Chapter 38 Outcome Measurements for Minimally Invasive Percutaneous Spine Techniques
Back-specific function measures
BOX 38-1 Selected Back-Specific Functional Instruments
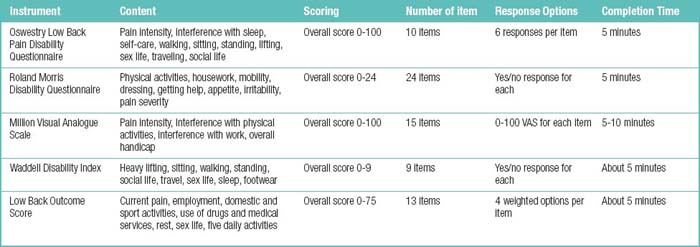
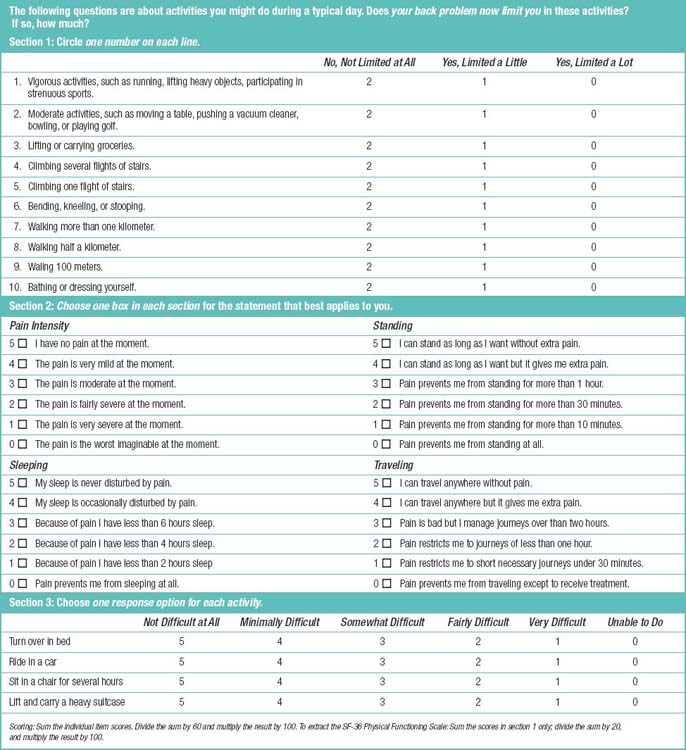
Oswestry Low Back Pain Disability Questionnaire (ODQ)
Roland Morris Disability Questionnaire (RMDQ)
Million Visual Analogue Scale (MVAS)
Waddell Disability Index (WDI)
Clinical Back Pain Questionnaire (CBPQ; Aberdeen Low Back Pain Scale)
Low Back Pain Rating Scale (LBPRS)
Quebec Back Pain Disability Scale (QBPDS)
North American Spine Society Lumbar Spine Questionnaire (NASS LSQ)
Resumption of Activities of Daily Living Scale (RADL)
Scoring System for Low Back Pain Proposed by Japanese Orthopaedic Association (JOA)
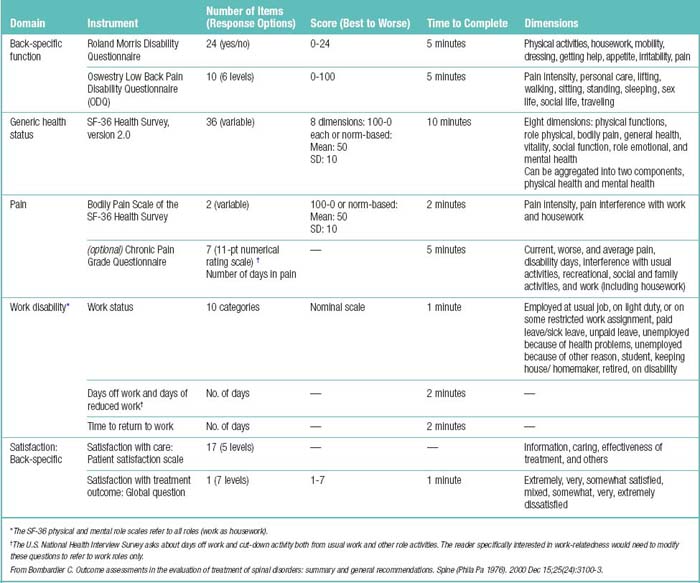
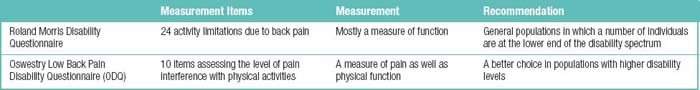
Table 38.3 Comparison between Roland Morris Disability Questionnaire and Oswestry Low Back Pain Disability Questionnaire (ODQ)
BOX 38-3 Oswestry Low Back Pain Disability Questionnaire (ODQ) [2]
Section 3: Lifting
 Pain prevents me from lifting heavy weights off the floor but I can manage if they are conveniently positioned, e.g., on a table.
Pain prevents me from lifting heavy weights off the floor but I can manage if they are conveniently positioned, e.g., on a table.Section 9: Social Life
Table 38.4 Scoring System for Low Back Pain Proposed by Japanese Orthopaedic Association (Maximum 15 Points)
| Subjective Symptoms (Maximum 9 Points) | |
Data from Subcommittee on Low Back Pain and Cervical Myelopathy Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association, Japan. Japanese Orthopaedic Association Back Pain Evaluation Questionnaire. Part 3. Validity study and establishment of the measurement scale. Journal of Orthopaedic Science. 2008; 13(3): 173-179. 5-0 is muscle strength rating with 5 as normal and 0 as no contraction.
Pain
Table 38.6 The Strengths and Weaknesses of Alternative Measures of Pain Intensity
| Scale | Strengths | Weakness(es) |
|---|---|---|
