Chapter 19 Panniculitis
Table 19-1. Major Forms of Panniculitis
| Septal Panniculitis
Lobular and Mixed Panniculitis Metabolic Derangements |
Infectious Panniculitis
Malignancy
Other Changes of the Fat
Lipodystrophy
Lipoatrophy
Lipohypertrophy
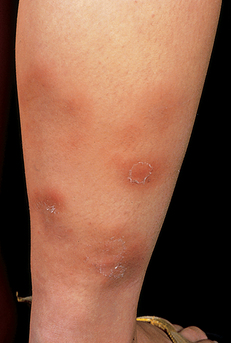
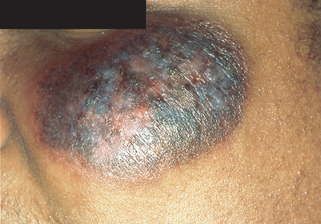
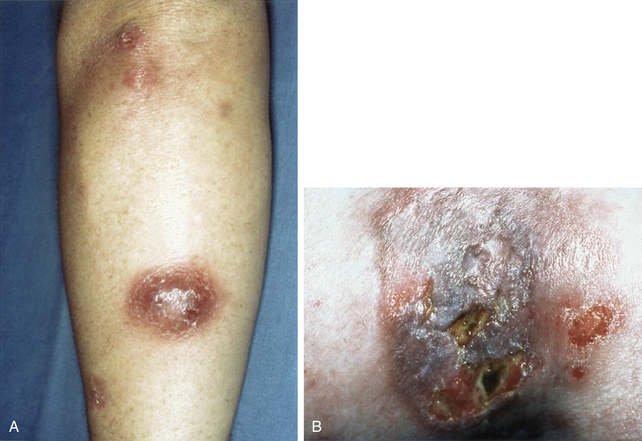
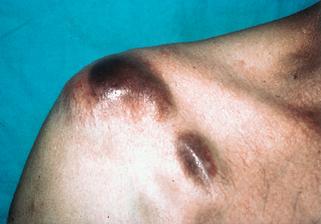
Figure 19-3. Erythema induratum demonstrating characteristic indurated subcutaneous nodules. Spontaneous ulceration is common.
(Courtesy of James E. Fitzpatrick, MD.)
Key Points: Panniculitis
Key Points: Erythema Nodosum
Key Points: Lupus Panniculitis
Mascaró JM Jr, Baselga E: Erythema induratum of Bazin, Dermatol Clin 26:439–445, 2008.

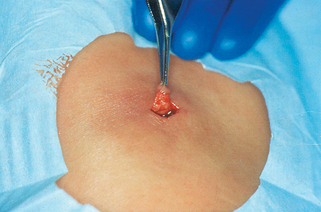
Figure 19-7. Alpha-1 antitrypsin deficiency panniculitis showing foci of hemorrhage in the center of the lesion.
(Courtesy of Kenneth E. Greer, MD.)
Chowdhury MM, Williams EJ, Morris JS, et al: Severe panniculitis caused by ZZ alpha-1-antitrypsin deficiency treated successfully with human purified enzyme (Prolastin), Br J Dermatol 147:1258–1261, 2004.
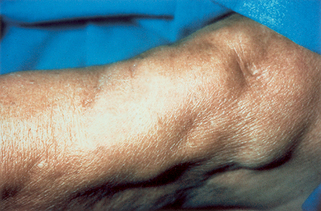
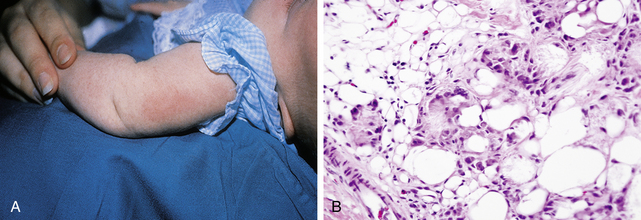
Figure 19-8. Sclerosing panniculitis with lipoatrophy caused by repeated injection of pentazocine.
(Courtesy of Kenneth E. Greer, MD.)