Oxygen transport
Normal oxygen transport
The total blood oxygen content is the sum of the dissolved oxygen and that bound to haemoglobin. Only a small fraction (2%) of the total oxygen in blood is in solution, and this dissolved oxygen is directly proportional to the arterial PO2. The arterial PO2 is also an important factor affecting the amount of oxygen that is bound to haemoglobin, as oxyhaemoglobin. The relationship is shown in the oxygen–haemoglobin dissociation curve (Fig 23.1).
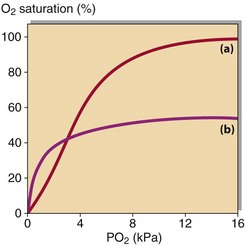
Fig 23.1 Dissociation curves – the relationship between PO2 and oxygen binding to haemoglobin. (a) The normal oxygen haemoglobin dissociation curve. (b) The effect of 50% CO.
Measurement of blood oxygen saturation, the percentage of the total haemoglobin present as oxyhaemoglobin, may be used to assess the ability of blood to carry oxygen to the tissues. This clearly depends on the relative amounts of both oxygen and haemoglobin, as well as their ability to bind together. Delivery of oxygen to the tissues also depends on blood flow, which is in turn influenced by other factors (Table 23.1).
When arterial PO2 is high (above 10 kPa), the blood haemoglobin is almost fully saturated with oxygen and measurements of oxygen saturation are not normally required. Indeed, measurements of oxygen saturation are not widely available outside of intensive therapy units. In patients exposed to carbon monoxide following smoke inhalation, the PO2 may give a misleading indication of the amount of oxygen being carried in the blood because carbon monoxide binds to haemoglobin with greater affinity than does oxygen (Fig 23.1).
Respiratory failure
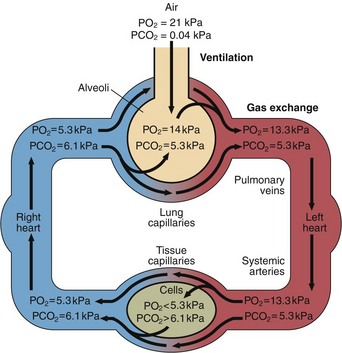
Figure 23.2 shows how the partial pressures of oxygen and carbon dioxide change as blood flows to the tissues and returns to the lungs. The mechanical process of moving air into and out of the respiratory tract is called ventilation. Carbon dioxide diffuses through alveolar membranes much more efficiently than oxygen, even though there is only a small pressure gradient. The PCO2 of arterial blood is thus identical to the PCO2 within the alveoli, and the arterial PCO2 is therefore a measure of alveolar ventilation. If ventilation is impaired, alveolar PO2 falls and alveolar PCO2 rises. Arterial blood reflects these changes. The main chemical stimuli to ventilation are shown in Table 23.2.
Table 23.2
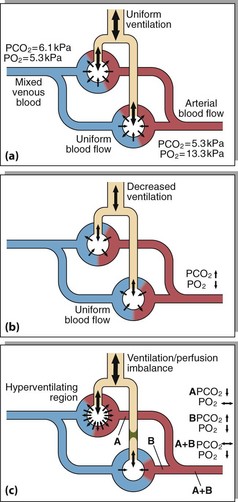
It is possible to calculate the alveolar–arterial PO2 gradient to determine the extent of defective gas exchange (Fig 23.3), but in practice it is rarely necessary to do this.
Ventilation/perfusion imbalance
In patients with a lobar pneumonia, some of the blood perfusing the lungs does not come into contact with functional alveoli and retains its carbon dioxide, and is not oxygenated. In blood reaching other parts of the lungs, gas exchange takes place efficiently. Arterial blood is a mixture of that exiting both regions. The increased PCO2 stimulates ventilation and ensures that the functioning alveoli are worked harder to restore PCO2 to normal. The blood gas results will show normal or even low PCO2 as a result of this hyperventilation (Fig 23.4). However, increased ventilation cannot dramatically raise alveolar PO2 as long as the patient is breathing air.