Pediatric Fever
Fever is the most common chief complaint of pediatric patients presenting to the emergency department (ED), accounting for up to 20% of ED visits. Most cases of fever are viral in origin, are benign in course, and resolve spontaneously. Fever tends to be of a higher clinical importance in younger children as they are immunologically immature and incompletely vaccinated. Management of children presenting to the ED varies dramatically by the age of the child, with the following common, albeit arbitrary, divisions: 0 to 28 days, 1 to 2 months, 2 to 3 months, 3 to 6 months, 6 to 36 months, and 3 years to adulthood.1 These divisions reflect differing immunologic and vaccination milestones as well as the spectrum of age-specific pathogens.
Perspective
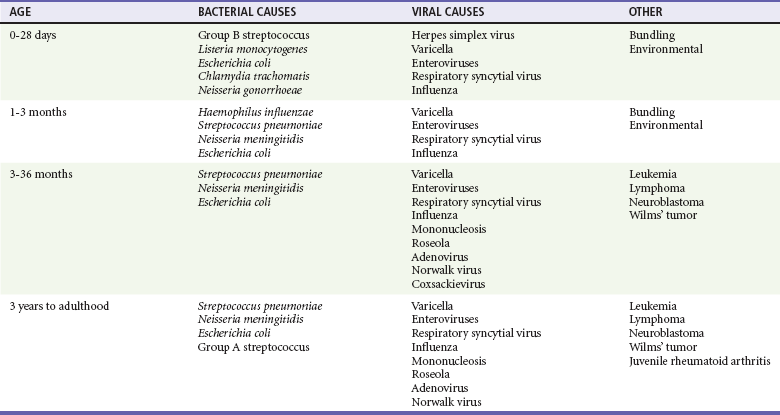
The cause of fever varies with the age of the child (Table 167-1). The majority of pediatric fever is due to infections, and most infections are attributable to a viral source. Upper respiratory infections, viral gastroenteritis, croup, bronchiolitis, stomatitis, roseola, infectious mononucleosis, and varicella are all known causes of fever. Most viral illnesses are benign and self-limited, but infection with herpes simplex virus (HSV) or respiratory syncytial virus (RSV), particularly in the first month of life, can lead to significant morbidity and mortality.
Bacterial disease is also an important cause of fever in children. Serious bacterial illness (SBI) is typically defined as the presence of pathogenic bacteria in a previously sterile site and includes urinary tract infection (UTI), bacteremia, meningitis, osteomyelitis, bacterial gastroenteritis, bacterial pneumonia, cellulitis, and septic arthritis. Studies have found the risk of SBI in febrile infants younger than 3 months with a temperature above 38.0° C to be between 6 and 10%; children younger than 28 days have the highest incidence.2 Pathogens change during early infancy, with vertical transmission of organisms such as group B streptococcus, Listeria monocytogenes, and HSV being more common in neonates. By 1 to 2 months of age, organisms such as Streptococcus pneumoniae, Neisseria meningitidis, and urinary pathogens (Escherichia coli or Enterococcus) become more common. In all children younger than 3 months, the urinary tract is the most common site of infection, followed by bacteremia and meningitis. UTIs are more common in white girls compared with other races and are of higher prevalence in patients in whom no source for infection is found and who have higher temperatures (i.e., >39.0° C).3
Children younger than 3 months may present with an apparent viral syndrome and still harbor serious bacterial illness. Levine and colleagues studied 1248 infants younger than 60 days who had temperatures above 38.0° C. Of these children, 22% were positive for RSV. Although, overall, children with documented RSV had a lower incidence of concomitant SBI than did those without RSV (12.5 vs. 7%), there was no significant difference in rates of SBI in children younger than 28 days (14.2% in RSV-negative neonates vs. 10.1% in RSV-positive infants). Most of the bacterial infections were UTIs.4 Older children 3 to 36 months of age with recognizable viral syndromes (e.g., croup, bronchiolitis, varicella, stomatitis) have a very low incidence of bacteremia. Greenes and co-workers found that among 1347 patients with temperature above 39.0° C who had a recognizable viral syndrome, the risk of bacteremia was 0.2%.5
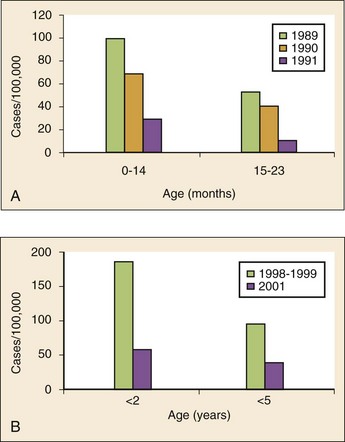
Occult bacteremia describes the presence of pathogenic bacteria in the bloodstream of a well-appearing febrile child in the absence of a focus of infection; it was first described as a clinical entity in the 1970s.6 The term typically refers to children 3 to 36 months of age who are highly febrile (>39.0° C) but appear well. Before the adoption of the conjugate vaccines against Haemophilus influenzae type b and S. pneumoniae, the incidence of bacteremia in this population was approximately 5%.7,8 Vaccination has proved remarkably effective, nearly eradicating H. influenzae type b as a significant pathogen and greatly reducing the burden of pneumococcal disease (Fig. 167-1).9–11 Currently, the rate of occult bacteremia is below 1%, with pathogens such as N. meningitidis becoming proportionally more prevalent. Continued surveillance is ongoing to ensure that there is not a rise in invasive disease caused by nonvaccine serotypes. Urinary pathogens, occurring in 2% of febrile children younger than 5 years, continue to be an important source of bacterial illness in infants and children. Rates are highest in boys younger than 6 months (2.7%) and girls younger than 12 months (6-8%).12,13
Bacterial illness in school-age children and adolescents includes focal infections, such as streptococcal pharyngitis, cellulitis, and pneumonia as well as bacteremia and meningitis. N. meningitidis has a bimodal distribution, with the highest incidence in children younger than 12 months (9.2/100,000 population). A second peak occurs during adolescence, when the rate of illness is 1.2/100,000 population, with a significant proportion of cases occurring in college students who reside in a dormitory setting (3.2/100,000 population).14
Distinguishing Principles of Disease
History
In dealing with a febrile child, history taking should focus on the length of illness, presence of localizing symptoms, and any pertinent past medical history. In infants younger than 28 days, birth history, particularly the presence of potentially transmittable maternal infection (HSV or group B streptococcus), is critically important. Immunization status, sick contacts, use of antipyretics before evaluation, and prior use of antibiotics are also important historical items. Defervescence after acetaminophen administration has not been shown to reliably exclude bacteremia in children of any age.15 Prior antibiotic use may mask the classic findings in diseases such as meningitis. Cough and congestion may suggest pneumonia or viral upper respiratory infection, whereas a harsh, barking, or seal-like cough is often a predominant complaint in viral laryngotracheitis (croup). Parents may report vomiting and diarrhea as a component of gastroenteritis or the presence of sore throat and lymphadenopathy with viral or streptococcal pharyngitis. Decreased oral intake or decreased urine output is frequently a complaint in gastroenteritis, but it may also be seen in patients with stomatitis as the painful aphthous ulcerations in the mouth make fluid intake difficult. Any history of lethargy, irritability, or altered mental status can be elicited with severe dehydration but raises the specter of meningitis or encephalitis. A rash occurs in many viral illnesses, such as roseola, but it also may be seen in life-threatening conditions, such as meningococcemia, Rocky Mountain spotted fever, and toxic shock syndrome. Complaints of headache and neck pain (meningitis or encephalitis) or ear pain (otitis media) are also important historical points.