| Verbal Rating Scale (VRS) |
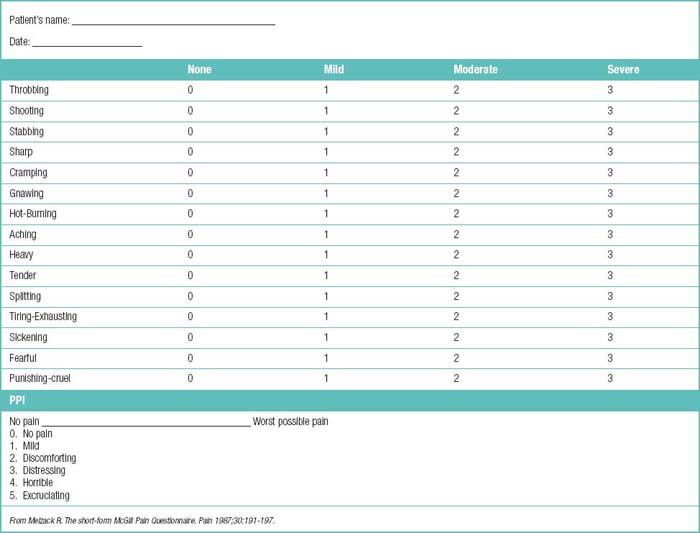
Table 38.7 McGill Pain Questionnaire
| What Does Your Pain Feel Like? |
|---|
| Statement: Some of the following words below describe your present pain. Circle ONLY those words that best describe it. Leave out any category that is not suitable. Use only a single word in each appropriate category – the one that applies best. |
| Group | Descriptor | Points |
|---|---|---|
| 1 (temporal) | flickering | 1 |
| quivering | 2 | |
| pulsing | 3 | |
| throbbing | 4 | |
| beating | 5 | |
| pounding | 6 | |
| 2 (spatial) | jumping | 1 |
| flashing | 2 | |
| shooting | 3 | |
| 3 (punctate pressure) | pricking | 1 |
| boring | 2 | |
| drilling | 3 | |
| stabbing | 4 | |
| lancinating | 5 | |
| 4 (incisive pressure) | sharp | 1 |
| cutting | 2 | |
| lacerating | 3 | |
| 5 (constrictive pressure) | pinching | 1 |
| pressing | 2 | |
| gnawing | 3 | |
| cramping | 4 | |
| crushing | 5 | |
| 6 (traction pressure) | tugging | 1 |
| pulling | 2 | |
| wrenching | 3 | |
| 7 (thermal) | hot | 1 |
| boring | 2 | |
| scalding | 3 | |
| searing | 4 | |
| 8 (brightness) | tingling | 1 |
| itchy | 2 | |
| smarting | 3 | |
| stinging | 4 | |
| 9 (dullness) | dull | 1 |
| sore | 2 | |
| hurting | 3 | |
| aching | 4 | |
| heavy | 5 | |
| 10 (sensory miscellaneous) | tender | 1 |
| taut | 2 | |
| rasping | 3 | |
| splitting | 4 | |
| 11 (tension) | tiring | 1 |
| exhausting | 2 | |
| 12 (autonomic) | sickening | 1 |
| suffocating | 2 | |
| 13 (fear) | fearful | 1 |
| frightful | 2 | |
| terrifying | 3 | |
| 14 (punishment) | punishing | 1 |
| grueling | 2 | |
| cruel | 3 | |
| vicious | 4 | |
| killing | 5 | |
| 15 (affective-evaluative- sensory: miscellaneous) | wretchedblinding | 12 |
| 16 (evaluative) | annoying | 1 |
| troublesome | 2 | |
| miserable | 3 | |
| intense | 4 | |
| unbearable | 5 | |
| 17 (sensory: miscellaneous) | spreading | 1 |
| radiating | 2 | |
| penetrating | 3 | |
| piercing | 4 | |
| 18 (sensory: miscellaneous) | tight | 1 |
| numb | 2 | |
