Polycystic Ovaries
Synonyms/Description
Polycystic ovarian syndrome (PCOS)
Stein-Leventhal syndrome
Etiology
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder in women of reproductive age, occurring in 4% to 6% of the female population. PCOS is a complex of symptoms often associated with obesity, type 2 diabetes, metabolic syndrome, and infertility. Historically there had been a lack of consensus regarding the features that define PCOS. In 2003 a consensus statement was developed between the European and American reproductive societies, known as the Rotterdam criteria, which standardized the definition of PCOS. The diagnosis requires two of the following three findings: (1) oligo-ovulation or anovulation, (2) clinical or biochemical signs of hyperandrogenism, (3) polycystic ovaries on ultrasound. It is important to note that the sonographic appearance of the ovaries is not always required for this diagnosis. The Rotterdam criteria clarify the difference between polycystic ovaries (PCO), which is a diagnostic finding, and PCOS, which is a diagnosis affecting multiple organ systems.
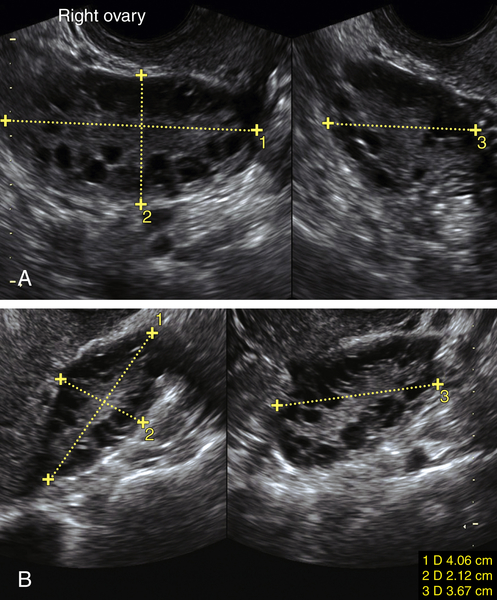
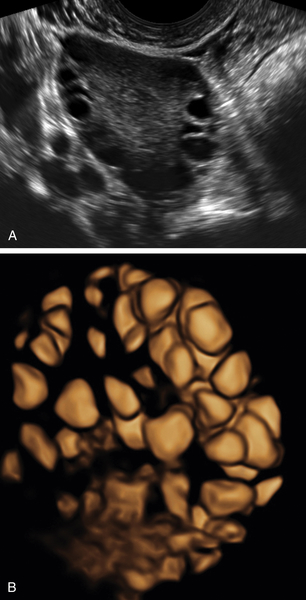
Ultrasound Findings
The Rotterdam sonographic definition of a PCO is the presence of either 12 or more follicles measuring 2 to 9 mm in diameter or an ovary that has an increased ovarian volume defined as greater than 10 cm3 (ovarian volume is calculated using simplified formula for prolate ellipsoid = 0.5 × length × width × thickness). Only one ovary with these findings is required with the following two exceptions.
This definition does not apply to women taking oral contraceptives.
If there is evidence of a dominant follicle (greater than 10 mm) or a corpus luteum on either ovary, the scan does not meet sonographic definition of PCO. Guidelines recommend the scan be repeated at another time (during ovarian quiescence or in the next cycle).
Differential Diagnosis
There is no differential diagnosis for a polycystic ovary when using the Rotterdam sonographic definition earlier on this page. Oral contraceptives can make the ovaries appear polycystic, and normally functioning ovaries can also appear polycystic. The ultrasound definition is limited to the appearance of the ovaries. It is important to take a clinical history in addition to the ultrasound findings so as not to overdiagnose PCOS. For example, many adolescent women have irregular menses because their hypothalamic-pituitary-ovarian axis has not yet matured, and they may have many small follicles.
Clinical Aspects and Recommendations
Ultrasound findings alone are not sufficient to diagnose or exclude PCOS in the absence of clinical information. Between 16% and 25% of the normal population have multicystic ovaries on ultrasound, but only 4% to 6% of women have polycystic ovarian syndrome. Conversely, when ultrasound reveals normal-appearing ovaries in a patient with oligo-ovulation or anovulation and hyperandrogenism, PCOS should be included in the differential diagnosis.
Patients with PCOS who are overweight should be encouraged to lose weight through diet and exercise. Drug therapies such as oral contraceptives or metformin can help with the symptoms of PCOS. PCOS may increase the risk for endometrial cancer, especially in patients with prolonged amenorrhea, because of equally long episodes of unopposed estrogen.
Suggested Reading
Balen A.H., Laven J.S.E., Tan S.L., Dewailly D. Ultrasound assessment of the polycystic ovary: international consensus definitions. Hum Reprod Update. 2003;9:505–514.
Polson D.W., Wadsworth J., Adams J. Polycystic ovaries: a common finding in normal women. Lancet. 1988;1:870–872.
Wilson J.F. In the clinic. The polycystic ovary syndrome. Ann Intern Med. 2011(154):3 ITC2-2-ITC2-15.