CHAPTER 9 Osteocapsular Arthroplasty of the Elbow
Arthroscopic osteocapsular arthroplasty is a procedure involving three-dimensional reshaping of the bones (i.e., removal of osteophytes), removal of any loose bodies, and capsulectomy to restore motion and function and to eliminate pain.1
Arthroscopic release is effective for soft tissue contractures of the elbow.2–5 When arthritic changes are present, bone work is also necessary.1,6–12
ANATOMY
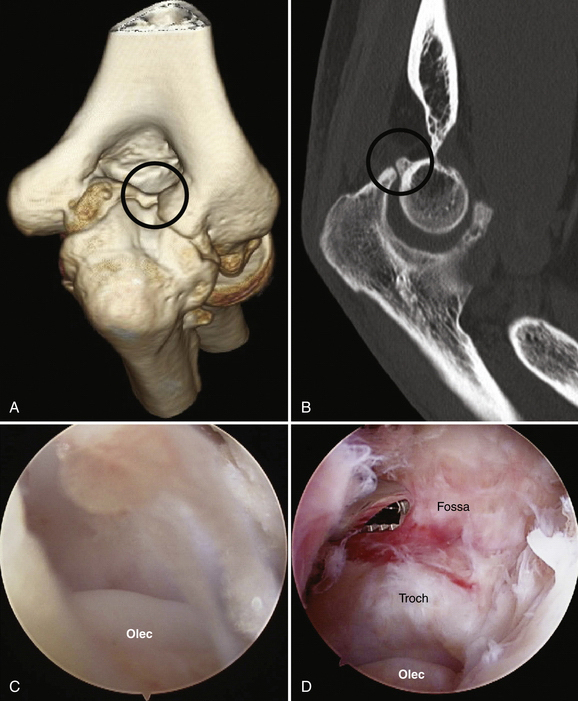
Osteophytes build up in typical locations along the margins of the joint and in the fossae. Although the patient may have osteophytes on the posteromedial olecranon, osteophytes alone do not always cause impingement pain. The relationship between bony osteophytes and impingement pain poses an apparent dilemma. It is not unusual to see osteophytes that impinge at the limit of motion in patients who have no pain. The question is why some osteophytes are painful and others are not. Based on experience and unpublished research in progress, I think the usual cause for impingement pain in such circumstances is a fractured olecranon osteophyte that has typically progressed to nonunion by the time of referral to the orthopedic surgeon.13 Nonunion fractures are best visualized (Fig. 9-1) on sagittal and coronal computed tomography (CT) reconstructions. The loose fragment is easily missed during arthroscopy because it is very small or covered with cartilage and not obviously loose. In some patients, the loose fragment is removed during osteophyte excision without ever being recognized. Other causes for the pain include loose bodies or buildup of inflamed soft tissue posteriorly.
PATIENT EVALUATION
History and Physical Examination
I have found that the diagnosis of posterior impingement due to fractured nonunited osteophytes can be confirmed with confidence on physical examination using the extension impingement test and the arm bar test.13 The extension impingement test is performed by starting with elbow near full extension and then quickly (but gently to prevent injury) snapping it into terminal extension. This maneuver reproduces the posterior or posteromedial pain experienced during provocative activities such as throwing. A simultaneous valgus load normally enhances the pain if the pathology is primarily posteromedial.
A similar test is the arm bar test, which is a variation of a martial arts maneuver. With the patient’s shoulder in full internal rotation, the examiner extends the elbow to its full limit and then (gently at first) hyperextends it. This is reproducibly performed with the patient’s shoulder in full internal rotation and 90 degrees of forward elevation. The patient’s hand is placed on the shoulder of the examiner, and the examiner pulls down on the olecranon, leveraging the elbow into extension. Reproduction of the patient’s pain is expected if impingement is present. I have found this test to be more sensitive than the extension impingement test if the patient’s symptoms are relatively minor or have diminished just before consultation.
