CHAPTER 79 Pelvic girdle and lower limb: overview and surface anatomy
This chapter is made up of two sections. The first is an overview of the general organization of the lower limb, with particular emphasis on the fascial skeleton, distribution of the major blood vessels and lymphatic channels, and the branches of the lumbar and sacral plexuses: it is intended to complement the detailed regional anatomy described in Chapters 80 to 84 Chapter 81 Chapter 82 Chapter 83 Chapter 84. The second section describes the surface anatomy of the lower limb.
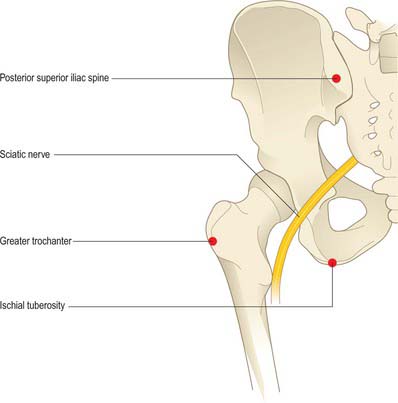
The structure of the lower limb is determined by its adaptations for weightbearing, locomotion and the maintenance of equilibrium (stability). Indeed, the adaptations for weightbearing and for stability, and the differing developmental histories of the limbs account for the major structural and functional differences between the upper and lower limbs. The inguinal (pelvicrural) and gluteal (buttock) regions are important anatomical junctional zones between the trunk and the lower limb through which longitudinally running nerves and vessels may pass in either direction. The inguinal region includes the junctional zones between the limb and abdominal cavity via the myopectineal orifice (the gap between the inguinal ligament and hip bone), and between the limb and pelvic cavity via the obturator foramen. The gluteal region includes the junctional zones between the limb and the abdominopelvic cavity via the greater sciatic foramen, and between the limb and the perineum via the lesser sciatic foramen (Fig. 79.1).
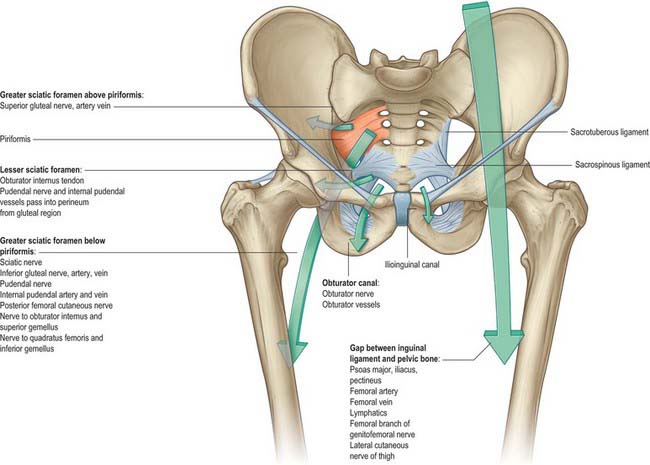
Fig. 79.1 Gateways from the abdomen, pelvis and perineum to the lower limb.
(From Drake, Vogl and Mitchell 2005.)
SKIN, FASCIA AND SOFT TISSUES
Fascial skeleton
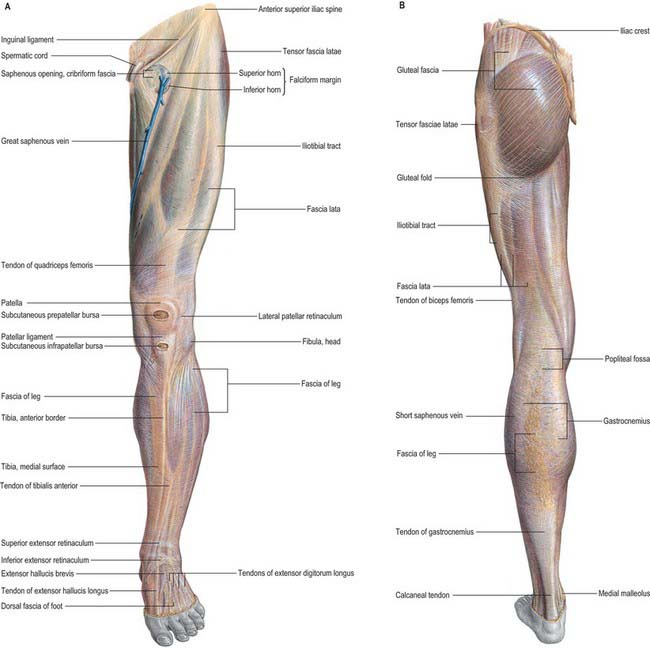
The ‘fascial skeleton’ (deep fascia) of the lower limb is well-defined and forms a tough circumferential ‘stocking-like’ structure that constrains the musculature (Fig. 79.2). Septa pass from the deep surface of this fascial sheath to the bones within, confining the functional muscle groups within osteofascial compartments. The tough fascia gives additional areas of attachment to the muscles and ensures that they work to maximal effect. Thickenings in the ensheathing layer may act as additional tendons (e.g. iliotibial tract). Elsewhere, thickenings in the fascial skeleton form fibrous retinacula where tendons cross joints. Although they are particularly prominent in the embalmed cadaver, these fascial layers are also readily demonstrable in the living, and are of considerable functional significance. The pattern of soft-tissue organization has a bearing on the physiological effects of the muscles and is crucial for efficient venous return from the limb. The fascial planes also control and direct the spread of pathological fluids (blood, pus) within the limb and play an important part in determining the degree and direction of displacement seen in long bone fractures.
Osteofascial compartments in the lower limb
The muscles of the thigh may be grouped into three compartments according to their function, namely anterior (extensor), posterior (flexor) and medial (adductor): only the anterior and posterior compartments possess distinct fascial boundaries. A very definite fascial separation into anterior (extensor), posterior (flexor) and lateral (evertor) compartments exists in the leg, and compartment syndrome is most common in this region (see below). Osteofascial compartments in the foot are described in Chapter 84.
The fascial boundaries that limit the osteofascial compartments are largely inelastic, which means that any condition that leads to an increase in the volume of the compartmental contents, e.g. muscle swelling caused by trauma or unaccustomed overuse, haemorrhage and local infection, is likely to cause an increase in intracompartmental pressure. If unrelieved, this increased pressure will lead to compressive occlusion of the vessels in the compartment and consequent ischaemic damage to the nerves and muscles of the compartment, a phenomenon known as compartment syndrome.
