19 Pediatric Trauma
Pearls
• Differences between adult and pediatric trauma care relate directly to the differences in physiology, anatomy, and mechanism of injury. The care of victims of all ages requires the same fundamental sequences of assessment and care (primary and secondary ABCDE surveys), but slight differences in their application.
• The most common serious complications of pediatric trauma are problems with airway and breathing rather than bleeding and shock, because the most serious pediatric trauma is blunt trauma involving the head.
Introduction
Trauma is the leading cause of pediatric mortality and morbidity in the United States,7 and it is a common reason for admission to a pediatric critical care unit (PCCU). Managing the child with multisystem trauma requires specific knowledge, precise management, and keen attention to detail.1,59 This chapter reviews essential aspects of nursing care of the pediatric trauma victim. Chapters 2, 3, 6, 9 and 11 contain additional helpful information.
Epidemiology and incidence of pediatric trauma
Frequency of Injuries
Although often preventable, injury continues to be the leading cause of death and disability for children older than 1 year.3,17 Nearly 3000 children 0 to 14 years old die every year as the result of injuries—more deaths than all diseases combined.45,47 Leading causes of injury death are falls, motor vehicle crashes, burn injuries, pedestrian injuries, and drowning.45,47 For additional information, see Epidemiology and Incidence of Pediatric Trauma in the Chapter 19 Supplement on the Evolve Website.
Intentional (Inflicted) Versus Unintentional Injuries
Injuries in the child can be categorized as either intentional or unintentional.19 Intentional injuries are inflicted injuries (i.e., child abuse) or injuries that result from neglect (see Intentional Injuries/Inflicted Trauma, later in the chapter). Unintentional injuries, such as many burns, drowning, and traffic-related injuries are often preventable.
Eighty to ninety percent of life-threatening pediatric trauma is blunt injury, resulting from motor vehicle-related causes and falls4,7; approximately half of motor vehicle-related injuries and fatalities are thought to be preventable with the use of age-appropriate safety restraints.27,60 Children can also sustain motor vehicle-related injuries as pedestrians or on bicycles. Although bicycle riding is a common childhood activity, it can be dangerous. The most severe head injuries are sustained when children who are not wearing bicycle helmets collide with motor vehicles.48,50,68 When a child is in a bicycle crash, a helmet will likely decrease the severity of head injuries.27
Role of Nurses and Healthcare Providers in Injury Prevention
Prevention of unintentional injuries requires an understanding of risk factors at each child’s developmental stage, and knowledge of risk-reducing actions.15,46,70 Nurses should use every “teachable moment” with families to increase parental awareness49 of the risk of unintentional injuries and to promote the use of appropriate safety equipment. A teachable moment can occur during encounters such as a well-child checkup or a parent visit to the school,20,35,60 but is probably not present when the child is in the PCCU after an injury occurred. Nurses will need to select the best opportunities and methods to teach injury prevention strategies. See the Chapter 19 Supplement on the Evolve Website, for information about injury prevention.
Physiologic differences affecting manifestation and treatment of injuries
Airway and Ventilation
Larynx and Advanced Airways
The larynx in infants and children is smaller and is more anterior and cephalad than the larynx in adults. Intubation of children is difficult and should not be attempted by inexperienced practitioners (see Chapter 9). Unless the injured child has upper airway injury, edema, or obstruction, bag-mask ventilation usually provides adequate short-term oxygenation and ventilation. However, if the duration of transport is long, continued bag-mask ventilation is suboptimal, and skilled personnel should insert an advanced airway before transport.
The laryngeal mask airway (LMA) is an acceptable advanced airway when used by experienced providers for supporting a comatose patient.16 The LMA can be inserted blindly and, when properly positioned, isolates the trachea and produces less gastric distension than bag-mask ventilation. The LMA cannot be inserted in a patient with a cough or gag reflex.
Either cuffed or uncuffed endotracheal tubes may be used in children, and cuffed tubes may be more appropriate if the child’s lung compliance is low (e.g., as following a pulmonary contusion) or if the child has high airway resistance or a large glottic air leak. If a cuffed tube is used, the cuff inflation pressure must be monitored and maintained at the pressure recommended by the manufacturer (typically less than 20-25 cm H2O).9a,38a
Providers can determine approximate airway equipment sizes (including endotracheal tubes) using a color-coded, length-based tape (e.g., a Broselow Pediatric Emergency Tape; Armstrong Medical Industries, Lincolnshire, IL).54 A table containing these approximate sizes is included on the inside back cover of this book.
Chest Wall
The chest wall of infants and children is highly compliant, so rib fractures occur in only approximately one third of children with blunt thoracic trauma.13 The child may sustain significant intrathoracic injuries, yet may not have rib fractures.3 If a rib fracture is present, it suggests that major thoracic trauma has occurred involving substantial force and energy transfer,13 and the trauma team should suspect that underlying organs including the liver, spleen, and lungs may be injured. Upper rib injuries are associated most commonly with pulmonary and major vessel injuries, whereas lower rib fractures typically are associated with liver, spleen, lung, and kidney injury.44
Cardiovascular Function and Circulating Blood Volume
Circulating Blood Volume
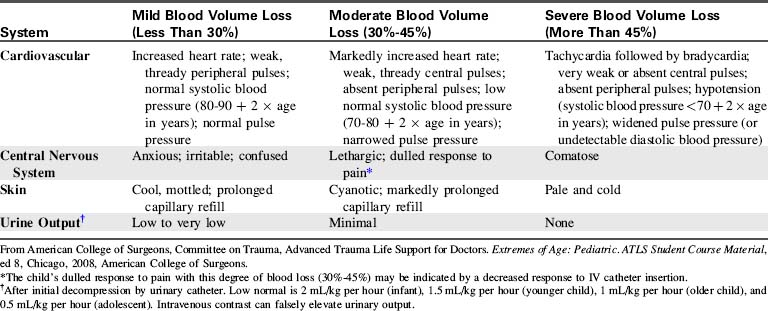
Tachycardia is an early sign of hemorrhage in children. Significant hemorrhage (10%-15% of circulating blood volume) will produce signs of poor systemic perfusion (e.g., mottled color, cool extremities, delayed capillary refill, thready peripheral pulses). Because the child can initially compensate for blood loss by increasing the heart rate and systemic vascular resistance, hypotension often does not develop unless the child acutely loses 20% to 25% or more of circulating blood volume.54
Neurologic Function
Spinal Cord Injury
Many children with spinal cord injury have ligamentous injury with no evidence of vertebral fracture or other radiographic abnormalities on routine (anteroposterior and lateral) spine radiographs or CT scan.42a These children have spinal cord injury without radiographic abnormality (SCIWORA), and many of these patients develop permanent neurologic injury.3,23
Nurses should carefully assess movement and sensation in all extremities on admission and at frequent intervals throughout the child’s hospitalization (see Chapter 11). The mechanism of injury should increase the index of suspicion of spinal cord injury. For example, a child wearing a lap belt without a shoulder strap who presents with abrasions or contusions on the lower abdomen may have an acute flexion injury of the lower spine (with or without a Chance fracture).
Data from the National Trauma Data Bank51 indicates that 66% of cervical spine injuries in children younger than 3 years are caused by motor vehicle crashes, and only 15% are from falls. In the National Trauma Data Bank, cervical spine injuries were present in approximately 2.3% of all children less than 3 years of age injured in motor vehicle crashes.51 However, cervical spine injuries in children younger than 3 years were still relatively uncommon.51
Fluid Administration
Vascular Access
If IV access cannot be achieved, intraosseous (IO) access is established; this route of access can be used for emergency fluid resuscitation and drug administration in patients of all ages.14 IO needles can be placed in the proximal or distal tibia or distal femur. Other placement options include the radius, ulna, pelvis, clavicle, and calcaneus. Medications and drugs can be given intraosseously until suitable venous access is achieved. Fluid may be delivered by infusion pump into an IO catheter, and bolus infusions can be provided through a syringe, an infusion pump, or a pressure bag (inflated up to 300 mm Hg). IO fluid boluses in children may be given as rapidly as 20 mL/kg over 5 min.
Initial stabilization of the pediatric trauma patient
Field Triage and Scoring
The trauma score (TS) is designed for scoring injury severity in the field; it uses the GCS score and the scoring of four additional physiologic parameters: systolic blood pressure, capillary refill, respiratory rate, and respiratory effort. Each category is scored and then totalled.10
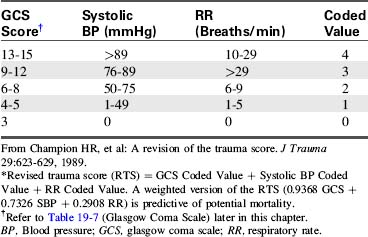
The revised trauma score (RTS) was created to identify patients for triage to a trauma center.11 It requires evaluation of fewer physiologic parameters than the TS. To calculate the RTS, the provider assigns a coded value to the GCS score, the systolic blood pressure, and the respiratory rate and then adds these three values together (Table 19-1). A weighted version of the RTS is a predictor of mortality; an RTS of less than four is correlated with a probability of survival of less than 60%, and should prompt consideration for transfer to a trauma center.2
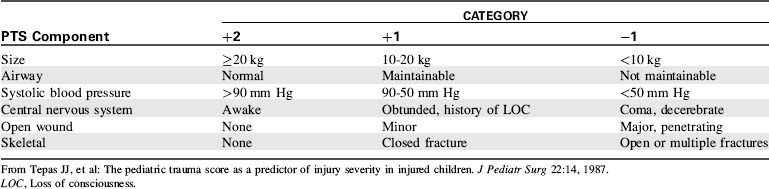
The pediatric trauma score (PTS) was developed to better identify the manifestations of injuries in children and better quantify their severity. The PTS evaluates the following six parameters: (1) patient size, (2) airway stability, (3) systolic blood pressure, (4) mental status, (5) wounds, and (6) skeletal injuries (Table 19-2).
