Ovarian Tumor Debulking
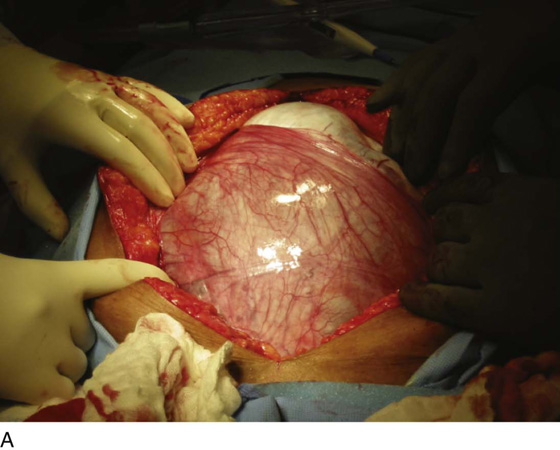
Ovarian cancer is a surgically staged disease, and most cases are advanced stage III or IV at the time of initial diagnosis. The cornerstone of therapy for ovarian cancer is maximal surgical cytoreduction, or tumor debulking, surgery. Ovarian cancer is thought to spread by contiguous growth and by dissemination through the lymphatics. Once the cancer has reached the external surface of the ovary, the cells exfoliate and implant inside the abdominal-pelvic cavity, causing peritoneal disease. Once ovarian cancer has disseminated, it tends to grow on the lining of the peritoneum and on the outside of the viscera in the abdomen and pelvis. Once outside the ovary, this malignancy has a predilection to metastasize to the deep portions of the anterior and posterior cul-de-sacs, the surface of the diaphragm (especially the right side), and the omentum, including both infracolic and gastrocolic portions. Additionally, ovarian cancer is found to involve the surfaces of the large and small bowel and its mesentery, the spleen, the liver, and the stomach. Approximately one fourth of cases of ovarian cancer are confined to the ovary. It is of paramount importance to completely surgically stage these cases at the time of diagnosis so that the appropriate treatment can be given. Surgery for an undiagnosed pelvic mass or a presumed ovarian cancer customarily begins with a vertical midline skin incision (Fig. 28–1A–D). This approach allows for removal of the mass or ovary (especially if it is large) and, more important, for maximal exposure of the abdominal-pelvic cavity, so that a thorough exploration can be performed. The incision usually is started at the level of the pubic symphysis and is extended cephalad. It can be extended all the way to the xyphoid process if necessary.
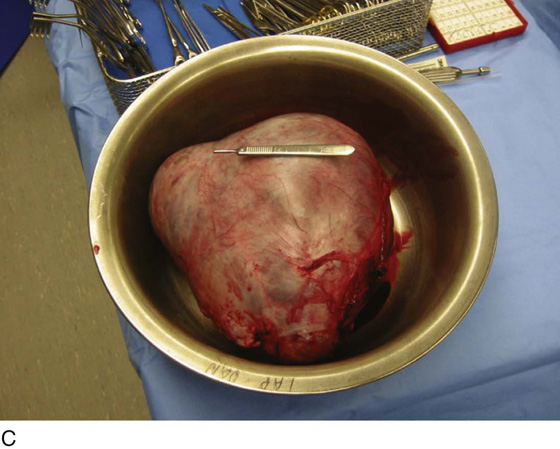
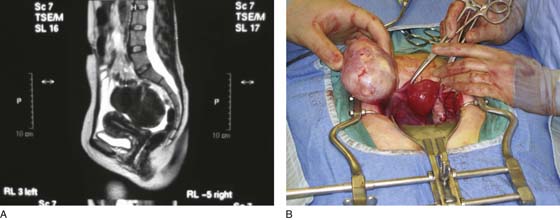
In a minority of cases, ovarian cancer can be confined to the ovary, and a “conservative staging procedure” can be performed (Fig. 28–2A, B). A conservative staging procedure consists of unilateral adnexectomy, pelvic washings, peritoneal biopsies, omentectomy, and lymph node dissection (usually to include pelvic and para-aortic areas; Fig. 28–3A, B). This conservative staging technique should be limited to children, adolescents, and women of childbearing years whose malignancy is grossly confined to one ovary.
