2 Overcoming medication errors in paediatric emergencies
Potential sources of medication errors
Doctors and nursing staff members who are not experienced in paediatric emergency medicine or the management of paediatric emergencies are especially at risk of making medication-related errors (see Table 2.1 for a breakdown of the types of errors that may lead to incorrect administration of a medication). Studies have shown that 10% to 15% of paediatric medication orders are erroneous, and that nearly one third of medication errors lead to harm in children. The potential for harm is higher in smaller children and infants and in the critically ill or injured, possibly because of the administration of multiple medications, limited time to double-check doses and altered pharmacokinetics and pharmacodynamics resulting from the physiological insults.
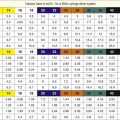
Table 2.1 Types of error that may be incurred in the administration of medications
| Type of error | Nature of error |
|---|---|
| Knowledge errors |
• Body weight not measured accurately.
• Inaccurate prediction method employed.
• Incorrect dose calculation – arithmetical errors.
• Incorrect dose dilution – wrong mass or volume of drug or diluent.
• Incorrect calculation of volume of dilution to administer.
• Incorrect volume administration.
• Incorrect weight type used for dose calculation – total body weight/lean body weight/ideal body weight (this has not yet been established in children).
• Inherent variability of drug content in manufacturer’s packaging (ampoule or vial). This is normally required to be within 10 to 15% of the stated mass of drug. For example, an ampoule of adrenaline 1 mg may contain anything between 0.9 mg and 1.15 mg of adrenaline. This consequently may lead to up to a 15% error in drug dose delivery.
• Complications related to drug preservatives, vehicles or diluents: the paucity of IV drug preparations designed for children has many unfortunate complications.
1. First obtain the correct milligram per kilogram dose either from memory (which may be very unreliable) or from appropriate reference material, and then determine if any age or physiology-related adjustments need to be made. Drug dose recommendations in children are generally based on body weight (or occasionally body surface area) and therefore appropriate drug administration requires an accurate measured or estimated body weight and a dose calculation, dilution and delivery that are free of errors. Not surprisingly, the most common medication errors in children in the ED are dosing errors, which can originate at any stage of the process – calculation, prescription, preparation or administration.
2. This base dose then needs to be converted to an actual total dose calculated from the patient’s body weight. Ideally, body weight should be measured for drug dose calculations. In practice it is often impossible to measure weight in children who are critically ill or injured and undergoing resuscitative treatment. Estimates of the patient’s weight by healthcare workers are notoriously inaccurate, but estimates of the child’s weight by the parents are often very accurate, and acceptable to be used in an emergency situation. Alternative methods, if parents do not accompany the child, include length-based prediction methods such as the PAWPER tape, the derived weight estimation method or the Broselow® tape. The prediction of weight in the ED, and the determination of which form of weight to use for drug calculations (lean body weight, ideal body weight, adjusted body weight or total body weight) has been dealt with elsewhere in this book.
3. Once the weight has been determined, the total dose to be administered needs to be calculated. This simple arithmetic exercise has been shown to be very poorly performed even by experienced doctors, and order of magnitude (tenfold) errors in drug doses calculations are common in children.
4. This dose, once calculated, must be communicated to the staff member who will prepare the drug for administration. This most commonly occurs via a verbal instruction or a handwritten prescription. Misunderstandings are frequent following verbal instructions. Illegible handwriting, incorrect positioning of the decimal point, transcription errors and mental lapses (such as using milligrams instead of micrograms inappropriately) are common causes of errors. Computerized systems are not immune from error either.
5. Once the drug order has been given, the drug must be correctly prepared, diluted and administered by the nurse or doctor. This process also requires the calculation of the millilitre volume of drug dilution to administer and is susceptible to error, especially in inexperienced hands. The wrong amount of drug, the wrong type or volume of diluent and the wrong volume administered to the patient are additional causes of errors.
Solutions and interventions to reduce medication errors
Any error-reduction system should focus on two important aspects:
• A reduction in preventable adverse events related to medications.
• A holistic approach to eliminating any potential sources of error that may occur during medication administration, rather than a system that focuses on the doctor. The system should assist the doctor, the nurse and the pharmacist from the process of prescription to the administration of the drug to the patient.
• Errors that do occur should be regarded as ‘system errors’ and not ‘personal errors’. This empowers individuals to report errors that do occur and allows the system to be improved. An appropriate (efficient and impartial) medication error reporting and analysis process should be established to produce information which can be used to improve the system.
• The availability of paediatric formularies and paediatric-specific reference materials in the ED, including internet access, is strongly recommended.
• Involve a pharmacist as part of the resuscitation team, if possible, to assist with the emergency medication administration process.
• The approach to the resuscitation of the paediatric patient should be pre-planned and standardized, both in the general emergency medicine management and the specific medication administration system. The entire process should be kept as simple as possible. The drug administration process in emergencies must be designed with a reduced reliance on calculations, both by the doctor and the nurse.
• Part of the approach to paediatric resuscitation should include an emphasis on teamwork with open communication. Many medication errors are intercepted before reaching the patient as a result of effective teamwork. Good communication has been identified as having an important role in reducing medication errors. Resuscitation aids should be available for all members of the team.
• Reduce the cognitive load during paediatric emergencies. Resuscitation aids have been shown to reduce patient harm through decreasing critical-thinking time spent on drug dose calculations and increasing critical-thinking time used for patient management. The ideal resuscitation aid is complete (it provides information on the patient’s weight, appropriate equipment sizes and complete drug dose information from dose to dilution to volume of administration (see below)), it is easy to use and is resilient (it can perform well under suboptimal conditions). The Broselow® tape on its own does not fulfil these conditions, but must be used with additional drug dose reference material.
• Ensure that doctors involved in the emergency care of children are appropriately trained in paediatric emergency medicine, receive continual proficiency training in resuscitation and are familiar with the use of the available resuscitation aids. Similarly, nurses should also have appropriate education and ongoing training.
• Computerized physician order entry systems, computer-based dose reference programs or web-based systems should be used if available. These have been introduced in the United States and have been shown to reduce drug dosing errors in the resuscitation situation. They are expensive, however, and many hospitals throughout the world will never have access to these systems. If present, technology should be used judiciously as it is not error-free, and alternatives should be available in the event of technology or power failure.
• Paper-based charts and tables (pre-printed medication order forms or ideally pre-printed forms containing complete drug dose information) have also been shown to improve the accuracy of medication prescription and delivery in children. These materials should be able to provide the team with the drug dose, the required dilution, and the volume of drug-dilution to administer, without any calculation or arithmetic required. Reference materials should also be ‘bed-based’ and not ‘provider-based’. They should be available to all members of the resuscitation team and not just a single individual. This will decrease the risk for errors for both doctor and nurse, and facilitate cross-checking and double-checking of doses and volumes. Pre-printed weight-specific charts have the further benefit of accommodating additional information such as age-specific changes in dose recommendations (e.g. suxamethonium: 3 mg/kg in infants, 2 mg/kg in children, 1.5 mg/kg in adults).
• Part of the standardized approach to the resuscitation of children must include references for a number of methods of estimating body weight, including a length-based weight estimation method (e.g. the PAWPER tape or Broselow® tape). Age-based formulas are useful when tapes are unavailable, but are not as accurate as the length-based systems. Body weight should be obtained early and this weight used for further calculations.
• Avoid verbal prescriptions if possible as they are associated with a high error rate. Written prescriptions should be legible, avoid abbreviations, trailing zeros (5.0 milligrams) and ‘naked decimal points’ (.5 micrograms).