Chapter 4 Other systems
Dental anaesthesia
Standards and Guidelines for General Anaesthesia for Dentistry
The Royal College of Anaesthetists 1999
Introduction
Background
Techniques
Cartwright D.P. Death in the dental chair. Anaesthesia. 1999;54:105-107.
Department of Health. General anaesthesia, sedation and resuscitation in dentistry (Poswillo Report). London: HMSO, 1990.
Flynn P.J., Strunin L. General anaesthesia for dentistry. Anaesth Intens Care Med. 2005;6:263-265.
Royal College of Anaesthetists. Standards and guidelines for general anaesthesia and dentistry. London: RCA, 1999.
Worthington L.M., Flynn P.J., Strunin L. Death in the dental chair: an avoidable catastrophe? Br J Anaesth. 1998;80:131-132.
Anaesthesia for ear, nose and throat surgery
General anaesthetic problems
Ear surgery
Nasal surgery
Throat surgery
Tonsillectomy
Extubate awake (protective reflexes), with head-down in left lateral position.
There are two approaches to induction:
Peritonsillar abscess (quinsy)
National Patient Safety Agency
Reducing the Risk of Retained Throat Packs after Surgery, April 2009
Anaesthesia and liver disease
Physiological changes in liver disease
Haematology. Anaemia, thrombocytopenia, coagulopathy.
GI. Oesophageal varices, delayed gastric emptying. Increased gastric volume and acidity.
Pharmacokinetic and pharmacodynamic changes
Assessment of surgical risk
Child’s (1963) classification assessed risk using albumin and bilirubin. Modified by Pugh et al (1973) (see Table 4.1). Perioperative mortality A<5%, B≈︀25%, C>50%.
Specific drugs
Anticholinergics. Little change in pharmacokinetics. Use normal doses.
Barbiturates. Increased sensitivity and prolonged excretion of thiopentone. Use <3–4 mg/kg.
Propofol. Increased sensitivity. Use 2 mg/kg for induction.
Anticholinesterases. Normal doses of neostigmine may be used.
Fabbroni D., Bellamy M. Anaesthesia for hepatic transplantation. Contin Edu Anaesth, Crit Care Pain. 2006;6:171-175.
Hartog A., Mills G. Anaesthesia for hepatic resection surgery. Contin Edu Anaesth, Crit Care Pain. 2009;9:1-5.
Lai W.K., Murphy N. Management of acute liver failure. Contin Edu Anaesth, Crit Care Pain. 2004;4:40-43.
Anaesthesia for ophthalmic surgery
Physiology
Regional anaesthesia
Local anaesthetic solution
Less painful injection if solution warmed to 35°C.
Retrobulbar and peribulbar blocks are equated with spinal and epidural blocks, respectively.
Compress eyeball for 10 min after injection to aid spread of LA using small pneumatic/lead balloon strapped over eye.
Complications of regional blocks
Open eye injury and full stomach
A study of rapid sequence induction using suxamethonium in 228 patients failed to show any loss of vitreous through the penetrating wound (Libonati et al 1985).
Three approaches to rapid sequence induction:
Local Anaesthesia for Intraocular Surgery
Royal College of Anaesthetists and Royal College of Ophthalmologists 2001
General comments
Preoperative assessment
Day of surgery
Canavan K.S., Dark A., Garrioch M.A. Sub-Tenon’s administration of local anaesthetic: a review of the technique. Br J Anaesth. 2003;90:787-793.
Hamilton R.C. Techniques of orbital regional anaesthesia. Br J Anaesth. 1995;75:88-92.
Johnson R.W. Anatomy for ophthalmic anaesthesia. Br J Anaesth. 1995;75:80-87.
Libonati M.M., Leahy J.J., Ellison N. The use of succinylcholine in open eye surgery. Anesthesiology. 1985;62:637-640.
Murgatroyd I.H., Bembridge J. Intraocular pressure. Contin Edu Anaesth, Crit Care Pain. 2008;8:100-103.
