P
P cell See cell, ganglion; cell, P.
p value See significance.
pachometer A device, mounted on a slit-lamp, that is used for measuring corneal thickness (or the depth of the anterior chamber). It consists of an optical system that provides two half-fields by means of two glass plates with parallel sides placed in front of one objective of the microscope, the other being occluded. These plates rest one on top of the other with the junction between them situated so as to horizontally bisect the objective. The top plate can be rotated while the bottom one is fixed. The observer viewing through the microscope sees two corneal optical sections and adjusts the top plate until the outer surface of the epithelium appears aligned with the inner surface of the endothelium (Fig. P1). The corneal thickness is then read directly from a scale attached to the pachometer and calibrated in millimetres. To increase the accuracy of the measurement a special eyepiece is used with the microscope. It has a magnification of × 10 and has two additional components: a horizontal slit and a bi-prism. The role of the eyepiece is to remove from the field of view half of the two optical sections. The measurement of the depth of the anterior chamber is made with a similar device but with a different scale. Note: also spelt pachymeter. Pachometry can also be carried out using slit-scanning topography in which a computerized system integrates a series of slit-beam images to produce a map of the curvature and elevation of the anterior and posterior surfaces as well as corneal thickness. An instrument with greater magnification (called a micropachometer) has been devised, principally for research purposes, using a projection system which incorporates variable doubling plates and forms two slit images on the cornea in conjunction with the viewing system of a slit-lamp and a magnification of up to × 100, mounted on another arm. This instrument allows the measurement of the thickness of the corneal epithelium alone with a precision that can reach ±1µm. The above pachometers are referred to as optical pachometers to differentiate them from ultrasonic pachometers, which use high-frequency ultrasound waves, reflected from the anterior and posterior corneal surfaces and a transducer probe placed against the cornea. Ultrasound and slit-scanning pachometers have higher reproducibility and less interobserver variation than subjective optical pachometers. Usage of pachometers (pachymeters) includes evaluation of contact lens wear, pre- and post-refractive surgery (e.g. PRK, LASEK, LASIK), glaucoma detection and monitoring corneal oedema.
See ultrasonography.
pad arm An extension of a spectacle frame either integral with the bridge or as a separate attachment to which a pad is fitted.
pad, nose One of a pair of protuberances attached to the bridge of a spectacle frame or mounting that rests against the side of the nose. Syn. nose pad.
See bridge, pad; pince-nez; spectacle frame, metal.
Paget’s disease See disease, Paget’s.
palinopsia Visual persistence of the image of an object in the absence of its original stimulus. There is usually a latent period, which may amount to several minutes between the visual stimulation and the corresponding mental image. The latter typically disappears within seconds, although it may persist in some cases for several minutes. The subsequent mental image is quite faithful to the original stimulus. It is usually associated with a lesion in the parieto-occipital or temporal-occipital areas as a result of a cerebral infarction, epilepsy, tumour, or brain injury. Syn. visual perseveration.
palisades of Vogt The crests of epithelium folds that run radially towards the cornea, at the limbus, from the bulbar conjunctiva. They are often seen in slit-lamp examination, especially in pigmented individuals, and clearly in fluorescein angiography. They may contain stem cells, which play a role in the regeneration of corneal epithelium cells.
palpebrae See eyelids.
palpebrae muscle, levator See muscle, levator palpebrae.
palpebral aperture; conjunctiva See under the nouns.
palpebral, elephantiasis See elephantiasis oculi.
palpebral fissure See aperture, palpebral.
palpebral ligament See ligament, palpebral.
palsy Synonym for paralysis, although it often implies partial paralysis.
abducens nerve p. See paralysis of the sixth nerve.
Bell’s p. A paralysis of the upper and lower muscles of the face on one side, due to an inflammation of the facial nerve. It results in a wider palpebral aperture and inability to close the eye on the affected size and drying of the cornea.
See sign, Bell’s; tears, artificial; tears, crocodile.
double elevator p. A condition characterized by limited or complete inhibition of the upward rotation of an eye, due either to paresis of its superior rectus and inferior oblique muscles, or to entrapment of the inferior orbital tissues. It may be congenital or acquired (e.g. a lesion in the pretectum). Treatment is principally surgical.
gaze p . Inability of the eyes to make conjugate movements due to a lesion in the cortical or subcortical oculomotor centres.
See paralysis of the fourth nerve; paralysis of the sixth nerve; paralysis of the third nerve.
supranuclear gaze p. A disturbance of the conjugate movements of the eye. If the lesion is in the frontal lobe, the patient is unable to direct the eyes to the contralateral side of the lesion (frontal gaze palsy). In bilateral lesion the patient is unable to turn the eyes voluntarily in any direction but is able to maintain fixation and perform pursuit movements. If the lesion is in the midbrain it produces Parinaud’s syndrome, in which there is an inability to elevate (and sometimes depress) the eyes on command and the pupils are large and may not react to light. If the lesion is in the paramedian pontine reticular formation there is ipsilateral horizontal gaze palsy, while lesions in the medial longitudinal fasciculus produce internuclear ophthalmoplegia.
See ophthalmoplegia, internuclear.
pannus Abnormal superficial vascularization of the cornea covering the upper half, or sometimes the entire cornea. It is characterized by a thick plexus of vessels. It is found in some cases of contact lens wear, mainly soft lenses. Pannus following contact lens wear is referred to as corneal vascularization. If induced by soft lenses, it can be reduced by changing to lenses of high oxygen transmissibility or ceasing contact lens wear. Deep corneal vascularization involving the stroma is usually the result of a disease process (e.g. interstitial keratitis, phlyctenular keratitis, severe long-standing trichiasis, trachoma).
panophthalmitis Acute inflammation of the eyeball involving all its structures and extending into the orbit. The disease develops very rapidly. The eyelids are red and swollen and there is severe chemosis of the conjunctiva. The cornea is often a whitish mass of necrotic tissue and there may be severe ocular pain.
See endophthalmitis.
pantoscopic angle See angle, pantoscopic.
Panum’s area; fusional space See under the nouns.
papilla Any small elevation shaped like a nipple.
Plural : papillae.
See follicle, conjunctival.
Bergmeister’s p. A cone-shaped, sheath of glial cells (astrocytes) and connective tissue covering the hyaloid artery formed during embryonic development over the optic disc and projecting into the vitreous humour. It usually atrophies before term but in some individuals it persists and a proliferation of glial cells form a glial veil. It may obscure the full view, or usually only part, of the optic disc and may sometimes suggest a disc tumour but it is in fact benign, stable and does not interfere with vision.
See hyaloid remnant.
lacrimal p. See lacrimal papilla.
p. lacrimalis See lacrimal tubercle.
papillary conjunctivitis, giant See conjunctivitis, giant papillary.
papillitis See neuritis, optic; pseudopapilloedema.
papilloedema A non-inflammatory oedema of the optic nerve head produced by raised intracranial pressure, and due most commonly to a cerebral tumour. It can also result from cerebral abscesses, meningitis, encephalitis, subarachnoid haemorrhages, head injury, hydrocephalus, etc. The optic disc appears raised above the level of the retina and its margins are blurred, the central vessels on the surface of the disc are displaced forward, the retinal veins are dilated and there is nearly always a loss of induced venous pulsation. The swollen disc displaces the retina and this causes an enlargement of the blind spot on visual field measurement. In the early stages visual acuity is not affected (unlike in papillitis), although if the condition persists there will be some loss. In advanced stages, there may be haemorrhages around the disc, secondary optic atrophy, exudates, as well as headaches and vomiting. The condition is usually bilateral. Note: also spelt papilledema. Syn. choked disc.
