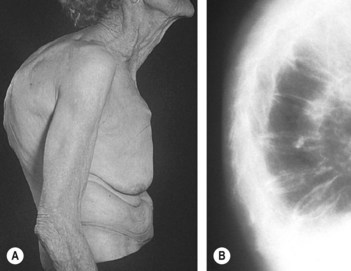
247 Osteoporosis of the spine (dowager’s hump)
Salient features
History
• History of back pain (usually the onset is sudden with severe pain in the dorsal spine)
• Spontaneous fractures and loss of height
• Long-term corticosteroid, heparin therapy or proton pump inhibitors (>7 years of last) (CMAJ 2008;179:319–26)
• Postmenopausal or has had an oopherectomy
• Smoker or consumes alcohol (>3 units/day)
• Is there a family history particularly in a parent
• What is the patient’s weight (body mass index (BMI) <22 kg/m2 is associated with osteoporosis)
• Associated conditions: rheumatoid arthritis, uncontrolled diabetes mellitus, Crohn’s disease, ankylosing spondylitis, multiple myleoma, Cushing syndrome, thyrotoxicosis, oestrogen deficiency in women and androgen deficiency in men, Marfan syndrome, Ehlers–Danlos syndrome, homocystinura.
Advanced-level questions
What are the types of osteoporosis?
• Type I results from accelerated bone loss, particularly trabecular bone, and is probably caused by oestrogen deficiency. It typically results in fractures of vertebral bodies and the distal forearm in women in their 60s and 70s.
• Type II results from age-related bone loss and is much slower. It occurs in both sexes and typically results in fracture of the proximal femur in the elderly.
• Secondary osteoporosis: accounts for about 20% of cases in women and 40% of cases in men.
What are the typical sites of fracture in osteoporosis?
Vertebrae, neck of femur and distal radius (Colles’ fracture).
What are the risk factors for osteoporosis?
• Independent of bone mineral density: age, previous fragility fracture, maternal history of hip fracture, corticosteroid therapy, smoking, alcohol intake >3 units/day, rheumatoid arthritis, BMI <22 (thin body type in women), falls, organ transplantation
• Depending on bone mineral density: untreated hypogonadism (secondary amenorrhoea), anorexia nervosa, malabsorption, endocrine disease (hyperthyroidism, primary hyperparathyroidism), chronic renal disease, chronic liver disease, chronic obstructive pulmonary disease, immobility, medications (aromatase inhibitors, androgen deprivation therapy).
How would you investigate such a patient?
• Radiographs and bone scans looking for fractures and to exclude metastases
• Serum calcium and phosphates, alkaline phosphatase and creatinine (remember osteoporosis is not a disorder of calcium metabolism)
• Urinary calcium and creatinine excretion: 24-h samples
• Urinary Bence Jones protein concentration and serum protein electrophoresis
• Thyroid-stimulating hormone concentrations
• Serum testosterone level in men
• DEXA scanning, which determines bone density, is the gold standard test.
What are the recommendations to measure bone mineral density?
• Radiographic evidence of osteopenia and/or vertebral deformity
• Loss of height, thoracic kyphosis (after radiographic confirmation of vertebral deformity)
• Prolonged corticosteroid therapy (prednisolone >7.5 mg daily for 6 months or more)
• Premature menopause (age <45 years)
• Prolonged secondary amenorrhoea (>1 year)
• Chronic disorders associated with osteoporosis
How would you estimate the 10-year probability of fracture risk in this patient?
FRAX is an electronic clinical tool (www.shef.ac.uk/FRAX/), developed by Professor John Kanis, that is used to determine fracture risk using seven clinical risk factors (previous fracture, hip fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, ingestion of ≥3 units of alcohol daily); the patients age, gender, height and weight; and bone mineral density of the femoral neck. This clinical tool derives an algorithm that estimates the 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture (hip, spine, proximal humerus or distal forearm).
How would you prevent osteoporosis?
• The goal of therapy is to half the risk of fracture
• Life-style advice: exercise, stop smoking and reduce alcohol consumption
• Regular weight-bearing exercise
• Replacement oestrogen therapy in postmenopausal women should be administered for at least 5 years
• Raloxifene (a selective oestrogen receptor modulator) is indicated in the prevention or treatment of osteoporosis in postmenopausal women. Lasofoxifene (a non-steroidal selective oestrogen receptor (ER) modulator), in postmenopausal women, was associated with reduced risks of non-vertebral and vertebral fractures, ER-positive breast cancer, coronary heart disease and stroke with no increase in the risk of endometrial cancer but an increased risk of venous thromboembolic events (N Engl J Med 2010;362:686–96). The results of this trial suggest that lasofoxifene offers no major clinically important benefits over raloxifene for the skeleton, breast, heart or reproductive tract
• Dietary calcium intake increased to 1.5 g/day (with no more than 500–600 mg in a single dose because of limited absorption with higher doses) and vitamin D3 800–1000 IU/day with a goal of achieving serum 25-hydroxyvitamin D of 30 µg/l (75 nmol/l) or higher
• Alendronate, a new bisphosphonate, is 1000 times more potent than etidronate in inhibiting bone resorption and hence is able to provide effective inhibition at a dosage that does not affect mineralization. It is indicated only in the prevention and treatment of postmenopausal osteoporosis and in the treatment of glucocorticoid-induced osteoporosis and osteoporosis in men
• Residronate significantly reduces the risk of hip fracture among elderly women with confirmed osteoporososis (N Engl J Med 2001;344:333–40). Risedronate (dosed daily, weekly or monthly) and zoledronate (dosed annually) are indicated for prevention and treatment of postmenopausal and glucocorticoid-induced osteoporosis and in treatment of osteoporosis in men
• Ibandronate (oral or intravenously) is indicated only for treatment of postmenopausal osteoporosis
• Calcitonin nasal spray results in decreased bone resporption and is indicated only for treatment of postmenopausal osteoporosis
• Denosumab, a human monoclonal antibody to the receptor activator of NF-κB ligand (RANKL), inhibits the development and activity of osteoclasts, decreasing bone resorption and increasing bone density
• Teriparatide (recombinant parathormone) as a subcutanous injection daily for up to 2 years is approved for the treatment of osteoporosis in postmenopausal women and in men who are at high risk for fracture. Teriparatide labelling in the USA carries a black-box warning for osteosarcoma. There is also a risk of renal malignancy
• Future treatments: vitamin D analogues, strontium salts, ipriflavone, calciomimetic drugs that stimulate intermittent production of parathyroid hormone, inhibitors of sclerostin (a protein produced by bone that is a negative regulator of bone formation) and its signalling pathway, testosterone in men with hypogonadism.
What are the precautions needed with bisphosphonates?
• An oral bisphosphonate should be avoided in patients with a history of oesophageal stricture but an intravenous bisphosponate may be considered.
• Bisphosphonate-associated osteonecrosis of the jaw is rare and most cases have been noted in cancer patients who received high doses intravenously (BMJ 2006 333:982–3).
• There is increased risk of clinical vertebral and hip fractures after bisphosphonates are discontinued, and, therefore, a drug holiday is not the best choice in those patients with a high risk of fracture.