In the PTS, large size and optimum status result in a score of 2 for each parameter; extremely small size or systemic dysfunction results in a score of −1 for each parameter. The highest possible score is a 12 and the lowest possible score is a −6.67 Children with a PTS totaling 8 or less have the highest potential for preventable mortality and morbidity, and they should be transported to a facility with the resources necessary to provide optimal pediatric care (e.g., a pediatric trauma center).67
The PTS is a conservative scoring system and will result in the triage of some children who have only moderate injuries; however, conservative triage is generally thought to be appropriate for injured children. The PTS has not been shown to be consistently superior to the RTS, so many centers continue to use the RTS for the triage of children and with good results. Because vital signs (e.g., particularly blood pressures) are often not evaluated in the field,22,38 a simple scoring system that uses fewer vital signs (e.g., the RTS) can be used more consistently than one requiring evaluation of heart rate and respiratory rate in addition to blood pressure (i.e., the PTS).
In 2006, the National College of Surgeons Committee on Trauma convened a panel of national experts on trauma field triage to develop consensus trauma triage criteria for adults and children based on physiologic criteria (GCS score, systolic blood pressure, and respiratory rate), anatomy of the injury (e.g., penetrating trauma to the head, neck, or torso; flail chest; two or more long bone fractures; amputation; pelvic fractures; open or depressed skull fractures), the mechanism of injury (e.g., falls of 10 feet [3.048 m], or a distance of more than twice or threefold the child’s height, high risk auto crashes, motor vehicle vs. pedestrian crashes, motorcycle crashes), special patient or system considerations (e.g., children should be preferentially triaged to pediatric trauma centers; patients with associated anticoagulation or bleeding disorders; the EMS provider judges transport is indicated59), and protocols.
The criteria contained in the National College of Surgeons Committee on Trauma guidelines are included in Box 19-1. A detailed explanation of these guidelines was published by the Centers for Disease Control and Prevention in 2009.56 A link to this publication is available in Triage of Injured Patients in the Chapter 19 Supplement on the Evolve Website.
Physical and Physiologic Findings
• Shock unresponsive to one bolus (defined as hypotension, with systolic BP less than 60 mm Hg in infants and less than 90 mm Hg in children) or associated with persistent prolonged capillary refill (systolic BP less than 90 mm Hg is contained in the NCS-Committee On Trauma Expert Panel Guidelines for transfer*)
• Clinical evidence of altered level of consciousness (GCS score less than 14*); coma is an absolute indication for transfer
• Respiratory rate less than 10/min or greater than 29/min*
• Any cardiac arrhythmias (including bradycardia)
Types and Anatomy of Injuries
• Virtually any penetrating injury of the head, thorax, abdomen, neck or extremities proximal to the elbow and knee*
• Unstable chest wall (flail chest)*
• Two or more proximal long bone fractures*
• Crushed, degloved, or mangled extremity*
• Amputation proximal to the wrist or ankle*
Mechanism of Injury and Evidence of High-Energy Impact
• Fall from height greater than 10 feet (3.048 m) or a distance of twice or three-fold the child’s height*
• Intrusion into vehicle greater than 1 foot (0.3 m) into passenger space or 1.5 feet (0.46 m) on any side*
• Death in same passenger compartment*
• Vehicle telemetry data consistent with high risk of injury*
• Motor vehicle versus pedestrian or bicyclist thrown or run over or with significant (greater than 20 mph) impact*
Special Patient or System Considerations
• Anticoagulation or bleeding disorder*
• Time-sensitive extremity injury*
• End-stage renal disease requiring dialysis*
BP, Blood pressure; EMS, emergency medical services; GCS, glasgow coma scale.
Modified from PCCC Transport Criteria, Harbor-UCLA Medical Center, Los Angeles, 1990; and Sasser SM, et al: Guidelines for field triage of injured patients: Recommendations of the National Expert Panel on Field Triage. Morbidity and Mortality Weekly Report 2009; 58 (RRO1):1-35.
Management of the pediatric trauma victim in the emergency department
Emergency Department Stabilization and Transfer
General indications for transfer of the critically ill child to a trauma center with a PCCU include multisystem trauma, shock requiring multiple transfusions or vasoactive drug therapy, head injury accompanied by alteration in level of consciousness, multiple long bone fractures, rib fractures in the young child, penetrating injuries, traumatic amputations, significant burns, and anticipated need for prolonged mechanical ventilation (see Box 19-1).56
Initial survey, resuscitation, and stabilization
The following information may apply to care in the ED, the acute care unit, or the PCCU. For further information regarding cardiopulmonary resuscitation in children, refer to Chapter 6.
Airway
Positioning, Jaw Thrust
The first priority of stabilization and management is to establish a patent airway. The tongue of the infant and small child is large relative to the size of the oral cavity and posterior pharynx. When the patient is unconscious, the tongue can fall into the posterior pharynx, causing obstruction.54 The sniffing position (head tilt, chin lift) usually opens the airway; however, this procedure should be performed as the initial airway maneuver only if cervical spine injury has been ruled out.
If the injured child is unconscious or if the child’s mechanism of injury or presentation suggests potential cervical spine injury, the cervical spine is stabilized at the same time the airway is opened. In these children, the “jaw thrust” should be used to relieve airway obstruction; the provider holds the head and neck steady while providing gentle forward-upward pressure at the angle of the mandible to open the airway.2 For some trauma victims, such as those with isolated injury of an extremity, a cervical spine injury is unlikely and no such precautions are needed. If the airway can’t be opened with a jaw thrust, a chin lift with a slight head tilt may be needed, because an adequate airway must be established.9a,38a
Suctioning
Relatively small amounts of foreign matter in the child’s hypopharynx can obstruct the airway. As a part of initial stabilization, providers should suction the airway to eliminate obstruction such as blood, mucus, loose teeth, or vomitus. Neonates and young infants are obligate nose breathers. In these infants, gentle nasal suctioning or opening of the airway may be the only intervention required to stimulate spontaneous ventilation.2
Spine Stabilization
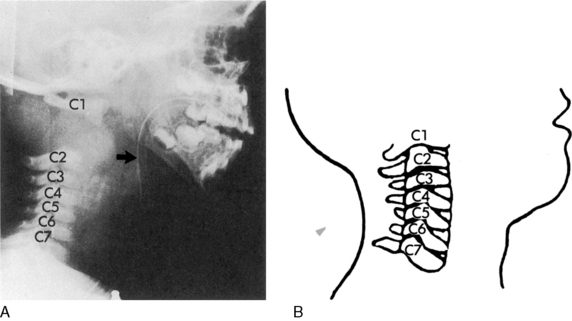
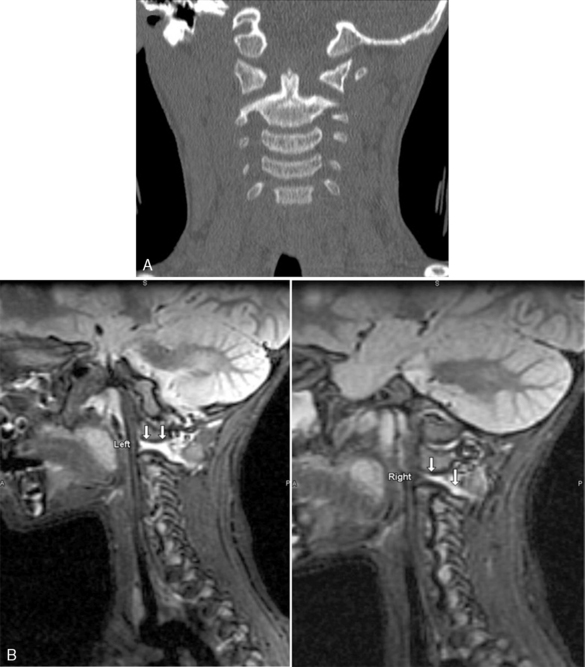
Spinal cord injuries are less common in children than in adults. When these injuries occur in children, they are generally associated with motor vehicle-related crashes, falls, and inflicted head trauma and can result in injuries of the upper or lower cervical spine (Fig. 19-1).4
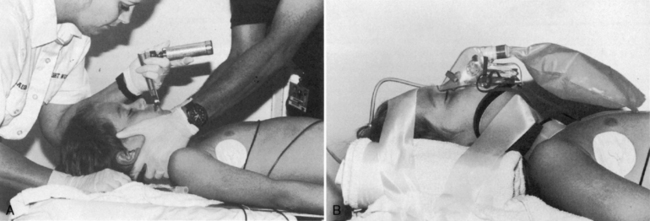
Spine stabilization and then immobilization is indicated after motor vehicle crashes, after pedestrian-related crashes, after crashes in which the child was unrestrained, for any unconscious trauma victim (because it is difficult to ascertain the extent of injury), and for any major trauma associated with head injury.2 Manual stabilization is provided initially, and then a device is used to immobilize the cervical spine during transport and initial evaluation (Fig. 19-2).
There are many acceptable methods for immobilizing the cervical spine. A semirigid collar (e.g., an extrication collar) immobilizes the cervical spine, but these collars are not recommended for use in children younger than 4 years.5 Foam collars can be applied easily and are available in small sizes, but they often provide no protection against head and neck movement. If an excessively large collar is applied, flexion of the neck may cause airway obstruction or hyperextension of the neck can result in the very movement and possible injury that the collar is designed to prevent.
Cervical spine immobilization in children requires a combination of a cervical collar (of the appropriate size) with a rigid spine board. The child’s head is supported in a neutral position on the board, using a board with head well or pads under the torso, and, foam blocks and straps. Towel rolls, and tape should be used to secure the torso and the head (see Fig. 19-2).3,25,29
If the mechanism of injury suggests thoracic spine trauma, providers should avoid any flexion or torsion of the torso. If lap belt injuries are suspected (see Secondary Survey, Abdomen), providers should prevent movement of the lumbar spine until further examination.55 The child should be log-rolled whenever turning is required until an injury to the spine is ruled out (i.e., the spine is cleared). If the child is sufficiently stable, the provider should evaluate and document movement and sensation of all extremities.
