Chapter 12 Paediatric Proximal Ulnar Fractures
Introduction
Fractures of the proximal ulna comprise several types of olecranon fractures together with fractures involving the coronoid process. The reported incidence is between 4% and 7% of paediatric elbow fractures1–3 and they are often seen as part of combined more complex elbow injuries. Their incidence may vary greatly, however, even between different regions of the same country. For example in the Malmö area of Sweden they represent only 1.7% of paediatric elbow fractures, which is equivalent to an annual incidence of 0.8 olecranon fractures per 10 000 children.2
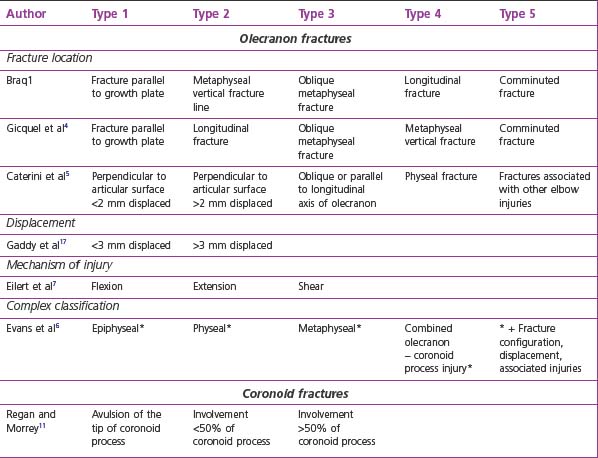
There are no widely accepted classification systems for olecranon fractures (Table 12.1). Bracq1 described a five-type classification system which was modified by Gicquel et al4 and which is based on the direction and localization of the fracture line. Another five-type classification system was introduced by Caterini et al.5 Their five categories differentiated between the direction of the fracture line, the degree of fracture displacement and the presence of associated injuries. A much more complex classification is described by Evans and Graham.6 They put emphasis on the anatomical site, the fracture configuration, the degree of intra-articular displacement and the type of associated injuries. The principal classification concentrates on four anatomically defined types: epiphyseal, physeal, metaphyseal and combined olecranon–coronoid process injuries. A simple two-group classification was advised by Papavasiliou et al.3 They separated intra-articular from extra-articular fractures, dividing the intra-articular fractures into four subgroups according to the degree of fracture displacement.
The mechanism of injury that produces different reproducible fracture patterns has also been used as a functional classification.7 In flexion type injuries the rare avulsion fracture and the much more frequent metaphyseal fractures of the olecranon occur. Fractures that result from injuries with an extended elbow usually result in greenstick type fractures of the olecranon with longitudinal fracture lines. They have associated injuries in 40–70% of cases. I am a firm believer in the functional classification and finds it very practical and useful.
Summary Box 12.1
Proximal ulna fractures account for 4–7% of paediatric elbow fractures.
They comprise olecranon and coronoid process fractures.
Several classification systems exist (Table 1), of which the functional classification based on the mechanism of injury is practical and helpful in planning treatment.
Background/aetiology
Olecranon fractures can occur after a fall onto the flexed or extended elbow.
In fractures that result from a flexion type injury a tension force acutely pulls on the posterior part of the olecranon mainly through the power of the triceps brachialis muscle but with assistance from the biceps, which produces a flexion force. This leads to a separation of the olecranon by a fracture line perpendicular to the longitudinal axis of the ulna, either through the metaphyseal area of the proximal ulna or through the proximal ulnar growth plate. The fracture line usually extends into the joint, making the injury an articular fracture. A rare flexion type injury that results from a direct blow to the olecranon creates shear forces at the area of impact, leading to a vertical fracture line with an intact proximal radio-ulnar joint. In these fractures the posterior periosteum does not disrupt and has the effect of an internal tension band.7
The extension type injury usually needs an additional valgus or varus stress to cause an olecranon fracture. In a fall on the outstretched hand the elbow joint is overextended with the olecranon locked in the olecranon fossa.1 Without additional valgus or varus stresses this injury mechanism most likely results in a supracondylar fracture. With additional valgus or varus stresses the olecranon may fracture in a greenstick type manner, producing longitudinal fracture lines that may extend well into the proximal ulnar shaft region. This fracture pattern is triggered by the specific anatomical properties of the growing proximal ulna. The olecranon represents a metaphyseal bony region with a strong periosteal sleeve. The periosteum may prevent true fracture displacement, allowing only for some bending in either a valgus or varus direction. This type of injury pattern makes associated lesions very likely.