BONES AND JOINTS
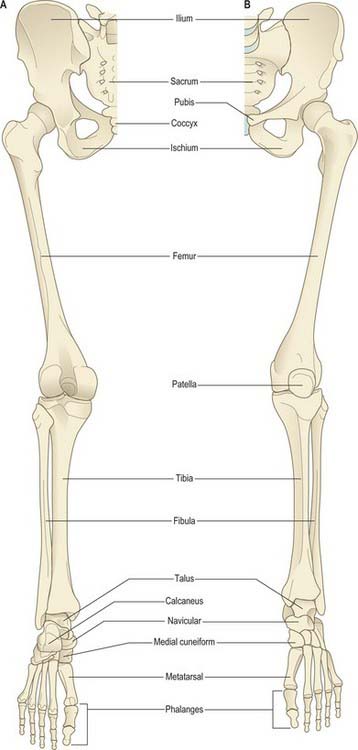
The bones of the lower limb are the three fused components of the pelvic girdle; the femur and patella (thigh); the tibia and fibula (leg); the tarsus, metatarsus and phalanges (foot) (Fig. 79.3). The hip bones (especially the ilium and ischium), femur, tibia and bones of the hindfoot are strong and their external (cortical) and internal (trabecular) structure is adapted for weightbearing.
MUSCLES
The muscles of the thigh lie in three functional compartments. The anterior or extensor compartment includes sartorius and the quadriceps group. Sartorius and rectus femoris are attached proximally to the pelvis and can thus act on the hip joint as well as on the knee, whereas the vasti are attached proximally to the femoral shaft, and, acting as a unit, are powerful knee extensors. The medial or adductor compartment contains the named adductor muscles and gracilis; pectineus may also be included. These muscles are attached proximally to the anterior aspect of the pelvis, and distally to the femur; gracilis has no femoral attachment, being attached distally to the proximal tibia, while a part of adductor magnus has a proximal attachment to the ischial tuberosity. The posterior (‘hamstring’) compartment includes semitendinosus, semimembranosus and biceps femoris. These muscles are attached proximally to the ischial tuberosity and act both to extend the trunk on the femur and to flex and rotate the knee. Adductor magnus, as may be inferred from the extent of its proximal attachment and its dual innervation, shares the first of these functions with the hamstrings. Biceps femoris is the only muscle of the thigh that is attached distally to the fibula, and has no tibial attachment.
Gastrocnemius, plantaris and popliteus are the only muscles of the leg that are attached proximally to the femur and they can therefore act on the knee as well as at the ankle. The remaining leg muscles are attached proximally to the tibia, fibula or both, and to the interosseous membrane. The intrinsic muscles of the sole of the foot are arranged in layers. They facilitate the actions of the long flexors of the toes, and by effecting subtle changes in the shape of the foot they help control foot posture in stance and locomotion.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ARTERIAL SUPPLY
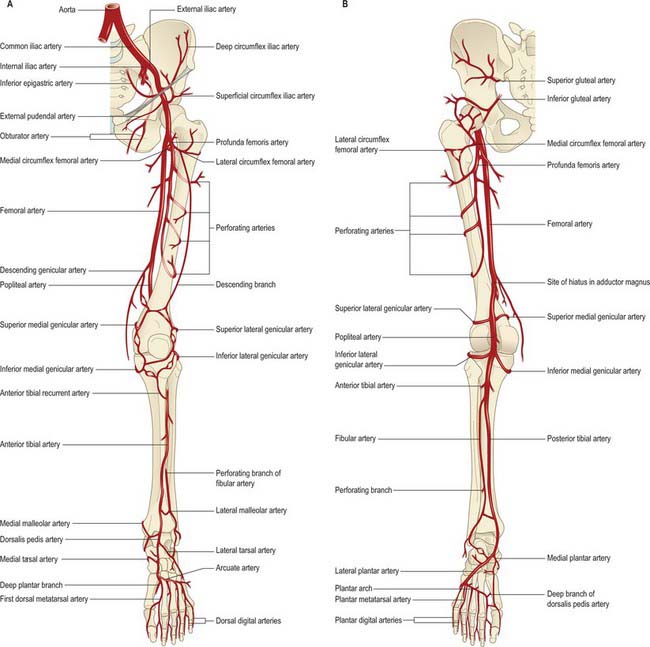
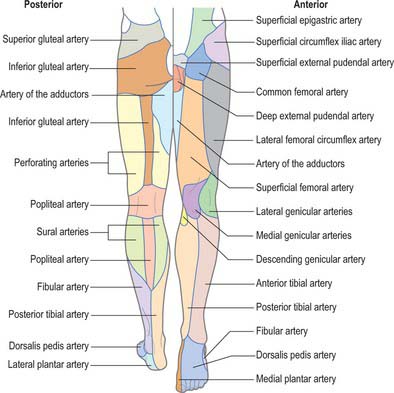
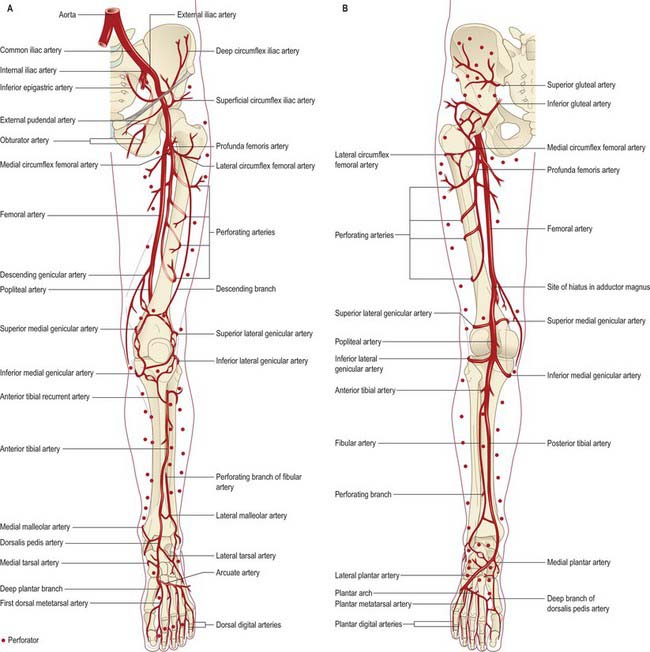
The femoral artery (the continuation of the external iliac artery) provides the principal arterial supply to the lower limb distal to the inguinal ligament and the gluteal fold (Figs 79.4, 79.5). The femoral artery courses within the anteromedial aspect of the thigh, becoming the popliteal artery on entering the posterior compartment of the thigh and dividing into its terminal branches in the posterior compartment of the leg. The obturator and inferior gluteal vessels also contribute to the supply of the proximal part of the limb. In the embryo the inferior gluteal artery supplied the main axial artery of the limb, which is represented in the adult by the arteria comitans nervi ischiadici (artery to the sciatic nerve).