Airway Management
Oropharyngeal and nasopharyngeal airways can help to maintain a patent upper airway. Oral airways are reserved for the child with absent cough and gag reflex. Oral airways must be sized appropriately, because airways that are too small can push the tongue back into the oropharynx and those that are too long can obstruct the pharynx.54 The length of the airway should equal the distance from the mouth to the angle of the mandible. Nasal airways can be inserted in the alert child or the unresponsive child who has no facial trauma; they may facilitate suctioning.
Intubation
Intubation may be necessary to maintain a patent airway and prevent anticipated deterioration. Indications for intubation of the pediatric trauma victim (Box 19-2) include: (1) inability to ventilate the child’s lungs adequately using a bag-mask device, (2) need for prolonged airway control and prevention of aspiration, (3) severe head injury (in anticipation of a need for controlled ventilation and oxygenation), (4) flail chest, (5) severe facial burns, and (6) shock unresponsive to volume infusion.2,54
Box 19-2 Indications for Intubation in the Pediatric Trauma Victim
• Significant respiratory distress
• Hypoxemia despite oxygen therapy
• Signs of airway obstruction: stridor, increased work of breathing; suprasternal, supraclavicular retractions
• Injuries associated with potential airway obstruction (e.g., inhalation injuries, crushing facial or neck injuries)
• Head injury or signs of increased intracranial pressure
• Thoracic injury (rib fractures, pulmonary contusion, flail chest, penetrating injuries)
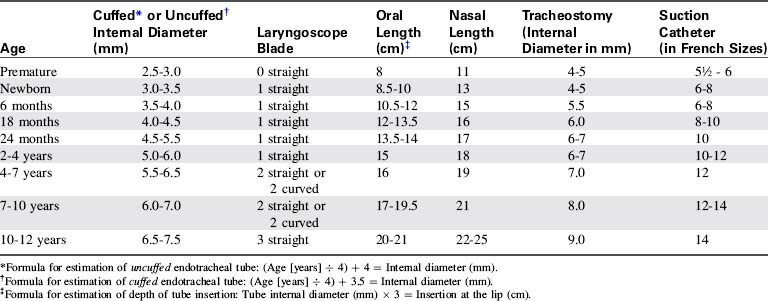
The nurse must be able to select intubation equipment of appropriate size. Formulas, tables, or a length-based tape that indicates the equipment sizes (i.e., the Broselow tape—see inside back cover) may be used (Table 19-3).54
In the past, only uncuffed tubes were used for children younger than 8 years, because there was concern that cuffed tubes could produce subglottic tracheal injury.2 However, for some children (e.g., those with noncompliant lungs, high airway resistance or large glottic air leak), the use of a cuffed tube may be preferable to an uncuffed tube, particularly if the child requires ventilation with high inspiratory pressure or maintenance of positive end-expiratory pressure.9a,38a Slightly different formulas are used to determine the internal diameter of a cuffed versus an uncuffed tube (see Table 19-3).
Gastric distension increases the risk of vomiting and aspiration, can stimulate a vasovagal reflex and bradycardia, compromises diaphragm movement, and can mimic or mask symptoms of abdominal injury. If gastric distension develops, providers should remove air through an orogastric tube. If the patient has craniofacial trauma with maxillofacial or basilar skull fracture, an orogastric tube is used for gastric decompression rather than a nasogastric tube. Case reports have documented intracranial migration of nasogastric tubes if they are inserted blindly.4,18
Sedation and administration of neuromuscular blockers are advisable before intubation of a conscious trauma victim, particularly if the child is struggling or has a full stomach. Rapid sequence intubation (also known as drug assisted intubation) is designed to reduce stimulation of gag reflex (and the associated risk of vomiting and aspiration) when the child has a full stomach or when the time of the last meal cannot be determined (for further information about rapid sequence intubation, see Chapter 9 and Box 9-11).
Cricothyrotomy and Tracheostomy
If positioning of the child, bag-mask ventilation, and intubation do not relieve airway obstruction and providers cannot deliver adequate ventilation, then injury to the larynx or trachea is likely to be present. Needle cricothyrotomy, although rarely necessary in the child, should be considered at this time.54 This procedure is challenging because it can be difficult to identify landmarks in the short neck of an infant or young child, and the needle is difficult to secure once it is inserted.
Ongoing Airway Assessment
If the intubated child’s condition suddenly deteriorates, the bedside nurse should provide bag-mask ventilation and quickly assess tube position and patency, and assess for complications such as a pneumothorax. The mnemonic D-O-P-E can be used to recall the causes of sudden deterioration in the child with an advanced airway: tube displacement, tube obstruction, pneumothorax, and equipment failure.9a,38a If the tube is no longer in the trachea, the nurse should remove it and provide bag-mask ventilation as needed until reintubation can be accomplished.
Breathing
Assessment of Ventilation and Oxygenation
The team should continuously assess the child’s respiratory rate and effort, ventilation, and response to oxygen administration. Apnea, gasping, and cyanosis despite oxygen therapy indicate the need for positive pressure ventilation (Box 19-3). The pulse oximeter and exhaled CO2 detectors are useful adjuncts to clinical assessment; they enable continuous evaluation of oxyhemoglobin saturation, CO2 elimination, and response to therapy.
As a general guide when a perfusing rhythm is present, infants require a spontaneous or assisted ventilation rate of at least 20/min, preschool-aged children require a minimum ventilation rate of 15/min, and school-aged children require a ventilation rate of at least 12/min to produce sufficient oxygenation and ventilation. Faster spontaneous respiratory rates are common in the presence of pain, fear, hemorrhage, or respiratory distress.2
Life-Threatening Thoracic Injuries
Injuries to the lung parenchyma or accumulation of intrathoracic air or fluid can impair oxygenation and ventilation and can produce cardiorespiratory failure. Injuries may be internal, external, or both. Common life-threatening thoracic injuries include tension pneumothorax, open pneumothorax (sucking chest wound), massive hemothorax, and cardiac tamponade. Additional injuries that are potentially life threatening include pneumothorax, tracheobronchial injuries, and pulmonary contusion. Fortunately, injuries resulting from penetrating trauma are relatively uncommon in children.7
Pneumothorax
Pneumothorax is a common complication of thoracic injury in children.13 Most injuries result from blunt chest trauma and are not associated with rib fractures. The child with pneumothorax may be asymptomatic or exhibit dyspnea, chest pain, and severe respiratory distress.44 Symptomatic children demonstrate hypoxemia, asymmetric chest wall movement, and decreased breath sounds or altered pitch of breath sounds on the involved side; this altered pitch may be difficult to identify in the small child because referred breath sounds from other parts of the chest may be heard over the pneumothorax.
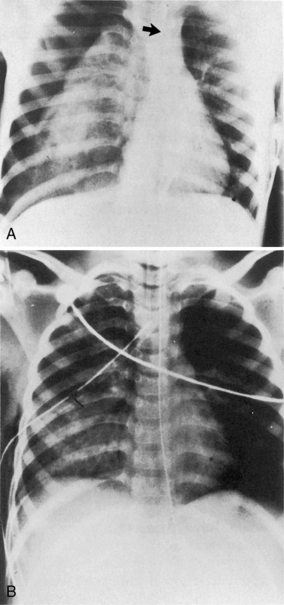
Tension Pneumothorax
Tension pneumothorax develops from progressive air entry into the pleural space from the lung or airways; this air accumulation elevates intrapleural pressure, compresses the lung, and can compromise cardiovascular function. The lung on the side of the tension pneumothorax is partially collapsed, and severe hypoxemia develops (Fig. 19-3; see Fig. 10-7). Breath sounds and chest expansion on the side of the pneumothorax are decreased or absent.
A tension pneumothorax shifts the mediastinum away from the affected side. This shift reduces venous return to the heart and decreases cardiac output; neck vein distension may be observed. In addition, the point of maximal impulse and the trachea shift away from the tension pneumothorax,4 although the tracheal shift may be difficult to appreciate in infants and children. The resultant decrease in cardiac output and oxygen delivery are life threatening. The mediastinal shift can result in compression of the contralateral lung, further compromising oxygenation and ventilation.
To perform needle decompression, insert a large-bore (13, 16, or 18 gauge) angiocatheter on the affected side, into the second intercostal space at the midclavicular line.54 The diagnosis of tension pneumothorax is confirmed when needle or tube thoracostomy results in evidence of air evacuation and immediate improvement in the patient’s condition. After initial air evacuation, the provider can use a stopcock to prevent entrainment of air into the chest. The provider can also attach the angiocatheter to tubing with the tubing tip placed 2 to 3 cm below the surface of a bottle of sterile water; this maintains an underwater seal until a chest tube is inserted.
Chest tubes are inserted to treat pneumothorax and hemothorax. Appropriate chest tube size is based on the age of the child (Table 19-4), and sizes can be predicted from length-based (e.g., Broselow) resuscitation tapes. Before the chest tube is inserted, the skin is prepared with a povidone iodine or chlorhexidine scrub, and the provider administers local anesthetic (e.g., lidocaine). A small stab wound is made in the skin and subcutaneous tissue along the long axis of the rib, in the fifth or sixth intercostal space at the midaxillary line. A curved hemostat followed by the chest tube is advanced through the chest wall and pleura, into the chest cavity (see Evolve Fig. 19-1 in the Chapter 19 Supplement on the Evolve Website for an illustration of chest tube insertion).
| Age | Chest Tube Size (French) |
| Full-term neonate (6 months) | 10-12 |
| Older infant (6-18 months) | 12-14 |
| Toddler (1-3 years) | 14-16 |
| Young school age (4-7 years) | 16-20 |
| Older school age (8-12 years) | 20-24 |
| Adolescent | 24-32 |
Sucking Chest Wounds
Sucking chest wounds result from penetrating trauma. These wounds allow air to move into and out of the pleural space, making a sucking noise.58 Treatment is immediate application of an occlusive dressing (e.g., Opsite [Smith and Nephew, Memphis, TN] or Vaseline gauze [Kendall, division of Covidien, Norwalk, CT]).