Table P1
Differential diagnosis between papilloedema and papillitis
| papilloedema | papillitis | |
| signs | ||
| disc elevation | raised | slightly raised |
| disc hyperaemia | present | present |
| disc margins | blurred | blurred |
| retinal veins | congested | congested |
| haemorrhages | near disc | some in late stage |
| pupil light reflex | normal | impaired |
| venous pulsation | absent | present |
| secondary optic atrophy | present in late stage | may appear in late stage |
| symptoms | ||
| visual acuity | normal, except in late stage | reduced |
| visual field | enlarged blind spot | central scotoma |
| diplopia | present | absent |
| colour vision | normal | impaired |
| pain | absent | present on moving the eyes |
| headache | present | absent |
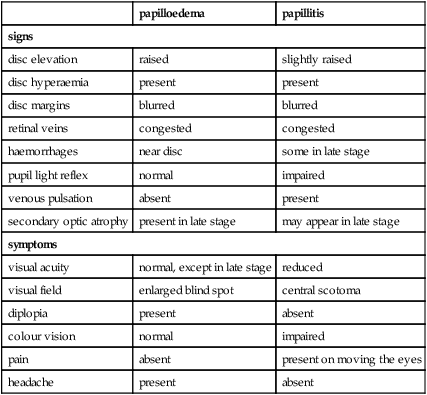
See atrophy, optic; neuritis, optic; pseudopapilloedema; syndrome, Foster Kennedy.
papilloma A tumour most commonly found on the conjunctiva, the limbus or the lid margins. It is usually benign. It should be excised but it is likely to recur.
papillomacular bundle; fibres See fibres, papillomacular.
paracontrast See metacontrast.
paradoxical ARC See retinal correspondence, abnormal.
paradoxical diplopia See diplopia, incongruous.
paraffin See tears, artificial.
parallax Apparent displacement of an object viewed from two different points not on a straight line with the object.
binocular p . The difference in angle subtended at each eye by an object that is viewed first with one eye and then with the other.
chromatic p. Apparent lateral displacement of two monochromatic sources (e.g. a blue object and a red object) when observed through a disc with a pinhole placed near the edge of the pupil. When the pupil is centred on the achromatic axis (in some people the pinhole may have to be placed away from the centre of the pupil), the two images appear superimposed. The relative displacement of the two images becomes reversed when the pinhole is on the other side of that axis. This phenomenon is attributed to the chromatic aberration of the eye.
See chromostereopsis; aberration, longitudinal chromatic.
monocular p. The apparent change in the relative position of an object when the eye is moved from one position to another.
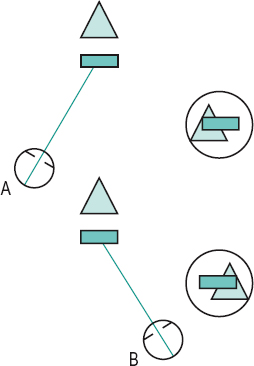
motion p . Apparent difference in the direction of movement or speed produced when the subject moves relative to his environment (Fig. P2). Example: when viewing the landscape through the window of a moving train near objects appear to move much more quickly than distant objects. See perception, depth; stereopsis.
relative binocular p. See acuity, stereoscopic visual.
paralysis Loss of action of a muscle due to injury or disease of that muscle or its nerve supply.
See palsy.
abducens p. See paralysis of the sixth nerve.
p. of accommodation See accommodation, paralysis of.
p. of convergence A condition characterized by an inability of the eyes to converge while all other monocular eye movements are unaffected. The patient notices diplopia in near vision, which usually occurs suddenly. It is presumably due to some lesion in the nuclei responsible for convergence, as may happen in tabes dorsalis or Parkinson’s disease.
divergence p. A condition characterized by an inability of the eyes to diverge while all other monocular eye movements are unaffected. It is characterized by a sudden development of diplopia with marked esotropia at distance and sometimes headaches. The key difference with divergence insufficiency is the sudden onset of symptoms. Its association includes encephalitis, multiple sclerosis, head trauma, cerebral haemorrhage, brain tumour and vascular lesions of the brainstem.
p. of the fourth nerve A condition characterized by a hypertropia of the eye with the affected superior oblique muscle. It may be due to a lesion of the fourth cranial nerve or its nucleus as a result of injury (the most common cause), vascular lesions, aneurysm or tumour. The patient usually presents with an abnormal head posture to avoid diplopia. If the condition does not recover by itself following therapy of the underlying cause, surgery is usually the only alternative treatment. Syn. trochlear paralysis.
See head posture, abnormal; nerve, trochlear; strabismus, paralytic.
oculomotor p . See paralysis of the third nerve.
p. of the sixth nerve A condition characterized by an esotropia of the eye with the affected lateral rectus muscle. It may be due to a lesion of the sixth cranial nerve or its nucleus as a result of a vascular disease (e.g. diabetes, hypertension), injury, or tumour. The patient presents with an abnormal head turn to avoid diplopia. If the condition does not recover by itself following therapy of the underlying cause, surgery is usually the only alternative treatment. Syn. abducens paralysis; lateral rectus palsy.
See head posture, abnormal; nerve, abducens; strabismus, paralytic; syndrome, Gradenigo’s; transposition.
p. of the third nerve A condition that leads to a wide impairment of motor function, as this nerve innervates most of the muscles of the eye. It may be due to a vascular disease (e.g. diabetes, hypertension), aneurysm (especially of the internal carotid artery), injury or tumour. In total paralysis only the lateral rectus and the superior oblique muscles will be spared and the eye will be in a position of abduction, slight depression and intorsion. Ptosis will also be present and the pupil will be dilated and non-reactive, and there will also be paralysis of accommodation. If the condition does not recover by itself following therapy of the underlying cause, surgery is usually the only alternative. Syn. oculomotor paralysis.
See circle of Willis; nerve, oculomotor; ophthalmoplegia; strabismus, paralytic; syndrome, Benedikt’s; syndrome, Weber’s; test, forced duction; transposition.
trochlear p . See paralysis of the fourth nerve.
parastriate area See areas, visual association.
parasympathetic nervous system See system, autonomic nervous.
parasympatholytic Pertains to a drug that blocks the effects of the parasympathetic nervous system. Examples: atropine, cyclopentolate. Syn. antimuscarinic, anticholinergic, atropine-like.
See acetylcholine; cycloplegia; mydriatic.
parasympathomimetic drug A drug with an action resembling that caused by stimulation of the parasympathetic nervous system. Example: a miotic of which there are two types: a direct-acting cholinergic, such as pilocarpine or carbachol; and the other, indirect-acting anticholinesterase, such as physostigmine, neostigmine, echothiophate iodide, demecarium bromide. Syn. cholinergic drug.
See miotics.
paraxial Pertains to light rays situated near enough to the axis of an optical system for the gaussian theory to apply.
paraxial approximation See ray, paraxial.
paraxial equation, fundamental Equation based on gaussian theory and dealing with refraction at a spherical surface:
< ?xml:namespace prefix = "mml" />

where n and n’ are the refractive indices of the media on each side of the spherical surface, r is the radius of curvature of the surface and l and l’ the distances of the object and the image from the surface, respectively. n/l and n’ /l’ are the vergences (or reduced vergences) of the incident and refracted light rays respectively. L’ – L corresponds to the change produced by the surface in the vergence of the light and is called the focal power (or vergence power, or refractive power) F of the surface. Thus
Focal power is usually expressed in dioptres and can be either positive or negative.
