Pelvic Trauma
Perspective
Epidemiology
Based on data from trauma registries, the majority of high-energy pelvic ring injuries are caused by motor vehicle collisions (MVCs), motorcycle crashes, and pedestrians being struck by motor vehicles, together accounting for 80 to 84% of pelvic fractures; and falls from height, which account for 5 to 12%1–5 of pelvic fractures. The mortality rates reported in the literature associated with pelvic fracture range from 9 to 22%1–5; in studies of large cohorts of trauma patients, the presence of pelvic fracture has been consistently shown to be an independent risk factor for death compared with trauma patients without pelvic fracture.6–8 Patients with pelvic fractures and with shock on arrival to the hospital have mortality rates of 33 to 57%.3,4 Increased age, shock on arrival at the hospital, high injury severity and revised trauma scores (which generally reflect the presence of multisystem injuries), and the need for transfusion have all been shown to increase the risk of death.3–5,9,10 The mortality rate among pedestrians struck by motor vehicles who sustain pelvic injury has been shown to be 23%.11
Despite advances in motor vehicle safety design, MVCs continue to be a major cause of pelvic fracture. Rates of pelvic fracture secondary to MVC range from 10 to 28%.9,12,13 Lateral impact remains the most prevalent mechanism for pelvic trauma in collisions, for which the widespread advent of front airbags has little effect. Some have speculated that the increased popularity of sport-utility vehicles in past decades is contributing to the severity of side-impact injuries, specifically as a result of the higher bumper in these vehicles striking the side of lower cars.9,12,14
Principles of Disease
Bony and Ligamentous Anatomy
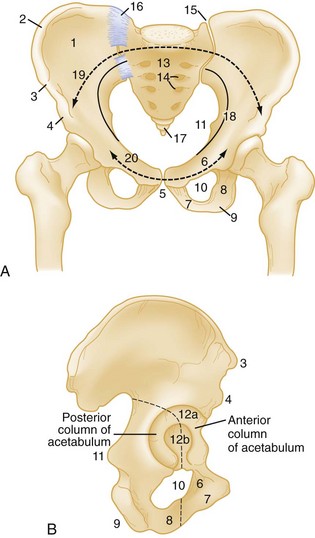
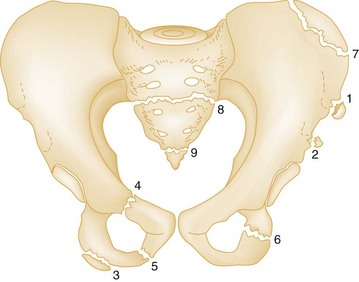
The pelvic ring is made up of right and left innominate bones and the sacrum. The innominate bones consist of the pubis, ischium, and ilium (Fig. 55-1). The bony pelvis provides protection for its visceral contents, serves as attachment points for muscles, and transmits weight from the trunk to the lower limbs. The main weight-bearing forces are transmitted through the posterior wall of the pelvis, called the posterior arch, which is composed of thick bone and ligaments. The rich network of major arteries, veins, and nerves that course in front of the posterior arch may be injured concomitantly with forces causing bony injuries of this arch.
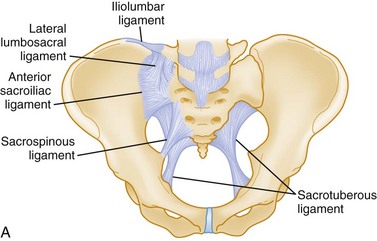
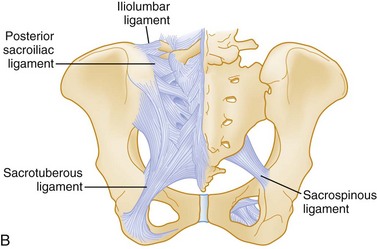
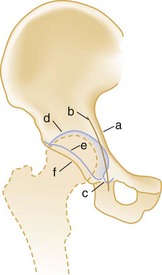
Knowledge of the ligamentous attachments of the pelvic ring is crucial to understanding how stability is maintained or disrupted in pelvic injury. The stability of the pelvis is maintained by ligaments, as well as the muscles and fascia that make up the pelvic floor. Anteriorly, the symphysis pubis provides the major mechanical stability. Posteriorly, a complex of strong ligaments—the sacrospinous, sacrotuberous, iliolumbar, and anterior and posterior sacroiliac (SI) ligaments—maintains the integrity of the posterior arch (Fig. 55-2). It is important to appreciate that mechanically unstable pelvic fractures are unstable primarily because of the disruption of these posterior ligaments.
Vascular Anatomy
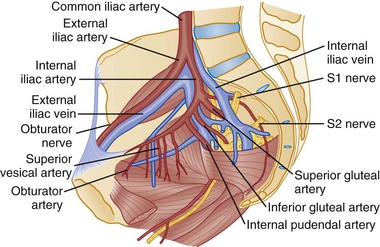
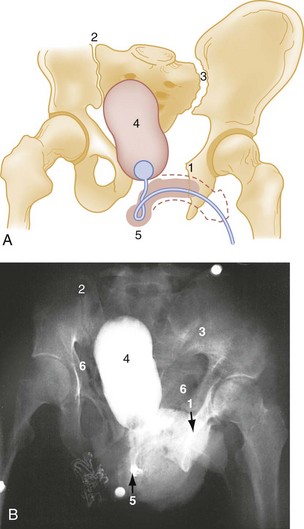
Most of the blood supply to the pelvis comes from the left and right internal iliac arteries. The internal iliac arteries course at the level of the SI joints. The various arteries that derive from the internal iliac arteries initially run in close proximity to the posterior pelvic arch and eventually anastomose extensively with one another, forming a rich collateral network (Fig. 55-3). The superior gluteal artery is the largest branch and is commonly injured in fractures of the posterior pelvic arch. The obturator and internal pudendal branches are often injured in fractures involving the pubic rami.
Pathophysiology and Key Patterns of Pelvic Fracture
Numerous classification schemes exist for pelvic fractures. Two widely used schemes for pelvic injury are presented here. The classification by Tile stresses the biomechanical stability of the pelvic ring15 (Box 55-1). The Young-Burgess classification emphasizes the mechanisms of injury16 (Box 55-2). From a practical viewpoint, it is highly useful to consider both of these elements in the assessment of a pelvic ring fracture. Within both classification systems exist numerous subtypes of injuries, the interobserver reliability of which has been questioned.17,18 For the emergency physician, a good understanding of both the underlying principles of pelvic stability and mechanisms of injury is far more important than a detailed knowledge of the numerous subtypes of injury that exist within the classification schemes. The broad distinction of mechanically stable from unstable fractures of the pelvic ring is clinically useful to bear in mind in assessing patients, as it has been demonstrated consistently over time that those with unstable injuries have higher mortality and greater transfusion requirements.16,19,20
Stable Injuries (Tile Type A)
Fractures of individual bones without involvement of the pelvic ring represent one third of all pelvic fractures. In general, most stable pelvic fractures heal well with rest and analgesic drugs for pain control (Fig. 55-4).15
Undisplaced or Minimally Displaced Fractures of the Pelvic Ring.: The normal pelvis is not totally rigid because of the slight mobility at the SI joints and symphysis pubis and the inherent elasticity of bone. A single break in the ring is possible. Nevertheless, the pelvis is not totally forgiving, and identification of a single break in the ring should prompt a search for a second disruption.