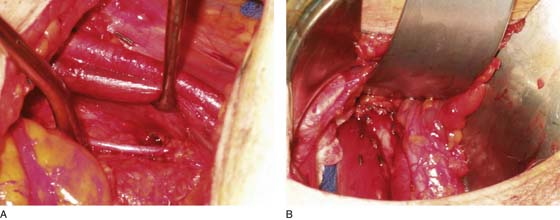
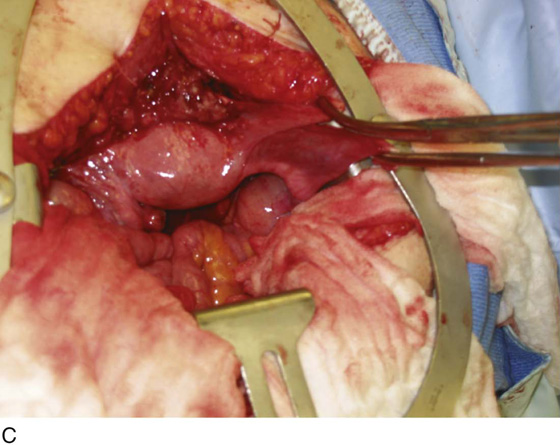
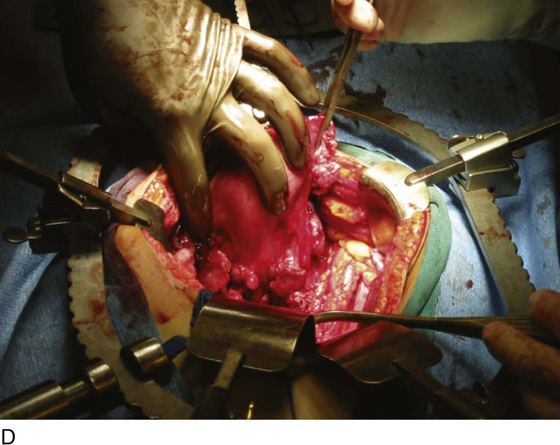
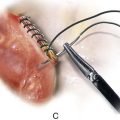
To date, no accurate screening test has been developed for ovarian cancer; therefore most ovarian cancers have spread into the abdominal-pelvic cavity by the time of diagnosis (Fig. 28–4A–D). The goal of surgical treatment in these cases is maximal tumor debulking, also termed surgical cytoreduction. This usually consists of total abdominal hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and tumor debulking. Additionally, ascites, if present, is removed as a component of this surgery. When gross bulky disease is found outside the abdomen, removal of lymph node tissue is usually reserved for those cases in which lymph nodes contain bulky disease. Often the omentum is a site of metastatic disease (Fig. 28–5). Commonly, most cases of metastatic disease for ovarian cancer are found in the omentum (Figs. 28–6A, B and 28–7A, B).
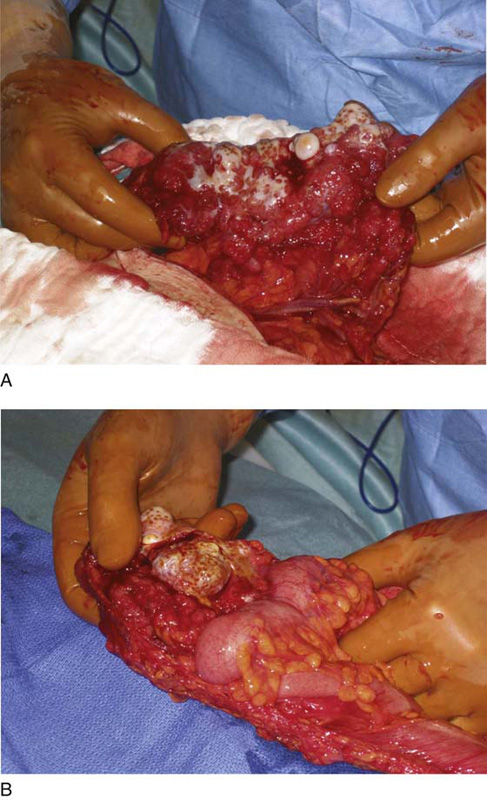
Optimal tumor debulking (defined as no residual disease = 1 to 2 cm at the conclusion of the surgery) provides a survival advantage to patients with ovarian cancer. Optimal tumor debulking often can involve surgery on such organs as bowel, bladder, liver, and spleen (Fig. 28–8). The concept of decreasing residual tumor burden is thought to make postoperative adjuvant therapy most effective. This correlates with a survival advantage in patients who undergo optimal tumor debulking for ovarian cancer.