At a reflecting surface or a mirror the equation becomes
where r is the radius of curvature of the surface or mirror. Syn. general refraction formula. See distance, image; distance, object; sign convention; theory, gaussian; vergence.
paraxial optics; ray See under the nouns.
paraxial region The hypothetical cylindrical narrow space surrounding the optical axis within which rays of light are still considered paraxial. Syn. gaussian space.
See ray, paraxial; theory, gaussian.
paraxial theory See theory, gaussian.
paresis Slight or partial paralysis.
Parinaud’s syndrome See syndrome, Parinaud’s.
Parks three-step test See test, three-step.
pars An anatomical part.
pars ciliaris muscle See muscle of Riolan.
pars plana; plicata See ciliary body.
pars planitis See uveitis, intermediate.
partial sight See vision, low.
parvo cells See cell, ganglion; geniculate bodies, lateral.
parvocellular layer See geniculate bodies, lateral.
parvocellular visual system See system, parvocellular visual.
past-pointing See pointing, past-.
patellar fossa See fossa, hyaloid.
pathological myopia See myopia, pathological.
pathology, ocular The discipline which deals with the nature of diseases of the eye and its surrounding structures, their effect on the ocular tissues and on ocular functions, as well as the causes and management.
pathway 1. A collection of nerve fibres (axons) along which nervous impulses travel. 2. A path or a route.
geniculocalcarine p. See radiations, optic.
geniculostriate p. 1. See radiations, optic. 2. Some authors consider this term to be a synonym of visual pathway.
magnocellular p . See system, magnocellular visual.
motor p. Pathway from the cortex to the muscles that control the movements of the eyes enabling them to act as a unit.
parvocellular p . See system, parvocellular visual.
retinotectal p. 1. The nervous pathway connecting the retina to the pretectal region (anterior to the superior colliculi) and from there to the Edinger–Westphal nucleus. It is involved in the pupillary light reflexes. 2. The nervous pathway between the retina and the superior colliculus. It is involved in the involuntary blink reflex to a dazzling light and in the eye movements occurring in response to the sudden appearance of a novel or a threatening stimulus.
See blind sight; fibres, pupillary; reflex, pupil light; pretectum.
uveoscleral p . An unconventional route through which the aqueous humour drains out of the eye. The aqueous passes from the anterior chamber across the iris root through small spaces between the ciliary muscle fibres into the supraciliary space and suprachoroid space. The fluid is believed to escape the eye via veins in the ciliary muscle and anterior choroid. The amount of aqueous outflow through this route amounts to between 10% and 15%, the rest flows out through the conventional pathway via the trabecular meshwork and into Schlemm’s canal. Prostaglandin drugs reduce the intraocular pressure by increasing the outflow through the uveoscleral pathway. This pathway is occasionally made use of in cyclodialysis.
visual p . Neural path starting in the photoreceptors of the retina and travelling through the following structures: the optic nerve, the optic chiasma, the optic tract, the lateral geniculate bodies, the optic radiations and the visual cortex where the pathway ends. The fibres of the optic nerve of one eye meet with the fibres from the other eye at the optic chiasma, where approximately half of them (the nasal half of the retina) cross over to the other side. Thus, there is semidecussation in the visual pathway (Fig. P3).
See area, visual; decussation; magnification, cortical; retinotopic map.
patient Term originating from the Latin patior meaning to suffer; one who suffers or is ill and requires treatment.
pattern A combination of acts or parts, forming a consistent or characteristic arrangement or behaviour.
A p. Neuromuscular anomaly of the eyes characterized by an increase in exotropia when the eyes fixate downward, or increase in esotropia when the eyes fixate upward. Upgaze and downgaze are usually measured at 25 degrees from the horizontal. Syn. A syndrome.
See strabismus, convergent; strabismus, divergent.
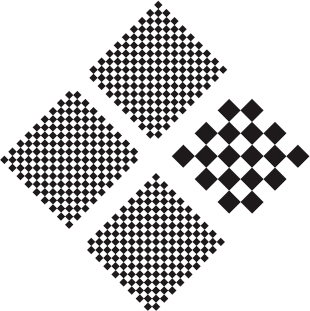
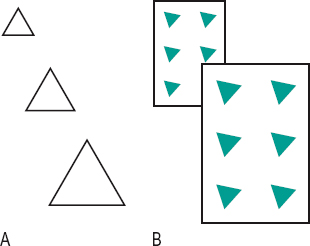
checkerboard p. A square set of equal size black and white squares placed adjacent to one another. It is used to test visual acuity. The common way of using this pattern is to present it in the form of a square diamond made up of four smaller diamonds. Three of these are composed of a pattern of much smaller squares than the fourth. Resolution of the pattern with larger squares consists in indicating where it is located (top, bottom, right or left) while the other three squares appear as a uniform grey. This acuity test is less dependent on cognitive factors than letters. (Fig. P4).
See acuity, visual; test type.
V p. A neuromuscular anomaly of the eyes characterized by an increase in exotropia when the eyes rotate upward, or increase in esotropia when the eyes rotate downward. Syn. V syndrome.
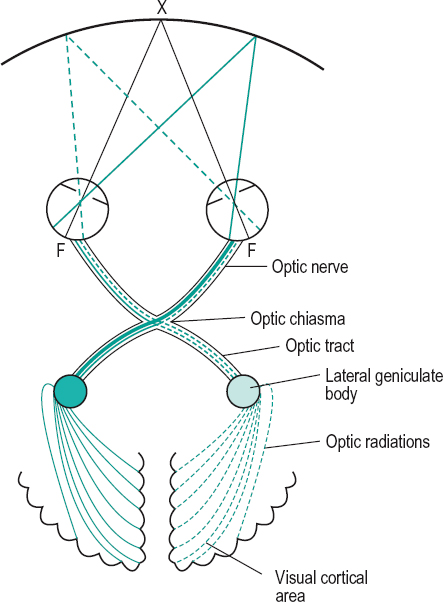
Table P2
Clinical manifestations of lesions in the visual pathway
| site of lesion | clinical manifestations |
| macula | central scotoma |
| papillomacular bundle | central or centrocaecal scotoma |
| other part of the retina | scotoma on the opposite side of the central fixation point |
| complete section of one optic nerve | total blindness of that eye absence of direct light reflex presence of consensual light reflex other eye: normal pupil reaction, direct but not consensual |
| pituitary enlargement pressing on inferior part of chiasma | bitemporal hemianopia or bitemporal superior quadrantanopia |
| aneurysm pressing on lateral part of the chiasma | binasal hemianopia |
| sagittal section in the middle of the | bitemporal hemianopia normal pupil reflexes if light falls on temporal |
| chiasma | retina |
| optic tract | contralateral incongruous homonymous hemianopia Wernicke’s pupillary reflex |
| lateral geniculate body | contralateral incongruous homonymous hemianopia normal pupil reflexes |
| anterior optic radiations on one side | contralateral incongruous homonymous hemianopia often sparing of the macula |
| normal pupil reflexes | |
| visual cortex on one side | contralateral congruous homonymous hemianopia often sparing of the macula normal pupil reflexes |
See strabismus, convergent; strabismus, divergent.
X p. A neuromuscular anomaly in which the visual axes are more divergent when the eyes fixate upward and downward, as compared to the primary position of gaze.
Y p. A neuromuscular anomaly of the eyes in which there is increasing exotropia as the eyes rotate straight upward with orthotropia in the primary position and on downward gaze.
paving-stone degeneration See degeneration, paving-stone.
PD Abbreviation for interpupillary distance and also, but more rarely, for prism dioptre.
PD gauge; meter See pupillometer.
pearls, Elschnig’s Transparent clusters formed by proliferation of epithelial lens cells found in the remains of the capsule of the crystalline lens following extracapsular cataract extraction. They rarely affect vision.