Once an open pneumothorax is sealed, the child will likely require chest tube insertion and treatment of the underlying lung injury (e.g., mechanical ventilation for treatment of a pulmonary contusion). Continuous observation is required to identify development of a pneumothorax.58 If the child has an advanced airway and is receiving positive pressure ventilation, a chest tube should be inserted.
Hemothorax
A hemothorax is the accumulation of blood in the pleural cavity. The severity of symptoms produced by the hemothorax is determined by the extent and rapidity of blood loss and by the presence of associated injuries (i.e., lung or great vessel tears).44 If the child is asymptomatic, the most effective immediate therapy is the placement of an IV catheter to replace ongoing blood loss, followed by placement of a chest tube to evacuate accumulated blood. Providers should monitor the child’s systemic perfusion and replace ongoing blood loss as needed.
If the child has significant hemorrhage and hemothorax, the child will demonstrate signs of poor systemic perfusion and respiratory compromise. In cases of large hemothorax, rapid blood replacement will be required. Significant ongoing hemorrhage (i.e., significant volume of blood loss via chest tube) may indicate rupture of a large thoracic vessel or lung laceration, and urgent exploratory thoracotomy is indicated.13
Cardiac Tamponade
Cardiac tamponade is a form of obstructive shock. Classic clinical signs include persistent hypotension, distension of neck veins, muffled heart sounds, and pulsus paradoxus (a fall in systolic arterial pressure of 8-10 mm Hg or more during spontaneous inspiration). However, these signs are virtually impossible to appreciate in patient with tachypnea and hypotension. The presence of a cardiac tamponade can be confirmed by echocardiography and, more recently, with the use of ultrasonography (e.g., emergency ultrasound or focused assessment with sonography for trauma [FAST]); fluid in the pericardium (i.e., hemopericardium) will appear black against the gray heart muscle.42
When tamponade is present, the tamponade must be evacuated by pericardiocentesis. Administration of autologous blood and fluid boluses may initially help support cardiac output. A pericardial drain can be placed or an emergency thoracotomy can be performed for pericardial decompression and immediate repair of the associated cardiac injury.4,13
To perform pericardiocentesis, the chest is cleaned and a needle is inserted in the left subxyphoid region. While constant negative pressure is applied, the needle is aimed superiorly and posteriorly. Once blood or fluid enters the barrel of the syringe, the needle is likely in the pericardium. At this point, the needle or catheter is held in place and blood is aspirated to decompress the pericardium.4
If neither a FAST scan nor ultrasonography is available, pericardiocentesis may be accomplished using an 18-gauge metal spinal needle joined to an alligator clamp (i.e., the alligator clamp is joined to the base of the needle) to allow simultaneous needle insertion and monitoring of the electrocardiogram (ECG). The alligator clamp is then joined to the electrode of an ECG recorder (see Evolve Fig. 19-2 in the Chapter 19 Supplement on the Evolve Website for an illustration of this technique).
Flail Chest
As noted previously, rib fractures are present in one third or less of children with blunt trauma. Rib fractures indicate injury associated with substantial force and energy transfer.3,13 When three or more contiguous ribs are fractured at two points, typically in the back,44 flail chest can develop.
Whenever rib fractures are present, providers should closely assess and monitor the child for evidence of underlying organ injury (e.g., liver, spleen, lung).13,44 Patients with flail chest always have associated pulmonary contusions, the primary cause of the hypoxia associated with this condition.
Diaphragm Rupture
Diaphragm rupture may be impossible to detect once positive pressure ventilation is instituted. Occasionally, herniation of abdominal contents into the chest will occur, and these will be apparent on the chest radiograph or CT scan; an inserted nasogastric tube may be visible in the left chest.13,44 Surgical repair through an abdominal or thoracic approach will be required.
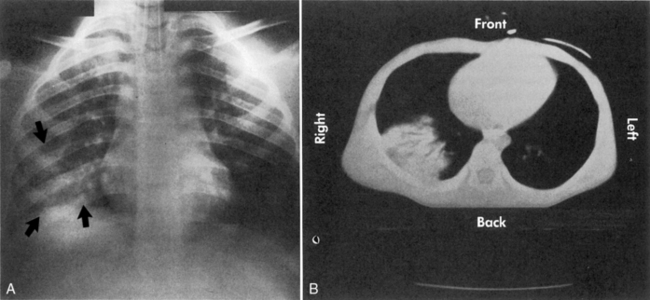
Pulmonary Contusion
A pulmonary contusion is a bruise on the lung resulting from lung parenchymal injury. Although a pulmonary contusion can be asymptomatic and diagnosed only on CT scan, it can cause respiratory compromise following major blunt chest trauma.13,44 A significant pulmonary contusion will cause hypoxemia, and opacification is visible on a chest radiograph or CT scan (see Figs. 19-3, B and 19-4).
Circulation
Cardiovascular compromise in the trauma patient generally is caused by hypovolemia, but it may also be caused by hypoxia or severe head injury. Even if effective cardiovascular function is present on arrival in the hospital, the trauma team should assess and reassess systemic perfusion to detect any signs of deterioration. These signs may be subtle in the child and include: tachycardia; weak peripheral pulses, mottled skin; cool, pale extremities; delayed capillary refill; and unusual irritability or lethargy (Box 19-4).
If the child has an ineffective or absent pulse in a central artery (e.g., carotid, femoral), or the infant has no brachial pulse, cardiopulmonary resuscitation is needed (see Chapter 6). Additional indications for the initiation of chest compressions include symptomatic bradycardia (a heart rate less than 60/min associated with signs of poor systemic perfusion) that is unresponsive to adequate oxygenation and ventilation.26,54
The most common terminal (prearrest) cardiac rhythm in pediatric patients is a bradycardia that deteriorates to an agonal rhythm or asystole. Ventricular tachycardia and ventricular fibrillation are less common in children than in adults. For further information regarding cardiopulmonary resuscitation in children, see Chapter 6. Survival following prehospital cardiac arrest and cardiovascular collapse in pediatric victims of blunt trauma is poor.26 To prevent arrest, providers must detect and treat signs of airway compromise, respiratory failure, and shock.
Recognition of Hypovolemia
As blood volume is depleted, the child’s blood pressure initially remains unchanged, because systemic vascular resistance increases proportionately.54 The pediatric trauma victim typically does not develop hypotension until approximately 30% of blood volume has been lost.2,13,25,54 This ability to compensate for blood loss with vasoconstriction and redistribution of blood flow means that signs of hemorrhage may be insidious in the child and vital signs alone may not identify evolving shock.2
The most consistent signs of hemorrhage will include tachycardia, alteration in responsiveness, peripheral vasoconstriction, thready pulses, and diminished pulse pressure.4,54 Hypotension is a late and ominous sign of cardiovascular compromise.54 Clinical findings can be used to classify the severity of the hemorrhage and to estimate the volume of blood loss (Table 19-5).
Noninvasive oscillometric blood pressure measurements may provide falsely high blood pressure measurements in the hypotensive patient.38a Such measurements are less reliable than intraarterial measurements in an unstable child.
Vascular Access
IO access is a suitable alternative to rapid peripheral venous cannulation for administration of crystalloid, colloid, blood, and drugs for the child in shock. IO needles provide access to the marrow cavity of a long bone in an uninjured extremity and are safe and effective, and they require less time to establish than venous cut downs.3,9a,38a,54,61 Drugs administered by the IO route reach the heart in approximately the same time as drugs given by central venous access.
IO access can be established in the anterior tibia 1 to 3 cm below the tibial tuberosity54 or in the inferior third of the femur, 3 cm above the external condyle, anterior to the midline.3 Bone marrow needles are preferred for this procedure. Occasionally, marrow will obstruct the flow of fluids through the needle, and the use of a pressure infusion device may be required to increase the rate of fluid administration.54
Central venous cannulation enables rapid fluid administration and assessment and continuous monitoring of central venous pressure. However, central venous cannulation should be performed only by personnel trained in these procedures. Ultrasound guidance may be helpful.42
The femoral vein can be used to gain access to the inferior vena cava. The advantage of the femoral vein approach is the distance from the major sites of activity during resuscitative efforts; however, some physicians prefer to cannulate other smaller vessels.54
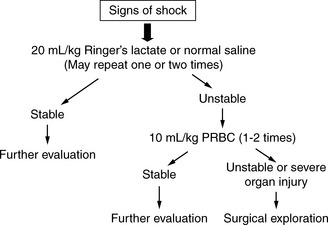
Treatment of Hypovolemia
Fluid resuscitation begins with a bolus of isotonic crystalloid solution (lactated Ringer’s solution or normal saline) administered in boluses of 20 mL/kg over 5 to 20 minutes.2,54 If the child has signs of substantial blood loss or shock, the bolus should be administered as quickly as possible, typically over 5 to 10 minutes. The patient with trauma and hemorrhage also will require blood administration. Typically one bolus of packed red blood cells (RBCs) is administered after every two to three boluses of isotonic crystalloid (Fig. 19-5).
If the blood pressure, capillary refill, and quality of peripheral pulses remain poor and tachycardia persists despite the administration of two or three fluid boluses, then substantial hemorrhage has likely occurred or a continuing source of blood loss is present.31 Surgical exploration should be considered if the child’s condition is still unstable despite administration of two boluses of packed RBCs (in addition to the isotonic crystalloids). Abdominal bleeding can result from a solid organ or major vessel injury, and the trauma team should look for occult retroperitoneal or pelvic bleeding.13 Additional causes of shock that is unresponsive to initial fluid resuscitation include cardiac tamponade, tension pneumothorax (discussed previously), and neurogenic shock.