Diagnostic Imaging
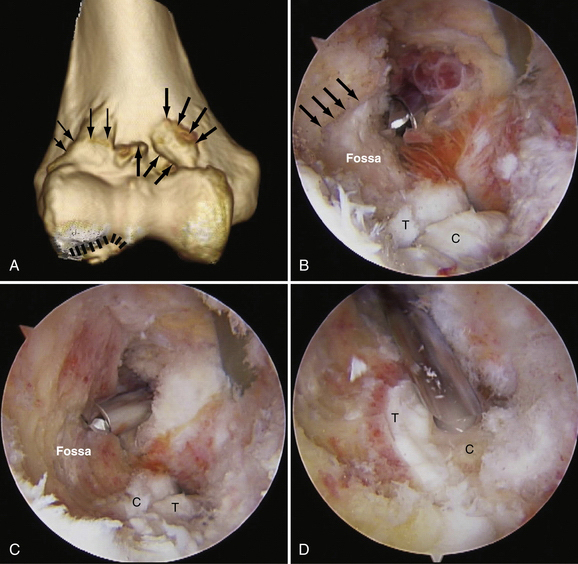
CT with three-dimensional surface rendering provides excellent imaging of the bony pathology (Fig. 9-2A). The individual bones can be isolated from each other and spun around in three dimensions, demonstrating the location and structure of each osteophyte and loose body. Two-dimensional sagittal and coronal reconstructions are also necessary, because they reveal the fine details not available in the three-dimensional images (see Fig. 9-2B), including nonunited fractures, the original floors of the fossae, and small loose bodies embedded in the cartilage surfaces. Axial two-dimensional reconstructions complete the imaging protocol.
TREATMENT
Alternative Surgical Treatments
Alternatives to arthroscopic osteocapsular arthroplasty include arthroscopic or open Outerbridge-Kashiwagi, open column, and open Tsuge procedures.6,8–12 In my experience, drilling a hole through the olecranon fossa does not adequately decompresses the coronoid fossa or the olecranon fossa, and it fails to address osteophytes in the radial fossa. It also eliminates the bony landmarks used to determine just how much bone should be removed from the fossa. The open column procedure does not permit as accurate and complete removal of osteophytes or contracted capsule (e.g., medial gutter) as the arthroscopic procedure. The Tsuge procedure has a high morbidity rate with no apparent advantages over arthroscopic osteocapsular arthroplasty.
Arthroscopic Technique
Arthroscopic osteocapsular arthroplasty is a complex procedure requiring a high level of experience in elbow arthroscopy for its safe and effective performance. I have learned by experience that it is best performed in a stepwise sequence, starting posteriorly and completing the work in the gutters before going anteriorly (Box 9-1).
Posterior Joint Compartment
Step 1: Get In and Establish a View.
The first step is to get in and establish a view. Place the scope in the posterolateral portal and the shaver in the posterior portal. Confirm by visualizing identifiable articular structures that you are inside the joint and that you have the correct anatomic orientation (see Fig. 9-2C). Touch the tips of the shaver and scope together by triangulation, and visualize the shaver blade. By using surface anatomic landmarks, it should be possible to verify the shaver is within the olecranon fossa. This can be confirmed by tactile feedback as the shaver is moved up and down the sides of the fossa and around its rim.
Step 2: Create a Space in Which to Work.
Creating a space in which to work involves synovectomy and removal of debris, scar tissue, and loose bodies so that the surgeon can see clearly (see Fig. 9-2D). The surgeon strips the capsule off the humerus proximally and removes remaining loose bodies. Adding a retractor through the proximal posterolateral or proximal posterior portal increases the space, just as retraction does with open surgery. Slight elbow extension helps.
Step 3: Bone Removal.