The bones of the lower limb receive their arterial supply from nutrient vessels, metaphysial arterial branches of the peri-articular anastomoses, and the arteries supplying the muscles that attach to their periosteum. The pattern of arterial supply is particularly relevant to fracture healing, the spread of infection and malignancy, and to the planning of reconstructive surgical procedures. For further details consult Cormack & Lamberty (1994), Taylor & Razaboni (1994) and Crock (1996).
Arterial perforators of the lower limb
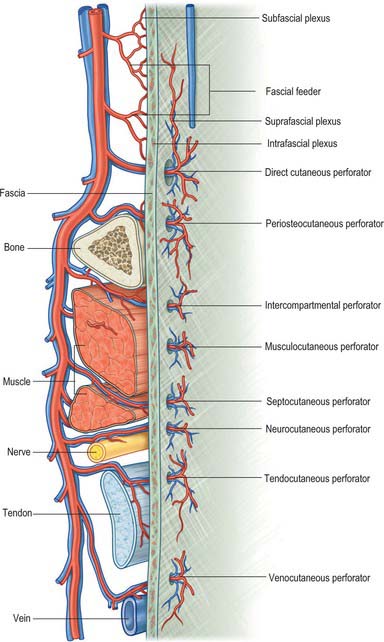
Achieving adequate and aesthetically satisfactory skin and soft tissue cover for large, superficial tissue defects is a perennial challenge in the field of plastic and reconstructive surgery, and accounts for a substantial part of the plastic surgeon’s workload. Generally, split-thickness and full-thickness skin grafts are suitable only for very superficial defects. To achieve tissue cover for deeper and larger tissue defects, the plastic surgeon employs one of a variety of autologous tissue flaps. The viability of a flap transplanted from one part of the body to another is crucially dependent on the blood supply of the flap. An appreciation of the angiosome concept (see Ch. 6), coupled with technological advances in reconstructive microsurgery, has stimulated the development and use of perforator (or perforator-based) flaps. These are flaps of skin or subcutaneous tissue supplied by one or more fascial ‘perforators’, i.e. arteries which reach the suprafascial plexus either directly from a source vessel, or indirectly from some other neighbouring tissue (Fig. 79.6). Perforator-based flaps are typically harvested with sparing of underlying muscle tissue and minimal trauma: their use is said to reduce postoperative pain, donor site morbidity and functional loss.
In the context of perforator flap surgery, the lower limb may be considered in terms of four anatomic regions: gluteal; anterior hip and thigh; knee and leg; ankle and foot. Each lower limb accounts for approximately 23% of the total body surface area (thigh 10.5%, leg 6.5%, buttock 2.5% and foot 3.5%) and contains an average of 90 arterial perforators (Fig. 79.7).
VENOUS DRAINAGE
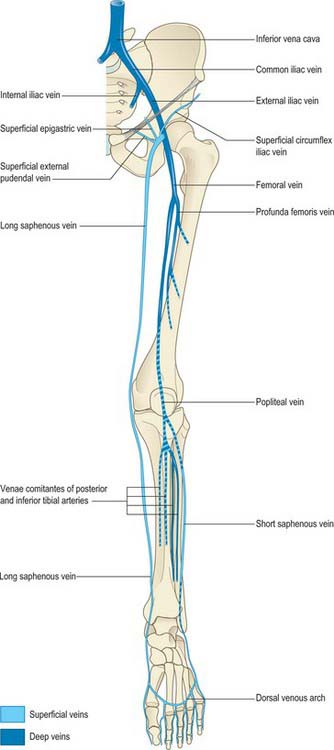
The veins of the lower limb can be subdivided, like those of the upper limb, into superficial and deep groups (Figs 79.8, 79.9). The superficial veins are subcutaneous and lie in the superficial fascia; the deep veins (beneath the deep fascia) accompany the major arteries. Valves are present in both groups, but are more numerous in the deep veins. (Valves are more numerous in the veins of the lower limb than in the veins of the upper limb.) Venous plexuses occur within and between some of the lower limb muscles. The principal named superficial veins are the long and short saphenous veins; their numerous tributaries are mostly unnamed. For details and variations consult Kosinski (1926).
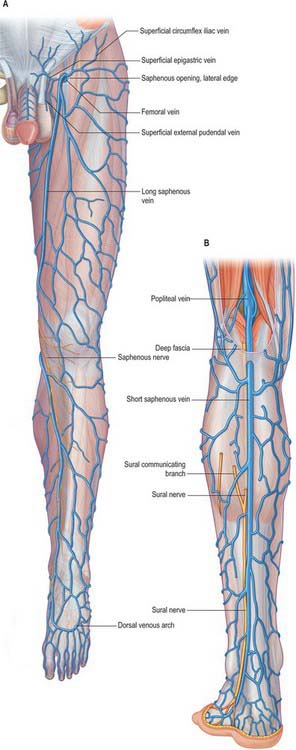
Fig. 79.9 A, The long saphenous vein and its tributaries. B, The short saphenous vein and its tributaries.
Venous (muscle) pumps
In a standing position, venous return from the lower limb depends largely on muscular activity, especially contraction of the calf and foot muscles, known as the ‘muscle pump’, whose efficiency is aided by the tight sleeve of deep fascia. ‘Perforating’ veins connect the long saphenous vein with the deep veins, particularly near the ankle, distal calf and knee. Their valves are arranged so as to prevent flow of blood from the deep to the superficial veins. At rest, pressure in a superficial vein is equal to the height of the column of blood extending from that vein to the heart. When calf muscles contract, blood is pumped proximally in the deep veins and is normally prevented from flowing into the superficial veins by the valves in the perforating veins. During muscular relaxation, blood is drawn into the deep veins from the superficial veins. If the valves in the perforating veins become incompetent, these veins become sites of ‘high pressure leaks’ during muscular contraction, and the superficial veins become dilated and varicose. Similar perforating connections occur in the anterolateral region, where varicosities may also occur. Valvar incompetence in the connecting veins between the long saphenous vein and femoral vein in the adductor canal may predispose to superficial varicosities in the medial aspect of the thigh (Dodd & Cockett 1976).