Disability: Neurologic Function
Signs of increased intracranial pressure include: deterioration in level of consciousness, pupil dilation (unilateral or bilateral), lack of response to a central painful stimulus, and, in the infant, a firm fontanelle. Late signs of increased intracranial pressure (often associated with impending brainstem herniation) include bradycardia, systolic hypertension with widening pulse pressure, and altered respiratory pattern, such as apnea (see Box 19-5).
Box 19-5 Signs of Increased Intracranial Pressure in Children
• Change in level of consciousness
• Decreased responsiveness (decreased eye contact, decreased response to parents or pain)
• Reduced ability to follow commands (hold up two fingers, wiggle toes, stick out tongue)
• Pupil dilation with decreased response to light
• Reduced spontaneous movement or deterioration in motor function or reflexive posturing
• Decorticate posturing, followed by decerebrate posturing and flaccid response to pain
• Cushing reflex or triad (bradycardia, systolic hypertension with widening pulse pressure, and altered respiratory pattern, such as apnea) may occur only as a late sign
Effective cerebral resuscitation in the pediatric trauma victim requires adequate shock resuscitation; cerebral perfusion will not be optimal if shock is present. The trauma team should provide shock resuscitation until systemic perfusion is effective. If signs of impending herniation develop (i.e., bradycardia, systolic hypertension, and altered respiratory pattern), it may be helpful to provide mild hyperventilation to reduce carbon dioxide levels and, thus, cerebral blood flow as a temporary emergency measure. Hyperventilation is not routinely performed unless signs of impending herniation are present. IV mannitol (0.25-0.5 g/kg) is given to shift water from the cellular to the extracellular (including intravascular) space; this rapidly decreases blood viscosity, leading to an increase in cerebral blood flow and tissue oxygen delivery. Hypertonic saline (3%-23.5%) may also be administered to produce an osmotic diuresis and improve cerebral perfusion; it may have other additional benefits. For further information, see Management of Increased Intracranial Pressure in Chapter 11.
Status epilepticus is uncommon, but must be identified and treated aggressively in the patient with increased intracranial pressure, because continuous seizures will increase cerebral metabolic oxygen consumption and will cause cerebral ischemia. Intermittent seizures will increase intracranial pressure transiently and are treated with diazepam (0.25 mg/kg).2 A prophylactic anticonvulsant (i.e., phenytoin) is typically administered for 1 week to infants and children with moderate or severe head injury (GCS less than 12) who are thought to be at high risk for seizures.
Secondary Survey: “head-to-toe” assessment
Head
The most common head injury in children is closed head injury.58 Closed head trauma is not always immediately recognizable. For this reason, the mechanism of injury and the initial response to therapy (or lack of response) should provide a high index of suspicion. The first priority of management is to maintain cerebral perfusion and treat increased intracranial pressure by performing intubation and providing adequate ventilation, oxygenation, shock resuscitation, osmotic diuresis, and analgesia and sedation if needed. Early identification of increased intracranial pressure is essential to reduce morbidity and mortality.
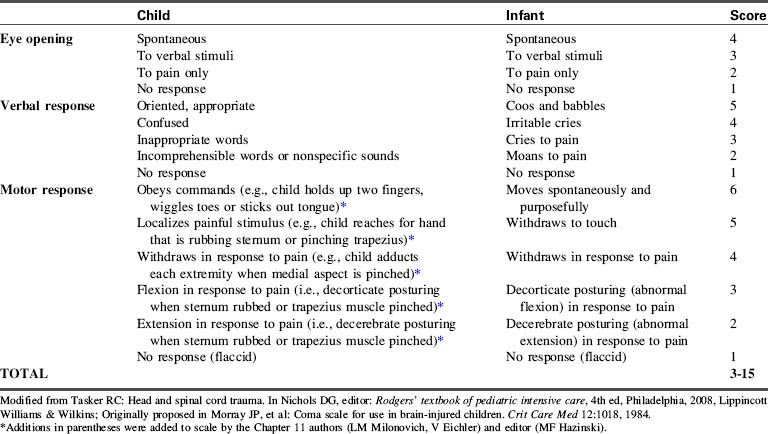
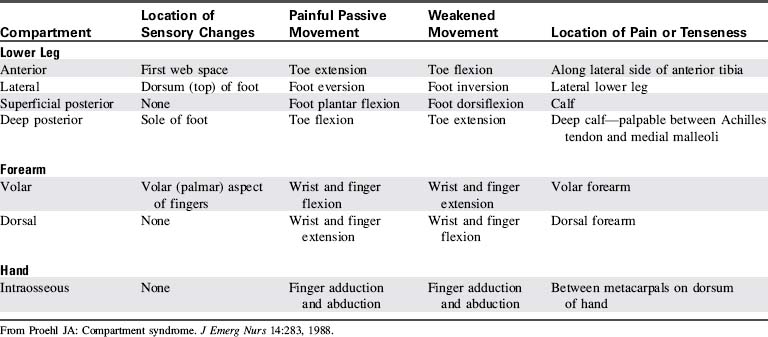
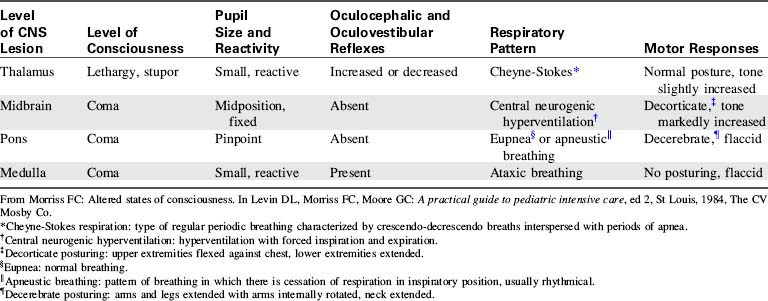
Providers should evaluate cranial nerve function when possible and immediately report any absence of cranial nerve function to the trauma surgeon or the trauma team leader. The nurse can often correlate patient neurologic function with the site of central nervous system injury through careful assessment of signs of cranial nerve function and evaluation of any abnormal posturing or respiratory patterns (Table 19-6).
Table 19-6 Relationship Between Anatomic Site of Injury, Level of Consciousness, Abnormal Pupil Response, Respiratory Patterns and Motor Responses
A CT scan will provide important information about the extent and severity of the head injury and potential causes of further deterioration, such as intraparenchymal, subdural, or epidural hemorrhage (Fig. 19-6). In addition, it will provide information about the need for surgical intervention. If a CT scan is performed to evaluate a head injury, the scan should include the upper cervical spine.23 Magnetic resonance imaging (MRI) has been used more often in recent years because it provides better detail of head injuries and may be more useful to predict outcome (see the following discussion under Neck and Spine).24
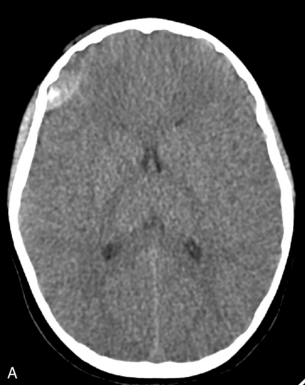

This child required urgent surgical intervention. (Images courtesy of Thomas Abramo, Nashville, TN.)
Brain injury causes the release of biomarkers that can be measured in the blood, cerebral spinal fluid, and extracellular brain fluid. These biomarkers include inflammatory mediators (e.g., interleukins, tumor necrosis factor), nerve growth factor, and adhesion molecules to proteins. Monitoring levels of biomarkers may be useful in evaluating the severity of brain injury and response to therapy and in predicting outcome.6,24
The trauma team and especially the bedside nurse should frequently assess the patient’s mental status. The use of a standardized scoring system will enable quantification of the patient’s progress and responsiveness and trends in the patient’s condition. The GCS or the modified (pediatric) GCS36 will be helpful (Table 19-7). Frequent assessments are needed to detect subtle signs of deterioration.
Occasionally children with diffuse cerebral injury will demonstrate sudden deterioration several hours after injury; such deterioration must be immediately detected and treated. For further information regarding the assessment and management of the child with head injury and increased intracranial pressure, see Chapter 11.
If spine trauma is suspected, hypotension persists, and hypovolemia and pericardial tamponade have been ruled out, then neurogenic shock may be present. Neurogenic shock results from a spinal cord injury that produces loss of autonomic (sympathetic nervous system) tone and results in vasodilation and hypotension (see below).25
The most consistent indicators of poor prognosis following closed head injury in children include flaccid paralysis and fixed, dilated pupils despite the restoration of satisfactory perfusion. Other poor prognostic indicators include the development of diabetes insipidus at or soon after admission (often indicates cessation of pituitary function), cardiovascular instability unrelated to hemorrhage, and disseminated intravascular coagulation. Brain injury results in the release of fibrinogen; severe head injury can result in substantial fibrinogen release and disseminated intravascular coagulation.3 Concentrations of some combinations of biomarkers of brain injury may predict poor outcome from head trauma, although research in this area continues to evolve.6,24
If a devastating neurologic injury is present and brain death is diagnosed or imminent, the family should be asked about organ donation. The request should be made in accordance with local protocols, which can vary by jurisdiction. For further information, see Brain Death in Chapter 11; see also Chapter 3.
