Head and uncinate process of pancreas drained by ventral pancreatic duct of Wirsung via major papilla
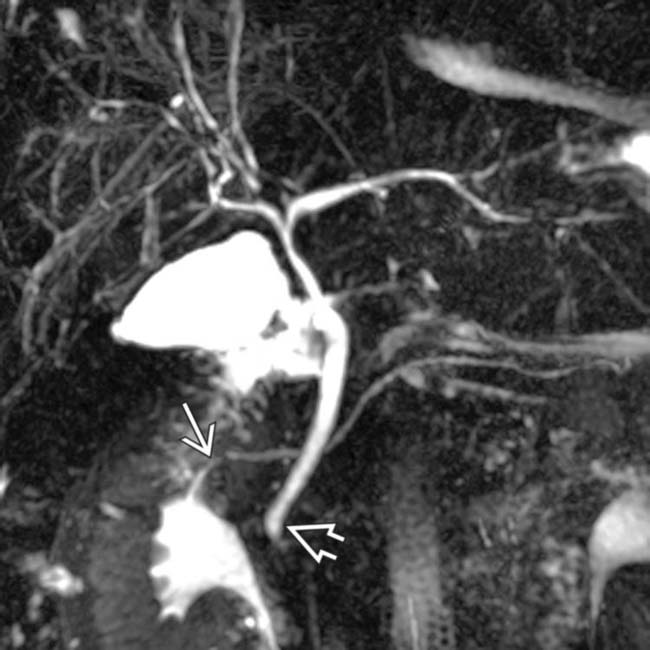
• MRCP: Best noninvasive modality for delineating divisum
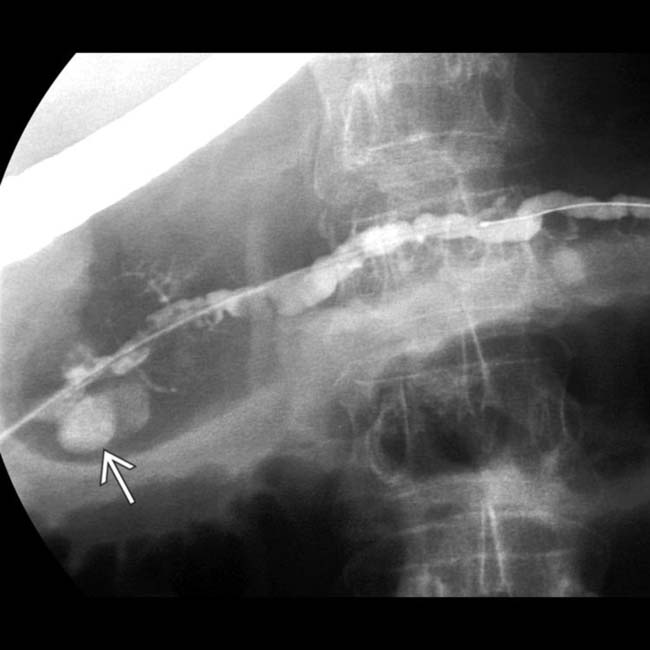
• ERCP: Most accurate method of diagnosing divisum
 Cannulation of major papilla reveals opacification of short, tapered, ventral pancreatic (Wirsung) duct
Cannulation of major papilla reveals opacification of short, tapered, ventral pancreatic (Wirsung) duct
 Cannulation of major papilla reveals opacification of short, tapered, ventral pancreatic (Wirsung) duct
Cannulation of major papilla reveals opacification of short, tapered, ventral pancreatic (Wirsung) duct
