Chapter 23 Partial Stapedectomy
HISTORY
In 1958, Shea1 advocated total stapes footplate removal when using the polyethylene strut prosthesis and a vein graft to seal the oval window. Shortly thereafter, Schuknecht2 advocated the use of a wire and fat prosthesis, and House and Greenfield3 later advocated the use of a wire with absorbable gelatin sponge (Gelfoam) prosthesis. The use of the wire/Gelfoam or wire/fat prosthesis necessitated total removal of the footplate for the wire prosthesis to function satisfactorily. Other methods that could be considered a partial stapedectomy technique included the shattered footplate procedure with the use of a polyethylene strut, and the subluxated footplate procedure, both of which necessitated removal of the superstructure of the stapes.4 These two techniques were quickly rejected because of the associated sensorineural hearing loss resulting from either surgical trauma or a perilymphatic fistula.
In 1961, the piston concept was introduced, in which a cup/piston prosthesis was used with a connective tissue graft of vein to seal the oval window.5 The introduction of the piston prosthesis no longer required a total removal of the stapes footplate. The concept evolved of “removing only that part of the footplate which comes out easily.”6 This newly introduced surgical technique consequently produced more successful hearing results and fewer inner ear complications. The same technique could be used for the thin blue footplate with minimal otosclerotic involvement, or for the obliterative footplate, in which only a stapedotomy opening (“drill-out”) could be created. Measurement of the distance between the long process of the incus and stapes footplate was eliminated because a 4-mm prosthesis would protrude into the vestibule 0.2 to 0.3 mm in virtually every case. This slight protrusion would create its self-centering effect. By interposing a vein graft between the prosthesis and vestibule, there was rarely a regrowth of otosclerotic bone, including the obliterative type. Also, because of this protrusion, migration of the piston in subsequent years was virtually unknown.
The 4 mm length is used in virtually every stapedectomy case whether it is a drill-out stapedotomy, a partial footplate removal, or a total footplate removal. Any connective tissue can be used with this prosthesis, but I prefer a vein graft that outlines the oval window opening and ensures a complete immediate seal of the oval window. Moon7 advocates the cup/piston prosthesis with areolar tissue. The cup/piston prosthesis is radiopaque and easy to localize and identify on routine mastoid radiographic views. Comparison of impedance studies of various stapes prostheses has shown the stainless steel cup/piston to be the closest in compliance to that of a normal mobile stapes.8 Hearing results reported by otologic surgeons who have used this technique have consistently confirmed a 96% air-bone gap closure to within 10 dB.9–11 Similarly, the complete closure (and overclosure) rate has been repeatedly confirmed at 80%, which the wire/tissue prosthesis and wire pistons have yet to attain.
Because the stapes does not increase in size with age, the 4 mm cup/piston prosthesis has been used in children 5 years old, adults, and elderly individuals. All patients who show an air-bone gap and normal results on otologic examination are candidates for stapedectomy surgery if stapedial fixation is found at the time of the middle ear exploration. Approximately 22% of patients with otosclerosis have a diminished cochlear reserve with a Shambaugh preoperative bone conduction classification of D or E. These patients have very severe mixed hearing losses, and in many, only a partial footplate removal can be obtained. These patients also most frequently show complete closure and overclosure of the air-bone gap. For these patients, the extra 10 dB of hearing gain is crucial because of their mixed hearing loss. Approximately 74% of the patients undergoing surgery have partial or total footplate removal that does not necessitate drilling. The remaining 26% require drilling to create a fenestra 0.8 mm in diameter or larger to accept the vein graft and cup/piston prosthesis.6
In 1980, Austin12 compared the results of total stapedectomy and partial stapedectomy, tissue seal and no tissue seal, and the small fenestra of Smyth. His statistical analysis, using chi-square tables for success or failure, sensorineural hearing loss, fistula, and complete air-bone gap closure, was computed. He concluded that a tissue seal provides a better success rate, a significantly lower risk of fistula, and a better hearing result in terms of complete closure or overclosure of the air-bone gap. Austin noted that in addition to the increased risk of sensorineural complications and fistulas, the small-diameter pistons used in stapedotomies did not provide as good a hearing result.
