8 Pacemaker, Defibrillator, and Lead Codes and Headers
Devices are used for more indications in the treatment of patients with bradyarrhythmias, tachyarrhythmias, and congestive heart failure, and more algorithms are developed either to stimulate multiple chambers (cardiac resynchronization) or to minimize unnecessary pacing when possible.1,2 It is noteworthy that, unlike some therapies, the generic pacemaker codes have withstood the test of time.
 Pacemaker Codes
Pacemaker Codes
Three-Position Ichd Code (1974)
In 1974 the Inter-Society Commission for Heart Disease Resources (ICHD) proposed a three-position code to allow a uniform system to describe the functionality of a pacemaker platform.3 The goal was to create a generic code that would work among all platforms; it would also allow for concise description of what was becoming a more complex issue. The first letter of the code was to distinguish the chamber(s) being paced. The second letter was to determine the chamber(s) that were sensed for intrinsic electrical depolarizations and to start the timer for determining the next paced beat delivery. The third letter of the code was to describe how the pacing was to be affected by a sensed event (i.e., inhibiting pacing or triggering pacing in response to sensing).
Position one can be the atrium (A), the ventricle (V), or both atrium and ventricle (D) for location of pacing. Position two again represents atrium (A), the ventricle (V), or both (D), meaning sensing can occur for spontaneous electrical depolarizations in either chamber. The third position describes whether sensing leads to inhibition of pacing (I), triggering the delivery of a pacing stimulus (T), or both inhibition and triggering (D). Tables 8-1 and 8-2 outline the options and different pacing configurations.
TABLE 8-1 The 1974 Three-Position ICHD Code or Three-Letter Identification Code*
| First Letter | Second Letter | Third Letter |
|---|---|---|
| Chambers paced | Chambers sensed | Mode of response |
* Letters used: A, atrium; D, double-chamber; I, inhibited; O, not applicable; T, triggered; V, ventricle.
Adapted from Parsonnet V, Furman S, Smyth NPD: Implantable cardiac pacemakers: Status report and resource guideline. Pacemaker Study Group, Inter-Society Commission for Heart Disease Resources (ICHD). Circulation 50:A-21, 1974. Copyright 1974 American Heart Association.
TABLE 8-2 Pacing Modes Described by the Three-Position ICHD Code
| Mode | Description |
|---|---|
| VOO | Asynchronous ventricular pacing; no sensing function |
| AOO | Asynchronous atrial pacing; no sensing function |
| DOO | Dual-chamber (AV-sequential) asynchronous pacing; no sensing function |
| VVI | Ventricular pacing inhibited by ventricular sensing |
| VVT | Ventricular pacing triggered instantaneously by ventricular sensing |
| AAI | Atrial pacing inhibited by atrial sensing |
| AAT | Atrial pacing triggered instantaneously by atrial sensing |
| VAT | Ventricular pacing triggered after a delay by atrial sensing |
| DVI | Dual-chamber (AV-sequential) pacing inhibited by ventricular sensing |
AV, Atrioventricular.
Modified from Parsonnet V, Furman S, Smyth NPD: Implantable cardiac pacemakers: status report and resource guidelines. Pacemaker Study Group, Inter-Society Commission for Heart Disease Resources (ICHD). Circulation 50:A21, 1974. Copyright 1974 American Heart Association.
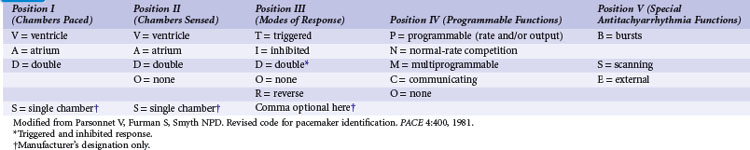
Five-Position Ichd Code (1981)
Table 8-3 shows the different options for all five positions, but as one would surmise, it is now assumed all devices can store information and can be programmed, thus obviating the need for that nomenclature. Currently, pacing platforms that provide antitachycardia pacing are typically identified based on the specifics of the device platform rather than an additional letter in the code (e.g., Medtronic EnRhythm pacing platform allows atrial antitachycardia pacing therapy). Using this convention, a single-chamber pacing system today would be described as VVIM to designate multiprogrammability or VVIC to designate the presence of telemetry (communication). In reality, this fourth letter is implied due to the presence of telemetry and multiprogrammability in all of our current platforms. Table 8-4 provides examples of the many different ways to describe pacemaker function that are highly descriptive of the available features on pacing systems, but not readily used in day-to-day management of pacemakers.