Physical Examination
The physical examination of the febrile child should begin with a complete set of vital signs, including pulse oximetry. Hypoxia or significant respiratory distress manifested by tachypnea, grunting respirations, nasal flaring, or retractions may accompany sepsis or pulmonary infection. Stridor can be seen with croup but also with retropharyngeal abscess, epiglottitis, or bacterial tracheitis. Signs of shock, such as hypotension and poor peripheral perfusion, should be noted. Children typically mount a tachycardic response to fever, and hypotension is often a late and dire finding. Tachycardia is often due to the fever itself, but tachycardia out of proportion to the degree of fever is often seen in other conditions, such as early shock, myopericarditis, and dehydration. Greenes and colleagues found that in infants younger than 12 months, heart rate increases linearly by 9.6 beats/minute with each 1° C increase in body temperature; however, caution must be exercised in attributing tachycardia to fever alone.16 Once oxygenation, ventilation, and perfusion have been assessed and deemed adequate, the physical examination should focus on a thorough search for focal infection. In young infants, particularly those younger than 3 months, and in children who lack immunocompetence, fever may be the only presenting sign of serious illness, including meningitis. The physical examination in this age group is sufficiently insensitive to exclude SBI, and clinicians should not be falsely reassured by a normal physical examination in small children.
Ancillary Testing
Numerous laboratory and radiographic studies can be used to evaluate the febrile child. In general, testing should be directed at identification of the source of infection or evaluation for complications. Several guidelines exist for the evaluation of febrile children, although there is marked variation in adherence to these guidelines. Pantell and associates found that office-based practitioners followed published guidelines only 42% of the time in the evaluation of febrile children.17 Clinicians with less experience and those based in the hospital tend to order more tests compared with more experienced clinicians and those practicing in an office setting.
White Blood Cell Count
An elevated white blood cell (WBC) count (>15,000/mm3) can be an indicator of bacteremia but is also present in many viral illnesses. Leukopenia (<5000/mm3) can also be a sign of SBI or early sepsis. Pneumococcal infection is classically associated with leukocytosis, whereas infection with N. meningitidis and H. influenzae may be present even with normal WBC counts. Lee and colleagues found that the rate of pneumococcal bacteremia increased from 0.5% in highly febrile children (>39.0° C) with a WBC count between 10,000 and 15,000/mm3 to 3.5% if the WBC count was 15,000 to 20,000/mm3 and up to 18% with a WBC count above 30,000/mm3.18
The WBC differential has also been used to risk stratify febrile children in various models; an increase in polymorphonuclear leukocytes and immature band forms increases the risk of bacterial disease. A rise in polymorphonuclear leukocytes is also seen early in some viral infections. An absolute neutrophil count (ANC) above 10,000/mm3 suggests increased risk of pneumococcal bacteremia in febrile children (0.8% for children with an ANC below 10,000/mm3 vs. 8% for children with an ANC above 10,000/mm3).19
Blood Culture
A blood culture is a useful diagnostic test when bacteremia is suspected. In infants and children, blood should be obtained after sterile preparation of the skin, which includes an alcohol preparation and swabbing of the skin with povidone-iodine solution, which is then allowed to dry. Many centers obtain blood for culture during intravenous catheter placement after sterile preparation of the skin has been performed. This technique has the advantage of eliminating a second venipuncture solely to obtain blood for culture, although the rates of contamination with this technique have been shown to be higher in children (9.1 vs. 2.8%).20 The risks of contamination should be weighed against the ability to obtain blood through a separate venipuncture. The yield of a single blood culture in infants and small children is actually good. The routine sending of more than one sample is generally not needed, and bacteremia is often accurately detected even if only 0.5 to 1 mL of blood is obtained. The advent of automated blood culture systems led to the identification of true pathogens more quickly than by traditional methods, often within 24 hours. Pathogens isolated in the first 24 hours are more likely to be true pathogens than are bacteria isolated after 24 hours.21
Urinalysis and Urine Culture
UTI is defined as the combination of bacteriuria and pyuria. Bacteriuria in the absence of WBCs on microscopic examination represents asymptomatic bacteriuria. Urine is typically analyzed with a dipstick, followed by microscopic analysis of a centrifuged specimen of urine. Hoberman and colleagues described the test characteristics of an “enhanced” urinalysis, which is examination with a hemocytometer of an unspun specimen of urine for pyuria (defined as >10 WBCs per high-power field) or the presence of any bacteria per high-power field in Gram’s stain of unspun urine. They reported a negative predictive value of 99.8%, perhaps making urine culture unneeded if pyuria and bacteriuria are absent by use of the enhanced urinalysis method.22 Many centers are not using this enhanced method. Because dipstick and microscopic analysis have lower sensitivities, most experts recommend sending urine for culture in high-risk groups (febrile girls <24 months of age, uncircumcised boys <12 months of age, and circumcised boys <6 months of age).
