CHAPTER 13 Patent Ductus Arteriosus
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations
 Congestive heart failure in the premature infant population is the most common indication for surgical ductal closure. Whereas echocardiography may demonstrate the presence and approximate size of the patent ductus, the decision to intervene should be based on clinical symptoms of congestive heart failure (respiratory compromise caused by excessive pulmonary blood flow, failure to maintain consistent weight gain, compromise of systemic perfusion manifested as renal insufficiency, or necrotizing enterocolitis). Echocardiographic evidence of significant pulmonary volume overload, such as left atrial and left ventricular enlargement, and a chest radiograph showing cardiac enlargement and prominent pulmonary vasculature support the clinical findings.
Congestive heart failure in the premature infant population is the most common indication for surgical ductal closure. Whereas echocardiography may demonstrate the presence and approximate size of the patent ductus, the decision to intervene should be based on clinical symptoms of congestive heart failure (respiratory compromise caused by excessive pulmonary blood flow, failure to maintain consistent weight gain, compromise of systemic perfusion manifested as renal insufficiency, or necrotizing enterocolitis). Echocardiographic evidence of significant pulmonary volume overload, such as left atrial and left ventricular enlargement, and a chest radiograph showing cardiac enlargement and prominent pulmonary vasculature support the clinical findings. In older children a medium-sized to large patent ductus may lead to chronic congestive heart failure symptoms, the risk of developing pulmonary hypertension, and ultimately Eisenmenger physiology. In the current era, the incidence of bacterial endarteritis is extremely low, although bacterial endarteritis was responsible for a large portion of the mortality from patent ductus arteriosus (PDA) in the pre-antibiotic era.
In older children a medium-sized to large patent ductus may lead to chronic congestive heart failure symptoms, the risk of developing pulmonary hypertension, and ultimately Eisenmenger physiology. In the current era, the incidence of bacterial endarteritis is extremely low, although bacterial endarteritis was responsible for a large portion of the mortality from patent ductus arteriosus (PDA) in the pre-antibiotic era. Because ductal patency is related to prostaglandin metabolism, medical closure is possible using the prostaglandin synthetase inhibitors indomethacin or other nonsteroidal anti-inflammatory drugs (NSAIDs). Only premature infants in the first week or two of life predictably respond to NSAID therapy, although the use of NSAIDs may be contraindicated because of renal insufficiency or concern about bleeding complications.
Because ductal patency is related to prostaglandin metabolism, medical closure is possible using the prostaglandin synthetase inhibitors indomethacin or other nonsteroidal anti-inflammatory drugs (NSAIDs). Only premature infants in the first week or two of life predictably respond to NSAID therapy, although the use of NSAIDs may be contraindicated because of renal insufficiency or concern about bleeding complications. Catheter-based therapy using Gianturco coils or the Amplatzer ductal occluder device has become the standard therapy, with few exceptions, for PDA in children beyond the newborn period.
Catheter-based therapy using Gianturco coils or the Amplatzer ductal occluder device has become the standard therapy, with few exceptions, for PDA in children beyond the newborn period.Step 3: Operative Steps
 Division of the ductus between vascular clamps with oversewing of the ends is the only method that can confidently be predicted to result in a 100% closure rate, but this technique is appropriate only for larger children with relatively longer ductal lengths.