TABLE 8-4 Pacing Modes Described by the Five-Position ICHD Code
| Mode | Description |
|---|---|
| VDD,M (VDDM) | Ventricular antibradycardia pacing inhibited by ventricular sensing, triggered after delay by atrial sensing; multiprogrammable device; no antitachyarrhythmia (antitachycardia) function. |
| DDD,M (DDDM) | Dual-chamber (AV-sequential) antibradycardia pacing inhibited by sensing in either chamber, with ventricular pacing triggered after delay by sensing in atrium after ventricular event; multiprogrammable device; no antitachycardia function. |
| VVI,MB (VVIMB) | Ventricular antibradycardia pacing inhibited by ventricular sensing; multiprogrammable device; pacing bursts for ventricular tachycardia, means of activation unspecified. |
| AAR,ON (AARON) | No antibradycardia function; nonprogrammable device; normal-rate competition for termination of atrial tachycardia, activated by atrial sensing. |
| AOO,OE (AOOOE) | Asynchronous atrial antibradycardia pacing; nonprogrammable device; externally activated atrial antitachycardia pacing, nature unspecified. |
AV, Atrioventricular.
Modified from Parsonnet V, Furman S, Smyth NPD: Revised code for pacemaker identification. PACE 4:400, 1981.
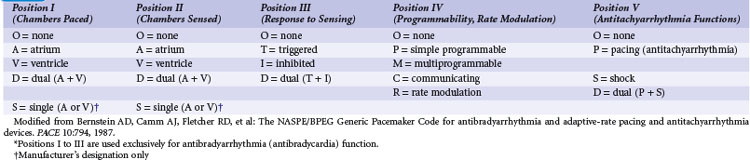
NASPE/BPEG Generic (NBG) Pacemaker Code
The Mode Code Committee of the North American Society of Pacing and Electrophysiology (NASPE), now known as the Heart Rhythm Society, in cooperation with the British Pacing and Electrophysiology Group (BPEG), developed a code in 1987 (Table 8-5).4 The one change still used today is the letter R in the fourth position to represent rate-modulated pacing to treat chronotropic incompetence. The R in the fourth position was developed in response to the many sensors available to help the pacemaker mimic sinus nodal function in response to external or internal stimuli. The other development in the nomenclature is the use of the letter S for shock delivery for tachyarrhythmias with the fifth position in the code.
The NASPE/BPEG Generic (NBG) Pacemaker Code retains all the characteristics of the 1974 ICHD Code and some of those of the later five-position codes. To deal with the increasing complexity of later devices, however, it was considered necessary to clarify several features and to define more explicitly how the code was to be used. Positions I, II, and III were still used exclusively for antibradycardia pacing, but position IV had the option of describing either programmability or rate-responsive pacing. With establishment of programmability in almost all devices, position IV evolved to denote the presence or absence of rate-response pacing. Position V is for describing the ability to deliver antitachycardia therapy, as either antitachycardia pacing or a shock. As of 1987, shocks were described as either low-energy cardioversions or high-energy defibrillation. No distinction was made between low-energy and high-energy shocks in the nomenclature. The original code of 1981 allowed for different letters to describe different forms of pacing trains used in tachycardia termination, such as burst (B), scanning (S), or external (E). The update of 1987 simplified the descriptors to pacing (P), shock (S), or pacing and shocks (D).4,5
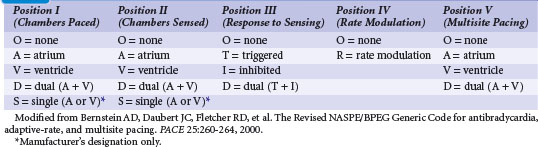
Revised NBG Code
The structure of the revised NBG Code is summarized in Table 8-6, with examples of its use in Table 8-7.6 Note that with each modification, the first three positions continue to describe antibradycardia pacing, but in this update, no mention of antitachycardia pacing is made.7 Positions I, II, and III indicate the chambers in which pacing and sensing occur and the effect of sensing on the triggering or inhibition of subsequent pacing stimuli. In this context, “sensing” refers specifically to the detection of spontaneous cardiac depolarizations (or spurious interference signals interpreted as spontaneous cardiac depolarizations) outside the refractory periods of the pulse generator. Position IV is now used only to indicate the presence (R) or absence (O) of an adaptive-rate mechanism (rate modulation). This position is also used to denote that changes can occur in pacing parameters, such as changes in the atrioventricular (AV) delay in response to increased heart rates.