• CT: May demonstrate abnormally large pancreatic head or 2 distinct pancreatic moieties separated by fat cleft
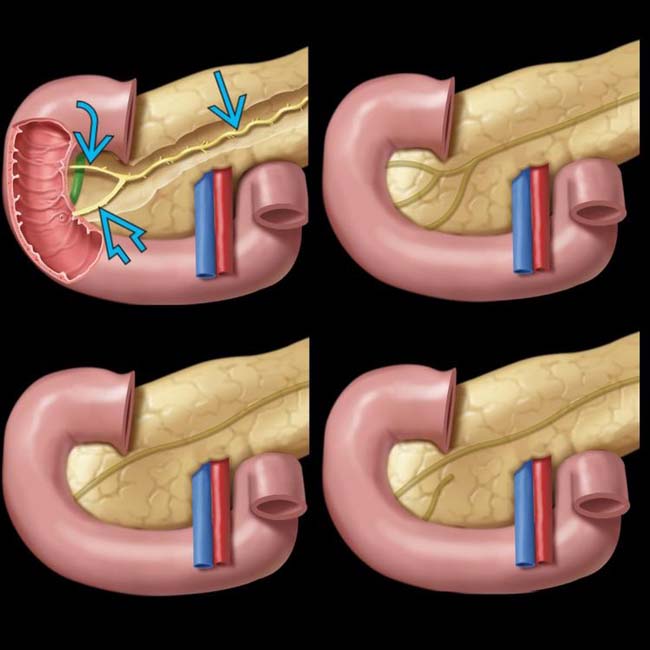
 , the accessory duct of Santorini
, the accessory duct of Santorini  , and the duct of Wirsung
, and the duct of Wirsung  . The lower right image shows pancreas divisum.
. The lower right image shows pancreas divisum.
 following cannulation of the minor papilla.
following cannulation of the minor papilla.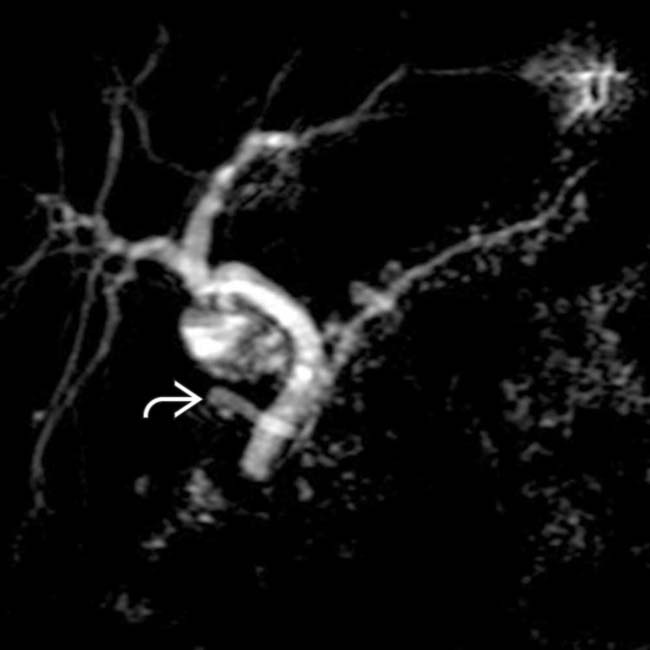
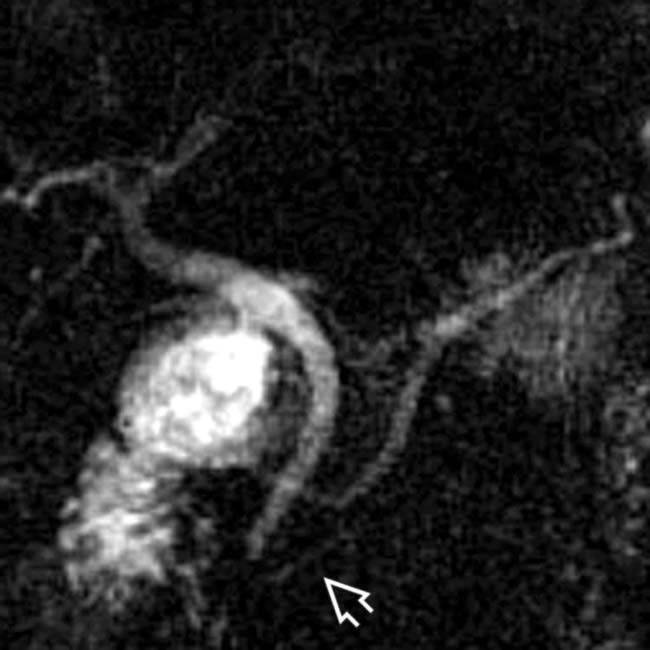
 . The ventral duct is not seen. Note the dilatation of multiple tiny pancreatic duct sidebranches throughout the gland, likely reflecting the patient’s history of chronic pancreatitis.
