexuses, one on each side, course in an inferior direction around the pelvic walls, medially to major vessels and somatic nerves. They give origin to the following subsidiary plexuses, which innervate the pelvic viscera:
Terminal branches of the inferior hypogastric plexuses penetrate and pass through the deep perineal pouch and innervate erectile tissues of the penis and the clitoris in the perineum (Fig. 5.62B). In men, these nerves, called cavernous nerves, are extensions of the prostatic plexus. The pattern of distribution of similar nerves in women is not entirely clear, but they are likely extensions of the uterovaginal plexus.
Sympathetic fibers enter the inferior hypogastric plexuses from the hypogastric nerves and from branches (sacral splanchnic nerves) of the upper sacral parts of the sympathetic trunks (Fig. 5.62A). Ultimately, these nerves are derived from preganglionic fibers that leave the spinal cord in the anterior roots, mainly of T10 to L2. These fibers:
 cause contraction of smooth muscle in the internal urethral sphincter in men and the internal anal sphincters in both men and women,
cause contraction of smooth muscle in the internal urethral sphincter in men and the internal anal sphincters in both men and women,
 cause smooth muscle contraction associated with the reproductive tract and with the accessory glands of the reproductive system, and
cause smooth muscle contraction associated with the reproductive tract and with the accessory glands of the reproductive system, and
 are important in moving secretions from the epididymis and associated glands into the urethra to form semen during ejaculation.
are important in moving secretions from the epididymis and associated glands into the urethra to form semen during ejaculation.
Parasympathetic fibers enter the pelvic plexus in pelvic splanchnic nerves that originate from spinal cord levels S2 to S4 (Fig. 5.62A). They:
 stimulate bladder contraction,
stimulate bladder contraction,
 modulate activity of the enteric nervous system of the colon distal to the left colic flexure (in addition to pelvic viscera, some of the fibers from the pelvic plexus course superiorly in the prevertebral plexus, or as separate nerves, and pass into the inferior mesenteric plexus of the abdomen).
modulate activity of the enteric nervous system of the colon distal to the left colic flexure (in addition to pelvic viscera, some of the fibers from the pelvic plexus course superiorly in the prevertebral plexus, or as separate nerves, and pass into the inferior mesenteric plexus of the abdomen).
Blood vessels
Arteries
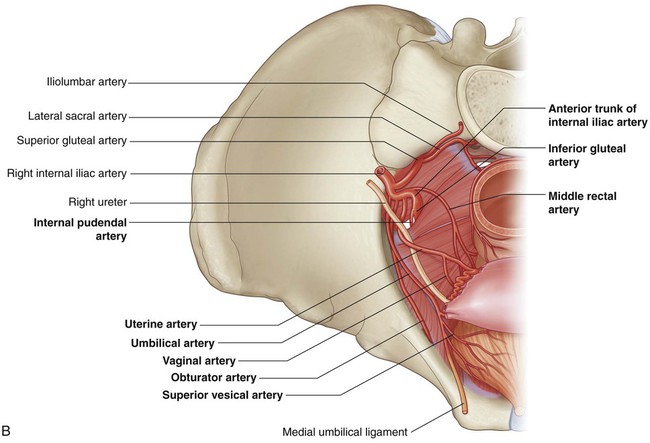
The major artery of the pelvis and perineum is the internal iliac artery on each side (Fig. 5.63). In addition to providing a blood supply to most of the pelvic viscera, pelvic walls and floor, and structures in the perineum, including erectile tissues of the clitoris and the penis, this artery gives rise to branches that follow nerves into the gluteal region of the lower limb. Other vessels that originate in the abdomen and contribute to the supply of pelvic structures include the median sacral artery and, in women, the ovarian arteries.