Neck and Spine
If the child has a mechanism of injury that is consistent with possible spinal cord injury, has neurologic signs of spinal cord injury, or is comatose or hypotensive without neurologic signs, then the extrication collar should remain in place until spinal cord injury is ruled out; this requires a combination of clinical assessment, cervical spine radiographs, CT scan, and possibly an MRI (Fig. 19-7).23
It is difficult to rule out cervical spinal cord injury solely on the basis of anteroposterior and lateral radiographs and CT scans, because many children experience spinal cord injuries that are not associated with abnormalities in standard radiographs and CT scans.3,23,42a Historically, a complete radiographic cervical spine series includes anteroposterior and lateral cervical spine radiographs and oblique and odontoid views.32,69
In adults, the CT scan has largely replaced radiographs for evaluation of the cervical spine, particularly in obtunded patients,33 but similar comparison data have not been published for children.23 Cervical spine subluxation or vertebral fracture can be identified with CT scan, and the combination of spine radiographs and limited CT scan of the occiput to the third cervical spine can increase identification of cervical spine injuries in obtunded or young children.21,23
If the child is awake and oriented, the presence of neck or back pain is suggestive of vertebral injury.23,69 The National Emergency X-Radiography Utilization Study Group developed a decision instrument of clinical criteria to rule out cervical spine injuries in patients with blunt trauma (Box 19-6)32 that performed well in a multicenter trial involving more than 3000 children. However, the study authors recommended caution in interpreting the results because there were fewer than 90 infants and toddlers in the study.69
Box 19-6 Clinical Criteria to Help Rule Out Cervical Spine Injury in Children: Modified National Emergency X-Radiography Utilization Study Group (NEXUS) Criteria23,32,69
If all five of the following clinical indicators are met, the likelihood of cervical spine injury in the child with blunt trauma is low. These criteria were shown to be valid in a multicenter study of nearly 3000 injured children 2-18 years old.69 Use caution in application for infants and toddlers (few infants and toddlers were evaluated in the multicenter study).
1. Absence of tenderness at the posterior midline of the cervical spine
2. Absence of neurologic abnormality (e.g., focal neurologic deficits)
3. Absence of altered level of consciousness or intubation
5. Absence of clinically apparent pain that might distract the patient from the pain of cervical spine injury (i.e., absence of distracting injury or pain)
Chest
As noted previously, children have softer, more compliant rib cages than do adults. Therefore rib fractures are relatively uncommon, occurring in one third or less of children with blunt trauma. Severe intrathoracic injury may be present despite the absence of rib or sternal fractures or other manifestations of abnormality on external examination.3,13 However, thorough chest inspection and palpation should reveal obvious signs of injury. The nurse may note chest asymmetry associated with respiratory effort or caused by rib fractures. Careful auscultation should identify localized alteration in the intensity or pitch of breath sounds; pulmonary edema may cause crackles and hypoxemia.
Chest radiographs, including anteroposterior and lateral films, should be performed on any child with severe injury to the chest or torso.13 CT scans may provide additional information and detail, particularly to evaluate airway abnormalities and fluid collections. A pulmonary contusion will produce localized opacification of the lung (see Fig. 19-4) and increased density on the CT scan.
Although rare, cardiac contusions may be present in any child with a history of blunt thoracic trauma. Clinical signs include chest pain, arrhythmias, and myocardial dysfunction. The child may have a new murmur or evidence of congestive heart failure, including systemic and pulmonary edema and a gallop rhythm. The diagnosis is made by evaluating cardiac isoenzymes, a 12-lead ECG, and an echocardiogram.4
The cardiac troponin complex consists of three troponins (C, I, and T) that are involved in the interaction of the actin and myosin filaments in cardiac muscle.37 These troponins are normally present only in cardiac muscle, and their levels will rise with cardiac necrosis (death of heart muscle) and myocardial injury. In adults, concentrations of troponins I and T are monitored to determine the presence of an acute coronary syndrome; elevation of troponins I and T can be more sensitive indicators of myocardial injury than elevation of the creatinine kinase myocardial band (CK-MB).37 Although troponin concentrations are normally negligible in children, they are often elevated after cardiac contusion. It is important to note that not all children with cardiac contusion demonstrate elevation of troponins, and troponins may be elevated by conditions other than cardiac contusions.30
Abdomen
Hemorrhage from thoracoabdominal injuries is a leading cause of traumatic death in pediatric victims, as are head injury and complications of airway and ventilation.4,54a Children do not often have penetrating abdominal injuries; blunt abdominal trauma accounts for the vast majority of pediatric abdominal injuries.
Providers should examine the child carefully to identify both overt and subtle signs of intraabdominal injuries. Fifteen percent of injured children with negative abdominal examinations are subsequently found to have significant intraabdominal injuries, even in the presence of normal mental status and vital signs.4,13
Signs of abdominal hemorrhage are difficult to detect in the comatose patient or one with spinal cord injury and loss of abdominal sensation. In these patients, additional evaluation and diagnostic studies are needed. Emergency ultrasound and FAST are now the diagnostic tools of choice for unstable (particularly those who are obtunded) patients, because they can be performed at the bedside as often as necessary, without radiation exposure or the need to transport the patient. With these devices, free fluid or blood (i.e., hemoperitoneum) appears black against the gray of organs.42 FAST scans have a higher specificity (i.e., when fluid is observed, the child has intraabdominal bleeding) than sensitivity (i.e., children can have organ injury without detection of free fluid or blood in the abdomen). Therefore FAST is often used in conjunction with the CT scan to detect intraabdominal bleeding in children with trauma and hypotension.42
A CT scan will usually reveal the presence of significant injury (see below). As noted above, a screening trauma CT scan can be performed in many medical centers in less than 10 min. The CT series includes scans of the head, neck, chest, abdomen, and pelvis using a rapid scanner that requires no repositioning of the child or transport to different rooms in the radiology department. Peritoneal lavage is rarely used in children because it is not as accurate as the use of FAST or a CT scan. In addition, it will create a painful site that complicates later assessment of abdominal tenderness.4
Injuries resulting from improperly positioned lap belts frequently produce abdominal ecchymosis and bruising (Fig. 19-8). If the lap belt was positioned across the lower abdomen and not over the pelvis, the bruising may indicate the possibility of intestinal and lumbar spine injury (Fig. 19-9).55,66
Any visible bruising on the abdomen should raise the suspicion of an intraabdominal injury.43 The bruise itself makes it more difficult to examine the conscious child, because the bruise will cause abdominal wall tenderness that is difficult to distinguish from tenderness associated with intraabdominal injury. Pain itself may be difficult to evaluate. The severity of pain does not necessarily correlate with the severity of abdominal injury.
Progressive abdominal distension is one of the first signs of major abdominal injury, so measurement of the abdominal girth, especially in infants and young children, may be helpful. Pain and abdominal distension will reduce the child’s effective tidal volume and ventilation, altering the child’s respiratory rate, respiratory effort, and chest expansion (Box 19-7). Unilateral splinting of respirations with or without evidence of rib fracture is an indication for liver and spleen scans.58 Additional high-risk variables, in addition to abdominal tenderness and systolic hypotension, found to be sensitive for radiographically confirmed intraabdominal injury in children after blunt torso trauma include: femur fracture, elevated liver enzymes, microscopic hematuria, and an initial hematocrit less than 30% (see Box 19-7); however, these variables were not specific for intraabdominal injury.34
Box 19-7 Physical Findings Suggestive of Abdominal Injury
Physical Signs
• Abdominal tenderness (high-risk variable*)
• Flank or abdominal mass, contusion, or wound
• Blood in the urethral meatus, hematuria (NOTE: Microscopic hematuria with more than five RBCs per high-powered field is high-risk variable*)
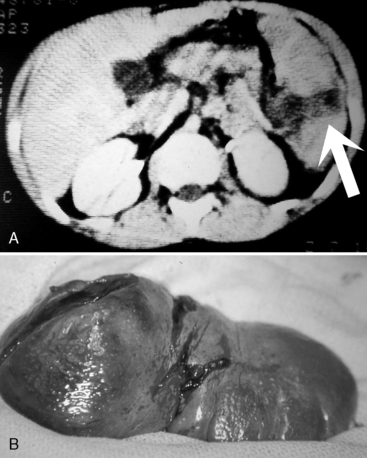
• Genital swelling or discoloration
Signs of splenic or hepatic injury include tachycardia, hypotension, and abdominal tenderness. The splenic injury will be apparent on a CT scan (Fig. 19-10). Splenic injury can cause a positive Kehr’s sign (referred pain to the left shoulder during compression of the left upper quadrant) and leukocytosis.13
Hepatic trauma (Fig. 19-11) can cause referred right shoulder pain instead of Kehr’s sign or left shoulder pain.13 Most significant hepatic injury will result in elevation of the serum transaminases (aspartate aminotransferase greater than 200 International Units/L and alanine aminotransferase greater than 125 International Units/L).28
Conservative management of splenic, hepatic, or renal contusions and lacerations includes supportive care and close observation in a PCCU. Typically, bleeding from such lacerations has ceased by the time the child arrives at the hospital, and these organs often will heal without intervention.4 If conservative management is provided, the child’s systemic perfusion must be monitored closely.
Surgical intervention is required in the presence of ongoing hemorrhage, hemodynamic instability (including the need for excessive fluid administration to maintain blood pressure and perfusion), hollow viscous perforation, or catastrophic organ injury.31 In hemodynamically stable patients, surgical exploration can be accomplished through laprascopy.64
When surgical intervention is required, the injured organ is often repaired rather than removed (see Evolve Fig. 19-3, A and B in the Chapter 19 Supplement on the Evolve Website for color surgical photographs of splenic injury and lap belt injury to the intestine). Removal of the injured spleen, liver lobe, or kidney usually is required only for devastating injury or if the organ is separated from its vascular supply.
Genitourinary Trauma
Genitourinary trauma is seldom life threatening. However, injured children are more prone to renal injuries than injured adults, because the kidneys are less well protected by muscle, ribs, and fat. Hematuria, abdominal pain, and flank hematomas are all signs of renal injury.13 The presence of threadlike clots in the urethra is a pathognomonic finding indicative of renal injury, and the amount of hematuria correlates well with the severity of renal trauma.62
Although insertion of a urinary catheter is routine during trauma resuscitation, a catheter should not be inserted in the trauma victim if frank blood is observed in the urinary meatus. Such blood often is caused by urethral disruption and is a contraindication to urinary catheter insertion.41 The presence of blood in the urinary meatus indicates the need for a retrograde urethrogram and urologic consultation.8a Severe renal injury with separation of the kidney from the urethra may not be associated with hematuria; these patients will demonstrate evidence of extravasation of urine that will be detected by a CT scan.