SURGICAL TECHNIQUE
Stapedectomy footplate surgery follows a very basic principle—be as atraumatic as possible in removing the footplate of the stapes. This principle is contingent on removal of “only that part of the footplate which comes out easily.”6
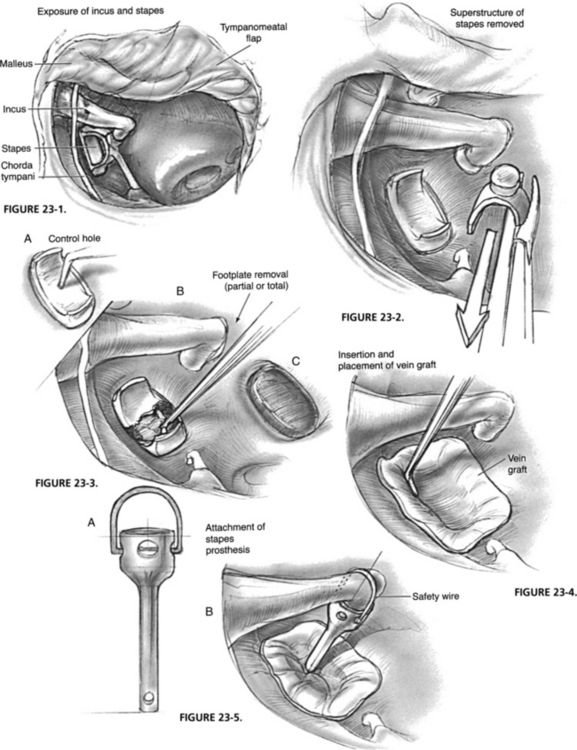
Routine stapedectomy is divided into three stages: (1) exposure of the middle ear, incus, stapes, and footplate area; (2) removal of the stapes superstructure; and (3) removal of the stapes footplate. If the opening is 0.8 mm or larger, the piston can function satisfactorily. The new fenestra must be sealed with a tissue graft; a self-centering 4 mm cup/piston bridges the gap from the oval window membrane to the incus (Figs. 23-1 to 23-5).
Footplate surgery can be classified as follows:
This prosthesis, because of its unique design, is a “smart” prosthesis—it can be fitted to the incus under many circumstances. It can fit an angled lenticular process; an extra-large lenticular process; an extra-long long process; a short long process; or a fractured, atrophic, or necrotic long process. When a narrow oval window niche or a prolapsed facial nerve is present, the prosthesis easily self-centers into the vein graft. When there is only partial footplate removal or drill-out for obliterative otosclerosis, the vein graft and prosthesis align perfectly because of the self-centering feature.9
POSTOPERATIVE RESULTS
Delayed hearing losses have been infrequent. In a 21-year period, the incidence of delayed conductive losses was 1.6%, and incidence of cochlear losses of more than 10 dB was 1.2%. The total continued long-term success rate is 93%. These data were derived from a 20-year study of 4815 stapedectomy cases.13 The causes of a delayed conductive loss and their incidence are as follows: otosclerotic regrowth, 3/1000; tympanofibrosis, 2/1000; malleus fixation, 1/1000; postoperative tympanic membrane perforation, 1/1000; incus necrosis, 1/1000; prosthesis migration, 1/3000; prosthesis extrusion (preoperatively healed perforation), 3/1000; and perilymphatic fistula (first vein graft too small), 1/1000. Delayed cochlear losses resulted primarily from perilymphatic fistula (vein graft too small), 1/2000; cochlear otosclerosis, 1/1000; presbycusis, 4/1000; and viral labyrinthitis, 2/1000.
DISCUSSION
Comparison with Wire/Stapes Prosthesis
Results with wire prostheses vary greatly; success rates range from 80% to 95%. With wire/piston stapedotomy procedures, there frequently is a residual, small air-bone gap in the low frequencies. Reports of complete closure are sparse, but the complete closure rate of the wire/fat prosthesis has been reported to be 15% to 20%, and the complete closure rate of the wire/piston stapedotomy procedure has been reported to be 50% or less. The cup/piston complete closure rate has consistently been 80%, however. Impedance studies have shown that wires have a very high compliance, whereas cup/piston prostheses have a compliance similar to that of a normal mobile stapes. This high compliance of wire prostheses reflects the imperfect attachment to the incus because the wire is crimped over the long process and eventually loosens slightly when notching of the incus occurs. Notching and loosening do not occur with the cup/piston prostheses.8
Stainless Steel Prostheses versus Polytef (Teflon) Prostheses
Many materials have been used and advocated for the fabrication of stapes prostheses. Polytef (Teflon) has many advocates because of its inertness and lack of tissue reaction. The stainless steel cup/piston prosthesis, which is fabricated of 316L stainless steel, has also shown a lack of tissue reaction. The main difference between both materials is the weight. A Teflon cup/piston prosthesis weighs 3.3 mg, and a stainless steel cup/piston prosthesis weighs 12.5 mg. An intact stapes freshly removed from the ear weighs 6 mg. Bluestone14 first reported that by loading a polyethylene stapes prosthesis with a steel core, he would obtain a 10 dB increase in hearing at 4000 Hz and 8000 Hz compared with that of the control group.
