Parkinson’s disease
Definition
Parkinson’s disease (PD) is a progressive neurological condition, resulting from the degeneration of dopamine-producing neurons located in the substantia nigra, part of the basal ganglia (S2.11).
Epidemiology
Aetiology
Outcome and prognosis
The dopaminergic neurons of the SN project to the striatum and normally modulate the activity of both the direct and indirect pathways within the basal ganglia (S2.11), having the opposite effect on each. The direct pathway facilitates the initiation and selection of the correct voluntary movement programmes to achieve a task, while the indirect pathway helps to prevent any unwanted movement programmes. In PD, the loss of dopaminergic cells in the SN means that the ability to modulate motor programme selection is lost and there is inappropriate competition between the correct and incorrect movement programmes being sent to the cortex. Consequently, a hypokinetic movement disorder presents, or in simple terms a lack of movement. As dopamine has a modulatory role (increasing or decreasing movement), a presentation of alternating background tone may also be observed (e.g. resting tremor). Also of relevance is the increased time in initiation of the long latency reflexes, which may reflect the problem with initiation of voluntary movement in PD. There are also dopamine-producing cells in three other non-motor pathways and a deficit here is thought to explain much of the neuropsychiatric pathology associated with PD. PD is both a chronic and progressive disease and although it is not considered to be fatal, the average life expectancy is generally lower than that of a healthy population.
Signs and symptoms
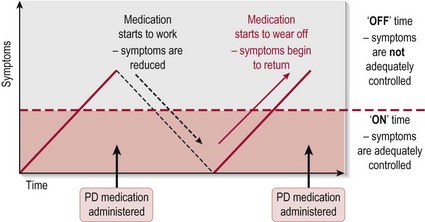
The clinical signs of PD become evident only when about 80% of the dopamine-producing neurons are lost and may fluctuate throughout the day as a consequence of medication. When symptoms are well controlled this is termed ‘on’ time and when not sufficiently controlled, ‘off’ time (Fig. 3.1).
The signs and symptoms presented will be a combination of:
Motor
The main characteristics of the disease are often represented by the mnemonic TRAP.
• Tremor (S3.18): In the majority of patients the tremor appears when at rest and is decreased with voluntary movement. It is often referred to as pill-rolling because of its action
• Rigidity (S3.19, 21): Apart from affecting voluntary movement, the muscle rigidity may also limit the individual’s ability to express themselves facially (masked face) or verbally (hypophonia). The lack of facial expression and weak voice often gives the wrong impression about the patient’s mental state and they should be given extra time to consider and act on information given, by all concerned
• Akinesia/bradykinesia (S3.18): The patient becomes slower in all movements (bradykinesia) and gradually voluntary movements show a decremental loss of amplitude, and akinesia (no movement) presents. Freezing during gait is a manifestation of akinesia and often exacerbated when trying to pass through a doorway or cluttered space
• Postural instability (S3.32): A failure of postural reflexes results in impaired balance and may lead to falls.
Sensory
• Pain (S3.29): Pain is common and can occur in up to 50% of people with PD. Patients may complain of sensory-type pains, which include paraesthesias, burning dysesthesias, coldness, numbness and deep aching within a nerve (neuropathic pain). It can also be a result of musculoskeletal pain, secondary to rigidity and hypokinesia
Cognitive
• Depression (S3.16): This occurs in 45% of people with PD and is related to the degeneration of dopaminergic neurons in limbic and pre-frontal systems.
