Osteomalacia, rickets, and vitamin D insufficiency
1. What are osteomalacia and rickets?
Osteomalacia and rickets are terms that describe the clinical, histologic, and radiologic abnormalities of bone that are associated with more than 50 diseases and conditions. Osteomalacia is a disorder of mature (adult) bone, whereas rickets occurs in growing bone. Although rickets and osteomalacia were initially viewed as distinct clinical entities, the same pathologic processes may result in either disorder. In both conditions, mineralization of newly formed osteoid (the bone protein matrix) is inadequate or delayed. In individuals with rickets, defective mineralization occurs in both bones and cartilage of the epiphyseal growth plates and is associated with growth retardation and skeletal deformities that are not typically seen in adults with osteomalacia.
2. Why is it important to know about osteomalacia and rickets?
In the United States at the beginning of the 20th century, rickets due to a deficiency of vitamin D was common in urban areas. In the 1920s, rickets was virtually eliminated by an appreciation of the antirachitic properties of sunlight and the use of cod liver oil (which contains vitamin D). However, with the development of effective treatments for previously fatal diseases that affect vitamin D metabolism (such as chronic renal failure) and with an improved understanding of both vitamin D and mineral metabolism, many additional syndromes with osteomalacia or rickets as a feature have emerged. Many later studies have demonstrated that undiagnosed vitamin D deficiency or insufficiency is common in the United States, and for a significant number of adult women with osteoporosis, vitamin D insufficiency may be an unsuspected component of their bone loss.
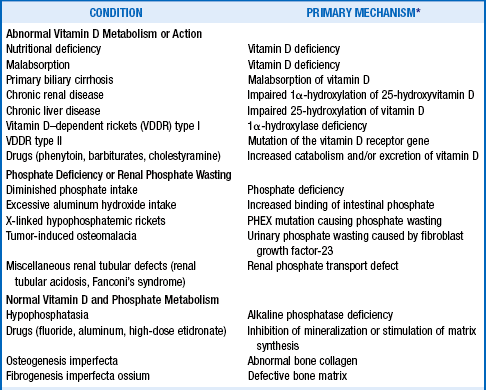
3. List the causes of osteomalacia and rickets
The primary abnormality of bone in patients with either osteomalacia or rickets is defective mineralization of the bone matrix. The major mineral in bone is hydroxyapatite—Ca10(PO4)6(OH)2. Thus, any disease that results in decreased availability to bone of either calcium or phosphorus may result in osteomalacia or rickets (Table 11-1). Causes of osteomalacia and rickets fall into three categories: (1) disorders associated with abnormalities of vitamin D metabolism or action that limit the availability of calcium for mineralization of bone, (2) disorders associated with abnormalities of phosphorus metabolism, and (3) a small group of disorders in which there is normal vitamin D and mineral metabolism.
4. Describe how vitamin D is synthesized and metabolized.
Serum vitamin D comes from two sources: dietary intake and conversion by ultraviolet (UV) irradiation of 7-dehydrocholesterol or ergosterol in the skin. Vitamin D is then transported through the blood to the liver, where it is converted to 25-hydroxyvitamin D (25-OHD) by the hepatic 25-hydroxylase enzyme. The 25-OHD is then converted in the kidney to the active hormone, 1,25-dihydroxyvitamin D, by the renal 1α-hydroxylase enzyme. This active vitamin D metabolite has effects in many tissues, including the intestine (increases calcium absorption), the kidney (increases calcium reabsorption), the parathyroid glands (decreases parathyroid hormone [PTH] secretion), and bone (stimulates osteoblast maturation and bone matrix synthesis) (Fig. 11-1). Studies have now suggested possible other roles for vitamin D in cardiovascular and neurologic diseases, insulin resistance and diabetes, malignancies, autoimmune conditions, and infections. From an understanding of how vitamin D is metabolized, it is apparent that even when dietary intake and UV-mediated vitamin D synthesis are normal, vitamin D deficiency may occur in association with severe malabsorptive, renal, or liver disease.
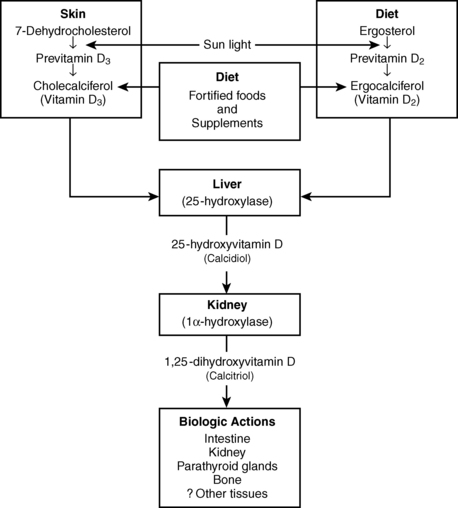
Figure 11-1. Synthesis and metabolism of Vitamin D.