Presentation, investigation, treatment options
Flexion type injury
Clinical presentation
The clinical presentation of a flexion type olecranon injury is characterized by local tenderness and swelling associated with an inability to actively extend the elbow. In children this may be difficult to test adequately because of pain and swelling. However, a multicentre prospective study has shown a high sensitivity of the elbow extension test at detecting any type of elbow fracture. In children there was an almost 50% likelihood of having sustained a fracture if the child was unable to actively extend the elbow.8 In those cases with major displacement of the fragments the gap between the bony pieces may be palpated.
Treatment options
The degree of fracture displacement will determine the treatment modality. Many of these fractures are not displaced or are mildly so, requiring plaster immobilization alone, or closed reduction followed by plaster immobilization with the arm in 80–90° of flexion.1 Some authors recommend plaster immobilization in elbow extension, but we have not found this to be either an appropriate or superior method of immobilization.
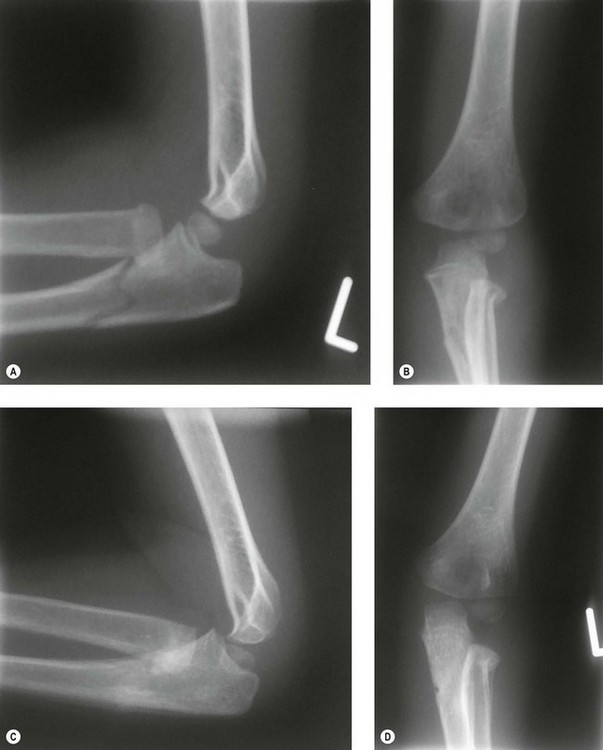
Moderately displaced fractures or unstable mildly displaced fractures that redisplace after closed reduction are best managed by closed reduction and percutaneous pinning by K-wires. Postoperatively an above-elbow cast in neutral is applied for 4 weeks. Severely displaced or irreducible fractures do need open reduction and internal fixation in order to achieve an anatomical position. The fixation method of choice in this situation is the classic K-wire fixation with AO tension band wire (Fig. 12.1).9
Extension type injury
Radiography
The incidence of associated fractures is estimated to be around 40–50%,1,5,6 with 20–31% being radial neck fractures (Fig. 12.2) and 3.5–12% lateral condyle fractures.1,4–6 Other accompanying lesions such as an elbow dislocation or medial epicondyle fractures are very rare. A proximal ulnar fracture may also be combined with a fracture dislocation of the radial head, leading to a Monteggia equivalent fracture pattern (Fig. 12.3),10 which account for 5–7.5% of associated lesions.5,6
Treatment options
The treatment has to address the olecranon fracture itself and the associated injuries. In most cases closed reduction without internal fixation is sufficient to treat the olecranon injury (Fig. 12.2). In severely displaced fractures or those that involve the joint line, closed reduction and K-wire pinning or even open reduction and pinning in an anatomically reduced position may be necessary. Special fracture configurations may require fixation by K-wires and tension band techniques or, in oblique fractures, screws or very rarely plate fixation. If the fracture extends into the proximal ulna, intramedullary rodding, i.e. in the Morote technique, is a good method of fixation (Fig. 12.3).