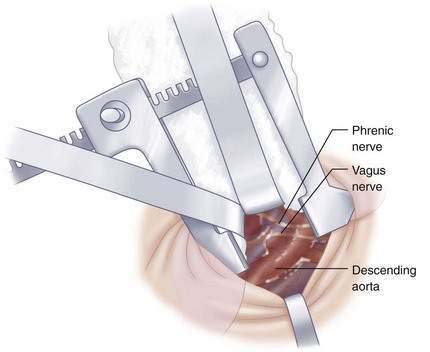
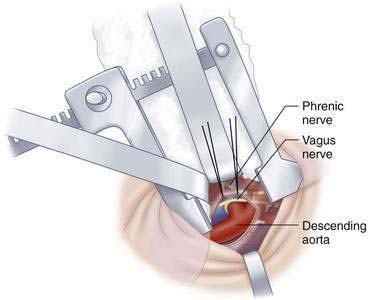
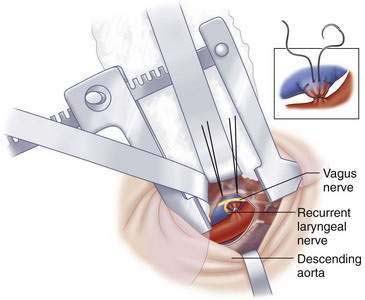
Division of the ductus between vascular clamps with oversewing of the ends is the only method that can confidently be predicted to result in a 100% closure rate, but this technique is appropriate only for larger children with relatively longer ductal lengths. Closure by Ligaclip may be used with open or thoracoscopic techniques. It is the simplest and most appropriate method in the premature infant. It is important to recognize that clips close first at their tips and then in the middle. It is essential to be able to dissect enough of the ductus to see that the tip does not close on the ductal wall itself and perforate it; rather, it must come together beyond the ductal wall. This may result in the need to use a larger clip size than expected from the initial exposure. Positioning the legs of the clip applier along the superior and inferior aspect of the ductus and then pushing the applier against the descending aorta while lifting the latter structure posteriorly and upward will allow good visualization of clip closure and also will minimize the risk of injury to the recurrent laryngeal nerve, which will tend to stay near the pulmonary end of the ductus.
Closure by Ligaclip may be used with open or thoracoscopic techniques. It is the simplest and most appropriate method in the premature infant. It is important to recognize that clips close first at their tips and then in the middle. It is essential to be able to dissect enough of the ductus to see that the tip does not close on the ductal wall itself and perforate it; rather, it must come together beyond the ductal wall. This may result in the need to use a larger clip size than expected from the initial exposure. Positioning the legs of the clip applier along the superior and inferior aspect of the ductus and then pushing the applier against the descending aorta while lifting the latter structure posteriorly and upward will allow good visualization of clip closure and also will minimize the risk of injury to the recurrent laryngeal nerve, which will tend to stay near the pulmonary end of the ductus. Simple ligation of a large ductus in a premature infant may be more difficult because of the need to perform circumferential dissection and the inability to feel when the suture is tied down securely without tearing through the fragile ductal wall, potentially resulting in a higher rate of incomplete closure.
Simple ligation of a large ductus in a premature infant may be more difficult because of the need to perform circumferential dissection and the inability to feel when the suture is tied down securely without tearing through the fragile ductal wall, potentially resulting in a higher rate of incomplete closure.Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Gould DS, Montenegro LM, Gaynor JW, et al. A comparison of on-site and off-site patent ductus arteriosus ligation in premature infants. Pediatrics. 2003;112(6 Pt 1):1298-1301.
Hillman ND, Mavroudis C, Backer CL. Patent ductus arteriosus. In: Mavroudis C, Backer CL, editors. Pediatric cardiac surgery. 3rd ed. Philadelphia: Mosby; 2003:223-233.
Jacobs JP, Giroud JM, Quintessenza JA, et al. The modern approach to patent ductus arteriosus treatment: complementary roles of video-assisted thoracoscopic surgery and interventional cardiology coil occlusion. Ann Thorac Surg. 2003;76(5):1421-1427.
Moin F, Kennedy KA, Moya FR. Risk factors predicting vasopressor use after patent ductus arteriosus ligation. Am J Perinatol. 2003;20(6):313-320.
Rao PS. Percutaneous closure of patent ductus arteriosus: state of the art. J Invasive Cardiol. 2007;19(7):299-330.
Raval MV, Laughon MM, Bose CL, Phillips JD. Patent ductus arteriosus ligation in premature infants: who really benefits, and at what cost? J Pediatr Surg. 2007;42(1):69-75.
Schneider DJ, Moore JW. Patent ductus arteriosus. Circulation. 2006;114(17):1873-1882.
Zbar RI, Chen AH, Behrendt DM, et al. Incidence of vocal fold paralysis in infants undergoing ligation of patent ductus arteriosus. Ann Thorac Surg. 1996;61(3):814-816.