See cataract extraction, extracapsular; ring, Soemmering’s.
pedicle, cone See cone pedicle.
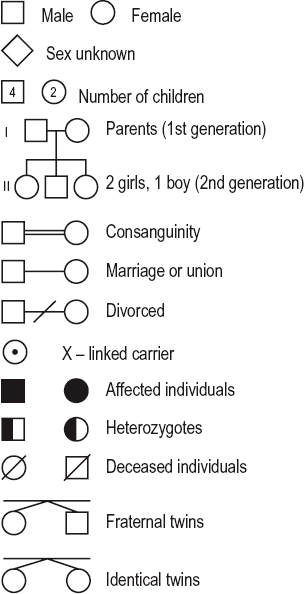
pedigree A chart or diagram of the ancestral history of a family or of an extended family (kindred), or of individual family members, their relationships and their status regarding a trait or condition. It is used in genetics to analyze inheritance. The analysis often begins with an affected family member (called a proband or propositus) through whom the family is ascertained (Fig. P5).
See gene; inheritance.
pegaptanib sodium See anti-VEGF drugs.
Pelli-Robson chart See chart, Pelli–Robson.
pellucid Allowing maximum passage of light.
pellucid marginal corneal degeneration See degeneration, pellucid marginal corneal.
pelopsia Anomaly of visual perception in which objects appear to be much nearer than they actually are. It may be due to vision in a very clear atmosphere, recent wear of an optical correction, neurosis, etc.
See metamorphopsia.
pemirolast potassium See mast cell stabilizers.
pemphigoid, cicatricial A rare, idiopathic, chronic systemic disease, most commonly of the elderly and characterized by recurrent blisters and bullae of the skin and mucous membranes, with subsequent scarring and shrinkage. The disease may affect only the conjunctiva (ocular pemphigoid). In this case, the clinical picture is a conjunctivitis with hyperaemia, mucous discharge and small vesicles, which on bursting result in ulceration, pseudomembranes, conjunctival subepithelial fibrosis and conjunctival shrinkage. The disease may give rise to adhesion between the palpebral and bulbar conjunctiva (symblepharon), ankyloblepharon, xerophthalmia, keratoconjunctivitis sicca, entropion, trichiasis and dry eye with corneal ulcer. There is pain or irritation and blurred vision. Treatment includes corticosteroids, surgery for entropion and trichiasis, and keratoprosthesis if vision is affected. Syn. benign mucous pemphigoid.
See conjunctivitis, pseudomembranous; syndrome, Stevens–Johnson; test, ocular ferning.
pemphigoid, ocular See pemphigoid, cicatricial.
penalization A clinical method of treating amblyopia and eccentric fixation in which vision by the fixating eye is decreased by various means (optical overcorrection, atropinization for near vision especially, and neutral density filters) in order to compel the amblyopic eye to fixate. Sometimes the treatment consists of using the amblyopic eye for near vision and the fixating eye for distance vision.
See attenuation; Bangerter foils; occlusion treatment; pleoptics.
pencil of light See light, pencil of.
pencil push-up See convergence insufficiency.
pencil-to-nose exercise See convergence insufficiency.
penetrance The frequency with which the characteristics transmitted by a gene appear in individuals possessing it. Penetrance is represented as the ratio of individuals who carry the gene and express its effects, over the total number of carriers of the gene in a population. Few of the genes in the genome show a high penetrance because environmental factors play a role in development. Examples: familial exudative vitreoretinopathy and neurofibromatosis (type 1 and type 2), which are both inherited as autosomal dominant, have 100% penetrance; about 90% of the children who carry the retinoblastoma gene develop the disease while the gene remains non-penetrant in the remaining 10% of the children.
See expressivity; vitreoretinopathy, familial exudative.
penetrating keratoplasty See keratoplasty.
pendular nystagmus See nystagmus.
penicillin See antibiotic.
penumbra 1. Region of very low illumination on a dark background. 2. Zone in which the brightness varies from some illumination to zero (umbra) in the shadow cast by an opaque object intercepting light from an extensive light source.
See shadow.
percept The complete mental image of an object obtained in response to sensory stimuli.
perception The mental process of recognizing and interpreting an object through one or more of the senses stimulated by a physical object. Thus one recognizes the shape, colour, location and differentiation of an object from its background.
See sensation; visual integration.
anorthoscopic p . See anorthoscope.
binocular p . Perception obtained through simultaneous use of both eyes.
contour p . See contour.
depth p . Perception of the distance of an object from the observer (absolute distance) or of the distance between two objects (relative distance). Our ability to judge the latter is much more precise than for the former. Many factors contribute to depth perception. Most important is the existence on the two retinae of different images of the same object (called binocular disparity or retinal disparity). There are also many other contributing factors, such as the characteristics of the stimulus (called cues), binocular parallax and, to a smaller extent, the muscular proprioceptive information due to the efforts of accommodation and convergence. Depth perception is more precise in binocular vision but is possible in monocular vision using the following cues: interposition (superposition), relative position, relative size, linear perspective, textural gradient, aerial perspective, light and shade, shadow and motion parallax (Fig. P6). Syn. spatial vision.
See acuity, stereoscopic visual; cell, binocular; cliff, visual; illusion, moon; perspective, aerial; perspective, linear; relief; room, Ames; room, leaf; stereopsis.
dermo-optical p. See perception, extrasensory.
extrasensory p. Perception obtained by means other than through the ordinary senses as, for example, telepathy (mind reading) or reading by moving a finger over a printed text (dermo-optical perception).
light p . (LP) Term used to indicate a barely seeing eye that can just see light but not the form of objects. Loss of light perception represents blindness.
subliminal p. Stimuli below the threshold of sensation (i.e. subliminal) may, in rare circumstances (e.g. exposure of 40 ms duration masked by another stimulus), unconsciously arouse perception. The effect is then of extremely short duration (less than 200 ms).
visual p . Perception obtained through the sense of vision.
perceptual span See reading.
Percival criterion See criterion, Percival.
peribulbar block See injection, peribulbar.
perichoroidal space See space, suprachoroidal.
pericorneal plexus See plexus, pericorneal.
perimeter An instrument for measuring the angular extent and the characteristics (e.g. presence of scotoma) of the visual field.
See campimeter; field, visual; isopter; screen, tangent.
arc p. Perimeter consisting of a semicircular arc, the inside surface of which is painted matt black or grey. The patient’s head is placed such that the eye under investigation is located at the centre of curvature of the arc. The visual field is determined by moving a target along the black surface of the perimeter until the patient either just sees it or just no longer sees it. The targets are small discs of varying colour and size attached to the end of black wands or may be projected on the arc, which can be rotated around the fixation point located at its centre. Thus the visual field can be tested along any meridian.
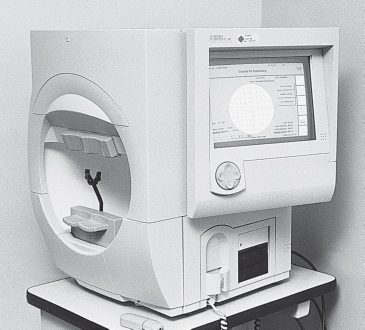
automated p . An instrument to test the visual field in which the presentation of the stimuli and the recording are carried out electronically and under the control of a built-in computer. There exist many types (e.g. Henson CFA, Humphrey Field Analyzer, Octopus, Dicon). Computerized perimeters have the following advantages: the examination strategy is reproducible; they can be operated by non-specialists; the testing routine (e.g. number of stimuli or their location) can be altered by modifying the program; each instrument can contain several examination routines aimed at testing various pathologies (e.g. one for glaucoma and another for hemianopic defects); the computer capacity can be used for quantifying the results as, for example, in the Henson CFA where the visual fields can be classified as normal, suspect or defective on the basis of a system included in the instrument (Fig. P7). Syn. computerized perimetry.