If the patient with a ramus fracture reports posterior pelvic pain and plain radiographs do not reveal posterior injury, further investigations may reveal occult posterior fractures. A study performed more than 35 years ago found that patients who sustained apparently isolated pubic ramus fractures showed increased uptake of radionuclides on bone scans in the acetabulum and SI joint, suggesting that occult bony or ligamentous injury accounted for the pain.21 More recently, a study that prospectively evaluated elderly patients who were diagnosed with isolated ramus fractures on plain films found that 95% had sacral fracture detected by magnetic resonance imaging (MRI).22 This study does not imply a need to perform MRI on all elderly patients with ramus fractures in the ED; rather, it enhances our understanding of the pathophysiology of ramus fractures and underscores the importance of adequate analgesia in these patients. The lateral compression type I fracture described by Young and Burgess (Fig. 55-5)—characterized by pubic ramus fracture with ipsilateral sacral compression—bears special consideration among the mechanically stable pelvic fractures, as it has been shown to be associated with a mortality rate of 8% with a high incidence of associated injuries.20,23,24
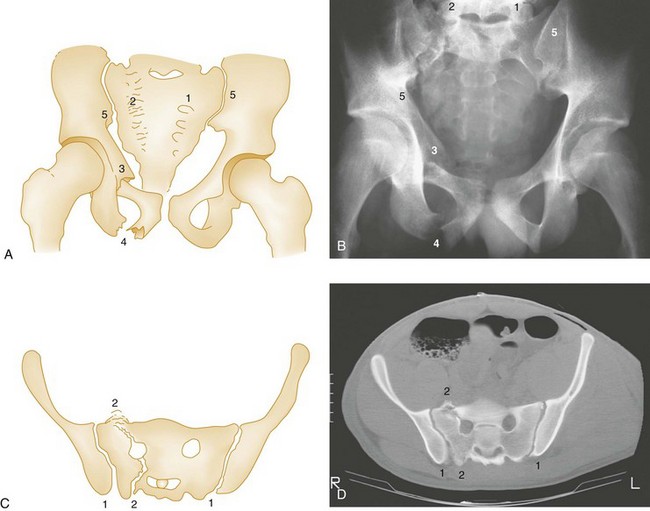
Also termed a straddle fracture, four-pillar injuries involve fractures of both pubic rami on both sides of the symphysis pubis, causing the so-called “butterfly segment” (Fig. 55-6). The injury is produced by a direct blow with a straddle mechanism. Although these fractures may occur without posterior arch disruption, four-pillar injuries are also commonly associated with lateral compression or vertical shear forces that may cause concomitant injuries to the posterior pelvic arch. CT of the pelvis is required in cases of four-pillar injuries to detect and classify precisely the posterior arch injury and plan orthopedic treatment.15 The genitourinary tract frequently is injured concomitantly with this type of pelvic fracture and should be evaluated carefully (see Fig. 55-6).
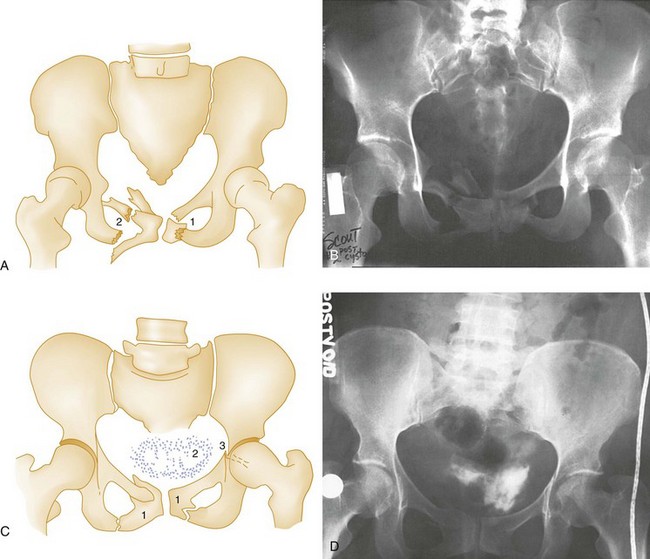
Figure 55-6 Four-pillar (straddle) fracture. A and B, Partial inlet view of pelvis shows straddle fracture. (1) and (2) Marked comminution of left pubic bone and comminuted right superior and inferior rami. This partial inlet projection shows displacement of fragments into the pelvis, which is not evident on the anteroposterior view of the same patient in C and D. A true inlet projection and computed tomography scan (not available) would provide further information about the posterior arch, which is injured frequently in straddle fractures and should be imaged (see text). C and D, Postvoid cystogram of the same patient with anteroposterior pelvis. (1) Fractures of pubic rami are seen again but do not appear to be as displaced compared with A and B because this projection is an anteroposterior view. Even minor degrees of angulation of the x-ray beam can change the appearance of pelvic fracture displacement. (2) Extravascular contrast indicates bladder rupture; (3) left acetabular fracture is seen in this projection but not in B because of the difference in projection. The acetabular fracture disrupts the ilioischial line (see also Fig. 55-13) and is a posterior column fracture.
Isolated fracture of the iliac wing was described by Duverney in 1751 and now bears his name. It is caused by direct trauma to the iliac crest, usually by lateral compression forces. Although displacement is usually minimal because of the arrangement of the muscle attachments of the abdominal wall, orthopedic consultation is recommended. The fracture may extend into the acetabulum, altering the treatment and prognosis. Severely displaced fractures of the iliac wing require open reduction and internal fixation.15 It is worth noting that a high incidence of major associated nonpelvic injuries among patients with isolated iliac wing fracture has been reported.23
Transverse Fractures of the Sacrum.: Transverse fractures of the sacrum do not compromise the pelvic ring. Transverse fractures at or below S4 are unlikely to be accompanied by neurologic injury.25 An upper sacral transverse fracture is the result of a flexion injury, such as being struck on the lower back by a heavy load while bending over, or by direct forces to the sacrum, as in a fall from a great height.25 The patient reports pain in the buttocks, perirectal area, and posterior thighs. There may be local pain, swelling, and bruising overlying the sacrum, and on gentle bimanual rectal examination, severe pain, abnormal motion, and palpable hematoma may be elicited. Radiographically, the fracture may be difficult to visualize on anteroposterior (AP) and lateral projections, in which case a pelvic outlet view may be helpful. Simple transverse fractures at or below S4 are treated conservatively. Above S4, neurologic injuries are common, necessitating careful clinical evaluation and surgery when neurologic compromise is present.
Avulsion Fractures.: These usually occur during athletic activities and are the result of a sudden, forceful muscular contraction or excessive muscle stretch. They are seen more commonly in older children and teenagers before closure of the corresponding physis occurs; adults may have the same symptoms from ligamentous injury at these sites without radiographic abnormality.
A portion of the iliac crest epiphysis may be avulsed by contraction of the abdominal muscles. Similarly, the anterior superior iliac spine may be avulsed by forcible contraction of the sartorius muscle. Forceful contraction of the rectus femoris (as in kicking a ball) can result in the less common injury of anterior inferior iliac spine avulsion; however, this radiographic finding should be distinguished from a normal variant, the os acetabuli, which is a secondary center of ossification at the superolateral margin of the acetabulum.26 Clinical examination is similar in these injuries and reveals local pain, swelling, and limitation of motion.
Stress Fractures.: Stress fractures occur with vigorous athletic or military training and in the last trimester of pregnancy.27 The diagnosis of stress fractures is based on the clinical evaluation and can be confirmed, if required, by radionuclide bone scan, although MRI has been shown to be a superior method for detecting these injuries.28
Partially Stable and Unstable Injuries (Tile Types B and C)
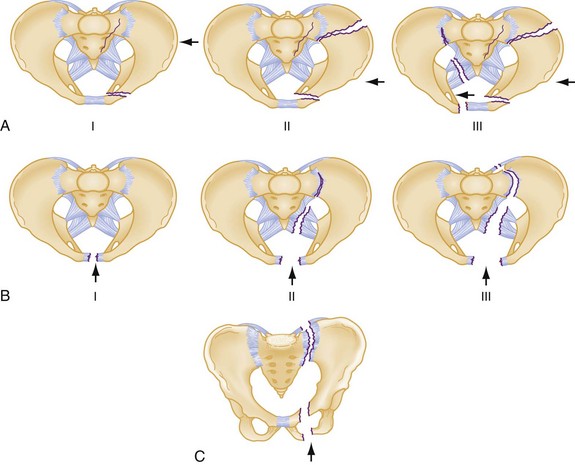
Anteroposterior Compression.: Severe AP compression forces result in disruption at or near the symphysis pubis. Symphysis widening of less than 2.5 cm is considered a stable injury (the symphysis should normally be ≤0.5 cm in an adult but can increase 2-3 mm during or after pregnancy); however, with continued force in the AP direction, the hemipelvis externally rotates, tearing the sacrospinous, sacrotuberous, and anterior SI ligaments. The SI joint opens and hinges on the intact posterior SI ligaments. The resulting injury is aptly described as an “open-book” fracture. The pelvis is rotationally unstable in the horizontal plane, but the intact posterior SI ligaments maintain vertical stability.15,16
When diastasis of the pubic symphysis is greater than 2.5 cm on the AP radiograph, the posterior injury is usually seen as widening of the SI joint and occasionally as a sacral or iliac fracture (see Fig. 55-5).15 If the injurious forces continue, they may separate the hemipelvis, and the SI joint is seen as widely separated on the plain AP radiograph (Fig. 55-7) and the CT scan.15 The AP radiograph may be misleading in suggesting a pure open-book fracture in cases with symphysis disruptions greater than 2.5 cm. These cases commonly are associated with vertical shear fractures, and careful clinical and computed tomography (CT) assessment for vertical instability is essential to classify the fracture properly and plan treatment.15
These same forces also may injure the neurologic and vascular structures at the posterior arch; the overall volume of the pelvis is increased in the open-book injury, facilitating the expansion of a retroperitoneal hematoma. Several studies have demonstrated that patients with severe grades of AP compression injuries have the highest crystalloid and blood requirements.16,19
Lateral Compression.: Lateral compression of the pelvic ring results in varying degrees of internal rotation of the affected hemipelvis. Initially, this causes buckling of the sacrum and horizontal pubic rami fractures. Rami fractures may occur on the ipsilateral or contralateral side, the latter being referred to as the “bucket-handle” fracture (Fig. 55-8).