5. Discuss the disease processes that interfere with the metabolism of vitamin D.
Clinically apparent vitamin D deficiency is rarely seen in the United States except when exposure to sunlight and intake of vitamin D–fortified milk and other dairy products are limited. However, many elderly Americans are at risk for occult vitamin D deficiency or insufficiency because of sun avoidance, sunscreen use, an age-related decrease in dermal vitamin D synthesis, impaired hepatic and renal vitamin D hydroxylation, and diminished intestinal responsiveness to 1,25-dihydroxyvitamin D. Celiac disease or sprue, regional enteritis, intestinal bypass surgery, partial gastrectomy, chronic liver disease, primary biliary cirrhosis, pancreatic insufficiency, chronic renal failure, and certain medications have also been associated with the development of osteomalacia.
6. List genetic disorders that interfere with vitamin D synthesis or action.
Two extremely rare genetic syndromes are also associated with rickets. Vitamin D–dependent rickets (VDDR) type I (also called pseudovitamin D deficiency rickets) is caused by an almost complete absence of renal 25-hydroxyvitamin D–1α-hydroxylase activity. VDDR type II results from a mutation of the vitamin D receptor gene that causes end-organ resistance to 1,25-dihydroxyvitamin D and lack of vitamin D action.
7. What conditions associated with abnormalities of phosphate metabolism result in osteomalacia or rickets?
Nutritional phosphate deficiency, decreased intestinal phosphate absorption due to ingestion of phosphate binders (such as aluminum hydroxide), or renal phosphate wasting may result in osteomalacia or rickets. Hypophosphatemic rickets (also called vitamin D–resistant rickets) is a syndrome of renal phosphate wasting and decreased renal synthesis of 1,25-dihydroxyvitamin D. Hypophosphatemic rickets, which is transmitted as an X-linked dominant trait, is the most common inherited form of rickets. Another syndrome, tumor-induced osteomalacia, is observed when usually benign neoplasms of mesenchymal origin secrete fibroblast growth factor-23 (FGF-23), which promotes renal phosphate wasting and produces osteomalacia.
8. Does chronic renal failure cause osteomalacia and rickets?
Chronic renal failure is associated with several bone diseases: osteomalacia or rickets, adynamic bone, osteitis fibrosa cystica (due to long-standing secondary hyperparathyroidism), and a combination of both osteomalacia and osteitis fibrosa cystica (termed mixed renal osteodystrophy). Rickets or osteomalacia is usually a late finding in the course of the kidney disease and is rarely seen before patients begin dialysis. Rickets or osteomalacia associated with chronic renal failure is caused by decreased circulating concentrations of 1,25-dihydroxyvitamin D, by aluminum intoxication from aluminum-containing antacids used as phosphate binders or an aluminum-contaminated dialysate, and possibly by the chronic metabolic acidosis associated with the renal failure.
9. What signs and symptoms are associated with osteomalacia?
In adults, osteomalacia may be asymptomatic. When symptomatic, osteomalacia may manifest as diffuse skeletal pain (often aggravated by physical activity or palpation), muscle weakness, and sometimes muscle wasting. The muscle weakness often involves the proximal muscles of the lower extremities and may result in a waddling gait and difficulties rising from a chair or climbing stairs. The bone pain is described as dull and aching and is usually located in the back, hips, knees, and legs and at sites of fractures. Fractures may result from only minor trauma.
10. Describe the clinical findings in rickets.
Because of impaired calcification of cartilage at the growth plates in children with rickets, the clinical manifestations of rickets are significantly different from those of osteomalacia. Widening of the metaphyses (the growth zones between the epiphysis and diaphysis), slowed growth, and various skeletal deformities are prominent in this condition. The effects of rickets are greatest at sites where bone growth is most rapid. Because the rate of skeletal growth varies with age, the manifestations of rickets likewise vary. One of the earliest signs of rickets in infants is craniotabes (abnormal softness of the skull). In older infants and younger children, thickening of the forearm at the wrist and of the costochondral junctions (also known as the rachitic rosary) and Harrison’s groove, a lateral indentation of the chest wall at the sites of attachment of the diaphragm, may be present. In older children, bowing of the tibia and fibula may be observed. At any age, if rickets (or osteomalacia) is associated with hypocalcemia, paresthesias of the hands and around the mouth, muscle cramps, presence of Chvostek and Trousseau signs, tetany, and seizures may be evident.
