1
Patient Supervision and Observation During Treatment
1. Discuss the “Problem-Solving Algorithm Utilized by PTAs in Patient/Client Intervention.”
2. Identify and discuss the rationale for clear and concise communication among all members of the rehabilitation team.
3. Discuss the skills necessary to provide patient supervision.
4. Define objective scales of measurement used to communicate changes in a patient’s status to the supervising physical therapist.
5. Apply proactive listening skills and objective scales of measurement to provide appropriate, accountable, and responsible observation and supervision of the patient during treatment.
6. Define open-ended and closed-ended questioning.
7. Define the quadrants of the basic dimensional model.
8. Discuss the four categories of behavior of the physical therapist assistant: dominance, submission, hostility, and warmth.
SUPERVISING THE PATIENT DURING TREATMENT
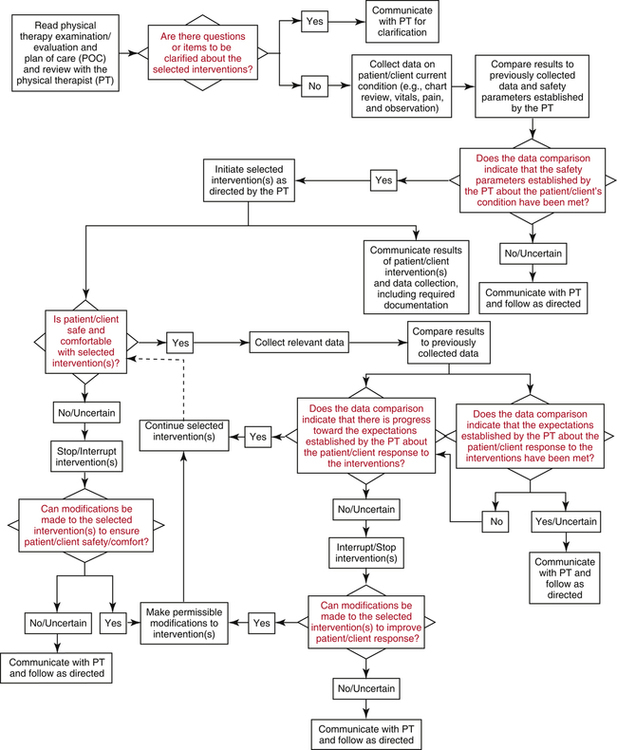
The PTA is responsible for carrying out prescribed selected interventions, patient supervision, data collection, and appropriate problem solving and clinical decision making. The American Physical Therapy Association’s Department of Education, Accreditation, and Practice developed the “Problem-Solving Algorithm Utilized by PTAs in Patient/Client Intervention,”1 which reflects current policies and positions on the problem-solving processes to be utilized by PTAs in the provision of selected interventions (Fig. 1-1). For proper care to be given, the PTA must monitor the patient’s response to selected interventions and accurately and swiftly report changes to the supervising PT. This involves constant patient interaction, observation, data collection, reassessment of initial data, problem solving, and responsive action to clarify and enhance the effectiveness of prescribed selected interventions. Changes in the patient’s status, both positive and negative, can occur throughout the treatment program, whether during a single visit or over the span of multiple treatments. Some of these changes are subtle and require keen awareness of the initial objective data and acute sensitivity to the patient’s subjective reports. Other changes are profound and sudden. In either situation, the PTA observes the patient and collects appropriate data, such as range of motion, strength, pain, balance, coordination, swelling, endurance, or gait deviations. When reported to the supervising PT, these changes dictate and can significantly affect the course of treatment.