Similar to the AP injury, with increasing disruption of the posterior ligaments comes increasing rotational instability. In the most severe lateral compression trauma, the ipsilateral pelvis internally rotates to such a degree that the contralateral pelvis may externally rotate. This is referred to as the “windswept” pelvis. Lateral compressive injuries result in varying degrees of horizontal rotational instability; however, the vertical stability of the pelvis is maintained (see Fig. 55-8).
Vertical Shear.: Vertical shear injuries represent the most unstable injuries to the pelvic ring and are associated with violent axial loading of the hemipelvis (e.g., fall from height, “submarining” underneath a dashboard). Fractures occur in vertical planes. Anteriorly, the symphysis and rami may be disrupted. Posteriorly, gross displacement and instability in the rotational and vertical planes may be present through the sacrum, the SI joint, or the ilium such that the hemipelvis may displace posteriorly and cephalad15,16 (see Fig. 55-9).
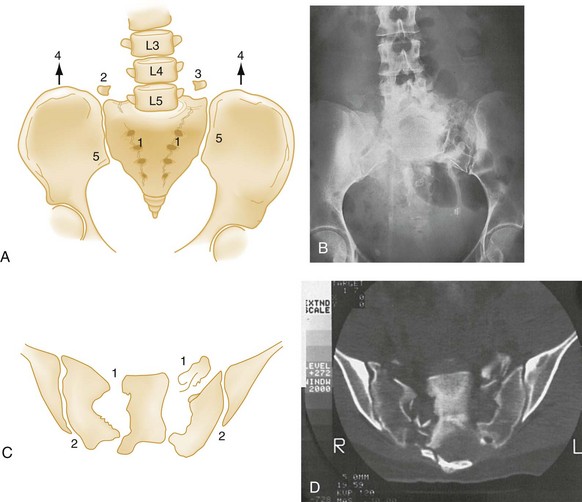
Avulsion of the ischial spine, the lower lateral lip of the sacrum, and the transverse process of the fifth lumbar vertebra (sites of insertion of ligaments) (Fig. 55-9 and Box 55-3) are important clues to the presence of vertical shear fractures.15 The vertical shearing forces transmitted through the bony pelvis are also transmitted through the rich vascular network and nerve plexus that are directly adjacent to the bone. This activity accounts for the major hemorrhage and neurologic injuries associated with vertical shear fractures.
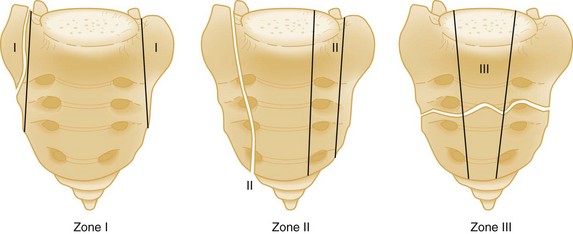
Vertical Sacral Fractures.: A crucial distinction in considering sacral fractures is that transverse fractures do not involve the pelvic ring, but vertical fractures do. Vertical sacral fractures are caused by high-energy injuries and were classified by Denis into three groups according to whether the fracture line extends (1) laterally to the sacral foramina, (2) through the foramina, or (3) medially to the foramina, involving the central spinal canal29 (Fig. 55-10). The radiographic diagnosis of this fracture hinges on careful examination of the symmetrical cortical lines that are normally present at the superior margins of the sacral foramina on the AP view. Disruption, distortion, or asymmetry of these lines is an important marker of sacral fractures.26
There is a high risk of neurologic complications associated with these injuries: 6% when lateral to the foramina, 28% when through the foramina, and 58% when medial to the foramina.29 Neurologic dysfunction correlates to the nerve roots involved but may include any bowel, bladder, or sexual dysfunction. Surgery is commonly performed for fractures associated with neurologic dysfunction, with the goals of bony fixation of the sacrum and decompression of affected nerve roots.
Open Pelvic Fractures
An open pelvic fracture is present when there is direct communication between the fracture site and a skin, rectal, or vaginal wound. These are potentially lethal injuries, especially if the open nature is not recognized: hemorrhage accounts for early mortality, but infection, sepsis, acute respiratory distress syndrome, and multisystem organ failure are all causes of delayed death.24,30 The majority of case series before 1991 reported mortality rates greater than 50%; rates reported from 1991 to 1999 ranged from 5 to 30%,30 although a recent series reported a 45% mortality rate.31
The skin over the posterior pelvis and gluteal area and perineum is inspected carefully for wounds. Some fractures are open only by virtue of a bone spicule penetrating the vagina or rectum and are identified by careful digital rectal examination (DRE) and vaginal examination. Hemorrhage from a large open laceration should be treated by direct manual pressure or pressure dressing. Pelvic fractures communicating with the rectum have traditionally mandated a diverting colostomy; however, a systematic review of the literature on this topic found no difference in infection rates between patients treated with colostomy and those treated without.32
Penetrating Pelvic Trauma
Because of the complex anatomy of the viscera, blood vessels, and nerves within the pelvis, penetrating trauma to this area presents a major challenge. Overall mortality in this group of patients has been reported to be 6 to 12%, but the mortality rate of patients in shock is 50%.33,34 Vascular injuries singly and in combination may involve the aorta; common iliac artery; and external, internal, and common iliac veins. Injuries to genitourinary structures and hollow viscera may occur, with fecal contamination from colorectal injury being a major concern. When present, the finding of blood on DRE is an important clue that rectal injury has occurred. Emergent surgical consultation is required in all cases of penetrating pelvic trauma.
Clinical Features
Age is an important consideration in patients with pelvic fracture. Osteopenic bone may be disrupted by lesser forces. Furthermore, studies consistently demonstrate higher morbidity and mortality among elderly patients with pelvic fracture. Although pelvic hemorrhage remains an important consideration among elderly patients with pelvic fracture, higher mortality rates are further influenced by a greater prevalence of preexisting medical conditions in this population that increase the risk of death from multisystem organ failure.35,36 Decreased physiologic reserves in older patients may limit success in the acute resuscitation and definitive treatment of injuries.
Injuries to other organ systems are extremely common in patients with pelvic fracture.2,4,5 It is important to identify all major injuries to other organ systems to prioritize definitive surgical treatment for the multiply traumatized patient. In women, it is important to consider the possibility of pregnancy and to test for pregnancy whenever appropriate.
Physical Examination
On inspection, rotation of the iliac crests indicates a serious pelvic fracture. Leg-length discrepancy may suggest a hip injury or cephalad migration of an unstable hemipelvis. Careful inspection of the skin and skin folds is necessary to identify open fractures. Perineal or genital ecchymosis or hematoma may be observed, and in cases in which many hours have elapsed since the injury, ecchymosis in the periumbilical area (Cullen’s sign) or flanks (Grey Turner’s sign) from retroperitoneal hemorrhage may be present. Careful palpation of the pelvic ring to seek the presence of point tenderness is imperative; palpation starts at the symphysis anteriorly and proceeds to both pubic rami, the iliac spines and crests, and finally to the sacrum and SI joints posteriorly. The presence of tenderness in any of these locations is an important indicator of pelvic ring injury in alert patients without distracting injury.37
The penis should be milked to examine for blood at the meatus. Although the value of the DRE has been questioned in the literature with claims that it has extremely low sensitivity as a diagnostic test, it remains useful as a screening tool.38 The DRE should evaluate sensation, sphincter tone, position and consistency of the prostate, presence of a presacral hematoma, bony contour of the sacrum and coccyx, mucosal penetration of bony spicules, and presence of frank or occult blood. In the setting of a pelvic fracture, female patients should undergo a vaginal examination to diagnose an open fracture. Because it is possible to create an open fracture iatrogenically through the vaginal or rectal wall, DRE and vaginal examination should be performed carefully, especially in an unconscious patient who cannot localize pain. The examiner should be mindful when performing these examinations that bony spicules can lacerate the examining finger. Extravasated urine may be detected in the scrotum or the subcutaneous tissues of the penis, vulva, or abdominal wall. The presence and quality of pulses in the lower limb should be assessed, as should sensation, strength, and deep tendon reflexes.