Lumbar Puncture
A sample of cerebrospinal fluid (CSF) should be obtained from any child with signs and symptoms of meningitis. Fluid should be obtained with the smallest pencil-point or noncutting spinal needle possible (typically a 22-gauge spinal needle) and sent for cell counts, manual differential, Gram’s staining, culture, and measurement of CSF protein and glucose concentrations. Meningoencephalitis due to HSV is a potential cause of fever, particularly in children, and if it is suspected, sending of CSF for HSV polymerase chain reaction testing is indicated. The CSF in bacterial meningitis typically contains more than 1000 WBCs/mL, although there is considerable overlap in the CSF profile of bacterial and viral meningitis, making a determination of viral or aseptic meningitis difficult on the basis of CSF parameters such as cell count, protein, and glucose; thus CSF culture of a pathogenic bacterium is the “gold standard.” A prediction rule has been developed and validated to differentiate bacterial from aseptic meningitis.23 Children who lack all of the following criteria have a low risk (0.1%) of bacterial meningitis: positive CSF Gram’s stain, CSF ANC of at least 1000 cells/mL, CSF protein concentration of at least 80 mg/dL, peripheral blood ANC of at least 10,000 cells/mL, and history of seizure before or at the time of presentation. This may obviate the need for empirical antibiotic therapy and hospital admission in some children who are at low risk for bacterial meningitis.
Contraindications to lumbar puncture include cellulitis over the proposed site of puncture, cardiopulmonary instability, bleeding diathesis or platelet count below 50,000/µL, focal neurologic deficits, and signs of increased intracranial pressure, including papilledema. In these patients, lumbar puncture should be deferred until the child is stable, and blood should be obtained for culture while the child is treated empirically, recognizing that up to 50% of children with meningitis will not have bacteremia.24
CSF contaminated by blood, or a traumatic lumbar puncture, can make interpretation of cell counts and differentials difficult. In these cases, fluid should be obtained for Gram’s stain and culture and the child treated presumptively for meningitis until culture data are available. Nigrovic and co-workers have shown that risk factors for a traumatic lumbar puncture include operator experience, excessive patient movement during the procedure, advancement of the needle with the stylet in place, and lack of local anesthesia.25
Chest Radiography
Chest radiographs may be useful in the workup of the febrile child and are indicated when hypoxemia, respiratory distress, tachypnea, or focal findings on lung examination are present. Children younger than 6 months may present with tachypnea as the sole finding of bacterial pneumonia. Truly occult pneumonia can also occur, particularly in the highly febrile child (>39.0° C) without apparent source of fever. Bachur and associates found that 26% of children with temperature above 39.0° C and WBC counts higher than 20,000 had radiographic evidence of pneumonia.26 Of note, this study was done in the era before the conjugate pneumococcal vaccine.
Rapid Viral Antigen Testing
Many clinical laboratories have the ability to perform rapid viral antigen testing for such common pediatric viral illnesses as influenza A and B and RSV. The presence of a viral “source” for the fever in an ill child may obviate the need for expensive, painful, and lengthy diagnostic workups for bacterial processes. Bonner and colleagues evaluated the impact of physician knowledge of the presence of a positive rapid influenza assay result.27 The investigators studied 391 patients aged 2 months to 21 years who presented with classic signs and symptoms of influenza. Of these patients, more than half had positive rapid assays for influenza, and the investigators noted that significantly fewer laboratory and radiographic studies were ordered if the treating clinician was aware of these results. There were also fewer antibiotics prescribed. A large multicenter trial of febrile infants 60 days of age or younger revealed a decreased risk (2.5 vs. 11.7%) if the infant was influenza positive.28
Specific Disorders
General Approach to the Febrile Infant and Child
Every effort should be made to obtain appropriate specimens for culture (blood and urine), even in the critically ill child, before antibiotic administration. Lumbar puncture may be deferred in the critically ill child until stabilization occurs. Empirical antibiotic therapy should be directed at the most likely causative organisms based on age. Sterilization of the CSF occurs quickly once antibiotic administration has been initiated: within 15 minutes to 2 hours in patients with meningococcal meningitis and within 4 to 10 hours in patients with pneumococcal meningitis.29
Serious Bacterial Illness
Children presenting with temperature above 38.0° C who are younger than 28 days are at particularly high risk for bacterial illness, with rates as high as 12% quoted in the literature.30,31 Often, fever is the only manifestation of potentially life-threatening disease, and other signs and symptoms may be exceedingly subtle. This has led to an aggressive approach to diagnostic testing, empirical antibiotic therapy, and hospitalization in this age group, even if the child appears well.
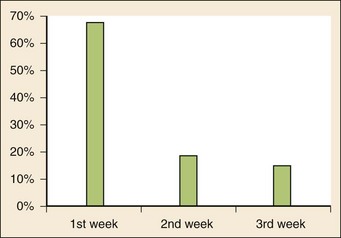
Children in this age group often present with nonspecific complaints, such as irritability, lethargy, poor feeding, and grunting. Besides fever, other signs of serious illness include a bulging fontanel, mottled extremities, petechiae, and tachypnea. Bacterial pathogens in this age group include group B streptococcus, L. monocytogenes, N. meningitidis, S. pneumoniae, and E. coli. Viral pathogens, including RSV and HSV, are also important considerations. Neonatal HSV infection in particular carries a high degree of morbidity and mortality and should be considered in any febrile neonate with a maternal history of genital herpes, who appears ill, who presents with fever and seizure, who has cutaneous vesicles on physical examination, or who has evidence of transaminitis or coagulopathy. HSV meningoencephalitis should also be considered in patients with fever and CSF pleocytosis but a negative CSF Gram’s stain. The risk period for HSV disease tends to be between 2 and 12 days of age (Fig. 167-2). Other noninfectious causes of a septic-appearing neonate include the acute salt-wasting crisis associated with congenital adrenal hyperplasia and undiagnosed duct-dependent congenital heart disease.
