CHAPTER 12 Pancreaticojejunostomy (puestow procedure)
Step 1. Surgical anatomy
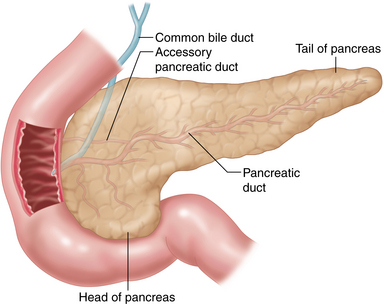
♦ The exocrine pancreas is drained via a main and an accessory duct (Figure 12-1).
♦ The main pancreatic duct is often affected in chronic pancreatitis. Preoperative ERCP (Endoscopic Retrograde Cholangiopancreatography) is effective in demonstrating ductal dilatation and the presence of stones (Figure 12-2).
Step 2. Preoperative considerations
Patient preparation
♦ To be considered for this procedure, patients must have failed conservative medical therapy and be managed by a multidisciplinary team, including primary care and gastroenterology.
♦ Patients should undergo appropriate pre-operative imaging, including a high-resolution computed tomography (CT) and ERCP, or Magnetic Resonance Cholangiopancreatography (MRCP) (Figure 12-2).
♦ It is critical to assess pancreatic duct dilatation and ductal strictures, and to rule out the presence of a potentially malignant mass.
♦ The pancreatic duct should be dilated to greater than 7 mm in diameter.
♦ Preoperative placement of a pancreatic stent for temporary pain relief may be appropriate. This is not a contraindication to surgery.
♦ Many patients will have nutritional deficiencies and diabetes. Appropriate treatment should be initiated for these comorbidities before these patients undergo surgery.
♦ Informed consent should be obtained. It is important to set expectations appropriately. The patients should not expect cure, but a 70% to 80% improvement in pain.
Room setup and patient positioning
♦ The patient is placed in split-leg position, and foot plates are used to prevent sliding.
♦ Monitors are placed above the patient’s head.
♦ The operative surgeon usually stands on the patient’s right side with the assistant at the patient’s left side. The surgeon may find it helpful to move to the position between the legs during certain parts of the procedure (e.g., dissection of the pancreas medially).
Step 3. Operative steps
Access and port placement
♦ A Veress needle is introduced along the left subcostal margin, in the midclavicular line, and a pneumoperitoneum is created to a pressure of 15 mmHg using carbon dioxide.
♦ A 12-mm camera port is placed 3 cm to the left of midline and approximately 8 cm above the umbilicus. A 10-mm, 30-degree laparoscope is then introduced into the peritoneal space.
♦ Under direct vision, a 12-mm working port is placed 4 cm to the right of the midline and 6 to 8 cm above the umbilicus. A 5-mm working port is placed in the right upper quadrant. An assistant 5-mm port is placed in the left upper quadrant.
♦ A 5-mm incision is made in the subxiphoid space, and the Nathanson retractor is introduced to elevate the left lobe of the liver.
Exposing the lesser sac
♦ Using the Harmonic scalpel, the gastrocolic ligament is divided below the gastroepiploic vessels and the lesser sac is entered.
♦ The greater curve is mobilized from the pylorus to the fundus to provide adequate exposure of the lesser sac and the pancreas. There are often inflammatory attachments between the posterior gastric wall and the pancreas, which need to be divided.
♦ The Nathanson retractor is then gently repositioned to elevate the stomach and maintain exposure of the lesser sac.
Identification of the pancreas and pancreatic duct
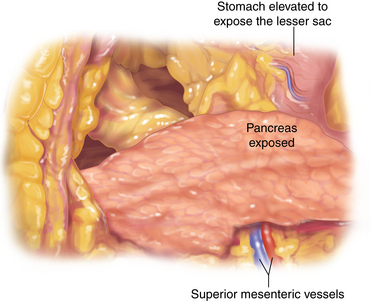
♦ The peritoneum along the superior and inferior border of the pancreas is divided and the pancreas clearly identified and exposed (Figure 12-3).
♦ The splenic vessels are visualized and preserved.
♦ The pancreatic head, neck, and body are typically thickened and fibrotic, with some distortion of the normal anatomy.
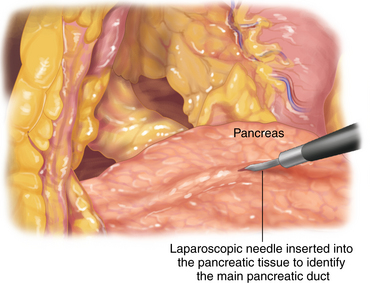
♦ The pancreatic duct is identified by inserting a laparoscopic needle aspirator in the pancreatic parenchyma, where the duct is thought to be situated (Figure 12-4).
♦ When available, an intraoperative ultrasound can assist with this.
♦ Aspiration of pancreatic fluid confirms the duct position.
♦ In patients with a preoperative pancreatic stent in place, duct identification can be easier.
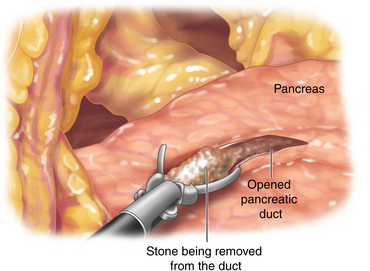
Opening of the pancreatic duct and stone extraction
♦ Using electrocautery, the pancreatic duct is entered in the body and opened longitudinally for the entire length of the pancreas, starting 1 to 2 cm away from the duodenal border and going distally, as far as possible. The ductotomy should be at least 7 cm in length.