Associated Pelvic Injuries
The overall incidence of bladder or urethral disruption associated with any pelvic fracture is approximately 4 to 6%, with increased risk among those with severe pelvic injuries.2 Because the urethra is far less exposed in women than in men, injury to the urethra in women with pelvic fracture is rare.39,40
A review of 721 patients with pelvic fracture revealed an incidence of bladder rupture in 5% of patients. Those with fractures of the anterior arch of the pelvis are at greatest risk for bladder injury: diastasis of the symphysis more than 1 cm and fracture around the obturator ring with displacement greater than 1 cm were associated with a tenfold and threefold increased risk of bladder rupture, respectively.41
The presence of gross hematuria indicates injury of the lower urinary tract. Blood at the urethral meatus necessitates a retrograde urethrogram followed by a cystogram. Gross hematuria is investigated with a combination of urethrography, intravenous pyelography, cystography, and CT. The sequence and types of examinations are individualized for each patient. Fracture to the inferomedial pubic ramus and increasing symphyseal diastasis have both been shown to be predictive of urethral injury.42 Of note, it has been reported that retrograde urethrocystography done before CT of the pelvis may impair the ability of CT to detect extravasation of contrast that would indicate active pelvic bleeding.43 Therefore if CT is to be performed, it should be done before retrograde urethrocystography.
Sexual dysfunction in both men and women is a recognized complication of pelvic trauma. The incidence of impotence associated with urethral rupture is significant. In the absence of urethral injury, sexual dysfunction in men still may occur secondary to neurovascular disruption associated with the pelvic fracture.38
Neurologic Injury
The risk of neurologic injury has been shown to correlate with instability of the pelvic injury, with a reported incidence of neurologic dysfunction of 1.5, 3.8, and 14% in Tile type A, B, and C fractures, respectively; acetabular fractures were associated with a 10% incidence of neurologic dysfunction.45 Neurologic injury occurs commonly in patients with vertical sacral fractures or transverse fractures above the S4 level. Among patients with vertical fractures that involve the foramina, 28% have associated neurologic deficits. In patients with fractures medial to the foramina involving the spinal canal, 57% have neurologic deficits.29
Gynecologic Injury
Blood at the introitus may indicate a urethral injury, open pelvic fracture, or local laceration without communication with the bony pelvis. Delayed urologic and sexual dysfunction and complications with pregnancy are common after pelvic injury.46 Gynecology consultation is indicated when there is injury to the female reproductive tract in association with a pelvic fracture and for all pregnant women who sustain pelvic fracture of any kind.
Associated Nonpelvic Injuries
The magnitude of force required to disrupt the pelvis commonly results in severe injuries to other organ systems. Among those patients who die with pelvic fracture, it is rare that the pelvic fracture is an isolated injury.1,2,19,47,48 Furthermore, associated injuries among trauma patients with pelvic fracture may contribute more to mortality than the pelvic injury itself.10
Some authors have described patterns of associated nonpelvic injuries with certain patterns of pelvic fracture; however, these findings have not been consistently reproduced in the literature.19,49 Severe injuries to head, spine, thorax, and abdomen may occur with both stable and unstable pelvic fractures; they may all occur with all major mechanisms of pelvic injury. One associated injury that reflects the dispersion of enormous forces throughout the body is the rupture of the thoracic aorta; albeit uncommon in blunt trauma, it is five to eight times more likely in older patients with pelvic fracture.2,50 Therefore the diagnosis of a pelvic fracture should prompt a careful evaluation for other system injuries.
Diagnostic Strategy
Plain Radiography
Routine radiographs of the pelvis are not necessary in cases of blunt trauma if the patient is asymptomatic, awake, and alert and has normal findings on physical examination of the pelvis.51–54 However, routine AP plain radiography of the pelvis (PXR) is advised by the Advanced Trauma Life Support (ATLS) guidelines for patients with severe mechanisms of injury who are symptomatic or whose examination is compromised by either decreased level of consciousness or distracting injuries.
On the AP radiograph, the symphysis pubis is normally no more than 5 mm wide, and a small (1- or 2-mm) vertical offset of the left and right pubic rami is normal.26 Overlapping at the symphysis pubis is abnormal and is the result of a severe crushing injury. Normally the SI joint is approximately 2 to 4 mm wide.26
On the AP view, the physician may judge the degree of pelvic rotation caused by technique and positioning by the presence of asymmetry in the size and shape of the left and right obturator foramina and iliac wings. Diastasis of the SI joint also causes an asymmetrical appearance of the obturator foramina and the iliac wings: If there is displacement into external rotation, the affected iliac wing appears broader, and the anterior iliac spine appears more prominent.26 Avulsion fracture of the fifth lumbar transverse process by the iliolumbar ligament often accompanies an SI joint disruption or a vertical sacral fracture and is a valuable clue to posterior arch injuries26 (see Fig. 55-9 and Box 55-3).
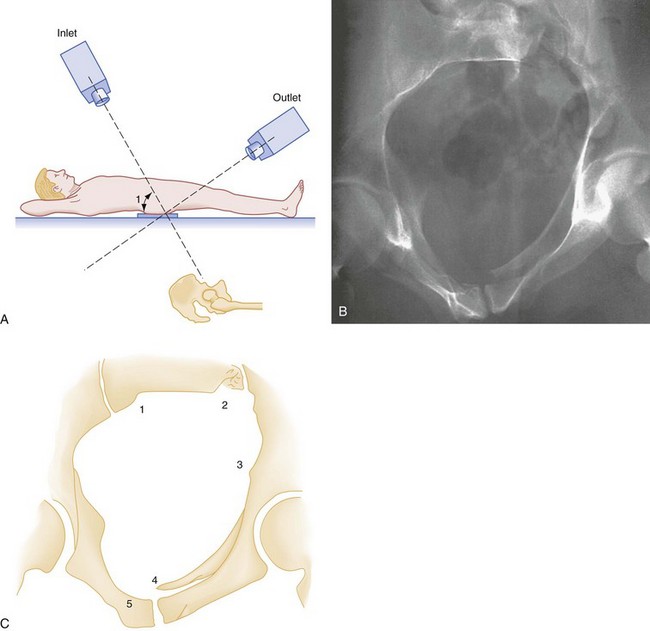
The reliability of the single AP PXR to detect pelvic fractures has been questioned in the literature. Two case series have reported sensitivities of only 64 and 68% with specificities of 90 and 98%, respectively, thus prompting the question of whether PXR is necessary at all when patients are to undergo immediate abdominopelvic CT evaluation.55,56 In particular, sacral fractures and SI joint disruptions are not well visualized on the AP view.57 However, the addition of inlet and outlet views of the pelvis has been shown to increase the sensitivity and specificity of plain radiographs in detecting significant pelvic fracture (Fig. 55-11) and SI joint disruption and should be considered in all patients with presumed stable anterior pelvic ring injuries with any complaints of posterior pelvic pain.58
When patients are too unstable to undergo CT investigation, the AP PXR is useful in screening for pelvic injuries that are most associated with major blood loss and potentially require urgent intervention.59,60 That is, although PXR may miss many fractures, a very abnormal PXR is predictive. Findings that predict the need for transfusion include open-book fracture or displacement of 0.5 cm or more at any fracture site in the pelvic ring and displaced symphysis pubis, displaced obturator ring fracture, or obvious vertical displacement in the posterior pelvis.61,62 It is important to note that all of these signs may be associated with posterior pelvic injury. Therefore the PXR remains a vital test when CT cannot be immediately performed and should be used to alert both surgeons and angiographers of the potential need for definitive management of pelvic hemorrhage.63
Computed Tomography
CT is the imaging test of choice for evaluating the injured pelvis. CT provides detailed information about the posterior arch and rotational deformities that indicate the relative stability of the pelvic ring; furthermore, the acetabulum, which may be difficult to assess with plain radiographs, can be well visualized with CT. CT has demonstrated a much higher sensitivity and specificity than plain radiography in detecting pelvic fracture.55,56 Furthermore, abdominopelvic CT provides detailed information about concomitant injury to abdominal organs that aids in the planning of laparotomy, external fixation of the pelvis, angiography, and definitive orthopedic management of the pelvic injury. Finally, it has been demonstrated that selective CT scanning of the chest, abdomen, and pelvis in patients who sustain high-energy trauma results in a high miss rate of important diagnoses that alter treatments plans versus “pan” CT scanning (i.e., including all of the head, neck, chest, abdomen, and pelvis).64,65 It should be noted that the decision to “pan” CT scan should be based on a combination of factors, such as abnormal vital signs, neurologic status, the detection of injuries on clinical examination, and the patient’s mechanism of injury. Clinical judgment should guide the decision, to avoid wasting resources and unnecessarily exposing patients to radiation.