Components of Patient Supervision
Clinical patient supervision can be viewed as a process with the following purposes:
 To gather relevant information and data
To gather relevant information and data
 To establish and enhance rapport, trust, and confidence
To establish and enhance rapport, trust, and confidence
 To facilitate understanding of the PTA’s concept of the patient’s problem as outlined, described, and initially determined by the supervising PT
To facilitate understanding of the PTA’s concept of the patient’s problem as outlined, described, and initially determined by the supervising PT
 To assist in the management of the patient
To assist in the management of the patient
 To provide a conduit or therapeutic outlet for the patient to voice concerns about his or her problem
To provide a conduit or therapeutic outlet for the patient to voice concerns about his or her problem
While providing selected interventions, the PTA makes observations of the patient, collects relevant data, and develops an objective assessment using appropriate scales of measurement (Box 1-1). Using applicable questioning techniques ensures that the patient is actively involved. This interactive approach to supervision, as well as the skills of the PTA to seek, understand, and accurately relay information related to the patient’s status distinguishes the PTA from an on-the-job trained aide.5
Patient Supervision by the Rehabilitation Team
The PTA must be aware of the key members of the rehabilitation team. The PT and PTA are involved with direct patient care on a daily basis and may be assisted by supportive personal, such as physical therapy aides or technicians. The occupational therapist and occupational therapy assistant, along with the speech language pathologist, audiologist, rehabilitation counselor, nurse, respiratory therapist, psychologist, and dietitian, play significant roles in daily patient care. These rehabilitation specialists seek to maximize recovery for each patient and always must be regarded as resources to meet specific patient needs as they are identified by any member of the team. Thus the PTA charged with direct patient care and supervision is only one vital member of the team, and he or she can take comfort in knowing that every member of the team is prepared to provide appropriate skills so that the patient can achieve the highest functional gains in recovery. Developing a team mindset helps the PTA to be responsible and accountable to the other members of the team for his or her own contribution and to reach out to others when their expertise is needed.7
Effective communication is the hallmark of a great team and should be maximized. To effectively supervise and provide the best care for the patient, the PTA must learn to communicate openly and freely, with honesty and respect, and in a professional manner with every member of the team.7 He or she must differentiate between the language used for communicating among peers and that used to define and explain injury, disease, and physical therapy interventions to a patient. The PTA must employ appropriate and professional medical terminology to outline and describe an orthopedic problem to a PT and must be able to use familiar terms to describe the same pathologic condition to a patient or family member. If the PTA uses medical jargon inappropriately, the patient or family member might perceive the PTA as insensitive, aloof, and impersonal. Generally use of language appropriate to the patient’s comprehension conveys understanding, sensitivity, warmth, and reassurance and removes uncomfortable and unnecessary barriers to communication.2
The PTA also must be aware that listening is an effective communication tool. Listening demonstrates interest and provides the opportunity for a better understanding of the patient’s concept of the problem.4 By active listening, the PTA is better able to integrate verbal and nonverbal messages that the patient may have received.4 In addition, patients may be more comfortable and trusting with a good listener and be more willing to provide information.4
Supervision of patients by the PTA must be done systematically and reliably with an emphasis on accountability and effective and efficient patient care. Appropriate and responsible investigative questioning of the patient during selected interventions helps the PTA focus on the areas to probe, findings to quantify, and objective changes to assess. As indicated in the “Problem-Solving Algorithm Utilized by PTAs in Patient/Client Intervention,”1 PTAs are responsible for reporting all findings to the supervising PT so that modifications can be made in accordance with changes in patient status.
Basic Patient Supervision Skills
Communication Skills
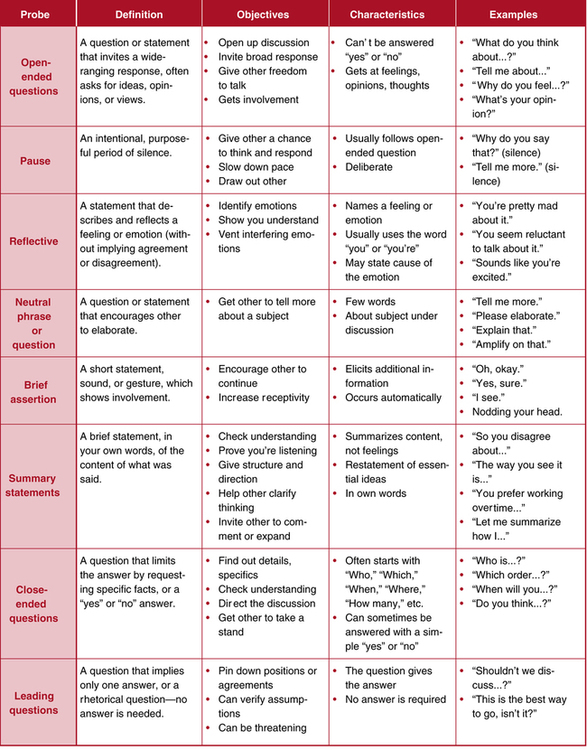
The PTA can be most effective if he or she develops an understanding of human behavior and adopts a proactive role in supervising patients. In a proactive role, the PTA does not wait to be placed in a reactive position. Use of appropriate probing questions is a proactive method to use during patient supervision. Questioning patients during treatment can be insightful, rewarding, and helpful for both the supervising PT and the PTA. The format of asking probing questions is critical and strongly influences the responses received (Fig. 1-2). Using open-ended questions invites the patient to share feelings, thoughts, concerns, and opinions.9 Examples are as follows:
These types of questions are generally not answered by “yes” or “no.” They open discussions and prompt the patient to express a wide range of views and opinions.9 Open-ended questions for patients have been described as “a good medium for facilitating rapport and, as such, are particularly useful….”4 Using open-ended questions promotes personal interactions between the PTA and patient, may allow the patient to give a more in-depth explanation of the problem, and may lead to discussions of what the patient identifies as important. Although this type of questioning does not enable the patient to give precise, clear answers, it is appropriate in situations that require compassion and empathy from the PTA and shared feelings between the PTA and patient.