Because of the high risk of bacterial pathogens and the difficulty in clinical assessment of children younger than 28 days, these patients require an aggressive diagnostic evaluation, including a complete septic workup. This consists of a complete blood count (CBC) with differential, blood culture, urinalysis and urine culture, and lumbar puncture. Lumbar puncture is indicated even in the presence of a UTI because of the risk of concomitant meningitis.32 All children in this age group should be admitted to the hospital with empirical antibiotics until culture data become available. Appropriate parenteral antibiotic regimens include ampicillin (100 mg/kg/24 hr divided every 6 hours) plus either gentamicin (5 mg/kg/24 hr divided every 8 to 12 hours) or cefotaxime (150 mg/kg/24 hr divided every 8 hours). Ceftriaxone should be avoided in infants younger than 28 days because of a theoretic risk of inducing acute bilirubin encephalopathy as ceftriaxone causes bilirubin to be displaced from its protein binding sites. Empirical acyclovir should be added if risk factors for HSV disease exist (60 mg/kg/24 hr, divided every 8 hours).
Infants 29 to 90 Days of Age
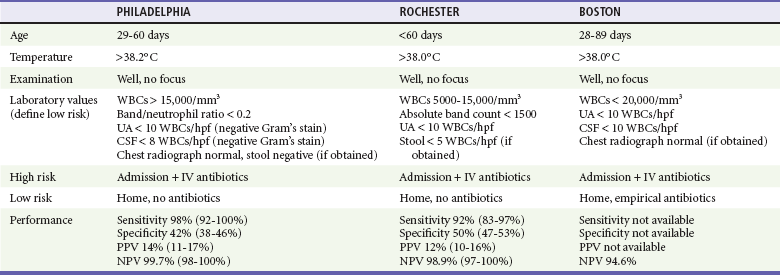
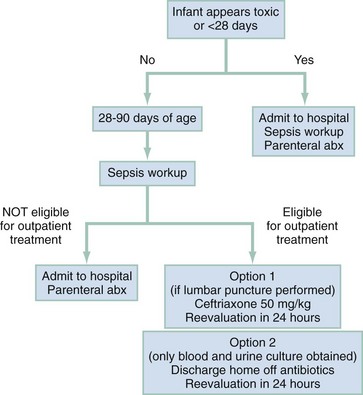
Various strategies (herein referred to as the Rochester, Philadelphia, and Boston criteria) for the evaluation of well-appearing children have been reported, compared, and retested in the literature.33–35 Each strategy has unique features, including the definition of fever (38.0° C vs. 38.2° C), the study population (0-3 months of age, 1-2 months of age, and 1-3 months of age), the clinical and laboratory variables studied, and the disposition (hospitalization with or without antibiotics or outpatient treatment with or without antibiotics). Each strategy seeks to identify a set of low-risk criteria that, if met, will allow less aggressive treatment or the withholding of empirical antibiotic therapy. The three main strategies are highlighted in Table 167-2. Baraff synthesized the recommendations of the Rochester, Philadelphia, and Boston criteria into an algorithm for the management of the previously healthy febrile infant 29 to 90 days of age (Fig. 167-3).36 To be low risk, the child had to have been previously healthy with an uncomplicated nursery stay, to be nontoxic clinically, and to have no focal source of bacterial infection. Low-risk laboratory criteria in this schema included a normal WBC count (between 5000 and 15,000 WBCs/mm3), fewer than 1500 bands/mm3, normal urinalysis (negative Gram’s stain and <5 WBCs per high-power field), and negative CSF Gram’s stain and cell counts (<8 WBCs/mm3), if obtained. When diarrhea was present, fewer than 5 WBCs per high-power field was the threshold for low risk.
Infants 3 to 36 Months of Age
The history in this age group should focus on the duration of illness, associated symptoms that may focus the evaluation, immunization history (particularly vaccination for H. influenzae type B and pneumococcus), and sick contacts. A thorough physical examination is essential to rule out serious focal infection, such as meningitis. Young children may demonstrate inconsolable irritability or lethargy as the sole manifestation of meningitis; furthermore, classic meningeal signs, such as nuchal rigidity, are seen in less than 27% of infants (0-6 months) with bacterial meningitis.37
Prior research has focused on assessment of children in this age group for the presence of occult bacteremia. It was found that a small percentage of highly febrile children (>39.0° C) 3 to 36 months of age were bacteremic.36,38–41 These children were noted to be highly febrile but lacked any localizing signs of infection. No historical or physical examination findings were sufficiently sensitive or specific to identify cases of occult bacteremia, making universal diagnostic testing necessary.42–44 A typical workup included a CBC and blood culture, and empirical antibiotic therapy was prescribed for children with WBC counts above 15,000/mm3. Empirical antibiotics were justified on the basis of studies that revealed treatment with antibiotics prevented focal sequelae of bacteremia such as meningitis and shortened the duration of fever.45–47 Before the advent of almost universal immunization against S. pneumoniae, the rate of occult bacteremia was approximately 3%, and although pneumococcal bacteremia resolves without therapy up to 75% of the time, a small proportion of children have sepsis or focal infections such as meningitis. Pneumococcal meningitis has a high degree of morbidity and mortality, including permanent neurologic disability, hearing loss, and death.48,49 Since the advent of Prevnar (conjugate pneumococcal vaccine), the number of invasive pneumococcal infections caused by vaccine-serogroup isolates among eight U.S. children’s hospitals has decreased more than 75% among children younger than 24 months. Because of the decline in invasive pneumococcal disease brought on by vaccination, the cost-effectiveness of mandatory blood testing has been called into question.50,51 Lee and colleagues evaluated the cost-effectiveness of various management strategies: no workup, relying on clinical judgment, blood culture, blood culture plus empirical antibiotics, WBC count plus blood culture and empirical antibiotics, and WBC count plus selective blood culture for WBC counts above 15,000 and empirical antibiotics. They found that at rates of pneumococcal bacteremia greater than 1.5%, obtaining a WBC count plus selective blood culture and empirical antibiotics were the most cost-effective approach. At rates of pneumococcal bacteremia less than 0.5%, strategies that used empirical testing and treatment were no longer cost-effective. They concluded that at lower rates of bacteremia, clinical judgment is more useful in selecting out high-risk populations who might benefit from selective testing and treatment.52
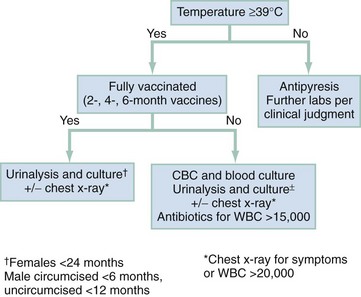
Although the incidence of pneumococcal bacteremia has declined in infants 3 to 36 months of age because of the aggressive campaign to vaccinate, infants 3 to 6 months of age have not yet completed the primary series of immunizations against S. pneumoniae and to a lesser extent H. influenzae. Thus, highly febrile infants (>39.0° C) without an apparent source on examination should be considered at risk for occult bacteremia and consideration given to obtaining a WBC count and blood culture as a screen. Empirical antibiotic therapy should be reserved for infants with WBC counts above 15,000/mm3 or those with an ANC ≥10,000/mm3. Although the conjugate pneumococcal vaccine contains antigens from the seven most common serotypes that cause invasive disease, there are approximately 90 serotypes that are capable of infecting humans. Continued bacterial surveillance is necessary to ensure that other serotypes do not rise in incidence to fill the void left by vaccination. No clinical prediction algorithm correctly identifies all patients with meningococcal disease.53 Additional signs and symptoms that may suggest meningococcemia are purpuric rash, bandemia, limb pain, and exposure to a person with the disease. An appropriate flow diagram for the workup of febrile infants 3 to 36 months of age is presented in Figure 167-4.