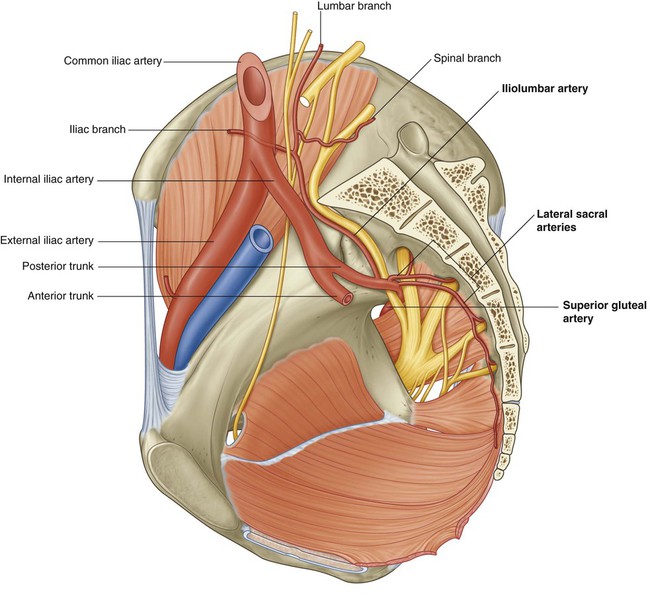
Internal iliac artery
The internal iliac artery originates from the common iliac artery on each side, approximately at the level of the intervertebral disc between LV and SI, and lies anteromedial to the sacro-iliac joint (Fig. 5.63). The vessel courses inferiorly over the pelvic inlet and then divides into anterior and posterior trunks at the level of the superior border of the greater sciatic foramen. Branches from the posterior trunk contribute to the supply of the lower posterior abdominal wall, the posterior pelvic wall, and the gluteal region. Branches from the anterior trunk supply the pelvic viscera, the perineum, the gluteal region, the adductor region of the thigh, and, in the fetus, the placenta.
Branches of the posterior trunk of the internal iliac artery are the iliolumbar artery, the lateral sacral artery, and the superior gluteal artery (Fig. 5.63).
 The iliolumbar artery ascends laterally back out of the pelvic inlet and divides into a lumbar branch and an iliac branch. The lumbar branch contributes to the supply of the posterior abdominal wall, psoas and quadratus lumborum muscles, and cauda equina, via a small spinal branch that passes through the intervertebral foramen between LV and SI. The iliac branch passes laterally into the iliac fossa to supply muscle and bone.
The iliolumbar artery ascends laterally back out of the pelvic inlet and divides into a lumbar branch and an iliac branch. The lumbar branch contributes to the supply of the posterior abdominal wall, psoas and quadratus lumborum muscles, and cauda equina, via a small spinal branch that passes through the intervertebral foramen between LV and SI. The iliac branch passes laterally into the iliac fossa to supply muscle and bone.
 The lateral sacral arteries, usually two, originate from the posterior division of the internal iliac artery and course medially and inferiorly along the posterior pelvic wall. They give rise to branches that pass into the anterior sacral foramina to supply related bone and soft tissues, structures in the vertebral (sacral) canal, and skin and muscle posterior to the sacrum.
The lateral sacral arteries, usually two, originate from the posterior division of the internal iliac artery and course medially and inferiorly along the posterior pelvic wall. They give rise to branches that pass into the anterior sacral foramina to supply related bone and soft tissues, structures in the vertebral (sacral) canal, and skin and muscle posterior to the sacrum.
 The superior gluteal artery is the largest branch of the internal iliac artery and is the terminal continuation of the posterior trunk. It courses posteriorly, usually passing between the lumbosacral trunk and anterior ramus of S1, to leave the pelvic cavity through the greater sciatic foramen above the piriformis muscle and enter the gluteal region of the lower limb. This vessel makes a substantial contribution to the blood supply of muscles and skin in the gluteal region and also supplies branches to adjacent muscles and bones of the pelvic walls.