Bladder rupture should be suspected if any degree of hematuria is detected in the child with a pelvic fracture. A cystogram is indicated to rule out bladder injury.8a
Extremities
Long bone fractures and pelvic fractures can produce significant blood loss, especially in older children. When a pelvic fracture is suspected, the trauma team should assess the integrity of other structures within the pelvis, including the urethra, bladder, and pelvic vessels. Disruption of pelvic vessels can cause rapid and severe blood loss.4
Compartment Syndrome
Compartment syndrome occurs when external forces compress an area of muscle, or when bleeding or edema increase pressure within the compartment that is created by sheaths of fascia surrounding the muscle bundle and related nerves and vessels. As the pressure within the compartment rises, vascular supply to the muscle and tissue is compromised and ischemic and nerve damage may develop.52
Signs of compartment syndrome include pain that worsens with movement, edema, altered movement and sensation, and decreased perfusion (cooling of the extremity with decreased intensity of the pulses); these can be recalled by considering the “five P’s”: pain, pallor, pulselessness, paresthesia, and paralysis.4,52 A sixth P can be added—puffiness.63 Specific clinical findings associated with involvement of the major compartments are listed in Table 19-8. A physician or other on-call provider should be notified immediately if signs of compartment syndrome develop, because urgent surgical intervention may be needed.
Bedside Doppler ultrasound examination can be used to evaluate blood flow. If the pressure in the compartment is measured, a pressure exceeding 40 cm H2O is considered an indication for surgical intervention (i.e., fasciotomy), but normal pressures and pressure thresholds are not well established in children.60
Treatment of compartment syndrome requires surgical release of the restriction surrounding the muscle. A fasciotomy is performed and the area is left open, but covered with a sterile dressing, and may require later skin grafting (see, also, Chapter 20).52
Skin
During initial stabilization of the trauma victim, visibility of some areas of skin will be compromised by pressure dressings. Once the primary survey and stabilization have been accomplished, the undressed pediatric patient should be examined carefully for the presence of other injuries, including contusions and burns. If burns are present, the trauma team should plan fluid resuscitation based on the estimated burn depth and extent. For information about burns, refer to Chapter 20.
Most fire-related deaths result from smoke inhalation, and the most common cause of death during the first hour after burn injury is respiratory failure.2 A history of closed space confinement should lead to evaluation for the presence of carbon monoxide poisoning. The child should be inspected for (1) singed eyebrows and nose hair, (2) dark sputum, (3) carbon deposits and inflammatory changes in the mouth, (4) cyanosis and dyspnea, and (5) altered level of consciousness. Initial treatment includes oxygen administration and close observation for deteriorating respiratory status. Note that carboxyhemoglobin is not detected by a pulse oximeter, so pulse oximetry will be falsely high in the presence of carbon monoxide poisoning (see Pulmonary Injuries in Chapter 20).
History
The Advisory Committee on Immunization Practices recommends administering a tetanus booster every 10 years. Clean, minor wounds do not require prophylaxis unless the patient has not received tetanus toxoid in more than 10 years or the history is unknown.39 If the wound is tetanus prone, prophylaxis is recommended if the tetanus toxoid was administered longer than 5 years before the injury. The Surgical Infection Society recommends administration of 25 IU tetanus prophylaxis if the wound is tetanus prone (e.g., from a bite) and if the patient is elderly, immunocompromised, or has not completed the tetanus vaccination regimen. For children a dose of 4 IU/kg is recommended.35
Intentional injuries/inflicted trauma
Definition and Epidemiology
Intentional injuries are inflicted injuries (e.g., child abuse) or injuries that occur as a result of neglect. In the United States it is estimated that 1% or more of all children are abused or neglected, and approximately 4000 children die annually as victims of abuse.57
The term child abuse applies to any maltreatment of a child, including infliction of physical injuries, sexual exploitation, infliction of emotional pain, or neglect. Child abuse usually is not a random, isolated act of violence, but rather a pattern of maladjusted behavior. The three components of the child abuse syndrome include the maladjusted adult, the vulnerable child, and the presence of situational stressors.65 For more information, refer to Intentional Injury/Inflicted Trauma; Definition and Epidemiology in the Chapter 19 Supplement on the Evolve Website.
History of Injuries Suggesting Intentional Injuries (Inflicted Trauma)
It is estimated that as many as 10% of children younger than 5 years who are seen in EDs with traumatic injuries have inflicted injuries.57 Healthcare workers must be vigilant in attempting to detect evidence of abuse and are obligated to report suspected abuse to the local child protective agency.9
Explanations for traumatic injuries that should be questioned include unknown injury, implausible sequence of events, self-inflicted injury, or sibling-inflicted injury. Any injury followed by a delay in seeking medical care is suspicious. Finally, when a child or a spouse names an adult as the cause of the injuries, the accusation usually is true.57
Characteristics of Injuries Suggestive of Intentional Injury
Implausible injuries are those that are inconsistent with the history. For example, if a child allegedly sustained multiple bruises when falling down the stairs, bruises will most likely be located over bony prominences; bruises will rarely appear over soft tissues. If a head injury occurs when the child falls out of bed, usually a single lump is present, and the skull is not fractured. Although small linear skull fractures may occur with minor falls, loss of consciousness and multiple bruises are inconsistent with a simple fall.57
Subdural hematomas are among the most common results of inflicted head injury in children. Many subdural hematomas are associated with skull fracture, and some may be associated with retinal hemorrhage (the shaken baby syndrome). Scalp bruises and traumatic alopecia also may be observed in these victims.57
Inflicted head trauma12 (formerly called shaken baby syndrome) is the term used to encompass the spectrum of inflicted head injuries, including associated cerebral, spinal, and cranial injuries and their complications. The trauma can result from the combination of vigorous shaking of the child associated with the application of force (e.g., the child is shaken and struck or is shaken while being held against a mattress in bed). However, injuries can also result from blunt head trauma and may be associated with spinal cord injury or hypoxia.12 These injuries include the primary injury as well as secondary injuries such as hypoxia, ischemia, increased intracranial pressure, and long-term complications including seizures, developmental delay, and other disabilities.12
Signs of inflicted head trauma include retinal hemorrhages and subarachnoid hemorrhage documented by cerebrospinal fluid examination and a CT scan. Additional injuries include brainstem and spinal cord hematoma, subdural hematoma or cerebral contusion, and spinal cord injuries.12
Intentional injuries should also be considered if the child has shock that does not respond to conventional therapy. For example, if the child exhibits shock and has a history of vomiting and diarrhea or a nonspecific history, and the child’s perfusion and level of consciousness do not improve with adequate hydration, then other causes of shock should be considered, such as intraabdominal injury (Fig. 19-12).
Responsibilities of the Healthcare Team
A thorough examination is required to identify all current injuries and evidence of healed injuries. A skeletal series of radiographs and possibly a bone scan will be performed to identify healed fractures. Levels of biologic markers of head injury can be determined from blood or cerebral spinal fluid and can assist in the identification of head injury when inflicted trauma is suggested in the child without neurologic symptoms.,6 These markers can also be useful for monitoring the child’s response to therapy and for predicting outcome of the head injury.24
If a child abuse team is present in the hospital, they should be consulted about the proper recording of injuries and documentation of parental statements. This team also is experienced in examining abused children and frequently will identify additional injuries that may be related to abuse.40
Transition from the pediatric critical care unit after injuries
The transition from the PCCU to an acute care unit may be stressful for the patient, family, and pediatric nurses. The patient and family generally have established a relationship with the PCCU staff that started at a time when the family mobilized defenses against feelings of helplessness and anger about the child’s injuries. As the child’s condition improves, the family’s defenses may be dropped. Because it may still be uncomfortable for the family to express feelings of anger toward the child, they may instead redirect them toward the new staff.53
Long-term follow-up
Relatively few pediatric trauma patients require inpatient treatment at a rehabilitation center. Most pediatric trauma victims are discharged to their homes and require minimal follow-up, usually one or two return outpatient visits. Some children require home health nurses, physical or occupational therapy, or outpatient services provided by either the acute-care or rehabilitation facility.8
1 American Academy of Pediatrics. Management of pediatric trauma policy statement. Pediatrics. 2008;121:849-859.
2 American Academy of Pediatrics and American College of Emergency Physicians: Pediatric trauma. . APLS: the pediatric emergency medicine resource. ed 4, Sudbury, MA; Jones and Bartlett:2006
3 American College of Surgeons, Committee on Trauma. Advanced Trauma Life Support for Doctors. Extremes of Age: pediatric trauma, ed 7, Chicago: American College of Surgeons; 2004:242-261.
4 Baird J.S., Cooper A. Multiple trauma. In Nichols D.G., editor: Rogers’ textbook of pediatric intensive care, ed 4, Philadelphia: Lippincott, Williams and Wilkins, 2008.
5 Spinal cord injuries. In Barkin R., Rosen P., editors: Emergency pediatrics, ed 3, Mosby: St Louis, 1990.
6 Berger R.P., et al. Multiplex assessment of serum biomarker concentrations in well appearing children with inflicted traumatic brain injury. Pediatr Res. 2009;65:97-102.
7 Borse N.N., et al. CDC childhood injury report: patterns of unintentional injuries among 0-19 year olds in the United States, 2000-2006. Atlanta GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2008.
8 Brogan D.R. Rehabilitation service needs: physicians perceptions and referrals. Arch Phys Med Rehabil. 1981;62:215.
8a Brown R.L., Garcia V.F. Genitourinary trauma. In O’Neill J., Grossfeld J.L., Coran A.G., Fonkalsrud E.W., editors: Grossfeld: pediatric surgery, ed 6, Mosby: Saint Louis, 2006. an imprint of Elsevier
9 Carroll C.A., Haase C.C. The function of protective services in child abuse and neglect. In Heifer R.E., Kempe R.S., editors: The battered child, ed 4, Chicago: University of Chicago Press, 1987.