Evaluation of Hemorrhage
Hemorrhage is the most devastating direct complication of pelvic fracture. In the original series of high-energy pelvic injuries used to formulate their classification system, Burgess and colleagues analyzed blood transfusions and found that an average of 14.8 units were required in the AP compression group, 9.2 units in the vertical shear group, and 3.6 units in the lateral compression group.16 The correlation between transfusion requirements and type of pelvic fracture has been confirmed in more recent studies that demonstrate that unstable fracture patterns increase the need for transfusion and risk of mortality,63 with one series reporting a median of 10 units of blood required (range 1-70 units).3
Major pelvic hemorrhage results from lacerations of the rich vascular network supplying the pelvis in the retroperitoneal space. Pelvic hemorrhage is commonly venous in origin and may be contained and tamponaded retroperitoneally by an intact peritoneum. However, it is possible for bleeding to extend beyond the retroperitoneum and dissect into the anterior abdominal wall (to the chagrin of the unwary clinician who introduces a scalpel or peritoneal dialysis catheter) or through the peritoneum into the abdominal cavity (see later). Bleeding also may occur from the marrow at the fracture sites.66 Finally, coagulopathy is another cause of persistent retroperitoneal bleeding and should be considered when the patient does not respond to fluid and blood replacement.
The combination of both pelvic and intra-abdominal bleeding is associated with devastating outcomes.63 In one large series, major pelvic injury was associated with intra-abdominal injuries in 31% of cases; the liver and spleen were injured in 10 and 6% of these cases, respectively.2 In the patient with pelvic fracture who is in shock, it is important to establish early whether there is hemorrhage within the abdominal cavity necessitating laparotomy. Diagnostic strategies for evaluation of pelvic fracture–associated hemorrhage include diagnostic peritoneal lavage (DPL), ultrasound, and CT. Regardless of the modality of evaluation, it is crucial to avoid unnecessary laparotomy because of the higher mortality rate for hemodynamically unstable patients with pelvic fractures who undergo a negative abdominal exploration.
Diagnostic Peritoneal Lavage
DPL is a widely accepted, rapid, and accurate means of establishing the presence of intra-abdominal hemorrhage. Although it has been largely supplanted in many centers by ultrasound and CT, DPL nevertheless remains an effective tool to assist with difficult triage decisions in the trauma patient. A pelvic fracture presents a special situation for DPL because of the possibility that a retroperitoneal hematoma may dissect into the anterior abdominal wall. However, when a fully open technique is used (i.e., the peritoneum is entered under direct visual control), the false-positive and false-negative rates are each 0.7%.67
DPL may be performed in the infraumbilical location in most patients; however, the supraumbilical location should be used if any of the following conditions are present: prior abdominal scars, time delay since the injury of more than 1 hour, or a hematoma encountered during the procedure.67
Gross aspiration of blood indicates possible major intra-abdominal hemorrhage, and laparotomy is recommended at the earliest opportunity for hemodynamically unstable patients.47 The lavage that is positive by cell count criteria alone is a special situation. If these patients are hemodynamically unstable, it is advisable to perform angiography with therapeutic embolization and external pelvic fixation before laparotomy.66,67
Ultrasound
Focused assessment with sonography in trauma (FAST) is widely used to identify free intraperitoneal fluid in the trauma patient. An important caveat to note is that FAST is not helpful for evaluating the retroperitoneal space where pelvic hemorrhage occurs. Although a positive FAST study that shows free fluid is widely used as a triage point to decide on laparotomy in a hemodynamically unstable patient, its reliability in patients with major pelvic injury has been questioned. Sensitivities ranging from 24 to 81% and specificities ranging from 87 to 96% for the detection of hemoperitoneum have been reported68,69 in patients with pelvic fracture; the presence of pelvic fracture has been reported to be a predictor of a false-negative FAST examination, with an odds ratio of 3.5 (95% confidence interval 1.3-9.2).70
Although these reports come from retrospective case series—and therefore do not necessarily represent the highest levels of evidence—the high incidence of false-negative FAST examinations reported in the literature in patients with pelvic injury is nonetheless cause for concern. This is because pelvic and intra-abdominal hemorrhages are highly associated and in combination result in major blood loss.63
Computed Tomography
CT is unquestionably the diagnostic test of choice for detecting pelvic and intra-abdominal injuries. It reveals bleeding in both the peritoneal and retroperitoneal spaces. CT with intravenous contrast often can distinguish a stable hematoma from ongoing bleeding from pelvic arteries. The presence or absence of extravasated intravenous contrast material on CT scan of the pelvis is useful in predicting which patients will require therapeutic angiography71; however, its absence does not rule out ongoing pelvic bleeding: One series found the sensitivity for the detection of arterial bleeding by CT to be only 66% in patients who also underwent angiography.72 It is worth noting that with improving CT technology, its use will continue to evolve for patients with pelvic hemorrhage. Specifically, pelvic CT angiography (CTA) has been reported to not only localize active pelvic bleeding but also distinguish bleeding from an arterial versus a venous source.73,74 This is a distinction that could have great impact on the decision to perform therapeutic angiography for active arterial bleeding. Advancing CT technology will require further study to define its role in patients with pelvic hemorrhage, but it is likely that it will also be concurrently incorporated into clinical practice.
Management
The mortality rate in patients with blunt trauma who have the combination of pelvic ring fractures and hemorrhagic shock is approximately 50%.1,2 ATLS guidelines advocate the initial use of crystalloid solutions to stabilize vital signs in the trauma patient. However, when severe hypotension is present in patients with severe pelvic fracture, transfusion of blood products (including packed red blood cells, plasma, platelets, and occasionally cryoprecipitate) is crucial early in the resuscitation. Some patients appear to achieve hemodynamic stability after minimal volume infusion only to decompensate precipitously. It is important to note that case series commonly report patients with severe pelvic injury who require transfusion of packed red blood cells on the order of 10 to 20 units within the first 24 to 48 hours.
The endpoint for fluid resuscitation should be evidence of end-organ perfusion. A large body of evidence from animal studies suggests that standard volumes of crystalloid fluids typically used in traumatic hemorrhagic shock to restore normal heart rate and blood pressure lead to greater volumes of blood loss compared with low-volume resuscitation strategies that accept lower systemic blood pressures.75,76 Furthermore, in a landmark human study of hypotensive patients with penetrating chest injury, it was shown that delaying fluid resuscitation (despite systolic blood pressure below 90 mm Hg) resulted in a higher rate of discharge from the hospital than did immediate fluid resuscitation.76a
Box 55-4 details the methods for controlling hemorrhage in the ED phase of the care of patients with pelvic fractures.
Control of Hemorrhage
In addition to blood transfusion, two important therapeutic modalities for control of hemorrhage are mechanical stabilization of the pelvis and angiographic embolization. There has been some debate as to which of these modalities should take precedence, and this has been predicated on institutional availability. As a general rule, angiography with therapeutic embolization of bleeding arteries is more effective than and takes precedence over invasive external fixation.77,78
Stabilizing the Pelvis
Noninvasive Techniques.: The most readily available means to quickly stabilize the pelvis in the ED may be realized with a simple sheet and towel clamps. Wrapping the pelvis tightly with a sheet and securing this with towel clamps has been shown to be effective in reducing an open-book pelvic injury (Fig. 55-12),79,80 thereby reducing the potential volume in the pelvis for blood loss. A technique of taping the lower extremities in internal rotation has also been described as a means of achieving a closed pelvic reduction in the presence of symphyseal diastasis.81
Other commercial circumferential compression devices have been developed to facilitate noninvasive stabilization of the pelvis. Generally speaking, in cadaveric studies, it appears these devices are effective at reducing the open-book pelvis.82,83 One retrospective comparison of patients with exsanguinating pelvic hemorrhage found that patients treated with a noninvasive splinting device had substantially lower transfusion requirements than those who had formal external fixation of the pelvis performed emergently (4.9 units vs. 17.1 units in the first 24 hours, P = .008). However, there was no statistically significant change in mortality between the two groups (26% vs. 37%, P = .11).84
Invasive Fixation.: External fixation of the pelvis is performed by orthopedic surgeons. The goal of fixation is to prevent movement at pelvic fracture sites and attendant bleeding.15 Although the acute application of an external fixator has not been proved to decrease morbidity or mortality in a prospective study, there is evidence that this technique improves clinical outcome by limiting hemorrhage and restoring mechanical integrity.66 Application of the fixator is time-consuming; therefore it should not delay more definitive treatment of pelvic bleeding by angiography or the treatment of other sources of severe blood loss. The timing of the application of the external fixator requires coordination among the trauma surgeon, orthopedic surgeon, and interventional radiologist. Early surgical consultation is vital to efficient planning and prioritization of surgical management.