| drawing | 3 | |
| squeezing | 4 | |
| tearing | 5 | |
| 19 (sensory) | cool | 1 |
| cold | 2 | |
| freezing | 3 | |
| 20 (affective-evaluative: miscellaneous) | naggingnauseating | 12 |
| agonizing | 3 | |
| dreadful | 4 | |
| torturing | 5 | |
| Pain score = SUM (points for applicable descriptors) | ||
| How Does Your Pain Change with Time? | ||
|---|---|---|
| Question | Response | Points |
| Which word or words would you use to describe the pattern of your pain? | continuous, steady, constantrhythmic, periodic, intermittent | 12 |
| brief, momentary, transient | 3 | |
| Do the following items increase or decrease your pain? |
|---|
| How Strong is Your Pain? | ||
|---|---|---|
| Statement: People agree that the following 5 words (mild, discomforting, distressing, horrible, excruciating) represent pain of increasing intensity. To answer each question below write the number of the most appropriate word in the space beside the question. |
| Question | Response | Points |
|---|---|---|
| Which word describes your pain right now? | mild | 1 |
| discomforting | 2 | |
| distressing | 3 | |
| horrible | 4 | |
| excruciating | 5 | |
| Which word describes it at its worst? | mild | 1 |
| discomforting | 2 | |
| distressing | 3 | |
| horrible | 4 | |
| excruciating | 5 | |
| Which word describes it when it is least? | mild | 1 |
| discomforting | 2 | |
| distressing | 3 | |
| horrible | 4 | |
| excruciating | 5 | |
| Which word describes the worst toothache you ever had? | mild | 1 |
| discomforting | 2 | |
| distressing | 3 | |
| horrible | 4 | |
| excruciating | 5 | |
| Which word describes the worst headache you ever had? | mild | 1 |
| discomforting | 2 | |
| distressing | 3 | |
| horrible | 4 | |
| excruciating | 5 | |
| Which word describes the worst stomach- ache you ever had? | mild | 1 |
| discomforting | 2 | |
| distressing | 3 | |
| horrible | 4 | |
| excruciating | 5 | |
| Interpretation: | ||
Adapted from Melzack R. The McGill pain questionnaire: major properties and scoring methods. Pain 1975;1:275–99.