The superior gluteal artery is the largest branch of the internal iliac artery and is the terminal continuation of the posterior trunk. It courses posteriorly, usually passing between the lumbosacral trunk and anterior ramus of S1, to leave the pelvic cavity through the greater sciatic foramen above the piriformis muscle and enter the gluteal region of the lower limb. This vessel makes a substantial contribution to the blood supply of muscles and skin in the gluteal region and also supplies branches to adjacent muscles and bones of the pelvic walls.
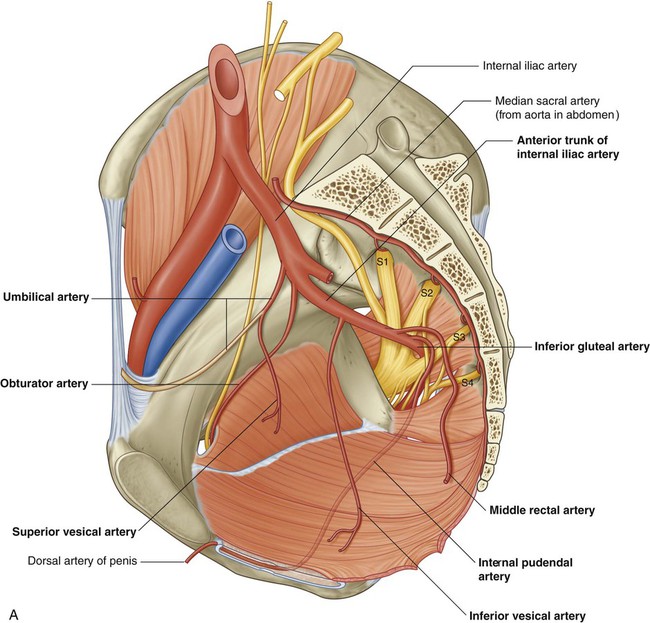
Branches of the anterior trunk of the internal iliac artery include the superior vesical artery, the umbilical artery, the inferior vesical artery, the middle rectal artery, the uterine artery, the vaginal artery, the obturator artery, the internal pudendal artery, and the inferior gluteal artery (Fig. 5.64).
 The first branch of the anterior trunk is the umbilical artery, which gives origin to the superior vesical artery and then travels forward just inferior to the margin of the pelvic inlet. Anteriorly, the vessel leaves the pelvic cavity and ascends on the internal aspect of the anterior abdominal wall to reach the umbilicus. In the fetus, the umbilical artery is large and carries blood from the fetus to the placenta. After birth, the vessel closes distally to the origin of the superior vesical artery and eventually becomes a solid fibrous cord. On the anterior abdominal wall, the cord raises a fold of peritoneum termed the medial umbilical fold. The fibrous remnant of the umbilical artery itself is the medial umbilical ligament.
The first branch of the anterior trunk is the umbilical artery, which gives origin to the superior vesical artery and then travels forward just inferior to the margin of the pelvic inlet. Anteriorly, the vessel leaves the pelvic cavity and ascends on the internal aspect of the anterior abdominal wall to reach the umbilicus. In the fetus, the umbilical artery is large and carries blood from the fetus to the placenta. After birth, the vessel closes distally to the origin of the superior vesical artery and eventually becomes a solid fibrous cord. On the anterior abdominal wall, the cord raises a fold of peritoneum termed the medial umbilical fold. The fibrous remnant of the umbilical artery itself is the medial umbilical ligament.
 The superior vesical artery normally originates from the root of the umbilical artery and courses medially and inferiorly to supply the superior aspect of the bladder and distal parts of the ureter. In men, it also may give rise to an artery that supplies the ductus deferens.
The superior vesical artery normally originates from the root of the umbilical artery and courses medially and inferiorly to supply the superior aspect of the bladder and distal parts of the ureter. In men, it also may give rise to an artery that supplies the ductus deferens.
 The inferior vesical artery occurs in men and supplies branches to the bladder, ureter, seminal vesicle, and prostate. The vaginal artery in women is the equivalent of the inferior vesical artery in men and, descending to the vagina, supplies branches to the vagina and to adjacent parts of the bladder and rectum.