Many stable AP and lateral compression fractures can be treated definitively by the external fixator.15 When the pelvis is vertically displaced, traction combined with external fixation is necessary to reduce the pelvis pending definitive open surgical repair.15 Most fixators can be constructed to allow convenient surgical access to the abdomen and groin.
The pelvic C-clamp is one type of external fixation device that can theoretically be applied rapidly by the orthopedic surgeon in the ED to externally stabilize the posterior pelvic arch on an emergency basis.85 It is likely more effective in reducing AP than vertical injuries.86 Institutional practices may influence the use of C-clamp over standard external fixation. Although the C-clamp may aid in stabilizing blood loss, its application does not obviate the need for angiography.87 It is unclear whether the C-clamp offers any additional advantage over wrapping the pelvis with a sheet during initial resuscitation efforts.
Angiography and Embolization
Embolization is highly effective for controlling arterial bleeding. One case series of 556 patients undergoing pelvic angiography reported that repeat angiography was necessary in only 7.5% of patients as a result of ongoing bleeding. These authors found that hypotension, a need for more than 2 units of packed red cells, symphysis widening, and more than two arteries embolized at the first angiogram predicted the need for repeat angiography.88
Angiography is indicated when hypovolemia persists in a patient with a major pelvic fracture despite control of hemorrhage from other sources. Although it is impossible to determine whether bleeding is venous or arterial in origin until angiography is performed, one study found that inadequate response to initial resuscitation (defined as failure to maintain a systolic blood pressure above 90 mm Hg after the administration of 2 or more units of packed red cells or less) and the presence of contrast extravasation on admission CT were both indicative of active arterial bleeding.77 Although the presence of contrast extravasation on CT is an indication for angiography, the absence of contrast blush on CT is not sufficient to rule out serious pelvic bleeding.77 SI joint disruption, persistent systolic blood pressure below 100 mm Hg, and female gender were shown to be predictors of need for embolization at the time of angiography.89
The timing of angiography is individualized for each patient depending on priorities for treatment of concomitant injuries. Posterior arch disruptions are associated with the most severe hemorrhage; angiography should be considered at an early stage for these patients. Whether patients undergo angiography immediately from the ED or angiography immediately precedes laparotomy, it is important to be mindful of the logistical delay that often occurs in mobilizing the angiography team, so this intervention should be anticipated as early as possible. The transfer of the patient to the angiography suite also requires orchestrating the necessary personnel and equipment to care for the critically injured patient there. The feasibility of use of mobile angiography equipment in the ED for acutely controlling pelvic hemorrhage has been reported; this removes the usual logistic delays while ensuring a greater degree of safety in monitoring patients during the procedure.90
Hemodynamically Unstable Patients with Pelvic and Intra-abdominal Hemorrhage
Patients who hemorrhage from both the pelvis and the abdomen have mortality rates above 40% and deserve special consideration. These patients may be too unstable to undergo CT imaging. Prioritizing the need for laparotomy versus angiography in these patients may be challenging when the need for laparotomy is based on the detection of intra-abdominal fluid by FAST or DPL. Unnecessary laparotomy performed in patients who are hemodynamically unstable with pelvic fracture has been shown to contribute to high mortality rates.91 Therefore in these cases, it is crucial that the efforts of the general surgeon, orthopedic surgeon, and interventional radiologist be coordinated to optimize the timing of necessary procedures.
Gross aspirates of blood on DPL are strong indicators for prompt laparotomy. Given the high rates of false-negative FAST examinations in pelvic trauma, caution should be used in making difficult triage decisions regarding laparotomy versus angiography on the basis of FAST findings in this setting. However, when the FAST examination does reveal hemoperitoneum, it is generally accepted that laparotomy be pursued first.92 When concurrent pelvic bleeding is highly suggested (e.g., severe open-book pelvis), it is advisable that angiography promptly follow laparotomy.
At the time of laparotomy, it may be appropriate for the orthopedic surgeon to place either an external fixator or a pelvic C-clamp. Packing of the pelvis at the time of laparotomy has been reported as a means to obtain hemostasis in pelvic hemorrhage.93,94 Although there is limited evidence from clinical studies to support packing, it has become a mainstay of treating pelvic hemorrhage at some centers, especially in Europe. Part of the rationale for use of packing rather than angiography is the fact that pelvic bleeding is commonly venous in origin, for which arteriography is useless. In contrast, packing may aid in tamponading bleeding from the posterior venous plexus. It is recommended that the pelvis be stabilized before packing to provide solid structural support against which packing may be performed.94 Intraperitoneal, retroperitoneal, and extraperitoneal techniques of packing have been described, with authors reporting retroperitoneal and extraperitoneal approaches being rapidly done even in the ED setting.94,95 A systematic review of pelvic packing concluded that for patients with hemodynamic instability caused by pelvic hemorrhage, packing could be used as a temporizing measure for control of bleeding until more selective treatments could be performed.96
For any trauma center, planning for challenging clinical situations by emergency physicians, trauma surgeons, and angiographers and the creation of protocols for care may be useful in optimizing a timely and coordinated response.78,97,98
Acetabular Fractures
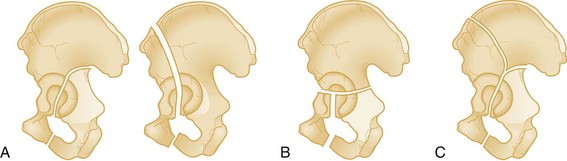
Acetabular fractures are broadly classified into three types15 (Fig. 55-13 and Box 55-5).
Type C fractures are readily apparent on plain radiographs as a result of disruption of the ilium.
Assessment of the AP pelvic radiograph should focus on the disruption of the ilioischial and iliopectineal lines as well as the anterior and posterior lips of the acetabulum (Fig. 55-14). Ramus fractures should be evaluated for possible extension into the acetabulum. Oblique views of the acetabulum (Judet views) can aid in visualizing the anterior and posterior columns. CT is, without question, the imaging test of choice for visualizing acetabular fractures and planning for possible surgical repair. It is important to note that because fracture of the acetabulum often occurs with a high-energy mechanism, even patients with isolated acetabular fractures may have significant hemorrhage necessitating blood transfusion.99 All patients with acetabular fracture require orthopedic referral in the emergency department.
Coccyx Fractures
Fractures of the coccyx occur frequently after a fall in the sitting position or a kick. Fracture and injury also may occur during parturition. Physical examination reveals local tenderness to palpation in the gluteal crease, with pain and sometimes abnormal motion of the coccyx during palpation on DRE. Normally, the tip of the coccyx moves 30 degrees anteriorly and 1 cm laterally.100 Displacement also is diagnosed on rectal examination, but attempts at reduction are not recommended.
Treatment of coccygeal fracture consists of bed rest, stool softeners, analgesia, and sitz baths to relieve muscle spasm. As activity is increased, maneuvers that may minimize discomfort include use of an inflatable rubber donut cushion, alternate sitting on the side of each buttock, slouching to displace body weight more proximally, and sitting on a hard chair rather than a soft one (sinking into a soft chair may distribute weight onto the coccyx).100 Because of muscle action on the fragment, healing is slow and patients should be cautioned that discomfort may be prolonged. In the case of persistent severe disability, an orthopedic consultation is indicated for considerations of local steroid injection or possible coccygectomy.101 Other causes of coccydynia (besides fracture) include trauma during parturition; faulty posture; midline disk herniations (caused by nonsegmental referral of pain from irritation of the dura); lumbar facet arthropathy; compression of the first, fourth, and fifth sacral roots; neuralgia from sacral plexopathy or sacrococcygeal neuropathy; infections; and local tumors.100
References
1. Balogh, Z, et al. The epidemiology of pelvic ring fractures: A population-based study. J Trauma. 2007;63:1066.
2. Demetriades, D, et al. Pelvic fractures: Epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002;195:1.
3. O’Sullivan, RE, White, TO, Keating, JF. Major pelvic fractures: Identification of patients at high risk. J Bone Joint Surg Br. 2005;87:530.
4. Starr, AJ, et al. Pelvic ring disruptions: Prediction of associated injuries, transfusion requirement, pelvic arteriography, complications, and mortality. J Orthop Trauma. 2002;16:553.
5. Smith, W, et al. Early predictors of mortality in hemodynamically unstable pelvis fractures. J Orthop Trauma. 2007;21:31.