9a Chameides L., Samson S., Schexnayder S., Hazinski M.F., editors. Pediatric advanced life support provider manual. Dallas: American Heart Association, 2011.
10 Champion H.R., Sacco W.J., Carnazzo A.J., et al. Trauma score. Crit Care Med. 1981;9:672.
11 Champion H.R., Sacco W.J., Copes W.S., et al. A revision of the Trauma Score. J Trauma. 1989;29:623-629.
12 Christian C.W., Block R., Committee on Child Abuse and Neglect; American Academy of Pediatrics. Abusive head trauma in infants and children. J Pediatrics. 2009;123:1409-1411.
13 Cooper A., et al. Mortality and truncal injury: the pediatric perspective. J Pediatr Surg. 1994;29:33-38.
14 DeBoer S., et al. Intraosseous infusion: not just for kids anymore. EMS Magazine. 2005. March
15 Dowd M.D., Bull M. Emergency medicine and injury prevention: meeting at the intersection. Clin Ped Emerg Med. 2003;4:83.
16 Emergency Cardiovascular Care Committee and American Heart Association. Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, Part 12: Pediatric advanced life support. Circulation. 2005;112:IV167-IV187. 2005
17 Finkelstein E.A., Corso P.S., Miller T.R. Incidence and economic burden of injuries in the United States. New York: Oxford University Press; 2006.
18 Fletcher S.A., et al. The successful surgical removal of intracranial nasogastric tubes. J Trauma. 1987;27:948.
19 Garbarino J. Preventing childhood injury: developmental and mental health issues. Am J Orthopsychiatry. 1988;58:1.
20 Gardner H.G. Office-based counseling for unintentional injury prevention. Pediatrics. 2008;119:202.
21 Garton H.J., Hammer M.R. Detection of pediatric cervical spine injury. Neurosurgery. 2008;62:700-708.
22 Gausche M., Henderson D.P., Seidel J.P. Vital signs as part of the prehospital assessment of the pediatric patient: a survey of paramedics. Ann Emerg Med. 1990;19:173.
23 Gore P.A., Chang S., Theodore N. Cervical spine injuries in children: attention to radiographic differences and stability compared to those in the adult patient. Semin Pediatr Neurol. 2009;16:42-58.
24 Guerguerian A.M., Lo M., Hutchinson J.S. Clinical management and functional neuromonitoring in traumatic brain injury in children. Curr Opin Pediatr. 2009;21:737-744.
25 Harris B., et al. The crucial hour. Pediatr Ann. 1987;16:4.
26 Hazinski M.F., et al. Outcome of cardiovascular collapse in pediatric blunt trauma. Ann Emerg Med. 1994;201:1229-1235.
27 Hazinski M.F., et al. Pediatric injury prevention. Ann Emerg Med. 1993;22:456.
28 Hennes H.M., et al. Elevated liver transaminase levels in children with blunt abdominal trauma: a predictor of liver injury. Pediatrics. 1990;86:87.
29 Herzenberg J.E., et al. Emergency transport and positioning of young children who have an injury of the cervical spine: the standard backboard may be hazardous. J Bone Joint Surg Am. 1989;71:15.
30 Hirsch R., et al. Cardiac troponin I in pediatrics: normal values and potential use in the assessment of cardiac injury. J Pediatrics. 1997;130:872-897.
31 Hoelzer D.F., et al. Selection and nonoperative management of pediatric blunt trauma patients: the role of quantitative crystalloid resuscitation and abdominal ultrasonography. J Trauma. 1986;26:57.
32 Hoffman J.R., et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343:94-99.
33 Holmes J.F., Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma. 2005;58:902-905.
34 Holmes J.F., et al. Validation of a prediction rule for the identification of children with intra-abdominal injuries after blunt torso trauma. Ann Emerg Med. 2009;54:528-533.
35 Howdiesheel T.R., Heffernan D., Dipiro J.T. Surgical infection society guidelines for vaccination after traumatic injury. Surg Infect. 2006;7:275-291.
36 James H., Anas N., Perkin R.M. Brain insults in infants and children. New York: Grune and Stratton; 1985.
37 Kanaan U.B., Chiang V.W. Cardiac troponins in pediatrics. Pediatr Emerg Care. 2004;20:323-329.
38 Kaufman C.R., et al. Evaluation of the pediatric trauma score. J Am Med Assoc. 1990;263:69.
38a Kleinman M.E., Chameides L., Schexnayder S.M., Samson R.A., Hazinski M.F., Atkins D.L., Berg M.D., de Caen A.R., Fink E.L., Freid E.B., Hickey R.W., Marino B.S., Nadkarni V.M., Proctor L.T., Qureshi F.A., Sartorelli K., Topjian A., van der Jagt E.W., Zaritsky A.L. Part 14: pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S876-S908.
39 Kretzinger K., et al. Preventing tetanus, diphtheria and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine. Morbid Mortal Weekly Rep. 2006;55(R17):1-33.
40 Krugman R. The assessment process of a child protection team. In Heifer R.E., Kempe R.S., editors: The battered child, ed 4, Chicago: The University of Chicago Press, 1987.
41 Kuppermann N., et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374:1127.
42 Levy J.A., Noble V.E. Bedside ultrasound in pediatric emergency medicine. Pediatrics. 2008;121:e1401-e.1412.
42a Luerssen T.G. Central nervous system injuries. In O’Neill J., Grossfeld J.L., Coran A.G., Fonkalsrud E.W., editors: Grossfeld: Pediatric surgery, ed 6, St Louis: Mosby, 2006.
43 Lutz N., et al. Incidence and clinical significance of abdominal wall bruising in restrained children involved in motor vehicle crashes. J Pediatr Surg. 2004;39:972.
44 McDevitt B.E., Foltin G.L., Cooper A. Thoracic trauma. In: Baren J.M., et al, editors. Pediatric emergency medicine. Philadelphia: WB Saunders, 2008.
45 Nance M.L., Carr B.G., Branas C.C. Access to pediatric trauma care in the United States. Arch Pediatr Adolesc Med. 2009;163:512.
46 Nansel T.R., et al. Preventing unintentional pediatric injuries: a tailored intervention for parents and providers. Health Educ Res. 2008;23:656.
47 Nathans A.B., Fantus R.J. National Trauma Data Bank—Pediatric Report, version 8. Chicago: American College Of Surgeons; 2008.
48 National Safe Kids Campaign. Bicycle injury fact sheet. Washington DC: National Safe Kids Campaign; 2004.
49 Nelson C.S., Wissow L.S., Cheng T.L. Effectiveness of anticipatory guidance: Recent developments. Curr Opin Pediatr. 2003;15:630.
50 Ortega H.W., Shields B.J., Smith G.A. Bicycle attitudes regarding bicycle safety-related injuries to children and parental. Clin Pediatr. 2004;43:251.
51 Polk-Williams A., et al. Cervical spine injury in young children: a national trauma data bank review. J Pediatr Surg. 2008;43:1718-1721.
52 Proehl J.A. Compartment syndrome. J Emerg Nurs. 1988;14:283.
53 Ragiel C.A. The Impact of critical injury on patient, family, and clinical systems. Crit Care Q. 1984;7:73.
54 Ralston M., et al. PALS provider manual. Dallas: American Heart Association, 2006.
54a Ramenofsky M. Pediatric abdominal trauma. Pediatr Ann. 1987;16:4.
55 Reid A.B., Letts R.M., Black G.B. Pediatric Chance fractures: association with intra-abdominal injuries and seatbelt use. J Trauma. 1990;30:384.
56 Sasser S.M., et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage. Morbidity and Mortality Weekly Report. 2009;58(RRO1):1-35.
57 Schmitt B.D. The child with nonaccidental trauma. In Heifer R.E., Kempe R.S., editors: The battered child, ed 4, Chicago: The University of Chicago Press, 1987.
58 Seidel J., Henderson D. Prehospital care of pediatric injuries. Los Angeles County, Torrance, CA: Harbor UCLA Medical Center; 1987.
59 Seidel J.S., et al. Emergency medical services and the pediatric patient: are needs being met? Pediatrics. 1984;5:769.
60 Shadgun B., et al. Diagnostic techniques in acute compartment syndrome of the leg. J Orthop Trauma. 2008;22:581-587.
61 Spivey W.H.L. Intraosseous infusions. J Pediatr. 1987;111:639.
62 Stalker H.P., Kaufman R.A., Stedje K. The significance of hematuria in children after blunt abdominal trauma. AJR Am J Roentgenol. 1990;154:569.
63 Strange J.M., Kelly P.M. Musculoskeletal injuries. In: Cardona V.D., et al, editors. Trauma nursing: from resuscitation through rehabilitation. Philadelphia: WB Saunders, 1988.
64 Streck C.J., Lobe T.E., Pietsch J.B., Lovvorn H.N.3rd. Laparoscopic repair of traumatic bowel injury in children. J Pediatr Surgery. 2006;41(11):1864-1869.
65 Steele B. Psychodynamic factors in child abuse. In Heifer R.E., Kempe R.S., editors: The battered child, ed 4, Chicago: The University of Chicago Press, 1987.
66 Stylianos S., Harris B.H. Seatbelt use and patterns of central nervous system injury in children. Pediatr Emerg Care. 1990;6:4.
67 Tepas J.J.: Update on pediatric trauma: severity scores. Report of the Ninety-Seventh Ross Conference on Pediatric Research: Emergency Medical Services for Children, Columbus. Ross Laboratories, Inc: 1989
68 Thompson R.S., Rivara F.P., Thompson D.C. A case-control study of the effectiveness of bicycle safety helmets. N Engl J Med. 1989;320:1361.
69 Viccellio P., Simon H., Pressman B.D., et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108:E20.
70 Zuckerman B.S., Duby J.C. Developmental approach to injury prevention. Pediatr Clin North Am. 1985;32:1.

 Be sure to check out the supplementary content available at
Be sure to check out the supplementary content available at