The inferior vesical artery occurs in men and supplies branches to the bladder, ureter, seminal vesicle, and prostate. The vaginal artery in women is the equivalent of the inferior vesical artery in men and, descending to the vagina, supplies branches to the vagina and to adjacent parts of the bladder and rectum.
 The middle rectal artery courses medially to supply the rectum. The vessel anastomoses with the superior rectal artery, which originates from the inferior mesenteric artery in the abdomen, and the inferior rectal artery, which originates from the internal pudendal artery in the perineum.
The middle rectal artery courses medially to supply the rectum. The vessel anastomoses with the superior rectal artery, which originates from the inferior mesenteric artery in the abdomen, and the inferior rectal artery, which originates from the internal pudendal artery in the perineum.
 The obturator artery courses anteriorly along the pelvic wall and leaves the pelvic cavity via the obturator canal. Together with the obturator nerve, above, and obturator vein, below, it enters and supplies the adductor region of the thigh.
The obturator artery courses anteriorly along the pelvic wall and leaves the pelvic cavity via the obturator canal. Together with the obturator nerve, above, and obturator vein, below, it enters and supplies the adductor region of the thigh.
 The internal pudendal artery courses inferiorly from its origin in the anterior trunk and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. In association with the pudendal nerve on its medial side, the vessel passes laterally to the ischial spine and then through the lesser sciatic foramen to enter the perineum. The internal pudendal artery is the main artery of the perineum. Among the structures it supplies are the erectile tissues of the clitoris and the penis.
The internal pudendal artery courses inferiorly from its origin in the anterior trunk and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. In association with the pudendal nerve on its medial side, the vessel passes laterally to the ischial spine and then through the lesser sciatic foramen to enter the perineum. The internal pudendal artery is the main artery of the perineum. Among the structures it supplies are the erectile tissues of the clitoris and the penis.
 The inferior gluteal artery is a large terminal branch of the anterior trunk of the internal iliac artery. It passes between the anterior rami S1 and S2 or S2 and S3 of the sacral plexus and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. It enters and contributes to the blood supply of the gluteal region and anastomoses with a network of vessels around the hip joint.
The inferior gluteal artery is a large terminal branch of the anterior trunk of the internal iliac artery. It passes between the anterior rami S1 and S2 or S2 and S3 of the sacral plexus and leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle. It enters and contributes to the blood supply of the gluteal region and anastomoses with a network of vessels around the hip joint.
 The uterine artery in women courses medially and anteriorly in the base of the broad ligament to reach the cervix (Figs. 5.64B and 5.65). Along its course, the vessel crosses the ureter and passes superiorly to the lateral vaginal fornix. Once the vessel reaches the cervix, it ascends along the lateral margin of the uterus to reach the uterine tube, where it curves laterally and anastomoses with the ovarian artery. The uterine artery is the major blood supply to the uterus and enlarges significantly during pregnancy. Through anastomoses with other arteries, the vessel contributes to the blood supply of the ovary and vagina as well.
The uterine artery in women courses medially and anteriorly in the base of the broad ligament to reach the cervix (Figs. 5.64B and 5.65). Along its course, the vessel crosses the ureter and passes superiorly to the lateral vaginal fornix. Once the vessel reaches the cervix, it ascends along the lateral margin of the uterus to reach the uterine tube, where it curves laterally and anastomoses with the ovarian artery. The uterine artery is the major blood supply to the uterus and enlarges significantly during pregnancy. Through anastomoses with other arteries, the vessel contributes to the blood supply of the ovary and vagina as well.
Ovarian arteries
In women, the gonadal (ovarian) vessels originate from the abdominal aorta and then descend to cross the pelvic inlet and supply the ovaries. They anastomose with terminal parts of the uterine arteries (Fig. 5.65). On each side, the vessels travel in the suspensory ligament of the ovary (the infundibulopelvic ligament) as they cross the pelvic inlet to the ovary. Branches pass through the mesovarium to reach the ovary and through the mesometrium of the broad ligament to anastomose with the uterine artery. The ovarian arteries enlarge significantly during pregnancy to augment the uterine blood supply.