11. What are the biochemical abnormalities seen with osteomalacia and rickets caused by vitamin D deficiency?
The laboratory abnormalities encountered with osteomalacia or rickets depend on the underlying defect or process causing the bone disease. To understand the biochemical abnormalities observed in conditions associated with abnormal vitamin D metabolism, an understanding of the body’s response to hypocalcemia and knowledge of the vitamin D metabolic pathway are necessary. Thus, in patients with nutritional vitamin D deficiency or malabsorption, low vitamin D levels result in low or low-normal serum calcium concentrations, which stimulate increased PTH secretion (secondary hyperparathyroidism). This hyperparathyroid state, in turn, causes increased renal phosphate excretion, decreased serum phosphate, elevated serum alkaline phosphatase values, and reduced urinary calcium excretion.
12. What are the vitamin D metabolite concentrations associated with the diseases that interfere with vitamin D metabolism or action?
Depending on the abnormality of vitamin D metabolism, different vitamin D metabolite patterns may be observed. In nutritional vitamin D deficiency, 25-OHD levels are low. In VDDR type I, which results from a deficiency of the renal 25-hydroxyvitamin D-1α-hydroxylase enzyme, normal or increased serum 25-OHD and low or undetectable serum 1,25-dihydroxyvitamin D levels are observed. In contrast, in VDDR type II, which causes resistance of target organs to 1,25-dihydroxyvitamin D, the values of both 25-OHD and 1,25-dihydroxyvitamin D are elevated.
13. What radiographic findings are associated with osteomalacia and rickets?
The biochemical abnormalities associated with rickets and osteomalacia are usually evident before radiographic abnormalities are observed. The most common radiographic change in patients with osteomalacia is a reduction in bone mass. Pseudofractures (also called Looser’s zones or Milkman’s fractures) or complete fractures also may be observed. Pseudofractures are transverse radiolucent bands ranging from a few millimeters to several centimeters in length, usually perpendicular to the surfaces of the bones. They are most often bilateral and are particularly common in the femur, pelvis, and small bones of the hands and feet. Patients with osteomalacia may have additional findings due to secondary hyperparathyroidism. Such findings include subperiosteal resorption of the phalanges, loss of the lamina dura of the teeth, widening of the spaces at the symphysis pubis and sacroiliac joints, and presence of brown tumors or bone cysts.
Certain radiographic abnormalities are observed primarily in children with rickets. These include fraying of the metaphyses of the long bones, widening of the unmineralized epiphyseal growth plates, and bowing of the legs. These skeletal deformities may persist into adulthood.
14. Discuss the histologic features of osteomalacia.
The two diagnostic histologic findings in osteomalacia are the presence of widened osteoid seams and increased mineralization lag time (the time necessary for newly deposited matrix to mineralize). The mineralization lag time is assessed clinically by administering two short courses of oral tetracycline several weeks apart before the bone biopsy is performed. Because tetracycline is deposited at the mineralization front in newly formed bone, the lag time may be determined by measuring the distance between the two fluorescent tetracycline bands in the biopsy specimen. Depending on the cause of the osteomalacia, hyperparathyroid bone changes may also be seen. Because of the varied clinical signs and symptoms, radiographic findings, and biochemical abnormalities associated with osteomalacia and rickets, none of these tests or findings is pathognomonic. The bone biopsy remains the gold standard in establishing the diagnosis of rickets and osteomalacia. The bone biopsy specimen must be evaluated by personnel specially trained in the interpretation of bone histology.
15. Describe the therapy for vitamin D deficiency.
The goal of therapy for patients with osteomalacia and rickets due to an abnormality of vitamin D metabolism is to correct the hypocalcemia and the deficiency of active vitamin D metabolites through the administration of calcium salts and vitamin D preparations. In the United States, vitamin D2 (ergocalciferol), vitamin D3 (cholecalciferol), 1,25-dihydroxyvitamin D (calcitriol), and calcitriol analogs are available. Each of these preparations has a different half-life and potency. The choice and dose of vitamin D preparation are determined by the underlying pathologic defect of vitamin D metabolism. For patients with vitamin D deficiency, treatment with ergocalciferol along with elemental calcium is often sufficient to heal the osteomalacia.