Work disability
The are five outstanding reasons for measuring work outcomes are as follows:
BOX 38-5 Listing of WL-26 items
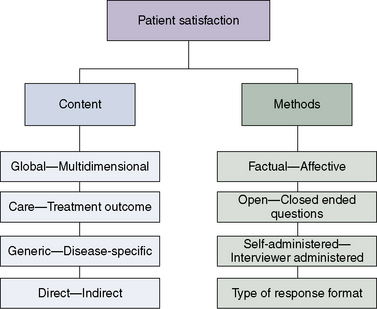
Patient satisfaction
Table 38.9 Sample Items According to Content Characteristics
| Global—Multidimensional |
PSS, Patient Satisfaction Scales [3]; PSQ, Patient Satisfaction Questionnaire [4]; CSQ, Client Satisfaction Questionnaire [5]; FOQ, Functional Outcomes Questionnaire [6]; GPAS, = General Practice Assessment Survey[7]. From Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine 2000;25:3167-3177.
BOX 38-6 Patient Satisfaction Subscales
Questions Included in “Information” Subscale (3)
The physician gave me enough information about the cause of my back pain.
The physician did not give me a clear explanation of the cause of my pain.
The physician told me what to do to prevent future back problems.
Questions Included in “Caring” Subscale (4)
The physician seemed to believe that my pain was real.
The physician did not understand the concerns I had about my back problem.
The physician did not seem comfortable dealing with my back pain.
The physician was not concerned about what happened with my pain after I left the office.
Questions Included in “Effectiveness” Subscale (3)
The treatment the physician prescribed for my back was effective.
The physician seemed confident that the treatment she/he recommended would work.
The physician gave me a clear idea of how long it might take for my back to get better.
Questions Not Included in Any Subscale (7)
After seeing the physician I did not know what I needed to do for my back pain.
The physician did not listen carefully to my description of my back problem.
The physician made me feel less worried about my back problem.
The physician performed a thorough examination of my back.
The physician did not understand what was wrong with my back.
The physician should have ordered more tests or radiographs.
1 Roland M.O., Morris R.W. A study of the natural history of back pain. Part 1: development of a reliable and sensitive measure of disability in low back pain. Spine. 1983;8:141-144.
2 Hupli M., Sainio P., Hurri H., et al. Comparison of trunk strength measurements between two different isokinetic devices used at clinical settings. J Spinal Disord. 1997;10:391-393.
3 Cherkin D., Deyo R.A., Berg A.O. Evaluation of a physician education intervention to improve primary care for low-back pain. II. Impact on patients. Spine (Phila Pa 1976). 1991;16(10):1173-1178.
4 Ware J.E.Jr, Snyder M.K., Wright W.R., Davies A.R. Defining and measuring patient satisfaction with medical care. Eval Program Plann. 1983;6(3–4):247-263.
5 Larsen D.L., Attkisson C.C., Hargreaves W.A., Nguyen T.D. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197-207.
6 Nork S.E., Hu S.S., Workman K.L., Glazer P.A., Bradford D.S. Patient outcomes after decompression and instrumented posterior spinal fusion for degenerative spondylolisthesis. Spine (Phila Pa 1976). 1999;24(6):561-569.
7 National Primary Care Research and Development Centre. General Practice Assessment Survey (GPAS) Manual. Manchester: University of Manchester, 1999.