Children Aged 3 Years to Adulthood
The incidence of occult bacteremia decreases after 3 years of age. Focal infections such as streptococcal pharyngitis, septic arthritis, pneumonia, peritonsillar abscess (most often in adolescents), and cellulitis become more common. Viral pathogens are also common, such as infectious mononucleosis. Infection with atypical pathogens, such as Mycoplasma pneumoniae, should also be considered in children presenting with pneumonia. Skin infections secondary to community-acquired methicillin-resistant Staphylococcus aureus (CMRSA) are also becoming more common. CMRSA occurs in all age groups but has clustered among such children as wrestlers (associated with contaminated wrestling mats) and football players (infected equipment).54,55 This diagnosis should be considered in all children who present with pyogenic skin infection and skin abscesses. Appropriate therapy includes incision and drainage of the abscess cavity. Antibiotic therapy in addition to incision and drainage for simple abscesses has not been shown to hasten resolution of the infection but should be considered for patients with large abscesses (>5 cm), with cellulitis, or with fever.56 The antibiotics used are dependent on local resistance patterns but could include trimethoprim-sulfamethoxazole or clindamycin.
There is also a second peak in incidence of meningococcal disease in adolescent children with an attack rate of 1.2 infections per 100,000 population. As opposed to infants, adolescents with meningococcal infection are more likely to present with meningococcemia (40 vs. 20%) and shock (69 vs. 27%) and to have a fatal outcome (22.5 vs. 4.6%). Meningococcal disease typically is manifested with one of three clinical syndromes: meningitis, bacteremia, or a combination of the two. College students residing in dormitories are at particular risk for infection, with attack rates of 3.2/100,000 population.57 The history in cases of meningococcal infection is often one of rapidly progressive fever, headache, and stiff neck. Shock, altered mental status or frank coma, petechiae or purpura, seizures, and myalgias are also seen. Some of the first signs of meningococcal infection include leg pain, cold hands and feet, and abnormal skin mottling.58 Children exposed to a patient with meningococcemia, particularly those with close contact with nasopharyngeal secretions, and who have any of the presenting signs should receive a full septic workup, admission to the hospital, and empirical treatment with antibiotics until results of blood and CSF cultures are known. Appropriate initial therapy for children suspected of having meningococcal infection is ceftriaxone 100 mg/kg IV.
In January 2005, the Food and Drug Administration approved the quadrivalent meningococcal conjugate vaccine (Menactra) for use in adolescents. This vaccine is a polysaccharide-protein conjugate directed against the four serotypes that cause most cases of invasive meningococcal disease in humans. The Advisory Committee on Immunization Practices recommends vaccination of adolescents at their 11- or 12-year-old well-child checkup, and the American Academy of Pediatrics (AAP) has also advised that all college freshmen living in dormitories be vaccinated. Use of the vaccine is associated with a 67% decrease in invasive disease and a 66% decrease in carriage rates.59
Febrile Seizures
Differentiation of a benign febrile seizure from one that heralds CNS infection can be difficult. The AAP has published consensus guidelines for the evaluation and management of febrile seizures.60 Laboratory and radiographic evaluation should be directed at finding the source of the fever, not driven by the seizure itself. The AAP suggests that a lumbar puncture be performed in any child with signs of meningeal irritation after the first febrile seizure and be considered in children who are incompletely immunized or have received prior antibiotic therapy. Routine referral for neuroimaging or electroencephalography is not indicated.61 There is also no role for antiepileptic therapy after a single febrile seizure. Two retrospective studies have shown that the incidence of meningitis after the simple or complex febrile seizures is exceedingly low and that infants with meningitis will demonstrate signs of sepsis or meningitis after the seizure, making empirical lumbar puncture based solely on a febrile seizure unnecessary.62,63
Fever and Petechiae
The presence of a petechial rash in the setting of a febrile illness is classically associated with meningococcal infection. In fact, Baker and colleagues found that the incidence of meningococcal infection was 7 to 11% in patients hospitalized with fever and petechiae.64 The rate of bacteremia of any cause was found to be much lower (1.9%) in an ED population. The differential diagnosis of fever and petechiae also includes disseminated intravascular coagulation, Rocky Mountain spotted fever, pneumococcal bacteremia, Streptococcus pyogenes infection, various viral infections, idiopathic thrombocytopenic purpura, Henoch-Schönlein purpura, and leukemia. Petechiae can also be caused mechanically from a tourniquet, retching, or violent coughing. Petechiae due to vomiting or coughing are typically confined to the skin above the nipple line, but petechiae caused by SBI can have any distribution.