LYMPHATIC DRAINAGE
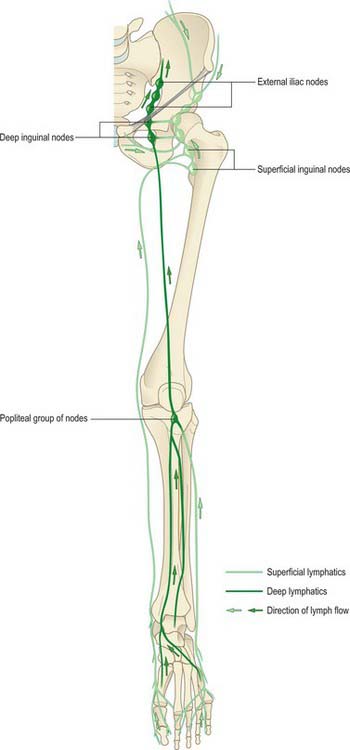
Most lymph from the lower limb traverses a large intermediary inguinal group of nodes (Fig. 79.10). Peripheral nodes are few and all are deeply sited. Except for an inconsistent node lying proximally on the interosseous membrane near the anterior tibial vessels, they occur only in the popliteal fossa. Enlarged popliteal nodes may be palpated along the line of the popliteal vessels while the passively supported knee is gradually moved from extension to semi-flexion. Inguinal nodes are found superficial and deep to the deep fascia. The deep nodes are few and lie alongside the medial aspect of the femoral vein. The superficial nodes may be divided into a lower vertical group that clothe the proximal part of the long saphenous vein, and an upper group that lie parallel to, but below, the inguinal ligament and which are related to the superficial circumflex iliac and superficial external pudendal vessels. Lymph from the lower limb passes from the inguinal nodes to the external and common iliac nodes, and ultimately drains to the lateral aortic group. Deep gluteal lymph reaches the same group through the internal and common iliac chains.
INNERVATION
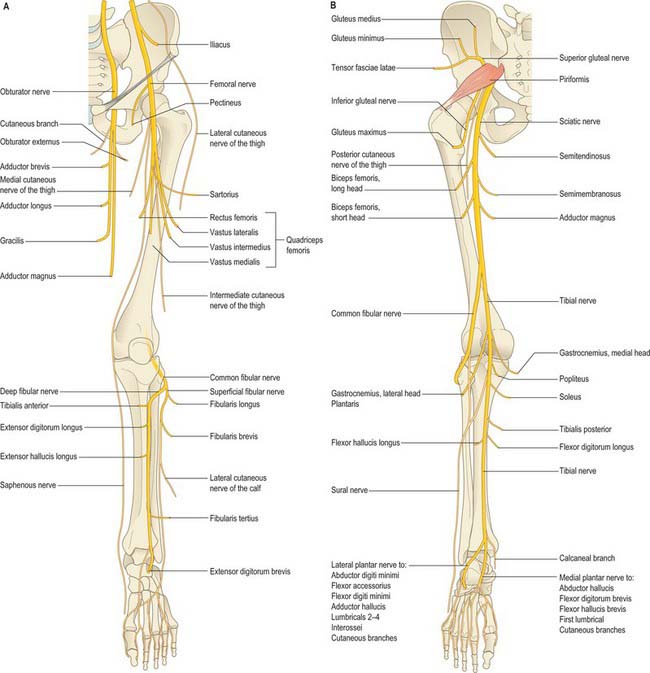
OVERVIEW OF THE LUMBAR AND SACRAL PLEXUSES
Nerves derived from the lumbar and sacral plexuses innervate the lower limb (Figs 79.11). The lumbar plexus lies deep within psoas major, anterior to the transverse processes of the first three lumbar vertebrae. The sacral plexus lies in the pelvis on the anterior surface of piriformis, external to the pelvic fascia, which separates it from the inferior gluteal and pudendal vessels. The lumbosacral trunk (L4 and L5) emerges medial to psoas major on the posterior abdominal wall and lies on the ala of the sacrum before crossing the pelvic brim to join the ventral ramus of S1.
OVERVIEW OF THE PRINCIPAL NERVES OF THE LOWER LIMB
Femoral nerve (L2–4)
The femoral nerve is the nerve of the anterior compartment of the thigh. It arises from the posterior divisions of the second to fourth lumbar ventral rami, descends through psoas major and emerges on its lateral border to pass between psoas and iliacus. It enters the thigh behind the inguinal ligament and lateral to the femoral sheath. Its terminal branches form in the femoral triangle about 2 cm distal to the inguinal ligament. In the abdomen the nerve supplies small branches to iliacus and a branch to the proximal part of the femoral artery. It subsequently supplies a large cutaneous area on the anterior and medial thigh, medial leg and foot, and gives articular branches to the hip and knee. The femoral nerve is described in detail on page 1383.
Obturator nerve (L2–4)
The obturator nerve is the nerve of the medial compartment of the thigh. It arises from the anterior divisions of the second to fourth lumbar ventral rami, descends through psoas major and emerges from its medial border at the pelvic brim. It crosses the sacroiliac joint behind the common iliac artery and lateral to the internal iliac vessels, runs along the lateral pelvic wall medial to obturator internus, and enters the thigh through the upper part of the obturator foramen. Near the foramen it divides into anterior and posterior branches which are separated at first by part of obturator externus and more distally by adductor brevis. It gives articular branches to the hip and knee, and may supply skin on the medial thigh and leg. The obturator nerve is described in detail on page 1383.