See Algorithm, Swedish Interactive Thresholding; perimetry, frequency doubling; perimetry, short wavelength automated; test, Esterman.
bowl p . See perimeter, Goldmann.
Goldmann p. Perimeter consisting of a hemispherical bowl, the inside radius of which is 30 cm. Targets of varying intensity and size are projected onto the inside white surface. The background luminance of the bowl is also controlled. In addition there is a telescope attached to the back of the bowl through which the practitioner can verify that the patient maintains fixation. Goldmann perimeter can be used either for kinetic or static perimetry, although it is more appropriately designed for the former. Syn. bowl perimeter.
See perimetry, kinetic; perimetry, static.
projection p. A perimeter in which the target is projected either onto an arc or a bowl such as the Goldmann perimeter.
perimetry The determination of the extent of the visual field, usually for the purpose of detecting anomalies in the visual pathway. See glaucoma; lens rim artifact; perimeter.
frequency doubling p. (FDP) A method of testing the visual field based on the frequency doubling illusion and thus assessing the functional integrity of the large-diameter retinal ganglion M cells, which are very susceptible to early glaucomatous damage. A commercial version of this method, which provides rapid and efficient visual field testing, is available (Humphrey Instruments/Welch Allyn). It is a computerized perimeter in which the stimulus display consists of a low spatial frequency (0.25 c/deg) sinusoidal grating which flickers in a counterphase fashion (i.e. light bars become dark and vice versa) at a rate of 25 Hz. The grating is presented in many locations throughout the visual field and the patient’s task is to detect it.
See glaucoma, open-angle; illusion, frequency doubling.
kinetic p. Measurement of the visual field with a moving target of fixed luminance.
short wavelength automated p. (SWAP)
A valuable procedure for detecting and monitoring visual defects in patients with ocular hypertension and patients with early glaucomatous visual field losses. It uses a blue stimulus on a yellow background, as may be arranged in an automated perimeter. It is a more sensitive and efficient method of detecting and monitoring early visual field losses than standard white-on-white automated perimetry (white stimulus on a white background).
See glaucoma, open-angle.
static p. Measurement of the visual field with a target that can be varied in dimension and luminance. The target can be presented in any part of the visual field.
period, critical A time after birth during which neural connections can still be modified by interference with normal visual experience or lesion of the visual pathway. If a person has an anomaly (e.g. amblyopia), the treatment is most likely to be effective during the earliest part of the critical period. In man it lasts up to about seven to eight years of age. If neural connections are impaired permanently during this period it will usually be impossible to repair later and the younger the child the more damaging it is. Example: binocularly sensitive cortical cells (stimulated by normal binocular vision) may never develop in uncorrected strabismus, or prolonged occlusion occurring during the critical period, especially before the age of three, and therefore the patient will not have binocular vision. Syn. plastic period. (However, this term relates more specifically to the time course during which the visual system is still responsive to treatment. This may differ from the critical period of development); sensitive period.
See myopia, form-deprivation; occlusion treatment.
periocular Situated around the eye.
perioptometry The measurement of the extent of the visual field or of peripheral visual acuity.
periorbita See orbit.
peripapillary Pertaining to the area surrounding the optic nerve head.
peripheral clearance See edge lift.
peripheral vision; visual acuity See under the nouns.
peripheral zone See optic zone diameter.
periphoria See cyclophoria.
periscope An optical instrument using two right angle reflectors in order to allow observation of an object from behind a shield or around an obstruction where direct vision is impossible. It has many applications, especially in the military forces (e.g. in tanks, submarines).
See lens, periscopic.
peristriate area See areas, visual association.
Perkins tonometer See tonometer, applanation.
Perlia’s nucleus See nucleus, Perlia’s.
persistent hyaloid artery See hyaloid remnant.
persistent hyperplastic primary vitreous
See vitreous, persistent hyperplastic primary.
persistent pupillary membrane See membrane, pupillary.
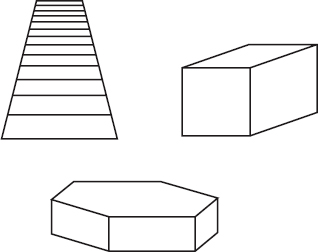
perspective One of the cues to perception of the third dimension induced by a graphic representation on a plane, as in a drawing, or as a monocular cue, such as aerial perspective or linear perspective. (Fig. P8).
See perception, depth.
aerial p . Perspective influenced by the state of clarity of the atmosphere. Far away objects appear less distinct and desaturated in colour due to the diffusion of light by the air in between the object and the eye. However, a very pure atmosphere may lead to underestimation of the distance of objects as they retain their distinctness and colour in this case. Aerial perspective is used by artists who soften and blur the colour and outlines of objects that they wish to appear as far away.
See shadow
geometrical p. See perspective, linear.
linear p. Perspective conveyed by drawing images in different sizes. For example, parallel lines receding into the distance are made to converge. (Fig. P8) Syn. geometrical perspective.
Peter’s anomaly A rare, congenital anomaly of the anterior segment of the eye. It is characterized by a central corneal opacity, usually accompanied by the adhesion of strands of iris tissue to the margins of the opacity, thinning of the stroma and attenuation or absence of Descemet’s membrane. A variant of Peter’s anomaly (called type 2) presents in addition to the above, either a displacement or a lack of transparency of the lens, which may even become adherent to the posterior surface of the cornea. It is frequently associated with glaucoma. Syn. anterior chamber cleavage syndrome.
See syndrome, Axenfeld’s; syndrome, Rieger’s.
Petit, canal of See canal of Petit.
Petzval surface The imaginary curved surface upon which images would be formed if curvature of field were the only aberration present. It is the curved surface in which the tangential and sagittal image shells of a point-focal lens coincide.
See astigmatism, oblique; curvature of field; lens, anastigmatic.
pH Symbol for the logarithm to base 10 of the reciprocal of the hydrogen (H) ion concentration measured in gram molecular weight in an aqueous solution. A solution with a pH 7.0 is neutral, one with a pH of more than 7.0 is alkaline, one with a pH lower than 7.0 is acid. It is a convenient way of expressing the acidity or alkalinity of solutions, particularly of contact lens buffer solutions. Alkaline ophthalmic solutions generally cause less discomfort than acidic ones. Note: pH stands for power (or potency) of H.
See acidosis.
phacocele Hernia of the crystalline lens through a rupture of the sclera near the limbus. It lodges underneath the conjunctiva. Syn. lenticele.
phacodonesis A tremulous condition of the crystalline lens. It usually results from an injury to the eye in which some or most of the zonular fibres are broken.
See iridodonesis.
phacoemulsification Procedure for removal of the crystalline lens in cataract surgery, which consists of emulsifying and aspirating the contents of the lens with the use of a low-frequency ultrasonic needle inserted into the eye near the limbus. This technique usually produces more rapid wound healing and early stabilization of refractive error with less astigmatism, due to the small incision. However, this technique may damage the corneal endothelium if excessive ultrasound is used. Following removal of the lens cortex and nucleus, an intraocular lens may be implanted within the remaining lens capsule. The lens is folded and inserted through a small incision (e.g. 3.2 mm) using a special injector. This procedure is preferred over other cataract extraction techniques due to both the rapid wound healing and the lower incidence of potentially vision threatening side effects (e.g. retinal detachment).