| Code | Meaning |
|---|---|
| VOO, VOOO, or VOOOO | Asynchronous ventricular pacing; no sensing, rate modulation, or multisite pacing. |
| VVIRV | Ventricular inhibitory pacing with rate modulation and multisite ventricular pacing (i.e., biventricular pacing or more than one pacing site in one ventricle). |
| This mode is often used in patients with heart failure, chronic atrial fibrillation, and intraventricular conduction delay; assessed by atrial fibrillation group in MUSTIC study.* | |
| AAI, AAIO, or AAIOO | Atrial pacing inhibited by sensed spontaneous atrial depolarizations; no rate modulation or multisite pacing. |
| AAT, AATO, or AATOO | Atrial pacing with atrial outputs elicited without delay on atrial sensing during alert period outside pulse generator’s refractory period (used primarily as diagnostic mode to determine exactly when atrial depolarizations are sensed); no rate modulation or multisite pacing. |
| AATOA | Atrial pacing with atrial outputs elicited without delay on atrial sensing during alert period outside pulse generator’s refractory period, without rate modulation but with multisite atrial pacing (i.e., biatrial pacing or more than one pacing site in one atrium).† |
| DDD, DDDO, or DDDOO | Dual-chamber pacing (normally inhibited by atrial or ventricular sensing during alert portion of VA interval or by ventricular sensing during alert portion of AV interval, and with ventricular pacing triggered after programmed PV interval by atrial sensing during alert portion of VA interval); no rate modulation or multisite pacing. |
| DDI, DDIO, or DDIOO | Dual-chamber pacing without atrium-synchronous ventricular pacing (atrial sensing merely cancels pending atrial output without affecting escape timing); no rate modulation or multisite pacing. |
| DDDR or DDDRO | Dual-chamber, adaptive-rate pacing; no multisite pacing. |
| DDDRA | Dual-chamber, adaptive-rate pacing with multisite atrial pacing (i.e., biatrial pacing or more than one pacing site in one atrium); assessed in multicenter DAPPAF study.‡ |
| DDDOV | Dual-chamber pacing without rate modulation but with multisite pacing (i.e., biventricular pacing or more than one pacing site in one ventricle).§ |
| DDDRD | Dual-chamber pacing with rate modulation and multisite pacing both in the atrium (i.e., biatrial pacing or pacing in more than one site in one atrium) and in the ventricle (i.e., biventricular pacing or pacing in more than one site in one ventricle). |
MUSTIC, Multisite Stimulation in Cardiomyopathy.
* Leclerq C, Walker S, Linde C, et al. Comparative effects of permanent biventricular and right-univentricular pacing in heart failure patients with chronic atrial fibrillation. Eur Heart J 23:1780-1787, 2002.
† Revault d’Allonnes G, Pavin D, Leclerq C, et al. Long-term effects of biatrial synchronous pacing to prevent drug-refractory atrial tachyarrhythmias: a nine-year experience. J Cardiovasc Electrophysiol 11:1081-1091, 2000.
‡ Fitts SM, Hill MR, Meral R, et al. Design and implementation of the Dual Site Atrial Pacing to Prevent Atrial Fibrillation (DAPPAF) clinical trial. J Interv Card Electrophysiol 2:139-144, 1998.
§ Cazeau S, Leclerq C, Lavergne T, et al. Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med 344:873-880, 2001.
Modified from Bernstein AD, Daubert J-C, Fletcher RD, et al. The Revised NASPE/BPEG Generic Code for antibradycardia, adaptive-rate, and multisite pacing. PACE 25:260-264, 2000.
As multisite pacing and physiologic pacing with leads in specific positions (e.g., Bachman bundle) are further investigated, use of the fifth letter may become more prevalent.8,9
 Defibrillator Codes
Defibrillator Codes
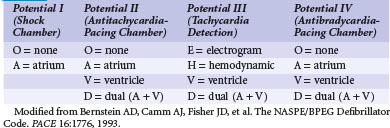
NASPE/BPEG Defibrillator (NBD) Code
On January 23, 1993, the NASPE (now Heart Rhythm Society) Board of Trustees approved the adoption of the NASPE/BPEG Defibrillator (NBD) Code (Table 8-8).10 It was developed by the NASPE Mode Code Committee, composed of members of NASPE and BPEG, and was intended for describing cardiac-defibrillator capabilities and operation. The resultant code for ICDs is similar in form to the long-established pacing code. Although the pacing code described antibradycardia pacing in detail and then acknowledged the presence of antitachycardia therapy, the ICD code describes the antitachycardia therapy in detail and then acknowledges the presence of antibradycardia pacing.
NBD Code, Short Form
As an additional means of concisely distinguishing among devices limited to cardioversion or defibrillation and those that incorporate antitachycardia and antibradycardia pacing, a short-form code was defined (Table 8-9). It is intended for use only in conversation and again rarely used given the widespread prevalence of both antitachycardia pacing and shocking across platforms and manufacturers.
| Code | Meaning |
|---|---|
| ICD-S | ICD with shock capability only |
| ICD-B | ICD with bradycardia pacing as well as shock |
| ICD-T | ICD with tachycardia (and bradycardia) pacing as well as shock |
ICD, Implantable cardioverter-defibrillator.
Modified from Bernstein AD, Camm AJ, Fisher JD, et al. The NASPE/BPEG Defibrillator Code. PACE 16:1776, 1993.