Sciatic nerve (L4, L5, S1–3)
The sciatic nerve is the nerve of the posterior compartment of the thigh and, via its major branches, of all the compartments of the leg and foot. Formed in the pelvis from the ventral rami of the fourth lumbar to third sacral spinal nerves, it is typically 2 cm wide at its origin and is the thickest nerve in the body. It enters the lower limb via the greater sciatic foramen below piriformis and descends between the greater trochanter and ischial tuberosity. The nerve passes along the back of the thigh, where it is crossed by the long head of biceps femoris, and divides into the tibial and common fibular (peroneal) nerves proximal to the knee: the level of bifurcation is variable. The tibial and common fibular nerves are structurally separate and only loosely held together within the sciatic nerve. The tibial nerve is derived from the anterior divisions of the sacral plexus and the common fibular nerve is made up of the posterior divisions of the plexus. The sciatic nerve gives off articular branches that supply the hip joint through its posterior capsule (these are sometimes derived directly from the sacral plexus) and the knee joint. All the hamstring muscles, including the ischial part of adductor magnus, but not the short head of biceps femoris, are supplied by the medial (tibial) component of the sciatic nerve. The short head of biceps is supplied by the lateral (common fibular) component. The sciatic nerve is described in detail on page 1384.
Tibial nerve (L4, L5, S1–3)
The tibial nerve is derived from the anterior divisions of the sacral plexus. It descends along the back of the thigh and popliteal fossa to the distal border of popliteus, then passes anterior to the arch of soleus with the popliteal artery and continues into the leg. In the popliteal fossa it lies lateral to the popliteal vessels, becomes superficial to them at the knee and crosses to the medial side of the artery. In the leg it is the nerve of the posterior compartment and descends with the posterior tibial vessels to lie between the heel and the medial malleolus. It ends beneath the flexor retinaculum by dividing into the medial and lateral plantar nerves. The tibial nerve supplies articular branches to the knee and ankle. Its cutaneous area of supply, including its terminal branches, includes the back of the calf, the whole of the sole, the lateral border of the foot and the medial and lateral sides of the heel. The tibial nerve is described in detail on page 1427.
Common fibular nerve (L4, L5, S1, S2)
The common fibular nerve (common peroneal nerve) is derived from the posterior divisions of the sacral plexus. In the leg it is the nerve of the anterior and lateral compartments. It descends obliquely along the lateral side of the popliteal fossa to the fibular head, lying between the tendon of biceps femoris and the lateral head of gastrocnemius, then curves lateral to the neck of the fibula lying on the bone deep to fibularis longus and divides into superficial and deep fibular (peroneal) nerves. Before it divides, it gives off articular branches to the knee and the superior tibiofibular joints, and cutaneous branches. The cutaneous area supplied by the common fibular nerve and its terminal branches includes the anterolateral and lateral surfaces of the leg and most of the dorsum of the foot. The common fibular nerve is described in detail on page 1427.
Gluteal nerves
The gluteal nerves arise from the posterior divisions of the sacral plexus. The superior gluteal nerve (L4, L5, S1) leaves the pelvis through the greater sciatic notch above piriformis and supplies gluteus medius, gluteus minimus, tensor fasciae latae and the hip joint. The inferior gluteal nerve (L5, S1, S2) passes through the greater sciatic notch below piriformis and supplies gluteus maximus. The gluteal nerves are described in detail on page 1384.
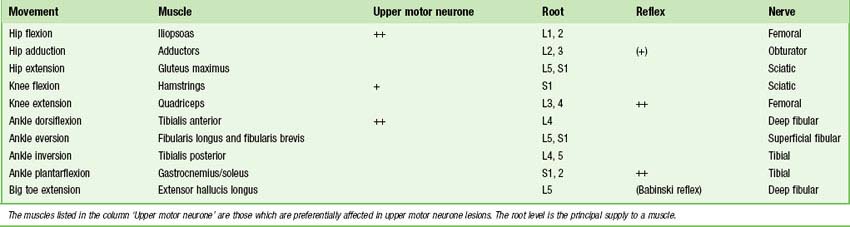
MOVEMENTS, MUSCLES AND SEGMENTAL INNERVATION
Most limb muscles are innervated by neurones which are derived from more than one segment of the spinal cord. The predominant segmental origin of the nerve supply for each of the muscles of the lower limb and for the movements which take place at the joints of the lower limb is summarized in Tables 79.1–79.4. Red has been used in Table 79.3 to highlight those muscles or movements which have diagnostic value (see below): damage to these segments or to their motor roots results in maximum paralysis. Data are based chiefly on clinical evidence (Sharrad 1995). The following caveats should be borne in mind when consulting these tables.
Table 79.1 Segmental innervation of the muscles of the lower limb
| L1 | Psoas major, psoas minor |
| L2 | Psoas major, iliacus, sartorius, gracilis, pectineus, adductor longus, adductor brevis |
| L3 | Quadriceps, adductors (magnus, longus, brevis) |
| L4 | Quadriceps, tensor fasciae latae, adductor magnus, obturator externus, tibialis anterior, tibialis posterior |
| L5 | Gluteus medius, gluteus minimus, obturator internus, semimembranosus, semitendinosus, extensor hallucis longus, extensor digitorum longus, finularis tertius, popliteus |
| S1 | Gluteus maximus, obturator internus, piriformis, biceps femoris, semitendinosus, popliteus, gastrocnemius, soleus, fibularis longus and fibularis brevis, extensor digitorum brevis |
| S2 | Piriformis, biceps femoris, gastrocnemius, soleus, flexor digitorum longus, flexor hallucis longus, some intrinsic foot muscles |
| S3 | Some intrinsic foot muscles (except abductor hallucis, flexor hallucis brevis, flexor digitorum brevis, extensor digitorum brevis) |
Table 79.2 Segmental innervation of joint movements of the lower limb
| Hip | Flexors, adductors, medial rotators | L1–3 |
| Extensors, abductors, lateral rotators | L5, S1 | |
| Knee | Extensors | L3,4 |
| Flexors | L5, S1 | |
| Ankle | Dorsiflexors | L4, 5 |
| Plantarflexors | S1, 2 | |
| Foot | Invertors | L4, 5 |
| Evertors | L5, S1 | |
| Intrinsic muscles | S2, 3 |
Table 79.3 Movements, muscles and segmental innervation in the lower limb. Muscles and movements that have diagnostic value are marked in red
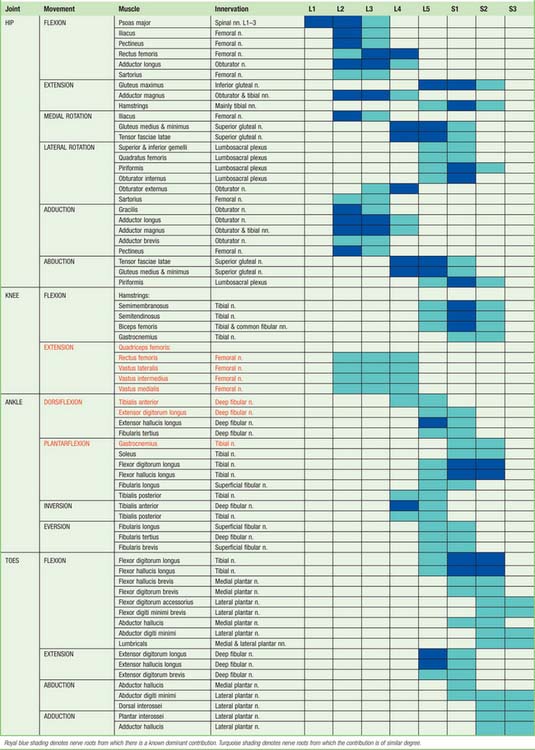 |
At the central nervous level of control, muscles are not recognized as individual actuators but as components of movement, and may therefore contribute to several types of movement, acting variously as prime movers, antagonists, fixators or synergists. Some muscles have been included in more than one place in Table 79.3, on the basis that a muscle which acts across one joint can produce a combination of movements (e.g. flexion with medial rotation, or extension with adduction) and a muscle which crosses two joints can produce more than one movement. It must also be remembered that these listings are not exhaustive.