Parness G., Underhill S. Regional anaesthesia for intraocular surgery. Contin Edu Anaesth, Crit Care Pain. 2005;5:93-97.
Raw D., Mostafa S.M. Drugs and the eye. BJA CEPD Rev. 2001;1:161-165.
Royal College of Anaesthetists and Royal College of Ophthalmologists. Local anaesthesia for intraocular surgery. London: Royal College of Anaesthetists and Royal College of Ophthalmologists, 2001.
Thind G.S., Rubin A.P. Local anaesthesia for eye surgery. Br J Anaesth. 2001;86:473-476.
Vachon C.A., Warner D.O., Bacon D.R. Succinylcholine and the open globe. Anesthesiology. 2003;99:220-223.
Vann M.A., Ogunnaike B.O., Joshi G.P. Sedation and anesthesia care for ophthalmologic surgery during local/regional anesthesia. Anesthesiology. 2007;107:502-508.
Anaesthesia for orthopaedic surgery
Anaesthetic management
Anaesthetic technique
Fat embolism syndrome (FES)
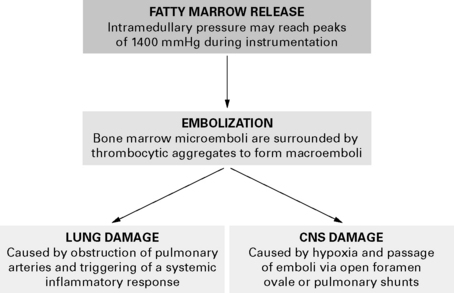
Severe FES may cause cardiovascular collapse, multiorgan failure and death. Pathophysiological changes occur in three steps (Fig. 4.1). FES also reported with burns, acute pancreatitis, hepatic failure, bone marrow harvest and extra-corporeal circulation.
Postoperative hyponatraemia
DVT prophylaxis
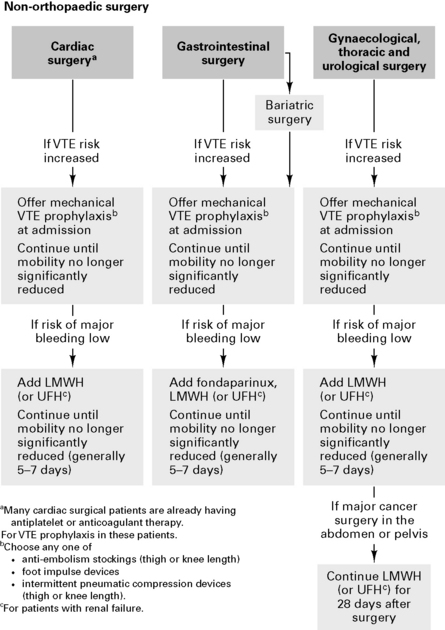
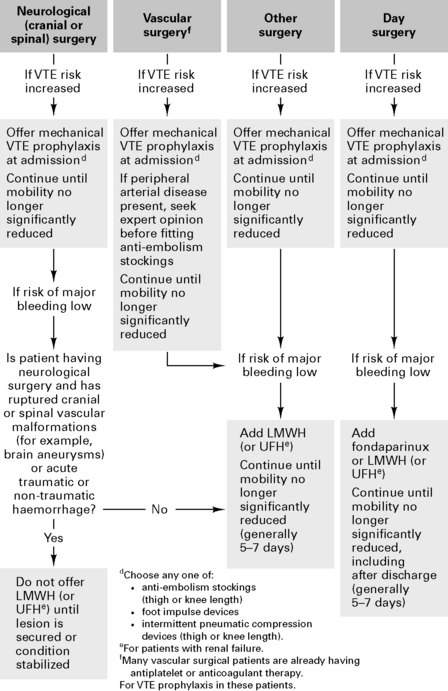
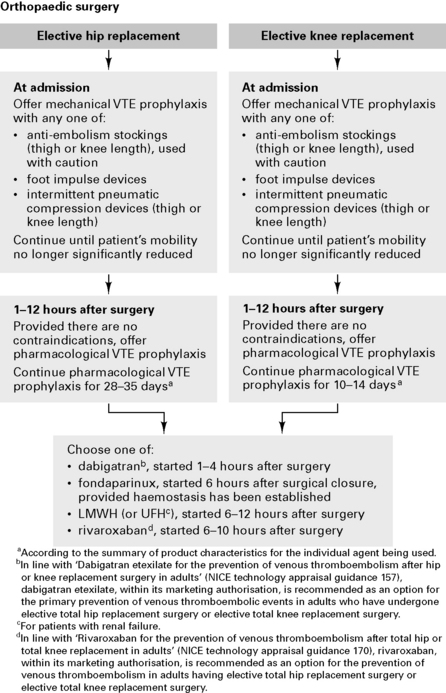
Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital, January 2010
Assessing the risks of VTE and bleeding
Patients who are at risk of VTE
Patients who are at risk of bleeding
All patients who have any of the following
Mechanical prophylaxis
Pharmacological prophylaxis
Connolly D. Orthopaedic anaesthesia. Anaesthesia. 2003;58:1189-1193.
Donaldson A.J., Thomson H.E., Harper N.J., et al. Bone cement implantation syndrome. Br J Anaesth. 2009;102:12-22.
Gardner A.C., Dunsmuir R.A. What’s new in spinal surgery? Contin Edu Anaesth, Crit Care Pain. 2008;8:186-188.
Gupta A., Reilly C.S. Fat embolism. Contin Edu Anaesth, Crit Care Pain. 2007;7:148-151.
