Osteoporosis
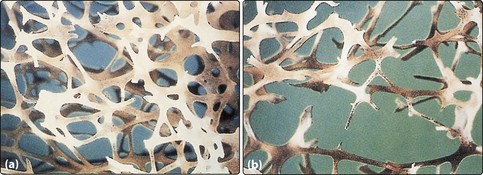
Bone is in a constant state of turnover, which is kept in balance by opposing actions of osteoblasts (bone formation) and osteoclasts (bone resorption). Osteoporosis results when, irrespective of the cause, this balance is disturbed and shifts in favour of resorption. It is defined as a progressive systemic skeletal disorder characterized by low bone mineral density (BMD), deterioration of the microarchitecture of bone tissue, and susceptibility to fracture (Fig 39.1). The World Health Organization (WHO) proposed a clinical definition based on measurements of BMD: a patient is osteoporotic based on a BMD measurement 2.5 standard deviations below typical peak bone mass of young healthy white women. This measurement of standard deviation from peak mass is called the T score. A T score of −2.5 (and below) is osteoporosis, while a score of −1 to −2.4 is osteopenia.
Risk factors
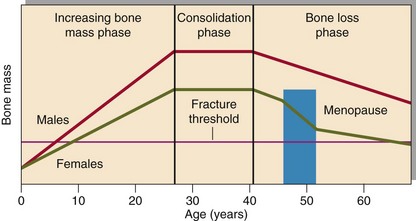
Age and menopause are the two main non-modifiable risk factors. Figure 39.2 shows the average bone mass throughout life. Peak bone mass is reached around 25–30 years. Contributing factors are genetic, dietary intake of calcium and vitamin D and physical exercise.
Other risk factors include history of previous fracture, family history of osteoporosis and hip fracture, sex hormone deficiency, smoking, alcoholism, immobility and sedentary lifestyle. Osteoporosis may also be secondary to endocrine disorders including Cushing’s syndrome, primary hyperparathyroidism, hypovitaminosis D (classically associated with osteomalacia), hypogonadism and hyperthyroidism, as well as systemic illnesses such as rheumatoid arthritis, chronic kidney and liver diseases and malignancies. The commonest cause of secondary osteoporosis is corticosteroid use. (Fig 39.3)