There is no universal consensus concerning the contribution that individual spinal roots make to the innervation of individual muscles: the most positive identifications, which are limited, have been obtained by electrically stimulating spinal roots and recording the evoked electromyographic activity in the muscles. Much of the information in Tables 79.1–79.4 is therefore based on neurological experience gained in examining the effects of lesions, and some of it is far from new. Spinal roots have been given turquoise shading when they innervate a muscle to a similar extent, or when differences in their contribution have not been described. Royal blue has been used to indicate roots from which there is known to be a dominant contribution. Minor contributions have been retained in the table in order to increase its utility in other contexts, such as electromyography and comparative anatomy.
Neurological localization of a lesion
In clinical practice it is only necessary to test a relatively small number of muscles in order to determine the location of a lesion. Any muscle to be tested must satisfy a number of criteria. It should be visible, so that wasting or fasciculation can be observed, and the muscle consistency with contraction can be felt. It should have an isolated action, so that its function can be tested separately. It should help to differentiate between lesions at different levels in the neuraxis and in the peripheral nerve, or between peripheral nerves. It should be tested in such a way that normal can be differentiated from abnormal, so that slight weakness can be detected early with reliability. Some preference should be given to muscles with an easily elicited reflex. Table 79.4 gives a list of movements and muscles chosen according to these criteria: in practice, these tests would be combined with tests of sensory function. Knowledge of the sequence in which motor branches leave a peripheral nerve to innervate specific muscles is very helpful in localizing the level of a lesion.
SURFACE ANATOMY
SKELETAL LANDMARKS
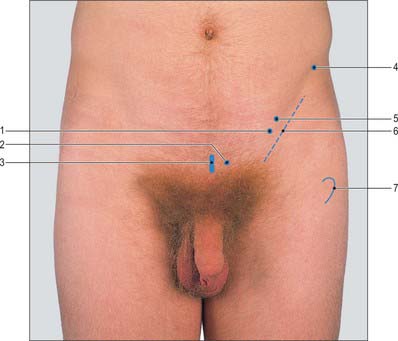
Pelvis
An oblique skin crease, the fold of the groin, marks the junction of the front of the thigh with the anterior abdominal wall, and lies distal to the inguinal ligament (Fig. 79.12). The anterior superior iliac spine lies above the lateral end of the fold and can always be palpated. At its medial end, the fold reaches the pubic tubercle. From the anterior superior iliac spine, the iliac crest is easily palpable along its entire length. It terminates posteriorly as the posterior superior iliac spine, which may be felt in the depression seen just above the buttock. This depression lies at the level of the second sacral segment, at the level of the middle of the sacroiliac joint and the termination of the spinal dural sac. The ischial tuberosity may be palpated in the lower part of the buttock. It is covered by gluteus maximus when the hip joint is extended, but can be identified without difficulty when the hip is flexed, e.g. in the sitting position, when the tuberosity emerges from under cover of the lower border of gluteus maximus and becomes subcutaneous, separated from the skin only by a pad of fat and the ischial bursa. In this position, the weight of the body is supported by the ischial tuberosities.
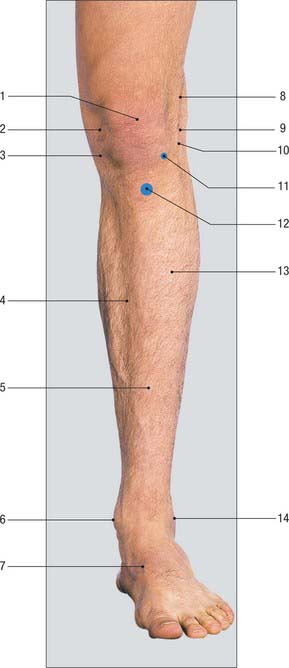
Knee
The patella and the medial and lateral condyles of the femur have been described above. The tibial condyles form visible and palpable landmarks at the medial and lateral sides of the patellar tendon (Fig. 79.13). The latter may be traced downwards from the apex of the patella to the tibial tubercle, which is easily seen as well as felt. When the knee is flexed, the anterior margins of the tibial condyles can be felt: each forms the lower boundary of a depression at the side of the patellar tendon. The lateral condyle is the more prominent of the two. The joint line of the tibiofemoral joint corresponds to the upper margins of the tibial condyles and can be represented by a line drawn round the limb at this level. The anterior horns of the menisci lie in the angles between this line and the edges of the patellar tendon. The iliotibial tract is attached to a prominence, Gerdy’s tubercle, on the anterior aspect of the lateral condyle that is usually 1 cm below the joint line and 2 cm lateral to the tibial tubercle.