. The ventral duct is not seen. Note the dilatation of multiple tiny pancreatic duct sidebranches throughout the gland, likely reflecting the patient’s history of chronic pancreatitis.IMAGING
General Features
MR Findings
• MRCP is best noninvasive modality for delineating course and drainage pattern of dorsal and ventral PDs
• Pancreas may demonstrate abnormally high signal on T2WI and low signal on T1WI with peripancreatic free fluid in setting of superimposed pancreatitis
Radiographic Findings
• ERCP: Most accurate method of diagnosing divisum, but carries risks of invasive procedure
DIFFERENTIAL DIAGNOSIS
Pancreatic Ductal Carcinoma
PATHOLOGY
General Features
• Etiology
• Anatomy of pancreas divisum
 Dorsal PD drains pancreatic anterior head, neck, body, and tail via long and narrow (and sometimes dilated) duct of Santorini into minor papilla
Dorsal PD drains pancreatic anterior head, neck, body, and tail via long and narrow (and sometimes dilated) duct of Santorini into minor papilla
 Dorsal PD drains pancreatic anterior head, neck, body, and tail via long and narrow (and sometimes dilated) duct of Santorini into minor papilla
Dorsal PD drains pancreatic anterior head, neck, body, and tail via long and narrow (and sometimes dilated) duct of Santorini into minor papilla
 entering the minor papilla and the common bile duct
entering the minor papilla and the common bile duct  entering the duodenum at the major papilla. The relationship between the pancreatic and common duct is referred to as the crossing duct sign.
entering the duodenum at the major papilla. The relationship between the pancreatic and common duct is referred to as the crossing duct sign.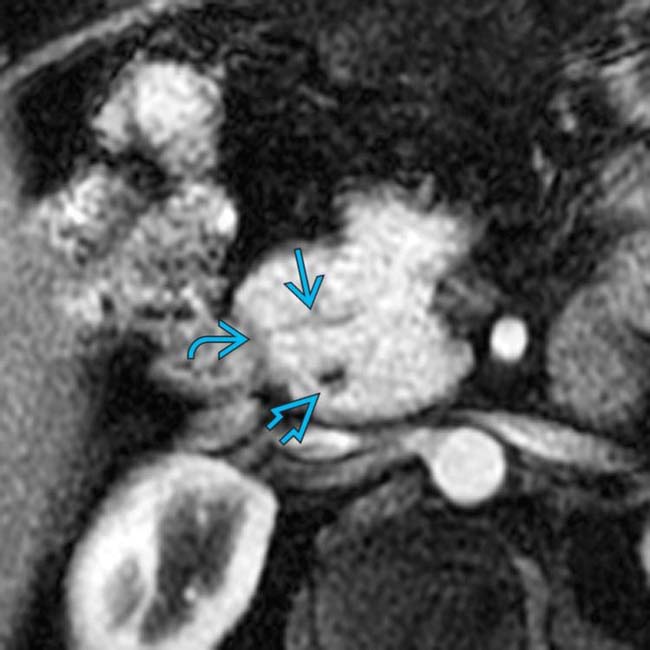
 entering the duodenum via the minor papilla
entering the duodenum via the minor papilla  . The common bile duct
. The common bile duct  is seen posteriorly as its enters the duodenum via the major papilla.
is seen posteriorly as its enters the duodenum via the major papilla.
 in a patient with pancreas divisum complicated by recurrent episodes of pancreatitis.