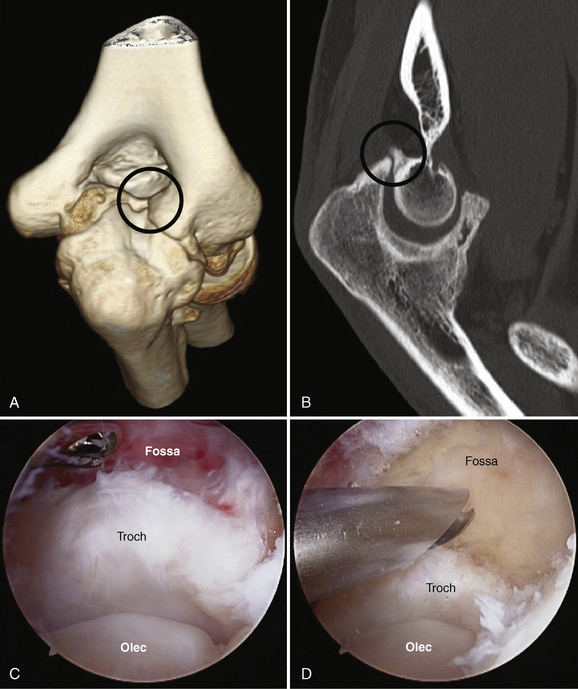
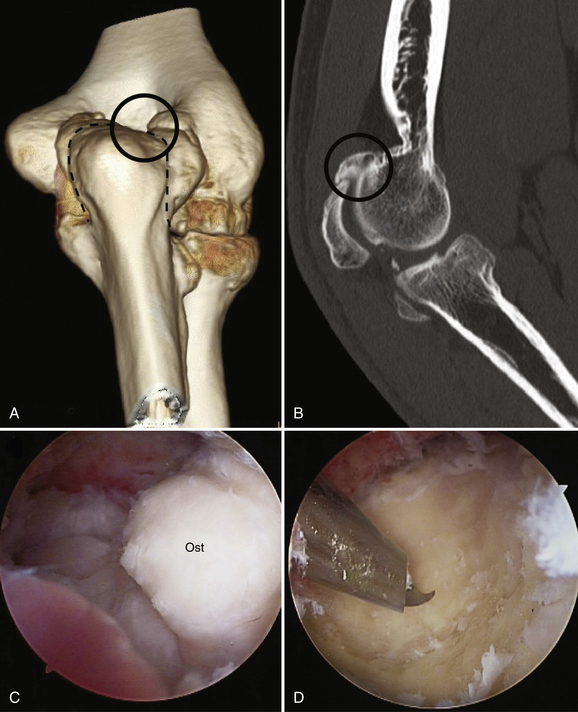
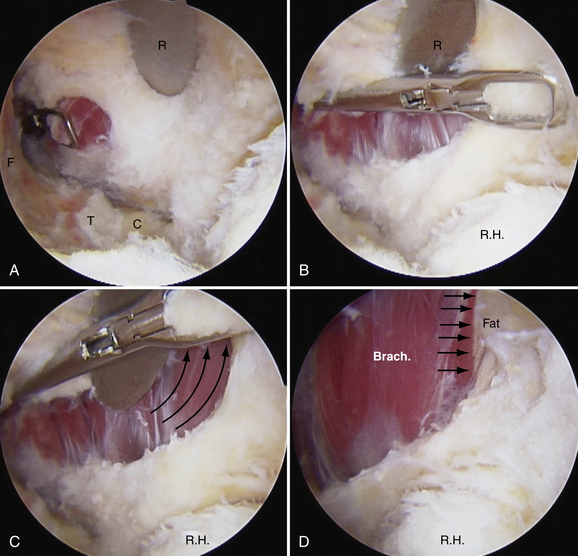
Bone removal is performed before capsulectomy (Figs. 9-3 and 9-4). It is helpful to use a retractor to hold the triceps away from the burr. In re-creating the olecranon fossa, the key is to find the original floor of the fossa. The preoperative CT scans are used to determine whether the original floor of the fossa is preserved and where it is. Except in the most advanced cases, it is usually partially preserved under the osteophytes.
When trimming the olecranon, avoid removing normal olecranon bone (i.e., take off only the osteophytes) in an overhead athlete to prevent increased strain in the medial collateral ligament during valgus stress. I usually do avoid using a burr on the medial corner of the olecranon, because it can wrap up the soft tissues and injure the ulnar nerve. I try to prevent this by changing to a shaver blade (4.8-mm Gator), which cuts rather than wraps or pulls tissue, after I pass the corner of the olecranon (Fig. 9-5). Fortunately, exposed trabecular bone (from having already cut into it posteriorly) is relatively easy to cut with a shaver blade.
Medial Gutter
The work in the medial gutter is performed with the arthroscope in the posterolateral portal and the shaver or working instrument in the posterior portal. Retractors can be placed through the proximal posterolateral or the proximal posterior portals (see Fig. 9-5D).
Step 1: Get In and Establish a View.
The key landmarks to identify are the medial edge of the ulnohumeral articulation and the posterior bundle of the medial collateral ligament, which appears as a series of corrugations or vertical bands within the posterior medial capsule.