Closed-ended questions are directed toward finding facts, obtaining specific responses, and filling in details. They can be very helpful in focusing and clarifying essential details of the patient’s condition.9 By asking the patient questions such as, “Where is your pain?” “When does your knee feel unstable?” or “Does your back hurt when you bend forward?” the PTA proactively directs the discussion and sequence of questions instead of sifting out pertinent information from among all the data gathered in open-ended questioning.
Behavior
The behavior of the PTA during patient supervision can either reassure the patient and demonstrate appropriate responsive professional care or create a sense of indifference. Four broad categories of behavior are dominance, submission, hostility, and warmth.2 Buzzotta and Lefton2 define these four categories as follows:
Warmth
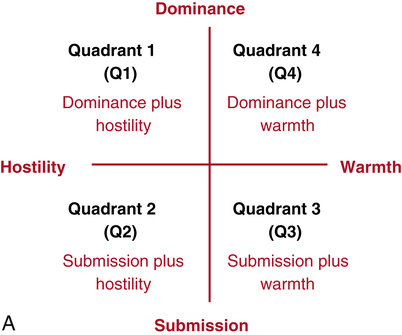
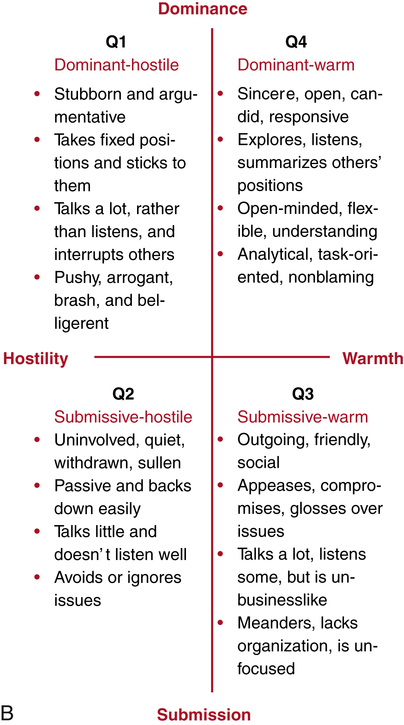
These four categories of behavior are used to describe the extremes of the basic dimensional model (Fig. 1-3, A). Quadrants (Q) are formed and certain patterns of behavior exist when two dimensions are combined, as described in the following:
Four patterns, or types, of human behavior come from this (Fig. 1-3, B).
| Dominance | Active behavior: leading, controlling, making things happen |
| Submission | Passive behavior: following, letting things happen, reacting |
| Hostility | A lack of concern or regard, and unresponsiveness for other people and their position/ideas |
| Warmth | Concern, regard, and responsiveness for other people and their position/ideas |
MODIFICATIONS DURING TREATMENT
Swelling (joint effusion) after knee surgery is common and occurs in about 13% of cases after knee ligament surgery.8 Usually the effusion is a hemarthrosis (blood within the joint, which can impair voluntary muscle contraction). In such a case the supervising PT provides baseline evaluation data about the degree of swelling present by making comparative circumferential measurements at midpatella, 2 inches superior to the midpatella, and 2 inches inferior to the midpatella. The PTA maintains daily records of the three comparative circumferential measurements. Because re-education and strengthening of muscle is influenced negatively by postoperative swelling, any increase or decrease in swelling necessitates a modification in the initial program outlined by the supervising PT. Thus the degree of swelling documented influences the adjustment made in the exercise prescription.
Isometric exercises generally are used early in the rehabilitation of acute postoperative knee injuries. Concentric and eccentric exercises are introduced as rehabilitation proceeds. Concentric and eccentric exercises are defined as dynamic, producing work, and creating changes in joint angles and muscle length.6 The progression from isometric to dynamic exercise produces an increase in force generated, increases muscle soreness, and causes greater articular stresses.3 If swelling and pain increase as the patient progresses from isometric to concentric and eccentric contractions, the PTA, with direction and input from the supervising PT, can adjust or modify the program back to isometrics or reduce the amount of resistance, joint angle of exercise, volume of exercise, or velocity of movement. The specific sequence or combination of these modifications depends on the patient’s specific needs, the surgical procedure, and the patient’s tolerance to exercise. Usually it is prudent to begin with the least drastic change in exercise prescription and then progress (Box 1-2).
UNDERSTANDING DIFFERENT PHILOSOPHIES OF PHYSICAL THERAPISTS
GLOSSARY
Dominance Exercising control or influence; being assertive; and putting one’s idea forward.
Hostility Defined as self-centered, unresponsive, and insensitive.
Responsibility A component of active involvement of all areas of patient care.
Submission Defined as following the lead of others, being passive and quick to comply.