Chapter 7 Papulosquamous skin eruptions
Habif TP: Clinical dermatology: a color guide to diagnosis and therapy, ed 4, St Louis, 2004, Mosby.
| Morphologic variants | Locational variants |
|---|---|
| Chronic plaque psoriasis | Scalp psoriasis |
| Guttate psoriasis | Palmoplantar psoriasis |
| Pustular psoriasis | Inverse psoriasis |
| Erythrodermic psoriasis | Nail psoriasis |
| Psoriatic arthritis |

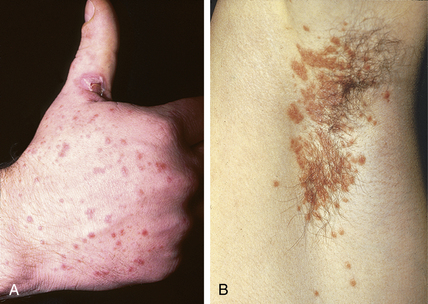
Figure 7-3. Distal psoriatic arthritis in an 11-year-old patient. Note the extensive nail changes.
(Courtesy of the William L. Weston, M.D. collection.)
Coal tar preparations can also be effective, especially if used with topical corticosteroids. Anthralin, a synthetic derivative of chrysarobin, a tree bark extract, is effective in daily, short applications for chronic plaque psoriasis, but its irritant qualities often worsen inflammatory psoriasis. Calcipotriene (Dovonex), a vitamin D3 analog, is an effective treatment for localized psoriasis, but its cost and the possibility of systemic absorption resulting in changes in calcium homeostasis preclude its use in extensive disease. Calcipotriene should be limited to a maximum dosage of 100 gm/wk. A newer and potentially more effective treatment is the combination of calcipotriene and the corticosteroid, betamethasone diproprionate (Taclonex).
Key Points: Papulosquamous Disorders
Naldi L, Rebora A: Clinical practice. Seborrheic dermatitis, N Engl J Med 360:387–396, 2009.