Because of the risk of serious illness in children with fever and petechiae, blood should be obtained for CBC and culture. In cases associated with pharyngitis, testing for group A streptococcus infection is indicated. Mandl and colleagues performed a prospective cohort study of 411 patients presenting to a pediatric ED with temperature higher than 38.0° C and petechiae in the hope of identifying clinical and laboratory criteria that would provide a means to screen for bacteremia.65 They found that an abnormal WBC count (<5000 WBCs/mm3 and >15,000 WBCs/mm3) or abnormal coagulation studies were predictive but not diagnostic of invasive bacteremia. Also, well-appearing children with normal WBC and coagulation studies were exceedingly unlikely to have invasive bacteremia. In their study, only two well-appearing children had bacteremia (S. pneumoniae), and this study was done in the pre-Prevnar era. Empirical antibiotic therapy (ceftriaxone 50 mg/kg IV or IM) should be considered in all children presenting with fever and petechiae, even if an outpatient disposition is anticipated.
Kawasaki Disease (Mucocutaneous Lymph Node Syndrome)
Kawasaki disease (KD) is one of the most common vasculitides in childhood and should be considered in any infant or child with prolonged fever.66 A more complete discussion of KD can be found in Chapter 171. Accurate diagnosis is important because the main complication of KD is the development of coronary artery aneurysms. Some patients will present with “incomplete KD,” which occurs when not all diagnostic criteria are met. Despite the lack of classic findings, these children are still at risk for coronary complications. Laboratory abnormalities found in cases of KD include leukocytosis, thrombocytosis (platelet counts as high as 1,000,000/mm3), and evidence of systemic inflammation with elevation in the erythrocyte sedimentation rate and C-reactive protein level.
Children with suspected KD should be hospitalized and receive therapy with intravenous immune globulin (2 g/kg infused during 10-12 hours) and aspirin (initial dose 80-100 mg/kg daily divided every 6 hours).67 Pediatric cardiology consultation for echocardiography is also indicated.
Toxic Shock Syndrome
Toxic shock syndrome (TSS) refers to the toxin-mediated clinical syndrome that occurs with infection with Staphylococcus aureus, although a similar illness is caused by infection with group A streptococcus. The toxin implicated in TSS is an exotoxin termed TSS toxin 1. The syndrome is classically associated with tampon use by menstruating women, although cases also occur in males and prepubertal girls and also result from other sources of infection with S. aureus.68–70
Clinical manifestations of TSS include fever (>38.9° C), hypotension, diffuse erythroderma, and multisystem involvement. Patients may present with vomiting or diarrhea, severe myalgias, oropharyngeal hyperemia, or altered mental status. Laboratory abnormalities are common and include elevated creatine kinase, elevated blood urea nitrogen or creatinine, transaminitis, and thrombocytopenia. The Centers for Disease Control and Prevention (CDC) has developed a set of findings for case definition (Box 167-1).
Fever and Underlying Chronic Medical Illness
Children with cancer, particularly those undergoing treatment with cytotoxic chemotherapy, are at particular risk for sepsis and bacterial infection.71 These life-threatening infections are most common during periods of profound neutropenia. Neutropenia is defined as an ANC of less than 500/mL or an ANC of less than 1000/mL that is falling. Children with cancer also frequently have indwelling catheters, predisposing them to surgical line infections.
Sickle Cell Disease
Febrile children with sickle cell disease are at particular risk for overwhelming infection.72 In fact, infection is the most common cause of sickle cell–related death, occurring in up to 40% of patients with sickle cell disease who die. Recurrent episodes of splenic infarction lead to functional asplenia early in life. Thus these patients are at particular risk for infection with encapsulated organisms, including S. pneumoniae and H. influenzae. Because of this risk of bacterial disease, it is recommended that all children with sickle cell disease be completely immunized. Prophylaxis with penicillin is recommended in children younger than 5 years, after which it can be safely discontinued in children who have not had a prior severe pneumococcal infection or surgical splenectomy.73 The dose of penicillin is 125 mg orally twice daily until 3 years of age (at about 14 kg) and 250 mg orally twice daily after 3 years of age.74
High-risk criteria for bacterial infection include toxic appearance, temperature higher than 40° C, abnormal WBC count (<5000 or >30,000 WBCs/mm3), and noncompliance with penicillin prophylaxis. Sickle cell patients are at particular risk for Salmonella osteomyelitis. All patients presenting with fever and sickle cell disease should have a blood specimen drawn for CBC, reticulocyte count, and culture. A reticulocyte count is important as many infections (e.g., parvovirus B19) can induce life-threatening aplastic crisis. Infection also predisposes children with sickle cell disease to acute chest syndrome.75 Common causes of infection include Chlamydia pneumoniae, Mycoplasma, RSV, S. aureus, and S. pneumoniae. Further laboratory and radiographic evaluation should be directed by the presenting history and physical examination findings.
Congenital Heart Disease
Children with congenital heart disease are at high risk for cardiovascular complications in the setting of febrile illness. Often, relatively minor viral illness can produce significant changes in cardiac function or make it difficult for children to be compliant with their oral medications. Children with congenital heart disease are also at risk for infective endocarditis. Infective endocarditis is heralded by fever and possibly a changing or worsening cardiac murmur. The modified Duke criteria for the diagnosis of endocarditis are presented in Box 167-2.76
Endocarditis is typically caused by S. aureus, viridans streptococci, Streptococcus bovis, enterococci, or infection with organisms from the HACEK group (Haemophilus species, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella species, and Kingella kingae). Children with suspected endocarditis should have blood culture specimens drawn and be admitted to the hospital for treatment and echocardiography. The American Heart Association recommends that initial antibiotic therapy be with ceftriaxone, 100 mg/kg IV or IM every 24 hours, or vancomycin, 40 mg/kg IV every 24 hours. Therapy is typically continued at least 4 weeks. Ceftriaxone can be combined with gentamicin, 3 mg/kg IV divided every 8 hours, if a shorter treatment duration (2 weeks) is desired.77 See Chapter 171 for a more complete discussion.