See after-cataract; biometry of the eye; cataract extraction; lens, intraocular; iridectomy.
phacolytic glaucoma See glaucoma, phacolytic.
phacoscope Instrument for observing the crystalline lens and measuring accommodative changes using the Purkinje–Sanson images, as in the ophthalmophakometer. See phakometer.
phagocytosis The process of ingestion of solid substances (e.g. cells, bacteria, parts of necrosed tissue) by cells and transported to a site within the cell where it is broken down by lysosomal enzymes.
phakic Refers to an eye possessing its crystalline lens or an intraocular lens implant.
See aphakia; eye, pseudophakic; lens, intraocular.
phakometer Optical instrument designed to measure the radii of curvature of the crystalline lens. The method is based on a comparison of the sizes of the third h’3 and fourth h’4 Purkinje images (typically determined by photography) with that of the first image h′1, that is the anterior corneal surface, the characteristics of which are easily measured. The radius of curvature of, say the fourth Purkinje image r′4 can be calculated using the approximate equation
where r1 is the radius of curvature of the front surface of the cornea. If the test object is near the eye a correction factor is necessary.
See image, Purkinje–Sanson; ophthalmophakometer; phacoscope.
phase The state of vibration of a light wave at a particular time. Light waves vibrating with the same frequency are said to be in phase if their peaks and troughs occur at the same time; otherwise they are said to be out of phase and one wave lags or precedes another by a phase difference (e.g. a fraction of a wavelength, or one wavelength, or a number of wavelengths). For waves exactly out of phase the phase difference is half a wavelength and for waves exactly in phase it is 0.
See interference; wavelength.
phenomenon 1. A remarkable event or appearance. 2. A fact or an occurrence that can be described or explained. Plural: phenomena.
Abney’s p. A slight change in hue resulting from a change in saturation. This is especially noticeable when white light is added to a monochromatic blue or green light.
Aubert’s p. If, in the dark the head is tilted slowly to one side while looking at a bright vertical line, this line will appear to tilt in the opposite direction. This phenomenon is due to the absence of compensatory postural changes. Syn. Aubert’s effect.
Aubert–Förster p. When targets (e.g. letters) of different sizes are placed peripheral to the foveal region and at different distances from the observer, visual acuity is better for the smaller targets nearer the observer than for the larger targets farther than the observer, although they subtend the same visual angle. Syn. Aubert–Förster law.
Bell’s p. An outward and upward rolling of the eyes when closing, or attempting to close the eyelids.
Bezold–Brücke p. A change in perceived hue of some spectral colours with a change in intensity. However, some wavelengths, such as 478, 503 and 578 nm, remain a constant hue with varying intensity. These are called invariant wavelengths or unique hues. Syn. Bezold–Brücke effect.
Bielschowsky’s p. In alternating hypertropia, occluding one eye leads to its rotation upward, and then placing a neutral density filter in front of the other eye gives rise to a downward movement of the occluded eye. See test, Bielschowsky’s phenomenon
Broca–Sulzer p. See effect, Broca– Sulzer.
Brücke–Bartley p. See effect, Brücke–Bartley.
crowding p. A difficulty or inability to discriminate small visual acuity tests when they are presented next to each other in a row, thus inducing contour interaction, whereas the same sized acuity symbols presented singly against a uniform background are resolved. Although this phenomenon may be experienced by normal patients, it is most often characteristic of amblyopic eyes and of people with reading difficulties. Syn. crowding effect.
See acuity, morphoscopic visual; amblyopia.
doll’s head p. Reflex movement of the eyes in a direction opposite to the direction of a rapid head turn, followed by a return towards the original position. These vestibular-elicited eye movements are aimed at maintaining fixation. The phenomenon can be used to assess the integrity of the vestibulo-ocular response system (doll’s head test). If the eye movements do not accord with the above, it may indicate a brainstem defect. Syn. doll’s eye sign.
entoptic p. See image, entoptic.
extinction p. A condition in which individual stimuli placed in the visual field are seen, but when the nasal field of one eye and the temporal field of the other eye are stimulated simultaneously the subject fails to see one of the stimuli. This condition is common following a stroke. Syn. pseudo-hemianopia.
See visual neglect.
Fick’s p. See Sattler’s veil.
jack-in-the-box p. When wearing very high positive lenses (e.g. in aphakia) there exists an area in the periphery situated between the outer extent of the field seen through the lens and the field beyond the edge of the lens, which is not seen (ring scotoma). This phenomenon refers to the disappearance and sudden reappearance of an object when the eye moves from the periphery to the centre passing over the ring scotoma. This phenomenon can be avoided by turning the head rather than the eye for peripheral viewing or by correcting with contact lenses. Modern aspheric lenses minimize this phenomenon as they have reduced peripheral power.
See field of view, real; scotoma, ring.
jaw-winking p. An abnormal condition associated with congenital ptosis, characterized by the elevation of the ptotic eyelid when the mouth is opened or the jaw is moved laterally to the side opposite to the ptosis. The eyelid droops again if the jaw maintains its new position or is closed. The condition often diminishes with time, otherwise surgery is the main treatment. Syn. Marcus Gunn phenomenon; Marcus Gunn jaw-winking syndrome.
Marcus Gunn p. See phenomenon, jaw-winking.
Mizuo’s p. The appearance of a golden brown colour of the retina as it adapts to light, in Oguchi’s disease. When adapted to darkness the fundus has the normal red appearance. Syn. Mizuo’s sign.
Pulfrich p. See stereophenomenon, Pulfrich.
Purkinje’s p. See Purkinje shift.
Riddoch p. Ability to perceive the motion of an object while being unable to detect any other features of that object, such as its colour or its form. This may occur in a scotomatous area of the visual field caused by a lesion somewhere in the visual pathway from the lateral geniculate body to the occipital and temporal cortex.
Troxler’s p. An image in the periphery of the retina tends to fade or disappear during steady fixation of another object. This phenomenon is rarely noticed due to the involuntary eye movements. When these are neutralized optically, as in stabilized retinal imagery, the phenomenon occurs readily even in central vision.
See movements, fixation; stabilized retinal image.
Uhthoff’s p. See Uhthoff’s symptom.
phenotype The observable characteristics (e.g. eye colour, height) of an individual that are the result of an interaction between the genes and the environment.
See expressivity; genotype
phenylephrine hydrochloride See alpha-adrenergic antagonist; mydriatic.
phi movement See movement, phi.
phlyctenulosis See keratoconjunctivitis, phlyctenular.
phoria Synonym for heterophoria as well as orthophoria.
phorometer An instrument for measuring heterophoria consisting usually of Maddox rods and rotary prisms mounted on a phoropter or trial frame.
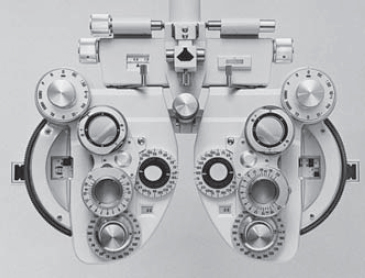
phoropter An instrument for measuring the ametropias, phorias and the amplitude of accommodation of the eyes. It consists of a large unit placed in front of the patient’s head in which there are three rotating discs containing convex and concave spherical and cylindrical lenses, as well as occluders, Maddox rods, pinholes, Polaroids, prisms and coloured filters. An attachment on the instrument allows sets of rotary prisms and cross-cylinders to be swung in front of each sight hole (Fig. P9). Syn. refracting unit; refractor; refractor head.