I reported a study comparing the hearing results in patients with a Robinson stainless-steel cup/piston prosthesis and vein graft in the first ear and a Robinson Teflon cup/piston prosthesis and vein graft in the second ear.15 This study eliminated all variables except the difference in weight of the prostheses. The preoperative hearing level in each ear was the same, as was the footplate pathology in both ears. The design of the prosthesis was exactly the same; only the weight differed. The stainless steel prosthesis weighed almost four times that of the Teflon prosthesis. The results showed that the high-frequency gains in hearing were slightly better for the stainless steel ear (14 dB) than for the Teflon ear (11 dB). The rate of complete closure and overclosure of the air-bone gap was significantly greater in the stainless steel ear (80%) than in the Teflon ear (52%), even though the overall closure of the air-bone gap to within 10 dB was 97% in the stainless steel ear and 96% in the Teflon ear. Impedance studies of this group showed that the compliance of the stainless steel stapes prosthesis most resembled that of the normal mobile stapes, whereas the Teflon prosthesis showed a slightly reduced compliance (high impedance), but as a cup/piston, its compliance curves were more within the range of the mobile stapes than any of the wire prostheses.
This study proved that the heavier prosthesis resulted in a much greater complete closure and overclosure of the air-bone gap, and that there was a small but significant hearing advantage in postoperative results when a metallic prosthesis was used (6 dB). In mixed-type hearing loss, this increased hearing can have a significant effect on the patient’s reaching a serviceable postoperative hearing level.15
Juvenile Otosclerosis
Otosclerosis is usually considered to be a disease of young and middle-aged adults, but juvenile otosclerosis occurs in 15.1% of stapedectomy cases before age 18. I presented an in-depth study of 610 patients (of a total of 4014 patients) who developed clinical otosclerosis before age 18 and underwent stapedectomy.16 Of these 610 patients, 35 underwent surgery before age 18, and 574 underwent surgery after age 18, but their hearing loss had developed during their juvenile years. The youngest patient was 5 years old, and the average age of onset was 11.5 years.
This study also revealed a very high incidence of bilateral otosclerosis (92%) when the hearing loss occurred before age 18. Of patients younger than 18 with otosclerosis, 80% had excellent cochlear reserve and did not show a deterioration of sensorineural function after stapedectomy. The longer the hearing loss existed, the greater the degree of footplate pathology that occurred. The probability of requiring a drill-out for obliterative otosclerosis increased fourfold when surgery was deferred to after age 18. Deferring a stapedectomy procedure in a child may not be in the best interest of the patient because of the progressive nature of the footplate pathology and the increased necessity of drilling the footplate.16
1. Shea J.J.Jr. Fenestration of the oval window. Ann Otol Rhinol Laryngol. 1958;57:932.
2. Schuknecht H. Stapedectomy and graft prosthesis operation. Acta Otolaryngol (Stockh). 1960;51:241-243.
3. House H.P., Greenfield E.C. Five-year study of wire-loop absorbable gelatin sponge technique. Arch Otolaryngol Head Neck Surg. 1969;89:420-421.
4. Goodhill V. Stapes Surgery for Otosclerosis. St Louis: Paul B Hoeber; 1961. p 136
5. Robinson M. The stainless-steel stapedial prosthesis: One year’s experience. Laryngoscope. 1962;73:514.
6. Robinson M. A four-year study of the stainless-steel stapes. Arch Otolaryngol Head Neck Surg. 1965;82:217-235.
7. Moon C. Stapedectomy connective tissue graft and the stainless-steel prosthesis. Laryngoscope. 1968;78:798-807.
8. Feldman A. Acoustic impedance measurement of post-stapedectomized ears. Laryngoscope. 1969;79:1132-1155.
9. Schondorf J., Pilorget J., Graber S. [The influence of the stapes prosthesis on the long-term results of stapedectomy.]. Head Neck Otolaryngol. 1980;28:153-157.
10. Elonka D., Derlacki E., Harrison W. Stapes prosthesis comparison. Otolaryngol Head Neck Surg. 1982;90:263-265.
11. Girgis T: Stapedectomy: Robinson stapes prosthesis versus wire prosthesis. Presented at American Society of Otology, Rhinology, and Laryngology, Middle Section Meeting, Chicago, January 1985.
12. Austin D.F. Stapedectomy with tissue seal. In: Snow J.B.Jr., editor. Controversy in Otolaryngology. Philadelphia: Saunders, 1980.
13. Robinson M. Total footplate extraction in stapedectomy. Ann Otol Rhinol Laryngol. 1981;90:630-632.
14. Bluestone C.D. Polyethylene stainless-steel core in middle ear surgery. Arch Otolaryngol Head Neck Surg. 1962;76:303.
15. Robinson M. Stapes prosthesis: Stainless steel versus Teflon. Laryngoscope. 1974;84:1982-1995.
16. Robinson M. Juvenile otosclerosis. Ann Otol Rhinol Laryngol. 1983;92:561-565.