Coronoid process fractures
Radiography
A classification system based on the size of the fractured coronoid process has been proposed and is useful as it guides treatment options.11 In type one there is an avulsion of the tip of the coronoid process, in type two less than 50% of the coronoid process is involved and in type three more than 50% is involved (Table 12.1).
Treatment options
After reduction of the elbow dislocation the size and displacement of the coronoid process fracture should be assessed. An undisplaced or minimally displaced fracture can be treated by plaster cast immobilization in neutral rotation of the forearm. Larger and more displaced fragments are an indication for open reduction and internal fixation (Fig. 12.4).
Surgical techniques, rehabilitation
Olecranon fractures
Open reduction
All severely displaced fractures and those that cannot be reduced anatomically are treated by open reduction and internal fixation through a direct posterolateral approach. Fragment fixation is achieved using K-wires only, K-wires plus a tension band with absorbable sutures or figure-of-eight wiring (Fig. 12.1). Even screws alone and tension bands attached to screws have been successfully used.
A different fixation concept which also facilitates metal removal uses two threaded pins and an adjustable lock for fracture compression. Preliminary results in a small group of patients are reported to be good.12 After open reduction an above-elbow split plaster is used for immobilization for 2 weeks. Functional treatment is established as early as possible, provided the fixation is stable.
Of all of these fixation methods, the tension band techniques have been shown to have higher biomechanical stability than K-wires and screws alone. The tension band wires in combination with screw fixation have proven to be the strongest.13 There is a tendency to use strong absorbable sutures such as PDS instead of wires as the tension band since these do not require removal.14 However, a biomechanical study that tested the strength of fixation of both constructs found lower failure loads and fewer compression forces at the fracture site when absorbable sutures were being used.15 For this reason, in older children ordinary tension band wiring should be used to allow for early functional treatment.
Coronoid process fractures
Undisplaced, minimally and moderately displaced fractures of the coronoid process with small and medium-sized fragments are managed conservatively, if the elbow is stable enough to allow early functional treatment. A split above-elbow cast is applied for 2–3 weeks, followed by early motion and intensive physiotherapy. For cases with persistent elbow instability and larger fragments we advise open reduction and K-wire or screw fixation through an anterior approach (Fig. 12.4). We also aim for early functional treatment after a 2- to 3-week period of plaster immobilization.
Outcome
The published results of olecranon fracture treatment are very good.16 In Braq’s series of 83 cases1 there were 86.5% favourable outcomes. In a medium-term study of 35 patients, all 23 patients with a fracture displacement of less than 3 mm and who were treated conservatively had a satisfactory outcome. Of the 12 patients who underwent open reduction and internal fixation, 10 could be reviewed and all demonstrated a satisfactory result.17
In a long-term case series follow-up of 39 patients who had sustained their fracture at an average age of 7.4 years and were reviewed at an average age of 32 years, only 7.6% had poor results. Thirty-four patients had a good result and in 85% of the cases an intra-articular fracture was noted. The long-term prognosis was related to the anatomical site of the fracture line and to the presence of associated lesions, which were noted to be a negative predictor.5
Other authors have reported very good clinical results in 85–90% of cases.1,4,16,18 The radiological outcome, however, was less favourable in some series. In Gicquel et al’s study4 35% of patients had unsatisfactory reduction of their fractures on the postoperative radiographs. The disappointing radiological follow-up, however, did not have any impact on the longer-term clinical outcome.