See Simultantest; trial case.
phosphene A visual sensation arising from stimulation of the retina by something other than light. The stimulation can be either electrical, mechanical (e.g. a blow to the head or pressure on the eyeball), or some electromagnetic waves such as X-rays.
See image, entoptic; photopsia; stimulus, adequate.
phosphorescence Luminescence that persists for some time after the exciting stimulus has ceased.
photic Pertaining to light or the production of light.
photocell Physical receptor that produces electric current when light is incident upon it. Syn. photoelectric cell.
photochemical Relating to a chemical change as a result of the absorption of light. Example: The action of light on rhodopsin in the photoreceptors of the retina.
See rhodopsin.
photochromatic interval See interval, photochromatic.
photochromatic lens See lens, photochromatic.
photocoagulation Process of changing blood and tissue from a fluid to a clotted state produced by the heat of an intense beam of light (e.g. laser), as used in the treatment or prophylactic treatment of retinal diseases (e.g. diabetic retinopathy, retinal detachments, retinal breaks, haemorrhages).
See laser; macular degeneration, age-related; retinal break; retinal detachment; retinopathy, diabetic.
photodynamic therapy See macular degeneration, age-related.
photoelectric Pertaining to the interaction between radiation and matter resulting in the absorption of photons and the consequent emission of electrons.
photokeratitis See keratoconjunctivitis, actinic.
photokeratoconjunctivitis See keratoconjunctivitis, actinic.
photokeratoscopy Determination of corneal curvatures and topography by photographing the corneal image of a target (usually black and white concentric rings) provided with the instrument. Measuring the size of the image and knowing the size of the object, it is possible to calculate the topography of the cornea. The theory is the same as that of the keratometer. A permanent photographic record is given with this method. The area of the cornea that is evaluated is much larger than with a keratometer.
See corneal topography; keratoscope; stereophotography; videokeratoscope.
photoluminescence See luminescence.
photometer An instrument for measuring the luminous intensity of a light source or a surface, by comparing it with a standard source. The comparison can be done either with the human eye (as in the Lummer–Brodhun or SEI exposure photometers) or with a photoelectric cell (as in the Pritchard photometer). Syn. illuminometer; luxometer. See illuminance; luminance.
flicker p . Visual photometer in which the observer sees a field illuminated alternately by two sources to be compared. When the sensation of flicker disappears, the intensity of the test source can be deduced by reading that of the reference standard source to which it is compared. For luminance difference, the frequency of alternation is chosen to be below the critical fusion frequency but for colour difference it is chosen above it.
See frequency, critical fusion.
Lummer–Brodhun p. A cube in which two adjacent or concentric portions of a comparison viewing screen are separately illuminated by the test source and a standard source. The instrument gives quite accurate readings when the two sources are of identical colour.
Macbeth p. Photometer using the Lummer–Brodhun cube, an eyepiece and a movable standard source illuminating a diffusing surface seen as an annulus by reflection within the cube. The portion of the source to be measured is seen through the cube as a spot within the annulus. The brightness of the annulus is adjusted until it matches that of the spot.
objective p. See photometer, physical.
physical p. A photometer employing a radiant energy sensitive element (e.g. a photoelectric cell, a thermopile) and an intensity indicator. Example: Pritchard photometer. Syn. objective photometer.
Pritchard p. See photometer, physical.
SEI exposure p.; subjective p. See photometer, visual.
visual p. A photometer in which the equality of brightness of a light source or a surface with a comparison standard source is made by visual observation. Examples: flicker photometer; Lummer–Brodhun photometer; Macbeth photometer; SEI photometer. Syn. subjective photometer.
photometry The measurement of light with a photometer.
Table P3
Common photometric units
luminous flux
lumens
luminous intensity (I)
candela = lumens/steradian
illuminance (E)
lux = lumens/m2
footcandle = lumens/ft2
luminance (L)
candela/m2
candela/ft2
footlambert
lambert
millilambert
1 footlambert (fL) = 3.426 cd/m2
1 lambert = 3183 cd/m2
1 millilambert = 3.183 cd/m2
1 candela/m2 = 0.2919 fL
1 candela/ft2 = 3.142 fL
See candela per square metre; flux, luminous; footcandle; footlambert; illuminance; intensity, luminous; lambert; luminance; millilambert; photometer.
photon The basic unit of radiant energy defined by the equation

where h is Planck’s constant (6.62 × 10–34 joule × second), v the frequency of the light and E the energy difference carried away by the emission of a single photon of light. The term photon usually refers to visible light whereas the term quantum refers to other electromagnetic radiations.
See theory, quantum; theory, wave; troland.
photonics Term referring to all the methods, procedures and systems used to measure, transmit or utilize light.
photophobia Abnormal fear or intolerance of light. It can be physiological, although it often accompanies inflammations of the anterior segment of the eye, especially anterior uveitis. It is also noted in patients with cone degeneration. Management is usually aimed at treating the primary cause (e.g. keratitis, uveitis), but in other cases (e.g. albinism, drug-induced mydriasis, recent aphakes, fear of light) tinted lenses will give relief.
See albinism; corneal abrasion; corneal erosion, recurrent; iritis; keratitis; monochromat; uveitis.
photophthalmia See keratoconjunctivitis, actinic.
photopic eye See eye, light-adapted.
photopic vision See vision, photopic.
photopigment Any pigment, such as the visual pigment found in the photoreceptors of the retina, which is altered by the absorption of light energy.
See pigment, visual; rhodopsin.
photopsia Hallucinatory perceptions such as sparks, lights or colours arising in the absence of light stimuli and observed when the eyes are closed. They occur often as a result of diseases of the optic nerve, retina (e.g. retinal and vitreous detachment) or the brain, migraine, or they can also occur with pressure upon the closed eye.
See floaters; flashes; retinitis, cytomegalovirus; spot, Fuchs’.
photoreceptor A receptor capable of reacting when stimulated by light, such as the rods and cones of the retina.
photorefraction A family of photographic techniques that provide a rapid, objective method of measuring the refractive error and accommodative response of the eye. Light emitted from a small flash source placed close to the camera lens is reflected from the eye and returned to the camera. Three methods have been developed: orthogonal, isotropic and eccentric (also called photoretinoscopy). The optical design of each method results in a specific photographic pattern, which varies with the degree to which the eye is defocused with respect to the plane of the camera. Photorefractive methods are not as accurate as retinoscopy but as they are entirely objective, much quicker and do not require prolonged fixation on the part of the patient, they are highly suited for testing infants and young children.
See optometer; refractive error; retinoscope.
photorefractive keratectomy See keratectomy, photorefractive.
photoretinoscopy See photorefraction.
photostress test See test, photostress.
phototransduction See transduction.
phototropism Reaction of certain plants and animals to move towards (positive phototropism) or away from (negative phototropism) a source of light.
phthiriasis Infestation of the eyelid margin by lice. It causes itching along the eyelid margin. Removal of the parasites is relatively easy either with forceps or by cryotherapy (removal under cold or freezing conditions).
phthisis bulbi Shrinkage and atrophy of the eyeball following a severe inflammation (e.g. uveitis), absolute glaucoma or trauma.
phthisis corneae Shrinkage and atrophy of the cornea following a severe inflammation of the cornea or trauma. It is associated with shrinkage of the globe.
phycomycosis A fungal infection caused by various microorganisms. These fungi may spread from the sinuses or the nasal tissue into the orbit, particularly in patients with diabetes, renal failure, malignant tumour or on steroid therapy. Therapy is aimed at the underlying disease, often accompanied by antifungal agents. Syn. zygomycosis.
physical optics See optics, physical.
physiological astigmatism; blind spot; cup; diplopia; optics; position of rest;
saline See under the nouns.
physostigmine A reversible anticholinesterase drug used as a parasympathomimetic which, when used in the eye constricts the pupil. It may be used in solution of 0.25–1% or ointment 0.25–0.50% in the treatment of glaucoma, but because of its side-effects its usage is rare nowadays. It is sometimes combined with pilocarpine. Syn. eserine.