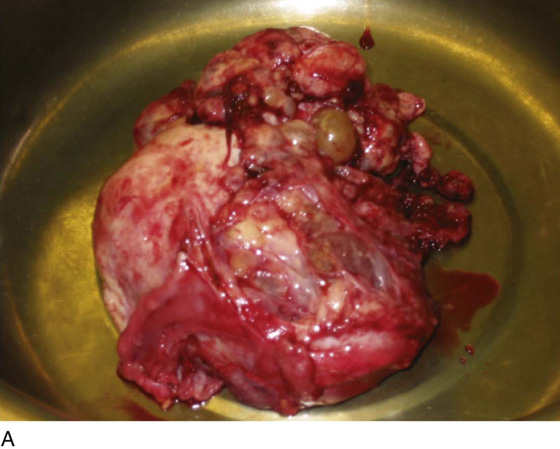
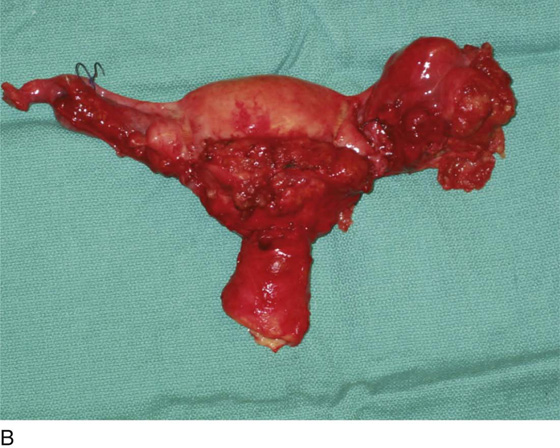
FIGURE 28–1 A. The right ovary is markedly enlarged and contains an adenocarcinoma. The right fallopian tube and mesosalpinx can be seen draping over the lower three quarters of the ovary. The vertical midline skin incision extends from the symphysis pubis to up above the umbilicus and provides adequate exposure in this case. B. The large ovarian mass has been delivered through the vertical midline skin incision. C. The adenocarcinoma of the right ovary measures 20 × 15 × 8 cm. D. Most of the right ovary was fluid-filled, but it did contain multiple thick septations and the adenocarcinoma of the ovary, which consisted of mixed serous and mucinous subtypes.
FIGURE 28–2 A. This preoperative magnetic resonance image (MRI) of the pelvis shows an ovarian mass clearly distinct from the bladder, the uterus, and the rectosigmoid colon. B. Ovarian cancer is confined to the left ovary, and a normal uterus and right ovary can be seen. Conservative staging can be employed in this case.
FIGURE 28–3 A. A pelvic lymph node dissection has been performed. The external iliac artery and vein have been stripped of all lymph node tissue and are being gently retracted by a vein retractor to expose the obturator nerve. The obturator lymph node pad has also been removed to expose the obturator internus muscle and the pelvic sidewall. B. A right-sided para-aortic lymph node dissection has been performed. Surgical clips can be seen on the surface of the psoas major muscle and the inferior vena cava. Medial to the inferior vena cava, the aorta can be seen as well as the ureter.
FIGURE 28–4 A. A cancerous ovary with extensive gross disease on its surface. B. The contralateral ovary and posterior uterine serosa contain gross metastatic disease. C. Extraovarian disease along the vesicouterine peritoneum causing obliteration of the anterior cul-de-sac. D. Extraovarian disease involving the posterior cul-de-sac.
FIGURE 28–5 Small metastatic implants of an ovarian malignancy can be seen throughout the omentum.
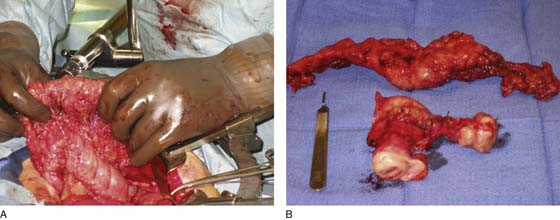
FIGURE 28–6 A. Metastatic ovarian cancer with omental caking involving the infracolic omentum. Metastatic tumor implants can be seen along the tinea coli of the transverse colon. B. A left ovary, uterus, cervix, and omentum depicting a left-sided ovarian cancer with metastatic disease along the anterior uterine serosa and in the omentum. Most of the disease is contained in the omentum.
FIGURE 28–7 A. A case of metastatic ovarian cancer replacing the omentum. B. An omental cake is shown firmly adherent to the transverse colon.
FIGURE 28–8 A portion of omentum with metastatic ovarian cancer that was firmly adherent to a portion of small bowel. To accomplish optimal tumor debulking, the portion of small bowel adherent to the omental cake was resected and a bowel reanastomosis was performed.