in a patient with pancreas divisum complicated by recurrent episodes of pancreatitis.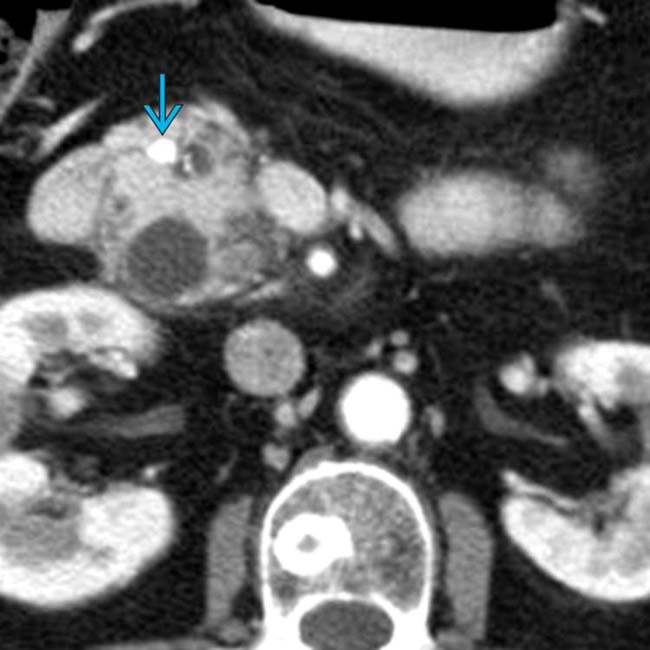
 within the duct of Santorini, which is of normal caliber downstream as it enters the minor papilla. The stone was confirmed and removed at ERCP, during which a pancreatic stent was also placed.
within the duct of Santorini, which is of normal caliber downstream as it enters the minor papilla. The stone was confirmed and removed at ERCP, during which a pancreatic stent was also placed.
 with a distal stricture due to prior pancreatitis. The main pancreatic duct (MPD)
with a distal stricture due to prior pancreatitis. The main pancreatic duct (MPD)  is seen in the body and tail. Note the separate duct of Wirsung
is seen in the body and tail. Note the separate duct of Wirsung  from the head and uncinate, indicating divisum.
from the head and uncinate, indicating divisum.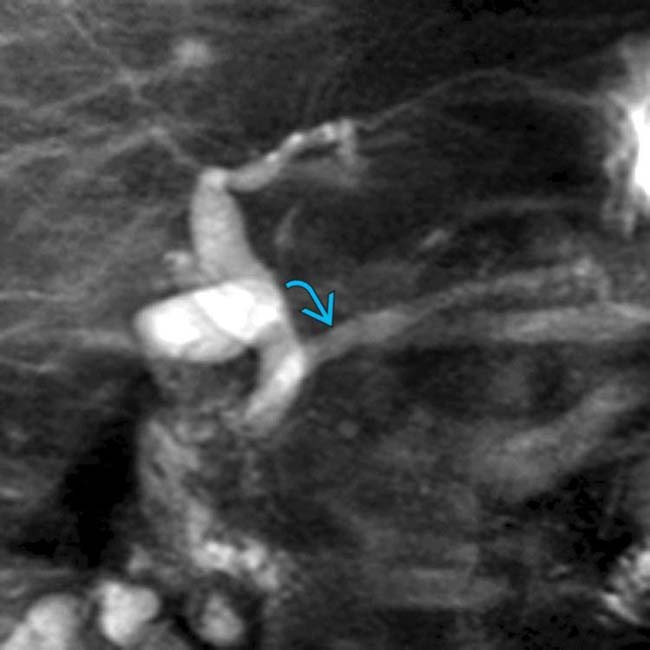
 without fluid accumulating in the duodenum, indicating a stricture at the minor papilla, likely the cause of the patient’s episodes of pancreatitis.
without fluid accumulating in the duodenum, indicating a stricture at the minor papilla, likely the cause of the patient’s episodes of pancreatitis.
 with a pancreas divisum configuration of the dorsal pancreatic duct.