See miotics; neostigmine; parasympathomimetic drug.
pia mater A delicate fibrous membrane closely enveloping the brain, spinal cord and the optic nerve. It terminates at the eye.
Pickford–Nicholson anomaloscope See anomaloscope.
Piéron’s law See law, Ricco’s.
Pigeon–Cantonnet stereoscope See stereoscope, Pigeon–Cantonnet.
piggyback lens See lens, piggyback.
pigment A coloured substance (e.g. haemoglobin, melanin) found in cells or tissue.
p. dispersion syndrome See syndrome, pigment dispersion.
p. epithelium See retinal pigment epithelium.
macular p. A yellow pigment, insensitive to light with a maximum absorption around 460 nm, and located in the inner layers of the macular area of the retina. It extends over an area of about 12° in diameter. Its density declines markedly with eccentricity. The major components of this pigment are the carotenoids: lutein and zeaxanthin. These yellow pigments absorb blue light maximally. The macular pigment has been thought to mitigate the effect of chromatic aberration and to protect the retina against short wavelength radiations. Moreover, lutein and zeaxanthin are antioxidants, which help protect the macula from oxidative stress, and larger plasma concentrations of these pigments may lower the risk of age-related macular degeneration.
See filter, red; macula lutea; oxidative stress.
visual p. Photosensitive pigment contained in the outer segments of both rods and cones. The chemical composition of the pigment in both cells is almost the same, there is only a slight difference in the protein opsin. The pigment in the rods is called rhodopsin. The cones contain three other types of pigments (one in each cone), which have spectral absorption curves with a maximum around 420, 530 and 560 nm. These three pigments form the basis of normal trichromatic colour vision. Syn. for cone visual pigments: cyanolabe, chlorolabe and erythrolabe, names sometimes used for the short-wave, middle-wave and long-wave sensitive cone pigments, respectively. Absorption of light by the visual pigments and the subsequent chemical changes that result in photoreceptor potentials represents the first stage in the visual process. Note: erythrolabe, meaning red pigment, has, in fact, its maximum spectral absorption around 560 nm, which is in the green-yellow portion of the visible spectrum.
See bleaching; cell, cone; cell, rod; colour vision, defective; densitometry, retinal; iodopsin; porphyropsin; rhodopsin; test, photostress; trichromatism; theory, Young–Helmholtz; transduction.
pigmentary glaucoma See glaucoma, pigmentary; syndrome, pigment dispersion.
pigmentary reaction of the retina See albinism; atrophy, gyrate; choroideremia; disease, Batten–Mayou; disease, Best’s; disease, Stargardt’s; dystrophy, cone; dystrophy, cone-rod; dystrophy, macular; dystrophy, pattern; fundus albipunctatus; fundus flavimaculatus; Leber’s congenital amaurosis; retinitis pigmentosa; syndrome, Bassen–Kornzweig; syndrome, Laurence– Moon–Bardet–Biedl; syndrome, Refsum’s; syndrome, Stickler’s; syndrome, Usher’s.
pilocarpine An alkaloid obtained from the leaves of Pilocarpus microphyllus and other species of Pilocarpus. It is a parasympathomimetic (direct-acting cholinergic) drug, which mimics the effect of acetylcholine causing miosis and accommodation. It counteracts sympathomimetic mydriatics. It is used in the treatment of glaucoma. Pilocarpine hydrochloride is most commonly applied to the eye as a 1% solution. Carbachol and bethanechol chloride are other parasympathomimetic drugs with similar effects to pilocarpine.
See parasympathomimetic drug; physostigmine.
pince-nez Eyeglasses without sides, held on the nose by tension from springs attached to the nose pads.
pincushion distortion See distortion.
pinealoma A tumour of the pineal body, a small glandular structure that lies between the two superior colliculi in a depression below the splenium of the corpus callosum. It may result in a loss of the pupil light reflex, vertical gaze palsy (especially in children), hydrocephalus, as well as a disturbance of the secretion of melatonin, which is related to the diurnal dark-light cycles.
Table P4
Cone pigments in normal and congenital dichromatic colour vision defects (excluding cases due to anomalies of the central visual pathway)
| colour vision | long-wave sensitive (around 560 nm) | middle-wave sensitive (around 530 nm) | short-wave sensitive (around 420 nm) |
| normal | present | present | present |
| protanope | absent or abnormal | present | present |
| deuteranope | present | absent or abnormal | present |
| tritanope | present | present | absent or abnormal |
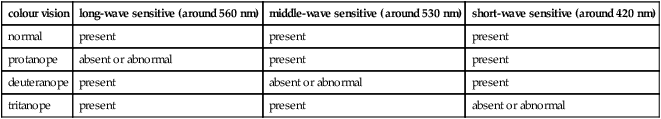
Syn. pineoblastoma. See nystagmus, convergence-retraction.
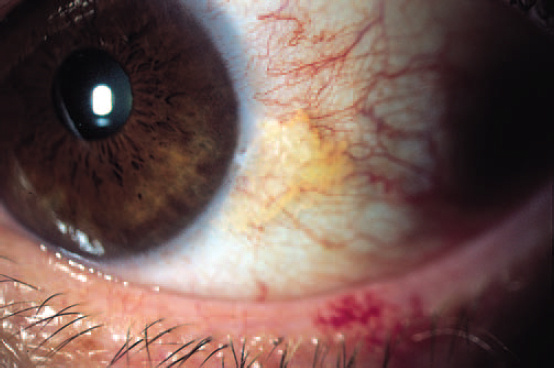
pinguecula A benign degenerative tumour of the bulbar conjunctiva that appears as a slightly raised, yellowish-white, oval shaped thickening on either side of the cornea, but usually the nasal side. Histologically, it consists of a deposition of hyaline substance. It becomes more common in elderly people, especially those exposed to high levels of ultraviolet radiation, wind and dust. Although benign, surgical excision may be requested for cosmetic reasons (Fig. P10).
See pterygium.
pinhole disc; spectacles See under the nouns.
pinhole test See disc, pinhole.
pink eye See conjunctivitis, contagious.
pit, optic A depression on each side of the end of the neural ectoderm (or neural tube) of the embryo. The pit deepens to form the optic vesicle. Syn. optic sulcus.
placebo A substance or a prescription (e.g. plano lenses) devoid of any physiological effect that is given merely to satisfy a patient. It is also used in research as a control against which the real effect of another product (similar in appearance) can be established.
See study, single-blind; trial, randomized controlled.
Placido disc See keratoscope.
Planck’s constant See photon.
Planck’s law See law, Planck’s.
plane A flat surface.
aperture p. A plane that passes through the aperture of an optical system.
apparent frontoparallel p. (AFPP) Plane passing through the fixation point and containing all other points judged to appear in the same frontal plane. At about 1 metre from the eye it more or less coincides with a frontal plane; this is the abathic distance. Closer to 1 metre it is often a concave surface with its concavity turned towards the observer and beyond 1 metre it is a convex surface with its convexity turned towards the observer.
See deviation, Hering–Hillebrand; horopter.
cardinal p’s. Planes, normal to the optical axis, which pass through the cardinal points of a lens or optical system. They are the focal planes, the nodal planes and the principal planes. (Sometimes, this definition also includes the object and image planes.)