6. Giannoudis, PV, et al. Prevalence of pelvic fractures, associated injuries, and mortality: The United Kingdom perspective. J Trauma. 2007;63:875–883.
7. Sathy, AK, Starr, AJ, Smith, WR. The effect of pelvic fracture on mortality after trauma: An analysis of 63,000 trauma patients. J Bone Joint Surg Am. 2009;91:2803–2810.
8. Schulman, JE, et al. Pelvic ring fractures are an independent risk factor for death after blunt trauma. J Trauma. 2010;68:930–934.
9. Henry, SM, Pollak, AN, Jones, AL, Boswell, S, Scalea, TM. Pelvic fracture in geriatric patients: A distinct clinical entity. J Trauma. 2002;53:15.
10. Hauschild, O, et al. Mortality in patients with pelvic fractures: Results from the German pelvic injury register. J Trauma. 2008;64:449–455.
11. Eastridge, BJ, Burgess, AR. Pedestrian pelvic fractures: 5-year experience of a major urban trauma center. J Trauma. 1997;42:695.
12. Rowe, SA, Sochor, MS, Staples, KS, Wahl, WL, Wang, SC. Pelvic ring fractures: Implications of vehicle design, crash type, and occupant characteristics. Surgery. 2004;136:842.
13. Stein, DM, et al. Risk factors associated with pelvic fractures sustained in motor vehicle collisions involving newer vehicles. J Trauma. 2006;61:21.
14. Inaba, K, Sharkey, PW, Stephen, DJ, Redelmeier, DA, Brenneman, FD. The increasing incidence of severe pelvic injury in motor vehicle collisions. Injury. 2004;35:759.
15. Tile, M. Fractures of the Pelvis and Acetabulum, 3rd ed. Philadelphia: Lippincott, Williams & Wilkins; 2003.
16. Burgess, AR, et al. Pelvic ring disruptions: Effective classification system and treatment protocols. J Trauma. 1990;30:848.
17. Furey, AJ, et al. Classification of pelvic fractures: Analysis of inter- and intraobserver variability using the Young-Burgess and Tile classification systems. Orthopedics. 2009;32:401.
18. Koo, H, et al. Interobserver reliability of the Young-Burgess and Tile classification systems for fractures of the pelvic ring. J Orthop Trauma. 2008;22:379–384.
19. Dalal, SA, et al. Pelvic fracture in multiple trauma: Classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29:781.
20. Manson, T, et al. Young-Burgess classification of pelvic ring fractures: Does it predict mortality, transfusion requirements, and non-orthopaedic injuries? J Orthop Trauma. 2010;24:603–609.
21. Gertzbein, SD, Chenoweth, DR. Occult injuries of the pelvic ring. Clin Orthop Relat Res. 1977;128:202.
22. Cosker, TD, Ghandour, A, Gupta, SK, Tayton, KJ. Pelvic ramus fractures in the elderly: 50 patients studied with MRI. Acta Orthop. 2005;76:513.
23. Abrassart, S, Stern, R, Peter, R. Morbidity associated with isolated iliac wing fractures. J Trauma. 2009;66:200–203.
24. Duchesne, JC, et al. Open-book pelvic fractures with perineal open wounds: A significant morbid combination. Am Surg. 2009;75:1227–1233.
25. Gibbons, KJ, Soloniuk, DS, Razazk, N. Neurologic injury and patterns of sacral fractures. J Neurosurg. 1990;72:889.
26. Rogers, LF, Bradd, FJ, Kennedy, W. Radiology of Skeletal Trauma. New York: Churchill Livingstone; 1992.
27. Mattila, VM, Niva, M, Kiuru, M, Pihlajamäki, H. Risk factors for bone stress injuries: A follow-up study of 102,515 person-years. Med Sci Sports Exerc. 2007;39:1061.
28. Kiuru, MJ, Pihlajamaki, HK, Hietanen, HJ, Ahovuo, JA. MR imaging, bone scintigraphy, and radiography in bone stress injuries of the pelvis and the lower extremity. Acta Radiol. 2002;43:207.
29. Denis, F, Davis, S, Comfort, T. Sacral fractures: An important problem. Clin Orthop Relat Res. 1988;227:67.
30. Grotz, MR, et al. Open pelvic fractures: Epidemiology, current concepts of management and outcome. Injury. 2005;36:1.
31. Dente, CJ, et al. The outcome of open pelvic fractures in the modern era. Am J Surg. 2005;190:830.
32. Lunsjo, K, Abu-Zidan, FM. Does colostomy prevent infection in open blunt pelvic fractures? A systematic review. J Trauma. 2006;60:1145.
33. Duncan, AO, et al. Management of transpelvic gunshot wounds. J Trauma. 1989;29:1335.
34. Malangoni, MA, Miller, FB, Cryer, HM, Mullins, RJ, Richardson, JD. The management of penetrating pelvic trauma. Am Surg. 1990;56:61.
35. O’brien, DP, et al. Pelvic fracture in the elderly is associated with increased mortality. Surgery. 2002;132:710.
36. Dechert, TA, Duane, TM, Frykberg, BP. Elderly patients with pelvic fracture: Interventions and outcomes. Am Surg. 2009;75:291–295.
37. McCormick, JP, Morgan, SJ, Smith, WR. Clinical effectiveness of the physical examination in diagnosis of posterior pelvic ring injuries. J Orthop Trauma. 2003;17:257.
38. Metze, M, Tiemann, AH, Josten, C. Male sexual dysfunction after pelvic fracture. J Trauma. 2007;63:394–401.
39. Black, PC, Miller, EA, Porter, JR, Wessells, H. Urethral and bladder neck injury associated with pelvic fracture in 25 female patients. J Urol. 2006;175:2140.
40. Carter, CT, Schafer, N. Incidence of urethral disruption in females with traumatic pelvic fractures. Am J Emerg Med. 1993;11:218.
41. Avey, G, Blackmore, CC, Wessells, H, Wright, JL, Talner, LB. Radiographic and clinical predictors of bladder rupture in blunt trauma patients with pelvic fracture. Acad Radiol. 2006;13:573.
42. Basta, AM, Blackmore, CC, Wessells, H. Predicting urethral injury from pelvic fracture patterns in male patients with blunt trauma. J Urol. 2007;177:571–575.
43. Spencer Netto, FA, et al. Retrograde urethrocystography impairs computed tomography diagnosis of pelvic arterial hemorrhage in the presence of a lower urologic tract injury. J Am Coll Surg. 2008;206:322–327.
44. Reference deleted in proofs.
45. Schmal, H, Hauschild, O, Culemann, U. Identification of risk factors for neurological deficits in patients with pelvic fractures. Orthopedics. 2010;33:8.
46. Copeland, CE, et al. Effect of trauma and pelvic fracture on female genitourinary, sexual, and reproductive function. J Orthop Trauma. 1997;11:73.
47. Papadopoulos, IN, et al. Auditing 655 fatalities with pelvic fractures by autopsy as a basis to evaluate trauma care. J Am Coll Surg. 2006;203:30.
48. Lunsjo, K, et al. Associated injuries and not fracture instability predict mortality in pelvic fractures: A prospective study of 100 patients. J Trauma. 2007;62:687.
49. Gustavo Parreira, J, et al. The role of associated injuries on outcome of blunt trauma patients sustaining pelvic fractures. Injury. 2000;31:677.
50. Ochsner, MG, Jr., et al. Associated aortic rupture-pelvic fracture: An alert for orthopedic and general surgeons. J Trauma. 1992;33:429.
51. Gonzalez, RP, Fried, PQ, Bukhalo, M. The utility of clinical examination in screening for pelvic fractures in blunt trauma. J Am Coll Surg. 2002;194:121.
52. Salvino, CK, et al. Routine pelvic x-ray studies in awake blunt trauma patients: A sensible policy? J Trauma. 1992;33:413.
53. Koury, HI, Peschiera, JL, Welling, RE. Selective use of pelvic roentgenograms in blunt trauma patients. J Trauma. 1993;34:236.
54. Duane, TM, Dechert, T, Wolfe, LG. Clinical examination is superior to plain films to diagnose pelvic fractures compared to CT. Am Surg. 2008;74:476–479.
55. Kessel, B, et al. Is routine portable pelvic x-ray in stable multiple trauma patients always justified in a high technology era? Injury. 2007;38:559.
56. Guillamondegui, OD, et al. Pelvic radiography in blunt trauma resuscitation: A diminishing role. J Trauma. 2002;53:1043.
57. Lunsjo, K, Tadros, AM, Hauggaard, A. Acute plain anterioposterior radiograph of the pelvis is not useful in detecting fractures of iliac wing and os sacrum: A prospective study of 73 patients using CT as gold standard. Australas Radiol. 2007;51:147–149.