16. What are the treatments for osteomalacia and rickets not due to vitamin D deficiency?
Osteomalacia associated with VDDR type II, which involves profound resistance to the effects of vitamin D, must be treated with the most potent vitamin D metabolite, 1,25-dihydroxyvitamin D, in extraordinarily high doses, along with large doses of oral calcium. In severe cases, high-dose intravenous calcium infusions are required to heal the rickets. VDDR type I is also treated with calcitriol, but physiologic doses are usually sufficient. For treatment of hypophosphatemic rickets, both phosphate supplements and calcitriol are necessary to heal the bone disease. Tumor removal or irradiation is required to treat tumor-induced osteomalacia. In chronic renal failure with aluminum-induced osteomalacia, aluminum can be removed from affected bone with the chelating agent deferoxamine. The bone disease can then be treated with calcium and calcitriol. Osteomalacia associated with renal tubular acidosis is treated with vitamin D and bicarbonate to correct the acidosis.
17. Why is vitamin D insufficiency important, and how is it diagnosed?
The association of vitamin D insufficiency with low bone mass and an increased risk of hip fracture has only been recently appreciated. It is generally agreed that the optimal circulating 25-OHD concentration is at least 30 ng/mL (75 nmol/L). Various writers and medical organizations have defined vitamin D deficiency as a 25-OHD concentration of either 10 or 20 ng/mL (25 or 50 nmol/L). The 25-OHD level in vitamin D insufficiency falls between these deficient and sufficient levels. Inadequate vitamin D status is a common problem. Data from the National Health and Nutrition Examination Survey (2001-2004) population demonstrated that only 23% had circulating concentrations of 25-OHD above 30 ng/mL, and 6% had values less than 10 ng/mL. As circulating 25-OHD concentrations decrease from sufficient levels, there is a growing negative impact on skeletal health. It therefore seems prudent to provide vitamin D supplementation to individuals with circulating 25-OHD levels less than 30 ng/mL.
18. What are the complications of treatment with vitamin D2 or vitamin D metabolites?
When high doses of vitamin D2 or one of the potent vitamin D metabolites are used, it is important to monitor carefully for the development of hypercalcemia. Mild hypercalcemia may be asymptomatic. However, severely hypercalcemic patients may complain of anorexia, nausea, vomiting, weight loss, headache, constipation, polyuria, polydipsia, and altered mental status. Impaired renal function, nephrocalcinosis, nephrolithiasis, and even death may eventually ensue. If vitamin D intoxication occurs, all calcium supplements and vitamin D preparations must be discontinued immediately, and therapy for hypercalcemia instituted.
Adams, JS, Hewison, M. Update in vitamin D. J Clin Endocrinol Metab. 2010;95:471.
Berry, JL, Davies, M, Mee, AP, Vitamin D metabolism, rickets, and osteomalacia. Semin Musculoskelet Radiol, 2002;6:173.
Carpenter, TO. The expanding family of hypophosphatemic syndromes. J Bone Miner Metab. 2012;30:1.
Demay, MB, Rickets caused by impaired vitamin D activation and hormone resistance. pseudovitamin D deficiency rickets and hereditary vitamin D resistant rickets. Favus MJ, ed. Primer on the metabolic bone diseases and disorders of mineral metabolism, 6. American Society for Bone and Mineral Research: Washington, DC, 2006;338.
Ginde, AA, Liu, MC, Camargo, CA, Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169:626.
Holick, MF, Brinkley, NC, Bischoff-Ferrari, HA, et al, Evaluation, treatment, and prevention of vitamin D deficiency. an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1911.
Holick, MF, Garabedian, M, Vitamin D. photobiology, metabolism, mechanism of action and clinical applications. Favus MJ, ed. Primer on the metabolic bone diseases and disorders of mineral metabolism, ed 6Washington, DC: American Society for Bone and Mineral Research;2006;106.
Holick, MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. 2006;116:2062.
Holick, MF. Vitamin D deficiency. N Engl J Med. 2007;357:266.
Jan de Beur, SM. Tumor-induced osteomalacia. In: Favus MJ, ed. Primer on the metabolic bone diseases and disorders of mineral metabolism. ed 6. Washington, DC: American Society for Bone and Mineral Research; 2006:345.
Malloy, PJ, Feldman, D. Genetic disorders and defects in vitamin D action. Endocrinol Metab Clin North Am. 2010;39:333.
Pettifor, JM. Nutritional and drug-induced rickets and osteomalacia. In: Favus MJ, ed. Primer on the metabolic bone diseases and disorders of mineral metabolism. ed 6. Washington, DC: American Society for Bone and Mineral Research; 2006:330.
Rosen, CJ. Vitamin D insufficiency. N Engl J Med. 2011;364:248.
Thacher, TD, Clarke, BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86:50.
Wolinsky-Friedland, M. Drug-induced metabolic bone disease. Endocrinol Metab Clin North Am. 1995;24:395.