Struma Ovarii
Synonyms/Description
Etiology
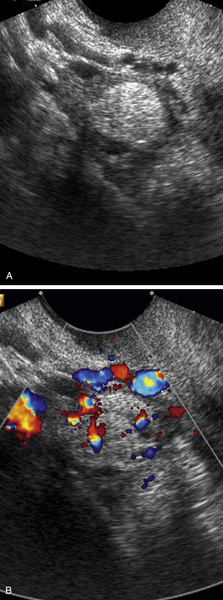
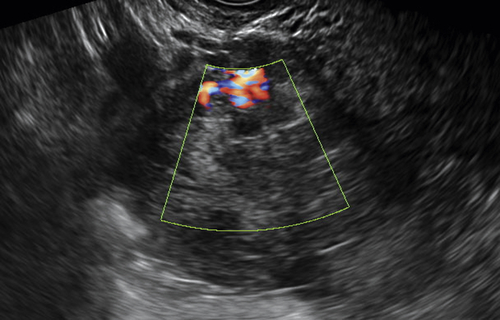
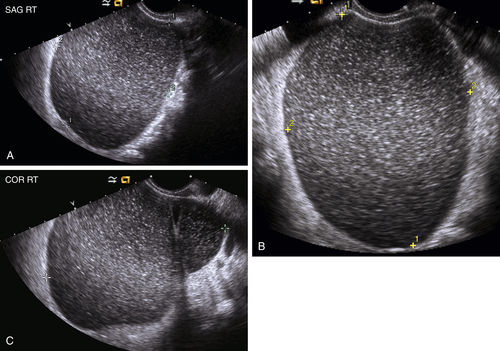
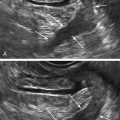
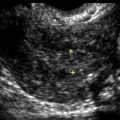
Ultrasound Findings
Differential Diagnosis
Clinical Aspects and Recommendations
Figures
Suggested Reading
Coyne C., Nikiforov Y.E. RAS mutation-positive follicular variant of papillary thyroid carcinoma arising in a struma ovarii. Endocr Pathol. 2010;21:144–147.
Doganay M., Gungor T., Cavkaytar S., Sirvan L., Mollamahmutoglu L. Malignant struma ovarii with a focus of papillary thyroid cancer: a case report. Arch Gynecol Obstet. 2008;277:371–373.
Manini C., Magistris A., Puopolo M., Montironi P.L. Cystic struma ovarii: a report of three cases. Pathologica. 2010;102:36–38.
Saba L., Guerriero S., Sulcis R., Virgilio B., Melis G., Mallarini G. Mature and immature ovarian teratomas: CT, US and MR imaging characteristics. Eur J Radiol. 2009;72:454–463.
Zalel Y., Seidman D.S., Oren M., Achiron R., Gotlieb W., Mashiach S., Goldenberg M. Sonographic and clinical characteristics of struma ovarii. J Ultrasound Med. 2000;19:857–861.