58. Resnik, CS, Stackhouse, DJ, Shanmuganathan, K, Young, JW. Diagnosis of pelvic fractures in patients with acute pelvic trauma: Efficacy of plain radiographs. AJR Am J Roentgenol. 1992;158:109.
59. Dormagen, JB, Tötterman, A, Røise, O, Sandvik, L, Kløw, NE. Efficacy of plain radiography and computer tomography in localizing the site of pelvic arterial bleeding in trauma patients. Acta Radiol. 2010;51:107–116.
60. Fu, CY, Wu, SC, Chen, RJ. Evaluation of pelvic fracture stability and the need for angioembolization: Pelvic instabilities on plain film have an increased probability of requiring angioembolization. Am J Emerg Med. 2009;27:792–796.
61. Cryer, HM, Miller, FB, Evers, BM, Rouben, LR, Seligson, DL. Pelvic fracture classification: Correlation with hemorrhage. J Trauma. 1988;28:973.
62. Blackmore, CC, et al. Predicting major hemorrhage in patients with pelvic fracture. J Trauma. 2006;61:346.
63. Eastridge, BJ, Starr, A, Minei, JP, O’Keefe, GE, Scalea, TM. The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. J Trauma. 2002;53:446.
64. Deunk, J, Dekker, HM, Brink, M. The value of indicated computed tomography scan of the chest and abdomen in addition to the conventional radiologic work-up for blunt trauma patients. J Trauma. 2007;63:757–763.
65. Deunk, J, Brink, M, Dekker, HM. Routine versus selective computed tomography of the abdomen, pelvis, and lumbar spine in blunt trauma: A prospective evaluation. J Trauma. 2009;66:1108–1117.
66. Dyer, GS, Vrahas, MS. Review of the pathophysiology and acute management of haemorrhage in pelvic fracture. Injury. 2006;37:602.
67. Mendez, C, Gubler, KD, Maier, RV. Diagnostic accuracy of peritoneal lavage in patients with pelvic fractures. Arch Surg. 1994;129:477.
68. Friese, RS, Malekzadeh, S, Shafi, S, Gentilello, LM, Starr, A. Abdominal ultrasound is an unreliable modality for the detection of hemoperitoneum in patients with pelvic fracture. J Trauma. 2007;63:97.
69. Tayal, VS, et al. Accuracy of trauma ultrasound in major pelvic injury. J Trauma. 2006;61:1453.
70. Hoffman, L, Pierce, D, Puumala, S. Clinical predictors of injuries not identified by focused abdominal sonogram for trauma (FAST) examinations. J Emerg Med. 2009;36:271–279.
71. Brasel, KJ, Pham, K, Yang, H, Christensen, R, Weigelt, JA. Significance of contrast extravasation in patients with pelvic fracture. J Trauma. 2007;62:1149.
72. Hagiwara, A, et al. Predictors of death in patients with life-threatening pelvic hemorrhage after successful transcatheter arterial embolization. J Trauma. 2003;55:696.
73. Uyeda, J, Anderson, SW, Kertesz, J. Pelvic CT angiography: Application to blunt trauma using 64MDCT. Emerg Radiol. 2010;17:131–137.
74. Uyeda, JW, Anderson, SW, Sakai, O. CT angiography in trauma. Radiol Clin North Am. 2010;48:423–438.
75. Stern, SA. Low-volume fluid resuscitation for presumed hemorrhagic shock: Helpful or harmful? Curr Opin Crit Care. 2001;7:422.
76. Revell, M, Greaves, I, Porter, K. Endpoints for fluid resuscitation in hemorrhagic shock. J Trauma. 2003;54(5 Suppl):S63.
76a. Bickell, WH, Wall, MJ, Pepe, PE. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105–1109.
77. Miller, PR, Moore, PS, Mansell, E, Meredith, JW, Chang, MC. External fixation or arteriogram in bleeding pelvic fracture: Initial therapy guided by markers of arterial hemorrhage. J Trauma. 2003;54:437.
78. Biffl, WL, et al. Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg. 2001;233:843.
79. Routt, ML, Jr., Falicov, A, Woodhouse, E, Schildhauer, TA. Circumferential pelvic antishock sheeting: A temporary resuscitation aid. J Orthop Trauma. 2006;20(1 Suppl):S3.
80. Nunn, T, Cosker, TD, Bose, D, Pallister, I. Immediate application of improvised pelvic binder as first step in extended resuscitation from life-threatening hypovolaemic shock in conscious patients with unstable pelvic injuries. Injury. 2007;38:125.
81. Gardner, MJ, Parada, S, Chip Routt, ML, Jr. Internal rotation and taping of the lower extremities for closed pelvic reduction. J Orthop Trauma. 2009;23:361–364.
82. Knops, SP, Schep, NW, Spoor, CW. Comparison of three different pelvic circumferential compression devices: A biomechanical cadaver study. J Bone Joint Surg Am. 2011;93:230–240.
83. DeAngelis, NA, Wixted, JJ, Drew, J. Use of the trauma pelvic orthotic device (T-POD) for provisional stabilisation of anterior-posterior compression type pelvic fractures: A cadaveric study. Injury. 2008;39:903–906.
84. Croce, MA, Magnotti, LJ, Savage, SA, Wood, GW, 2nd., Fabian, TC. Emergent pelvic fixation in patients with exsanguinating pelvic fractures. J Am Coll Surg. 2007;204:935.
85. Archdeacon, MT, Hiratzka, J. The trochanteric C-clamp for provisional pelvic stability. J Orthop Trauma. 2006;20:47.
86. Archdeacon, MT, Safian, C, Le, TT. A cadaver study of the trochanteric pelvic clamp for pelvic reduction. J Orthop Trauma. 2007;21:38.
87. Sadri, H, Nguyen-Tang, T, Stern, R, Hoffmeyer, P, Peter, R. Control of severe hemorrhage using C-clamp and arterial embolization in hemodynamically unstable patients with pelvic ring disruption. Arch Orthop Trauma Surg. 2005;125:443.
88. Gourlay, D, Hoffer, E, Routt, M, Bulger, E. Pelvic angiography for recurrent traumatic pelvic arterial hemorrhage. J Trauma. 2005;59:1168.
89. Salim, A, Teixeira, PG, DuBose, J. Predictors of positive angiography in pelvic fractures: A prospective study. J Am Coll Surg. 2008;207:656–662.
90. Morozumi, J, Homma, H, Ohta, S. Impact of mobile angiography in the emergency department for controlling pelvic fracture hemorrhage with hemodynamic instability. J Trauma. 2010;68:90–95.
91. Verbeek, D, Sugrue, M, Balogh, Z. Acute management of hemodynamically unstable pelvic trauma patients: Time for a change? Multicenter review of recent practice. World J Surg. 2008;32:1874–1882.
92. Heetveld, MJ, Harris, I, Schlaphoff, G, Sugrue, M. Guidelines for the management of haemodynamically unstable pelvic fracture patients. ANZ J Surg. 2004;74:520.
93. Cothren, CC, et al. Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: A paradigm shift. J Trauma. 2007;62:834.
94. Tötterman, A, Madsen, JE, Skaga, NO, Røise, O. Extraperitoneal pelvic packing: A salvage procedure to control massive traumatic pelvic hemorrhage. J Trauma. 2007;62:843.
95. Suzuki, T, Smith, WR, Moore, EE. Pelvic packing or angiography: Competitive or complementary? Injury. 2009;40:343–353.
96. Papakostidis, C, Giannoudis, PV. Pelvic ring injuries with haemodynamic instability: Efficacy of pelvic packing, a systematic review. Injury. 2009;40(Suppl 4):S53–S61.
97. Jeske, HC, Larndorfer, R, Krappinger, D. Management of hemorrhage in severe pelvic injuries. J Trauma. 2010;68:415–420.
98. Davis, JW, Moore, FA, McIntyre, RC, Jr. Western trauma association critical decisions in trauma: Management of pelvic fracture with hemodynamic instability. J Trauma. 2008;65:1012–1015.
99. Magnussen, RA, Tressler, MA. Predicting blood loss in isolated pelvic and acetabular high-energy trauma. J Orthop Trauma. 2007;21:603–607.
100. Traycoff, RB, Crayton, H, Dodson, R. Sacrococcygeal pain syndromes: Diagnosis and treatment. Orthopedics. 1989;12:1373.
101. Maigne, JY, Lagauche, D, Doursounian, L. Instability of the coccyx in coccydynia. J Bone Joint Surg Br. 2000;82:1038.