Jandziol A.K., Griffiths R. The anaesthetic management of patients with hip fractures. BJA CEPD Rev. 2001;1:52-55.
Lane N., Allen K. Hyponatraemia after orthopaedic surgery. BMJ. 1999;318:1363-1364.
Mellor A., Soni N. Fat embolism. Anaesthesia. 2001;56:145-154.
NICE. Venous thromboembolism: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital, 2010. January 2010 http://guidance.nice.org.uk/CG92
Anaesthesia and renal failure
Acute renal failure
| Prerenal | Renal | |
|---|---|---|
| Urine: plasma (U:P) osmolality | >2:1 | <1:2 |
| U:P urea | >20 | <10 |
| U:P creatinine | >40 | <10 |
| Urine Na+ (mEq/L) | <20 | >60 |
Chronic renal failure
Causes of chronic renal failure:
Pharmacokinetic and pharmacodynamic changes
Common conditions associated with chronic renal failure
Neurological. Peripheral and autonomic neuropathy. Mild uraemic encephalopathy.
Specific drugs
Anaesthetic management for chronic renal failure patients
Craig R.G., Hunter J.M. Recent developments in the perioperative management of adult patients with chronic kidney disease. Br J Anaesth. 2008;101:296-310.
Rabey P.G. Anaesthesia for renal transplantation. BJA CEPD Rev. 2001;1:24-27.
Short A., Cumming A. ABC of intensive care. Renal support. BMJ. 1999;319:41-44.
Anaesthesia for urological surgery
Transurethral resection of the prostate
Lithotomy position
Increased CVP in the lithotomy position may cause angina or precipitate heart failure.

 scatter and ↑ shunting, together with impaired respiration from ascites, causing hypoxia.
scatter and ↑ shunting, together with impaired respiration from ascites, causing hypoxia.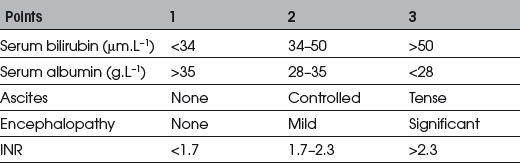




 mismatching and release of vasoactive substances from the lungs. Severe pain during intramedullary nailing may also contribute.
mismatching and release of vasoactive substances from the lungs. Severe pain during intramedullary nailing may also contribute.