Median sacral artery
The median sacral artery (Figs. 5.64A and 5.65) originates from the posterior surface of the aorta just superior to the aortic bifurcation at vertebral level LIV in the abdomen. It descends in the midline, crosses the pelvic inlet, and then courses along the anterior surface of the sacrum and coccyx. It gives rise to the last pair of lumbar arteries and to branches that anastomose with the iliolumbar and lateral sacral arteries.
Veins
Pelvic veins follow the course of all branches of the internal iliac artery except for the umbilical artery and the iliolumbar artery (Fig. 5.66A). On each side, the veins drain into internal iliac veins, which leave the pelvic cavity to join common iliac veins situated just superior and lateral to the pelvic inlet.
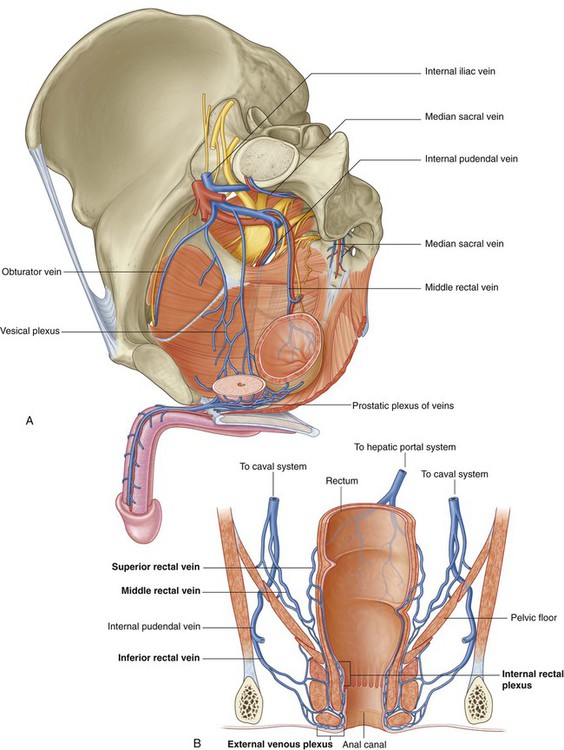
Within the pelvic cavity, extensive interconnected venous plexuses are associated with the surfaces of the viscera (bladder, rectum, prostate, uterus, and vagina). Together, these plexuses form the pelvic plexus of veins. The part of the venous plexus surrounding the rectum and anal canal drains via superior rectal veins (tributaries of inferior mesenteric veins) into the hepatic portal system, and via middle and inferior rectal veins into the caval system. This pelvic plexus is an important portacaval shunt when the hepatic portal system is blocked (Fig. 5.66B).
 The median sacral veins coalesce to form a single vein that joins either the left common iliac vein or the junction of the two common iliac veins to form the inferior vena cava.
The median sacral veins coalesce to form a single vein that joins either the left common iliac vein or the junction of the two common iliac veins to form the inferior vena cava.
 The ovarian veins follow the course of the corresponding arteries; on the left, they join the left renal vein and, on the right, they join the inferior vena cava in the abdomen.
The ovarian veins follow the course of the corresponding arteries; on the left, they join the left renal vein and, on the right, they join the inferior vena cava in the abdomen.
Lymphatics
Lymphatics from most pelvic viscera drain mainly into lymph nodes distributed along the internal iliac and external iliac arteries and their associated branches (Fig. 5.67), which drain into nodes associated with the common iliac arteries and then into the lateral aortic or lumbar nodes associated with the lateral surfaces of the abdominal aorta. In turn, these lateral aortic or lumbar nodes drain into the lumbar trunks, which continue to the origin of the thoracic duct at approximately vertebral level TXII.