Other
• Sleep disturbances (S3.16): The causes are multifactorial but degeneration of the sleep regulation centres in the brain stem and thalamocortical pathway is implicated
• Autonomic disturbance (S3.16): Autonomic dysfunction is common in PD due to the underlying pathophysiology of the condition affecting the catecholaminergic neurons of the autonomic nervous system. Symptoms include: urinary dysfunction (40%); constipation (50%); orthostatic hypotension (a fall in systolic blood pressure of over 20 mmHg on standing) (48%); weight loss (50%) and dysphagia
• Dystonia: Abnormal, sustained, painful twisting muscle contractions are experienced by 20% of patients with PD
Secondary complications
• Psychosocial (S3.16): Anxiety, apathy, psychosis and visual hallucinations, dementia. Change in role and financial difficulty
• Change in postural alignment (S3.20)
• Decreased muscle strength (S3.30)
• Altered gait (S3.19): Shuffling gait – characterized by short steps, with feet barely leaving the ground. Festinating gait – the presentation of a stooped posture, altered balance and shuffling steps results in a gait that gets progressively faster and faster, ultimately becoming unsafe
• Decreased range of movement (S3.28)
• Falls (S3.34): In the UK, two-thirds of people with PD fall at least once each year and many of them are at risk of falling again.
References and Further Reading
Ascherio, A, Chen, H, Weisskopf, M, et al. Pesticide exposure and risk for Parkinson’s disease. Annals of Neurology. 2006; 60:197–203.
Barbeau, A. Manganese and extrapyramidal disorders (a critical review and tribute to Dr George C. Cotzias). Neurotoxicology. 1984; 5:13–35.
Bower, JH, Maraganore, DM, Peterson, BJ, et al. Head trauma preceding PD: a case–control study. Neurology. 2003; 60:1610–1615.
Chiueh, CC, Andoh, T, Lai, AR, et al. Neuroprotective strategies in Parkinson’s disease: protection against progressive nigral damage induced by free radicals. Neurotoxicity Research. 2000; 2:293–310.
Di Monte, DA, Lavasani, M, Manning-Bog, AB. Environmental factors in Parkinson’s disease. Neurotoxicology. 2002; 23:487–502.
Elbaz, A, Moisan, F. Update in the epidemiology of Parkinson’s disease. Current Opinion in Neurology. 2008; 24:454–460.
Goldman, SM, Tanner, CM, Oakes, D, et al. Head injury and Parkinson’s disease risk in twins. Annals of Neurology. 2006; 60:65–72.
Hoehn, M, Yahr, M. Parkinsonism: onset, progression and mortality. Neurology. 1967; 17:427–442.
Jenner, P. Oxidative mechanisms in nigral cell death in Parkinson’s disease. Movement Disorders. 1998; 13:24–34.
Lepoutre, A, Devos, D, Blanchard-Dauphin, A, et al. A specific clinical pattern of camptocormia in Parkinson’s disease. Journal of Neurology, Neurosurgery and Psychiatry. 2006; 77:1229–1234.
Lieberman, A. Depression in Parkinson’s disease: a review. Acta Orthopaedica Scandinavica. 2006; 113:1–8.
Lindquist, SL, Bonini, NM. Parkinson’s disease mechanism discovered. www.sciencemag.org, 2006.
Nambu, A. A new dynamic model of the cortico-basal ganglia loop. Progress in Brain Research. 2004; 43:461–466.
National Institute for Health and Clinical Excellence. Parkinson’s disease: diagnosis and management in primary and secondary care (Clinical guideline 35). www.nice.org.uk/CG035, 2006.
National Institute for Health and Clinical Excellence. The assessment and prevention of falls in older people (Clinical guideline 21). www.nice.org.uk/CG021, 2004.
National Service Framework for Long-term (Neurological) Conditions. www.dh.gov.uk/longtermconditions.
The Parkinson’s Disease Society. The professional’s guide to Parkinson’s disease. www.parkinsons.org.uk/PDF/PubProfessionalGuideNov07.pdf, 2007.
Willems, A. Rescue Consortium Katholieke Universiteit Leuven. Belgium, Available from www.rescueproject.org, 2005.
Xia, R, Sun, S, Threlkeld, J. Analysis of interactive effect of stretch reflex and shortening reaction on rigidity in Parkinson’s disease. Clinical Neurophysiology. 2009; 120:1400–1407.