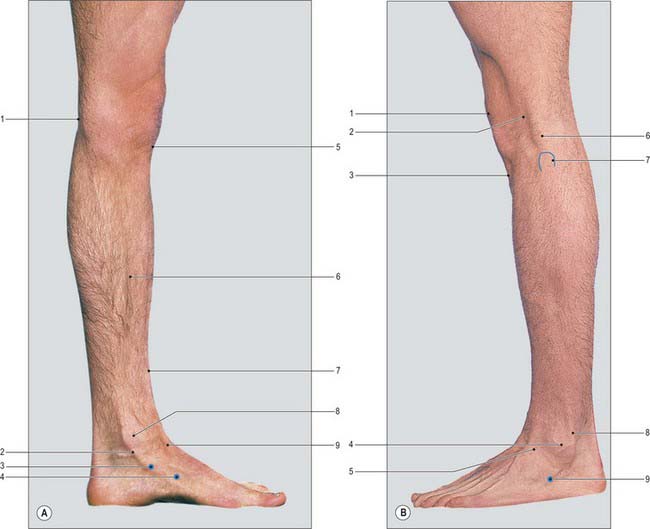
Leg and ankle
The subcutaneous medial surface of the tibia corresponds to the flat anteromedial aspect of the leg. Above, this surface merges with the medial condyle of the tibia, and below it is continuous with the visible prominence of the medial malleolus of the tibia (Fig. 79.14A). The sinuous anterior border of the tibia can be felt distinctly throughout most of its extent, but inferiorly it is somewhat masked by the tendon of tibialis anterior, which lies to its lateral side. The lateral malleolus of the fibula forms a conspicuous projection on the lateral side of the ankle: it descends to a more distal level than the medial malleolus and is placed on a more posterior plane (Fig. 79.14B). The lateral aspect of the lateral malleolus is continuous above with an elongated, subcutaneous, triangular area of the lower shaft of the fibula. The lateral part of the anterior margin of the lower end of the tibia can be detected immediately in front of the base of the lateral malleolus; the line of the ankle joint can be gauged from it.
Foot
The dorsal aspects of the bodies of the metatarsal bones can be felt more or less distinctly, although they tend to be obscured by the extensor tendons of the toes. The tuberosity on the base of the fifth metatarsal bone forms a distinct projection, which can be both seen and felt, half-way along the lateral border of the foot.
MUSCULOTENDINOUS AND LIGAMENTOUS LANDMARKS
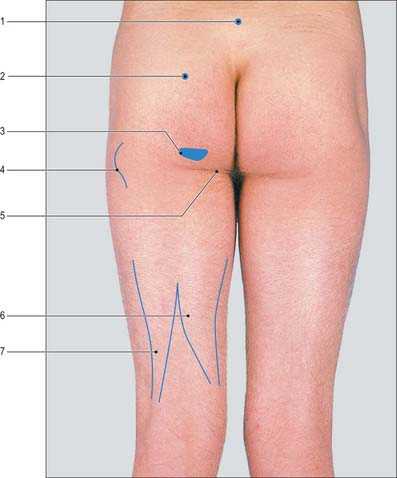
Buttock and hip
The horizontal gluteal fold marks the upper limit of the posterior aspect of the thigh. It does not correspond to the lower border of gluteus maximus but is caused by fibrous connections between the skin and the deep fascia. The natal cleft, which separates the buttocks inferiorly, starts above at the third or fourth sacral spine. The upper border of gluteus maximus begins on the iliac crest some 3 cm lateral to the posterior superior iliac spine and runs downwards and laterally to the apex of the greater trochanter. Its lower border corresponds to a line drawn from the ischial tuberosity, through the midpoint of the gluteal fold, to a point about 9 cm below the greater trochanter (Fig. 79.15). Although gluteus maximus overlaps the ischial tuberosity in the standing position, on sitting it slides superiorly posterior to the tuberosity, leaving it free to bear weight. The muscle can be felt to contract when the hip is extended against resistance.
Gluteus medius completely covers the underlying gluteus minimus. Both muscles lie in a slight depression superolateral to gluteus maximus and inferior to the anterior portion of the iliac crest. They constitute the major abductors of the hip and are demonstrated by asking the subject to stand on one limb. The ipsilateral muscles contract and tilt the pelvis in order to stabilize the centre of gravity, and the contralateral gluteal fold will rise. If the hip abductors are paralysed, e.g. in congenital dislocation of the hip or in a long-standing fracture of the neck of the femur, this mechanism is disturbed and the normal tilting of the pelvis does not occur. Indeed, when the patient stands on the affected hip, the pelvis tilts downwards on the contralateral side (Trendelenburg’s sign).
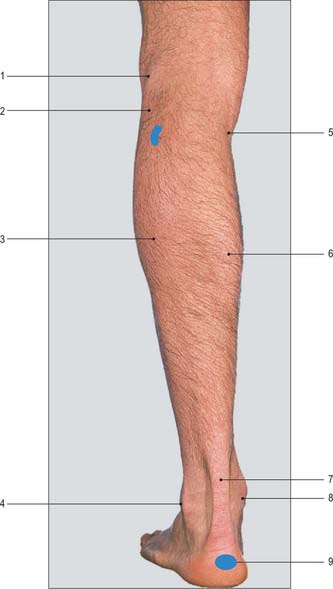
Knee
The large depression that can be seen at the back of the knee when the joint is actively flexed against resistance corresponds to the popliteal fossa (Fig. 79.16). The transverse skin crease of the popliteal fossa is 2–3 cm above the tibiofemoral joint line. The fossa is bounded on the lateral side by the prominent tendon of biceps femoris, which can be felt between the finger and thumb and can be traced downwards to the head of the fibula. Three tendons can be felt on the medial side of the fossa. Semitendinosus is the most lateral and posterior, and gracilis is the most medial and anterior. These two tendons stand out sharply and can be seen when the knee is flexed against resistance and the limb actively adducted. The third tendon is that of semimembranosus: it is more deeply situated and can be felt in the interval between the tendons of semitendinosus and gracilis. It is much thicker than the other two tendons and broadens rapidly as it is traced upwards. Distally, in thin individuals, the upper border of the pes anserinus can be palpated. The upper borders of the two heads of gastrocnemius form the medial and lateral inferior boundaries of the popliteal fossa.
Leg
The muscles in the anterior osteofascial compartment of the leg form a gentle prominence over the upper two-thirds of its anterolateral aspect: this prominence is accentuated when the foot is actively dorsiflexed. In the lower third of the leg these muscles are replaced by their tendons. The tendon of tibialis anterior can be seen just lateral to the anterior border of the tibia and traced downwards and medially across the front of the ankle (Fig. 79.14A). The other tendons cannot be examined satisfactorily above the ankle. Immediately above the medial malleolus and close to the medial border of the tibia, the tendons of tibialis posterior and flexor digitorum longus can be felt (rather indistinctly) when the foot is actively inverted and plantar flexed.