with a pancreas divisum configuration of the dorsal pancreatic duct.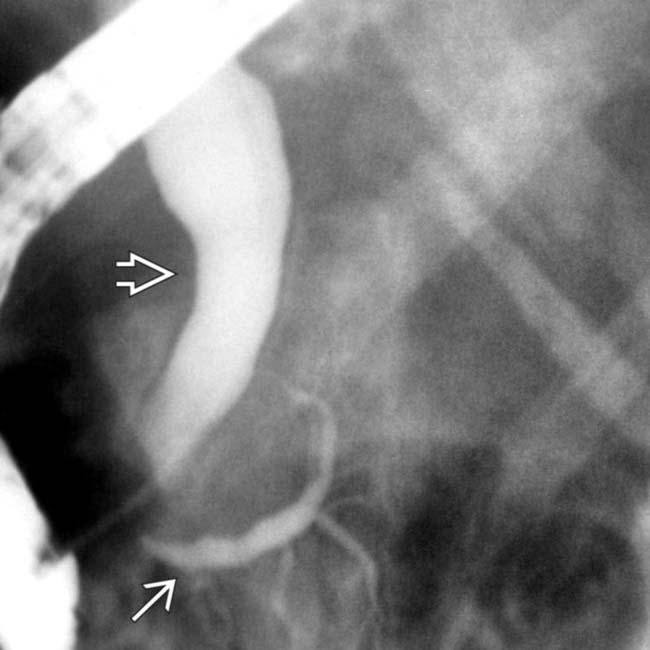
 and a dilated common bile duct
and a dilated common bile duct  following cannulation of the major papilla.
following cannulation of the major papilla.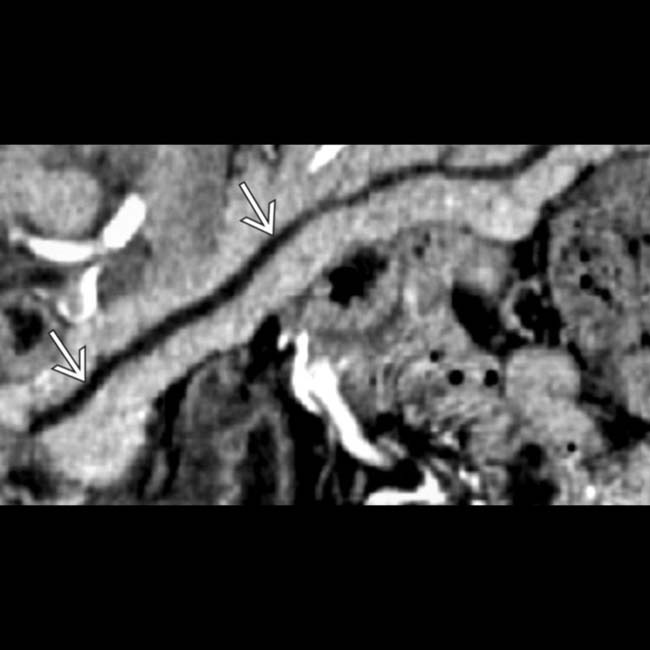
 continuing into the minor papilla.
continuing into the minor papilla.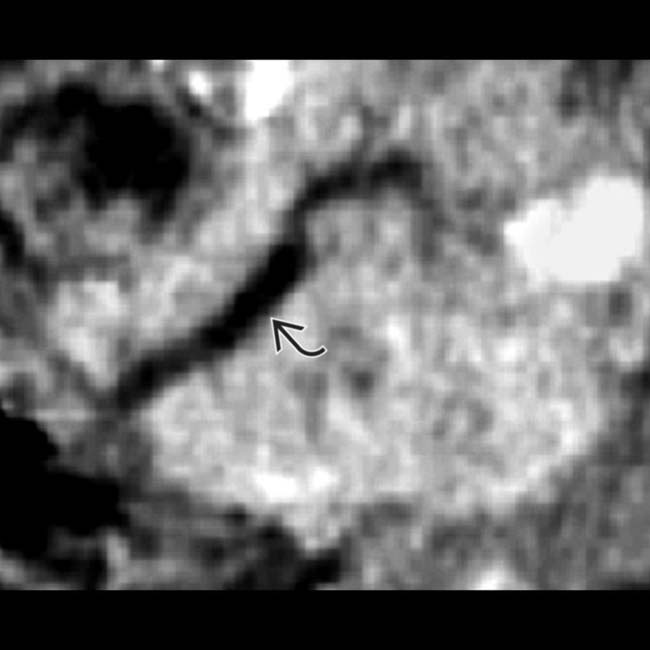
 ending blindly within the head of the pancreas.