References
1. McCarthy, PL, et al. Fever without apparent source on clinical examination, infectious diseases, and lower respiratory infections in children. Curr Opin Pediatr. 1998;10:101.
2. Slater, M, Krug, SE. Evaluation of the infant with fever without source: An evidence based approach. Emerg Med Clin North Am. 1999;17:97.
3. Shaw, KN, et al. Prevalence of urinary tract infection in febrile young children in the emergency department. Pediatrics. 1998;102:e16.
4. Levine, DA, et al. Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections. Pediatrics. 2004;113:1728.
5. Greenes, DS, Harper, MB. Low risk of bacteremia in febrile children with recognizable viral syndromes. Pediatr Infect Dis J. 1999;18:258.
6. McGowan, JE, Jr., et al. Bacteremia in febrile children seen in a “walk-in” pediatric clinic. N Engl J Med. 1973;288:1309.
7. Anderson, AB, et al. Haemophilus influenzae type b unsuspected bacteremia. Pediatr Emerg Care. 1987;3:82.
8. Harper, MB, Fleisher, GR. Occult bacteremia in the 3-month-old to 3-year-old age group. Pediatr Ann. 1993;22:484.
9. Obonyo, CO, Lau, J. Efficacy of Haemophilus influenzae type b vaccination of children: A meta-analysis. Eur J Clin Microbiol Infect Dis. 2006;25:90.
10. Whitney, CG, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348:1737.
11. Kaplan, SL, et al. Decrease of invasive pneumococcal infections among 8 children’s hospitals in the United States after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatrics. 2004;113:443.
12. American Academy of Pediatrics. Practice parameter: The diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. Committee on Quality Improvement, Subcommittee on Urinary Tract Infection. Pediatrics. 1999;103:843.
13. Hoberman, A, Walk, ER. Urinary tract infections in young febrile infants. Pediatr Infect Dis J. 1997;16:11.
14. Bilukha, OO, et al. Prevention and control of meningococcal disease: Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2005;54:1.
15. Baker, RC, et al. Severity of disease correlated with fever reduction in febrile infants. Pediatrics. 1989;83:1016.
16. Hanna, CM, Greenes, D. How much tachycardia in infants can be attributed to fever? Ann Emerg Med. 2004;43:699.
17. Pantell, RH, et al. Management and outcomes of care of fever in early infancy. JAMA. 2004;291:1203.
18. Lee, GM, Fleisher, GR, Harper, MB. Management of febrile children in the age of the conjugate pneumococcal vaccine: A cost-effectiveness analysis. Pediatrics. 2001;108:835.
19. Kuppermann, N, Fleisher, GR, Jaffe, DM. Predictors of occult pneumococcal bacteremia in young febrile children. Ann Emerg Med. 1998;31:679.
20. Strand, CL, Wajsbort, RR, Sturmann, K. Effect of iodophor vs iodine tincture skin preparation on blood culture contamination rate. JAMA. 1993;269:1004.
21. Kaplan, RL, et al. Time to detection of positive cultures in 28- to 90-day-old febrile infants. Pediatrics. 2000;106:E74.
22. Hoberman, A, et al. Enhanced urinalysis as a screening test for urinary tract infection. Pediatrics. 1993;91:1196.
23. Nigrovic, LE, et al. Clinical prediction rule for identifying children with cerebrospinal fluid pleocytosis at very low risk of bacterial meningitis. JAMA. 2007;297:52.
24. Talan, DA, Hoffman, JR, Yoshikawa, TT, Overturf, GD. Role of empiric parenteral antibiotics prior to lumbar puncture in suspected bacterial meningitis: State of the art. Rev Infect Dis. 1988;10:365.
25. Nigrovic, LE, Kuppermann, N, Neuman, MI. Risk factors for traumatic or unsuccessful lumbar punctures in children. Ann Emerg Med. 2007;49:762.
26. Bachur, R, Perry, H, Harper, MB. Occult pneumonias: Empiric chest radiographs in febrile children with leukocytosis. Ann Emerg Med. 1999;33:166.
27. Bonner, AB, et al. Impact of the rapid diagnosis of influenza on physician decision-making and patient management in the pediatric emergency department. Pediatrics. 2003;112:363.
28. Krief, WI, et al. Influenza virus infection and the risk of serious bacterial infections in young febrile infants. Pediatrics. 2009;124:30.
29. Kanegaye, JT, Soliemanzadeh, P, Bradley, JS. Lumbar puncture in pediatric bacterial meningitis: Defining the time interval for recovery of cerebral spinal fluid pathogen after parenteral antibiotic pretreatment. Pediatrics. 2001;108:1169.
30. Kadish, HA, et al. Applying outpatient protocols in febrile infants 1-28 days of age: Can the threshold be lowered? Clin Pediatr. 2000;39:81.
31. Baker, MD, Bell, LM. Unpredictability of serious bacterial illness in febrile infants from birth to 1 month of age. Arch Pediatr Adolesc Med. 1999;153:508.
32. Bachur, R, Caputo, GL. Bacteremia and meningitis among infants with urinary tract infections. Pediatr Emerg Care. 1995;11:280.
33. Baker, MD, et al. Outpatient management without antibiotics of fever in selected infants. N Engl J Med. 1993;329:1437.
34. Baskin, MN, O’Rourke, EJ, Fleisher, GR. Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone. J Pediatr. 1992;120:22.
35. Jaskiewicz, JA, et al. Febrile infants at low risk for serious bacterial infection: An appraisal of the Rochester criteria and implications for management. Febrile Infant Collaborative Study Group. Pediatrics. 1994;94:390.
36. Baraff, LJ. Management of fever without source in infants and children. Ann Emerg Med. 2000;36:602.
37. Walsh-Kelly, C, et al. Clinical predictors of bacterial versus aseptic meningitis in childhood. Ann Emerg Med. 1992;21:910.
38. McCarthy, PL, et al. Fever without apparent source on clinical examination, infectious diseases, and lower respiratory infections in children. Curr Opin Pediatr. 1998;10:101.