 Lead Code
Lead Code
NASPE/BPEG Pacemaker-Lead (NBL) Code
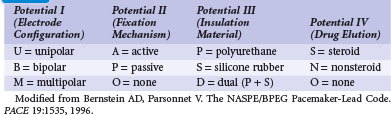
In 1996 the NASPE Board of Trustees voted to adopt a generic code for pacemaker leads, to be known as the NASPE/BPEG Pacemaker-Lead (NBL) Code. The code was approved subsequently by BPEG, and its definition and usage conventions were published as a NASPE Policy Statement. The NBL Code is a four-position generic code intended for use in conversation, record keeping, writing, and labeling. All four positions (potentials), as defined in Table 8-10, are used in every circumstance, unlike the NBG Code, for which only three or four of the five positions are often used. Table 8-11 provides examples of the use of the simple NBL Code.11
| Code | Meaning |
|---|---|
| UPSO | Unipolar passive-fixation lead with silicone-rubber insulation but without elution of an anti-inflammatory agent |
| BAPS | Bipolar active-fixation lead with polyurethane insulation and steroid elution |
Modified from Bernstein AD, Parsonnet V. The NASPE/BPEG Pacemaker-Lead Code. PACE 19:1535, 1996.
The NBL Code is designed so that it cannot be confused with the NBG or NBD Codes. As with those earlier codes, the characteristics were chosen in terms of clinical priority to describe characteristics with significant influence on the behavior of the device under consideration. For this reason, the NBL Code does not address such features as connector design and electrode location. Moreover, until there was emergence of clearer patterns in the electrode configurations used for cardioversion and defibrillation, with or without the pulse generator housing serving as part of the electrode system, it was believed that attempts to design a practical code encompassing leads used for cardioversion and defibrillation as well as pacing would be premature.12
 Headers
Headers
In the early history of pacing systems, differences among lead sizes, pacing configurations and polarity, and manufacturer variability led to a wide variety of pacemaker/ICD headers (connections of the lead[s] to the generator). With the proliferation of international standards (IS-1) technology, many of the connection issues of the past have disappeared. IS-1 lead technology and defibrillation connections (DF-1) header standards have resolved many of the differences in compatibility between manufacturers and platforms. Physicians now have a wider array of generators and systems from which to choose depending on patient need. The new international standard connections for leads and defibrillation leads (IS-4 and DF-4) will likely replace the bulkier IS-1/DF-1 technology (Figs. 8-1 and 8-2). This will further streamline connections and decrease the complexity and frequency of connections that could be a failure point in the system function. This should reduce the size of the junction for connecting the lead(s) to the generators, commonly referred to as headers (Figs. 8-3 and 8-4). With IS-4/DF-4 technology, rather than making three separate connections between ICD pace/sense, right ventricular (RV) defibrillation coil, and superior vena cava (SVC) coil with the header, an IS-4 lead will have one connection with a DF-4 header, minimizing the risk of poor contact between header set screw and lead pin.
1 Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350(21):2140-2150.
2 Mirowski M. The automatic implantable cardioverter-defibrillator: an overview. J Am Coll Cardiol. 1985;6:461-466.
3 Parsonnet V, Furman S, Smyth NPD. Implantable cardiac pacemakers: status report and resource guidelines. Pacemaker Study Group, Inter-Society Commission for Heart Disease Resources (ICHD). Circulation. 1974;50:A21.
4 Bernstein AD, Camm AJ, Fletcher RD, et al. The NASPE/BPEG Generic Pacemaker Code for antibradyarrhythmia and adaptive-rate pacing and antitachyarrhythmia devices. Pacing Clin Electrophysiol. 1987;10(4 Pt 1):794-799.
5 Bernstein AD, Brownlee RR, Fletcher RD, et al. Report of the NASPE Mode Code Committee. PACE. 1984;7:395.
6 Bernstein AD, Daubert JC, Fletcher RD, et al. The Revised NASPE/BPEG Generic Code for antibradycardia, adaptive-rate, and multisite pacing. PACE. 2000;25:260-264.
7 Bernstein AD, Camm AJ, Furman S, Parsonnet V. The NASPE/BPEG codes: use misuse, and evolution. PACE. 2001;24:787-788.
8 Epstein AE, Dimarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: executive summary. Heart Rhythm. 2008;5(6):934-955.
9 Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices), with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51:e1-e62.
10 Bernstein AD, Camm AJ, Fisher JD, et al. The NASPE/BPEG Defibrillator Code. PACE. 1993;16:1776.
11 Bernstein AD, Parsonnet V. The NASPE/BPEG Pacemaker-Lead Code. PACE. 1996;19:1535.
12 Gregoratos G, Cheitlin MD, Conill A, et al. ACC/AHA Guidelines for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). J Am Coll Cardiol. 1998;31:1175-1209.