ending blindly within the head of the pancreas.
 extending into the ampulla. The pancreatic duct is not seen extending into the major papilla.
extending into the ampulla. The pancreatic duct is not seen extending into the major papilla.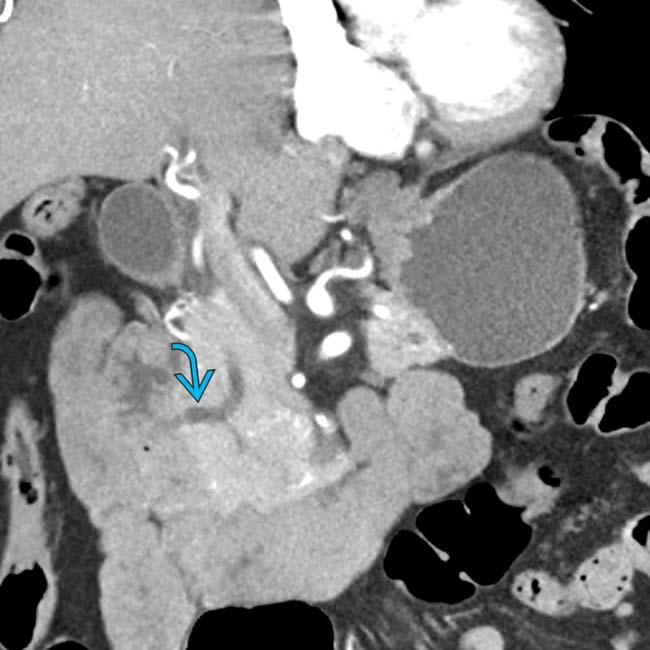
 . The dorsal duct was seen to be contiguous with the main pancreatic duct (not shown) and the ventral duct was not visualized, compatible with pancreatic divisum.
. The dorsal duct was seen to be contiguous with the main pancreatic duct (not shown) and the ventral duct was not visualized, compatible with pancreatic divisum.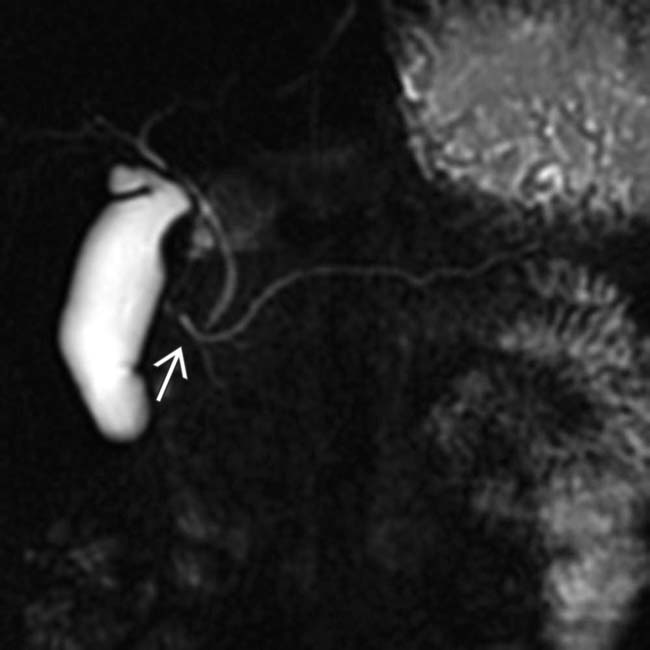
 , compatible with pancreatic divisum.