39. McGowan, JE, Jr., et al. Bacteremia in febrile children seen in a “walk-in” pediatric clinic. N Engl J Med. 1973;288:1309.
40. Anderson, AB, et al. Haemophilus influenzae type b unsuspected bacteremia. Pediatr Emerg Care. 1987;3:82.
41. Harper, MB, Fleisher, GR. Occult bacteremia in the 3-month-old to 3-year-old age group. Pediatr Ann. 1993;22:484.
42. Teach, SJ, Fleisher, GR. Duration of fever and its relationship to bacteremia in febrile outpatients three to 36 months old. The Occult Bacteremia Study Group. Pediatr Emerg Care. 1997;13:317.
43. Kuppermann, N, Fleisher, GR, Jaffe, DM. Predictors of occult pneumococcal bacteremia in young febrile children. Ann Emerg Med. 1998;31:679.
44. Isaacman, DJ, et al. Predictors of bacteremia in febrile children 3 to 36 months of age. Pediatrics. 2000;106:977.
45. Jaffe, DM, et al. Antibiotic administration to treat possible occult bacteremia in febrile children. N Engl J Med. 1987;317:1175.
46. Fleisher, GR, et al. Intramuscular versus oral antibiotic therapy for the prevention of meningitis and other bacterial sequelae in young, febrile children at risk for occult bacteremia. J Pediatr. 1994;124:504.
47. Baraff, LJ, Oslund, S, Prathe, M. Effect of antibiotic therapy and etiologic microorganism on the risk of bacterial meningitis in children with occult bacteremia. Pediatrics. 1993;92:140.
48. Arditi, M, et al. Three-year multicenter surveillance of pneumococcal meningitis in children: Clinical characteristics, and outcome related to penicillin susceptibility and dexamethasone use. Pediatrics. 1998;102:1087.
49. Pikis, A, et al. Long-term sequelae of pneumococcal meningitis in children. Clin. Pediatr. 1996;35:72.
50. Nigrovic, LE, Malley, R. Evaluation of the febrile child 3 to 36 months old in the era of pneumococcal conjugate vaccine: Focus on occult bacteremia. Clin Pediatr Emerg Med. 2004;5:13.
51. Kuppermann, N. The evaluation of young febrile children for occult bacteremia: Time to reevaluate our approach. Arch Pediatr Adolesc Med. 2002;156:855.
52. Lee, GM, Fleisher, GR, Harper, MB. Management of febrile children in the age of the conjugate pneumococcal vaccine: A cost-effectiveness analysis. Pediatrics. 2001;108:835.
53. Kuppermann, N, Malley, R, Inkelis, SH, Fleisher, GR. Clinical and hematologic features do not reliably identify children with unsuspected meningococcal disease. Pediatrics. 1999;103:E20.
54. Begier, EM, et al. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin Infect Dis. 2004;39:1446.
55. Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus infections among competitive sports participants—Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000-2003. MMWR Morb Mortal Wkly Rep. 2003;52:793.
56. Lee, MC, et al. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis. 2004;23:123.
57. Kaplan, SL, et al. Multicenter surveillance of invasive meningococcal infections in children. Pediatrics. 2006;118:e979.
58. Thompson, MJ, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet. 2006;367:397.
59. Ramsay, ME, et al. Herd immunity from meningococcal serogroup C conjugate vaccination in England. BMJ. 2003;326:365.
60. American Academy of Pediatrics Subcommittee on Febrile Seizures. Febrile seizures: Guideline for the neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. 2011;127:389.
61. Sharma, S, et al. The role of emergent neuroimaging in children with new-onset afebrile seizures. Pediatrics. 2003;111:1.
62. Kimia, A, et al. Utility of lumbar puncture for first simple febrile seizure among children 6 to 18 months of age. Pediatrics. 2007;123:6.
63. Kimia, A, et al. Yield of lumbar puncture among children who present with their first complex febrile seizure. Pediatrics. 2010;126:62.
64. Baker, RC, et al. Fever and petechiae in children. Pediatrics. 1989;84:1051.
65. Mandl, KD, et al. Incidence of bacteremia in infants and children with fever and petechiae. J Pediatr. 1997;131:398.
66. Holman, RC, et al. Kawasaki syndrome hospitalizations in the United States, 1997 and 2000. Pediatrics. 2003;112:495.
67. Oates-Whitehead, RM, et al. Intravenous immunoglobulin for the treatment of Kawasaki disease in children. Cochrane Database Syst Rev. (4):2003.
68. Reingold, AL, et al. Toxic shock syndrome surveillance in the United States, 1980 to 1981. Ann Intern Med. 1982;96:875.
69. Centers for Disease Control and Prevention. Update: Toxic-shock syndrome—United States. MMWR Morb Mortal Wkly Rep. 1983;32:398.
70. Osterholm, MT, et al. Toxic shock syndrome: Relation to catamenial products, personal health and hygiene, and sexual practices. Ann Intern Med. 1982;96:954.
71. Auletta, JJ, O’Riordan, MA, Nieder, ML. Infections in children with cancer: A continued need for the comprehensive physical examination. J Pediatr Hematol Oncol. 1999;21:501.
72. Wilimas, JA, et al. A randomized study of outpatient treatment with ceftriaxone for selected febrile children with sickle cell disease. N Engl J Med. 1993;329:472.
73. Falletta, JM, et al. Discontinuing penicillin prophylaxis in children with sickle cell anemia: Prophylactic Penicillin Study II. J Pediatr. 1995;127:685.
74. Redding-Lallinger, R, Knoll, C. Sickle cell disease—pathophysiology and treatment. Curr Probl Pediatr Adolesc Health Care. 2006;36:346.
75. Vichinsky, EP, Neumayr, LD, Earles, AN, Williams, R. Causes and outcomes of the acute chest syndrome in sickle cell disease. National Acute Chest Syndrome Study Group. N Engl J Med. 2000;342:1855.
76. JS, Li, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633.
77. Baddour, LM, et al. Infective endocarditis: Diagnosis, antimicrobial therapy, and management of complications: A statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association—executive summary: Endorsed by the Infectious Diseases Society of America. Circulation. 2005;11:3167.