♦ The duct should be thoroughly examined and all stones removed. A review of the preoperative imaging can be helpful for identifying the relative position of the stones; these ductal regions should be carefully evaluated (Figure 12-5).
Creation of the roux limb
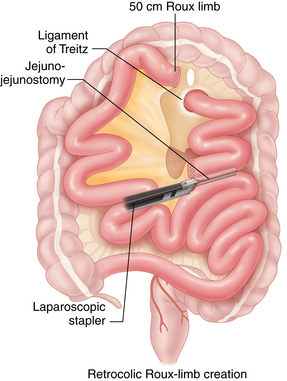
♦ The transverse colon is elevated to identify the ligament of Treitz.
♦ The jejunum is divided 40 cm distal to the ligament of Treitz using an endoscopic stapler (e.g., Endo-GIA 2.5 × 60 mm stapler, Covidien, Mansfield, Massachusetts). The mesentery of the small bowel is divided with the Harmonic device.
♦ A 50-cm Roux limb is measured and a side-to-side stapled jejunojejunostomy is created. To do this, the loops of bowel are approximated using an interrupted 2-0 silk suture. Enterotomies are made in the opposing segments of the small bowel using a Harmonic scalpel or hook electrocautery. A side-to-side jejunojejunostomy is created by two firings of the Endo-GIA 2.5 × 60 mm stapler in opposing directions. The common enterotomy is closed using another firing of the 2.5 × 60 mm Endo-GIA stapler. The mesenteric defect is closed using a running 2-0 silk suture (Figure 12-6).
♦ An opening is made in the transverse mesocolon, through the avascular area above the ligament of Treitz. The Roux limb is passed in a retrocolic fashion and placed over the pancreas. This should have no tension.
Pancreaticojejunostomy
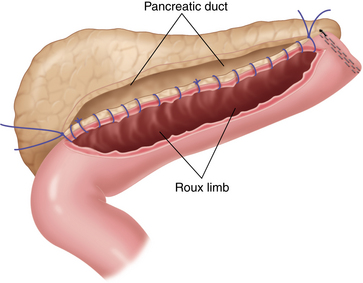
♦ A laparoscopic one-layered pancreaticojejunostomy is performed. The distal end of Roux limb is sutured using an interrupted 2-0 silk suture to the pancreatic parenchyma at the tail of the pancreas. The small bowel is opened for the same length as the pancreatic duct has been exposed.
♦ A 2-0 Vicryl suture is used as a running suture, to create a pancreaticojejunostomy, starting at the tail of the pancreas and moving toward the midline, taking full bites of the bowel wall and the pancreatic duct (Figure 12-7).
♦ A second suture is started at the head of the pancreas, run along the inferior border of the pancreas toward the middle in a similar fashion, and tied to the first suture.
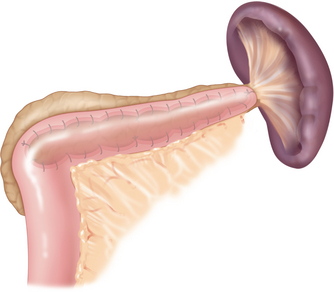
♦ The superior aspect of the pancreaticojejunostomy is sutured in a similar fashion (Figure 12-8).
Step 4. Postoperative care
♦ Patients are provided with a patient-controlled analgesia (PCA), and the nasogastric tube is kept in overnight.
♦ After removal of the nasogastric tube on the first postoperative day, the patients are given sips and then advanced to liquids the next day.
Step 5. Pearls and pitfalls
♦ This is an uncommon procedure with few published reports. Most described techniques are similar to what has been described here.3–5
♦ Previous history of recurrent attacks of pancreatitis can make entry into the lesser sac difficult, and care should be taken during this part.
♦ Conversion to open surgery should be considered when anatomic landmarks and structures are not clear, and palpation is thought to help in this process.
♦ The pancreatic tissue is usually thick, and thus the likelihood of pancreatic leak is relatively low.
Hines O, Reber H. Chronic pancreatitis. In Zinner M, Ashley S, editors: Maingot’s Abdominal Operations, ed 11, New York: McGraw Hill, 2007. Chap. 8
Cahen DL, Gouma DJ, Nio Y, et al. Endoscopic versus surgical drainage of the pancreatic duct in chronic pancreatitis. N Engl J Med. 2007;356(7):676-684.
Kurian MS, Gagner M. Laparoscopic side-to-side pancreaticojejunostomy (Partington-Rochelle) for chronic pancreatitis. J Hepatobiliary Pancreat Surg. 1999;6(4):382-386.
Palanivelu C, Shetty R, Jani K, et al. Laparoscopic lateral pancreaticojejunostomy: a new remedy for an old ailment. Surg Endosc. 2006;20;3:458-461.
Tantia O, Jindal MK, Khanna S, et al. Laparoscopic lateral pancreaticojejunostomy: our experience of 17 cases. Surg Endosc. 2004;18;7:1054-1057.