, compatible with pancreatic divisum.
 crossing the common bile duct to drain into the expected location of the minor papilla. The diminutive ventral duct is not seen. Note the distended gallbladder
crossing the common bile duct to drain into the expected location of the minor papilla. The diminutive ventral duct is not seen. Note the distended gallbladder  as well as fluid within the duodenum
as well as fluid within the duodenum  .
.








































































 separating the ventral and dorsal pancreatic segments.
separating the ventral and dorsal pancreatic segments.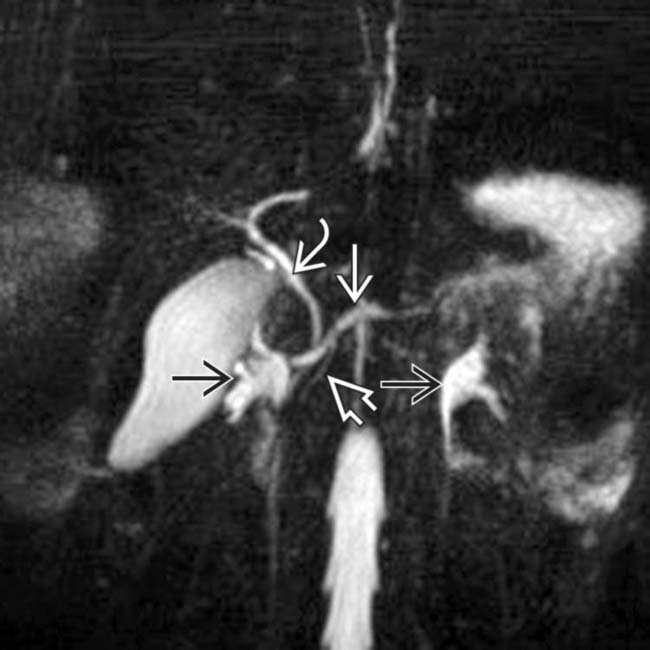
 crossing the common bile duct
crossing the common bile duct  to drain into the minor papilla. A small ventral duct
to drain into the minor papilla. A small ventral duct  can be seen in the pancreatic head, coursing toward the major papilla. Note also the fluid-filled renal collecting systems
can be seen in the pancreatic head, coursing toward the major papilla. Note also the fluid-filled renal collecting systems  , an occasional source of confusion.
, an occasional source of confusion.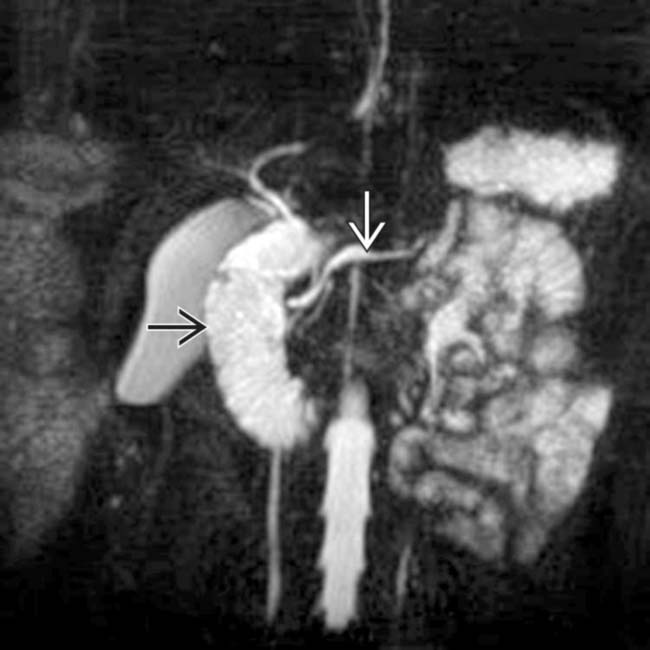
 filling with pancreatic juice. The diameter of the main pancreatic duct
filling with pancreatic juice. The diameter of the main pancreatic duct  does not change, indicating no functional obstruction.
does not change, indicating no functional obstruction.