The bulky prominence of the calf of the leg is formed by gastrocnemius and soleus, both of which can be identified either when the foot is plantar flexed against resistance, or when the heel is raised from the ground by standing on tiptoes. The two heads of gastrocnemius unite to form the inferior angle of the popliteal fossa. The medial head of gastrocnemius descends to a lower level than the lateral head. Soleus lies deep to gastrocnemius; when tensed, it bulges from under gastrocnemius, particularly on the lateral side, and its fleshy belly extends to a more distal level. Both muscles end below in the conspicuous calcaneal tendon which can be gripped between the finger and thumb and followed downwards to its insertion into the posterior aspect of the calcaneus (Fig. 79.16).
Foot
When the toes are actively dorsiflexed, the belly of extensor digitorum brevis forms a small elevation on the dorsum of the foot, a little in front of the lateral malleolus. It is the only intrinsic muscle of the foot to arise from the dorsum of the foot. The tendon of tibialis anterior stands out conspicuously on the medial side when active dorsiflexion of the toes is combined with inversion: it can be traced downwards and medially to the medial cuneiform bone. Also in dorsiflexion, the tendon of extensor hallucis longus can be identified lateral to tibialis anterior. Still more laterally, and immediately in front of the lateral part of the inferior end of the tibia, the tendons of extensor digitorum longus and fibularis tertius are crowded together as they pass through the fibrous loop of the inferior extensor retinaculum. More distally, these tendons diverge to their insertions.
VESSELS, PULSES AND NERVES
Nerves
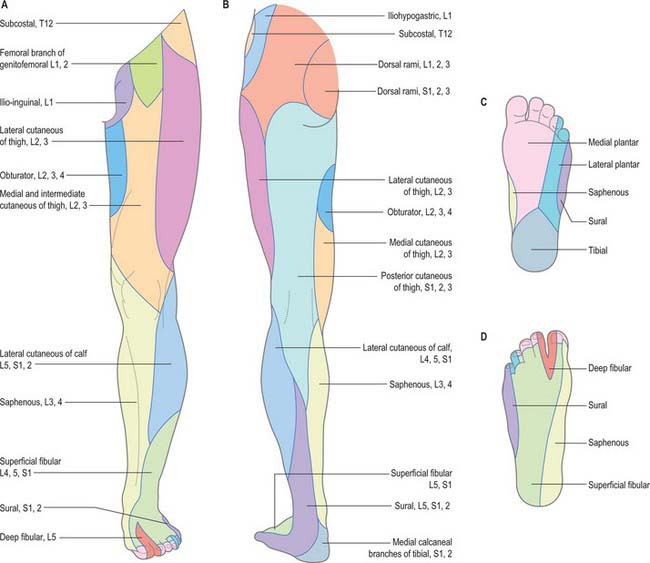
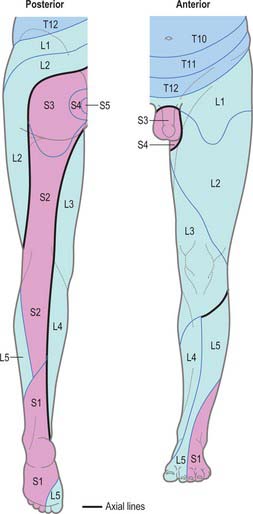
The areas of distribution and spinal segments of origin of the cutaneous nerves of the lower limb are shown in Figure 79.17.
The course of the sciatic nerve can be represented by a line that starts at a point midway between the posterior superior iliac spine and ischial tuberosity, curves outwards and downwards through a point midway between the greater trochanter and the ischial tuberosity (Fig. 79.18), and then continues vertically downwards in the midline of the posterior aspect of the thigh to the upper angle of the popliteal fossa, where it divides into the tibial and common fibular nerves (if it has not already done so at a higher level).
With one exception, the cutaneous nerves of the foot are not normally visible. The superficial fibular nerve is frequently seen and palpated over the dorsolateral aspect of the ankle and midfoot when the ankle is plantar flexed and the fourth toe passively flexed. This is particularly true in individuals with little subcutaneous fat. While the lateral branch is often seen, the medial branch is rarely visible. These superficial nerves are at risk from surgery in the anterior ankle region (especially during arthroscopy): they can be identified reliably by passive plantarflexion and inversion of the foot whilst running the blunt end of a ballpoint pen across the anterior ankle. An easily palpable click will localize the nerves, even in patients who are not thin.
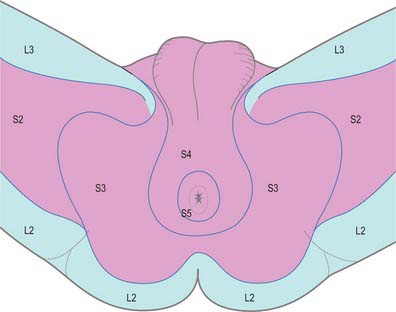
Dermatomes
Our knowledge of the extent of individual dermatomes, especially in the limbs, is largely based on clinical evidence. The dermatomes of the lower limb arise from spinal nerves T12 to S3 (Fig 79.19 and 79.20).
Myotomes
The predominant segmental origin of the nerve supply for each of the muscles of the lower limb and for the movements which take place at the joints of the lower limb are summarized in Tables 79.1–79.4.
CLINICAL PROCEDURES
Joint injection and aspiration
Careful aseptic technique is essential for all joint aspirations and injections.
Cormack GC, Lamberty BGH 1994, see Bibliography.
Crock HV. Atlas of Vascular Anatomy of the Skeleton and Spinal Cord. London: Martin Dunitz, 1996.
Dodd H, Cockett FB. The Pathology and Surgery of the Veins of the Lower Limb, 2nd edn. Edinburgh: Churchill Livingstone, 1976.
Kosinski C. Observations on the superficial venous system of the lower extremity. J Anat. 1926;60:131-142.
Sharrard WJW. The distribution of the permanent paralysis in the lower limb in poliomyelitis; a clinical and pathological study. J Bone Joint Surg Br. 1955;37-B(4):540-558.
Michel Salmon: Anatomic Studies, Book 1. In: Taylor GI, Razaboni RM. Arteries of the Muscles of the Extremities and Trunk. St. Louis: Quality Medical Publishing, 1994.