All series have stated that associated lesions contribute clearly to worse clinical results1,4,6 and radiological appearances.1,6
Complications
Complications directly related to proximal ulnar fractures are infrequent. All complications, such as restriction of postoperative motion, neurovascular damage, compartment syndrome, delayed bony healing, pseudarthrosis and loss of reduction, have been reported, but in small numbers.16 Olecranon overgrowth with elongation of the proximal ulna has been observed mainly in chronic avulsion injuries but also in acute cases with delayed union and following open reduction and internal fixation.3 Although loss of position may also occur and impair long-term elbow function, fragment displacement of less than 2 mm can be accepted and will not result in a functional deficit.5
1 Bracq H. Fractures de l’olécrane. In: Fractures du coude chez l’enfant. Symposium of SOFCOT, directed by Pouliquen JC. Rev Chir Orthop. 1987;73:469-471.
2 Landin LA, Danielsson LG. Elbow fractures in children: an epidemiological analysis of 589 cases. Acta Orthop Scand. 1986;57:309-312.
3 Papavasiliou VA, Beslikas TA, Nenopoulos S. Isolated fractures of the olecranon in children. Injury. 1987;18:100-102.
4 Gicquel P, De Billy B, Karger CS, et al. Olecranon fractures in 26 children with mean follow-up of 59 months. J Pediatr Orthop. 2001;21:141-147.
5 Caterini R, Farsetti P, D’Arrigo C, et al. Fractures of the olecranon in children: long-term follow-up of 39 cases. J Pediatr Orthop B. 2002;11:320-328.
6 Evans MC, Graham HK. Olecranon fractures in children. Part 1: a clinical review. Part 2: a new classification and management algorithm. J Pediatr Orthop. 1999;19:559.
7 Eilert RE, Erickson MA. Fractures of the proximal radius and ulna. In: Beaty JH, Kasser JR, editors. Rockwood and Wilkins’ fractures in children. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:443-490.
8 Appelboam A, Reuben AD, Benger JR, et al. Elbow extension test to rule out elbow fracture: multicentre, prospective validation and observational study of diagnostic accuracy in adults and children. BMJ. 2008;337:a2428.
9 Dormans JP, Rang M. Fractures of the olecranon and radial neck in children. Orthop Clin North Am. 1990;21:257-267.
10 Bado JL. The Monteggia lesion. Clin Orthop. 1967;50:71-86.
11 Regan W, Morrey BF. Classification and treatment of coronoid process fracture. Orthopedics. 1992;15:845-848.
12 Gicquel P, Giacomelli MC, Karger C, et al. Surgical technique and preliminary results of a new fixation concept for olecranon fractures in children. J Pediatr Orthop. 2003;23:398-401.
13 Murphy DF, Greene WB, Dameron TB. Displaced olecranon fractures in adults. Clin Orthop. 1987;224:215-223.
14 Gortzak Y, Mercado E, Atar D, et al. Pediatric olecranon fractures: open reduction and internal fixation with removable Kirschner wires and absorbable sutures. J Pediatr Orthop. 2006;26:39-42.
15 Parent S, Wedemeyer M, Mahar AT, et al. Displaced olecranon fractures in children: a biomechanical analysis of fixation methods. J Pediatr Orthop. 2008;28:147-151.
16 Graves SC, Canale T. Fractures of the olecranon in children: long-term follow-up. J Pediatr Orthop. 1993;13:239-241.
17 Gaddy BC, Strecker WB, Schoenecker PL. Surgical treatment of displaced olecranon fractures in children. J Pediatr Orthop. 1997;17:321-324.
18 Karlsson MK, Hasserius R, Karlsson C, Besjakov J, Josefsson PO. Fractures of the olecranon during growth: a 15–25-year follow-up. J Pediatr Orthop B. 2002;11:251-255.