Step 3: Bone Removal.
Extreme caution is necessary when using motorized instruments medial to the posteromedial corner of the olecranon. Beyond the posteromedial corner of the olecranon, I usually change from a burr to shaver blade, which avoids the risk of drawing tissues into the burr due to Bernoulli-Venturi effects (see Fig. 9-5B).
Step 4: Capsulectomy.
The posteromedial capsule must be released to restore flexion in elbows that lack flexion preoperatively. It can be released through a small incision over the cubital tunnel, which permits concurrent ulnar nerve decompression. Alternatively, the posteromedial capsule can be released arthroscopically if the surgeon has the skill and is fully knowledgeable of the three-dimensional location of the nerve in this area (see Fig. 9-5C and D).
Lateral Gutter
Work in the lateral gutter begins by switching the instruments so that the arthroscope is in the posterior portal and the shaver is in the posterolateral portal. It is helpful, but not always necessary, to use a retractor in the proximal posterolateral portal to retract the soft tissues at the posterolateral corner away from the olecranon and to open up the lateral gutter.
Anterior Joint Compartment
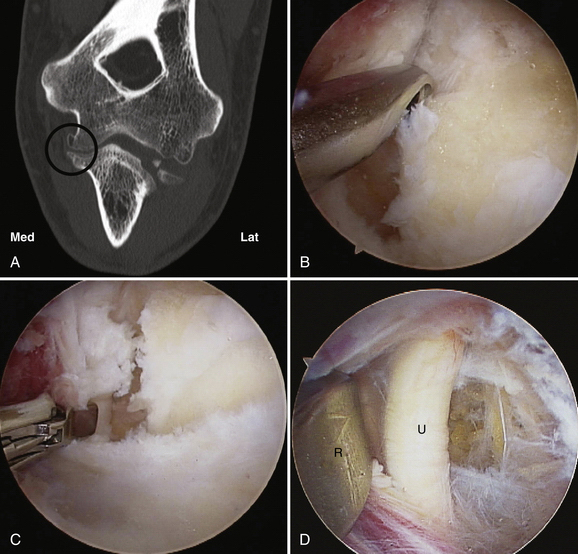
Three portals are routinely used for osteocapsular arthroplasty involving the anterior joint, and occasionally, a fourth is used. The anterolateral and proximal anteromedial portals are used for the arthroscope and working instruments, respectively, and the proximal anterolateral portal is used for a retractor. Occasionally, a second retractor is used, and it is placed in the anteromedial portal.
Step 3: Bone Removal.
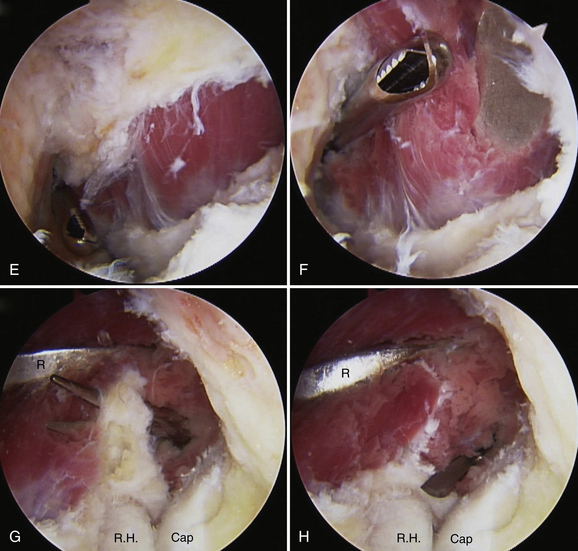
In re-creating the coronoid and radial fossae, the key is to find the floor of the fossa, which is usually at least partially preserved under the osteophytes (Fig. 9-6). Removing the periosteal soft tissue layer under the osteophytes exposes smooth cortical bone, which is readily distinguished from the overlying trabecular bone in the osteophytes. Bone debris is removed using the shaver, because it will not wash off the surface of exposed muscle with irrigation alone.
Step 4: Capsulectomy.
Anterior capsulectomy is performed by first releasing the capsule along the supracondylar ridges if this was not done during the stage of creating a space in which to work. The capsule is cut from medial to lateral aspects with a wide duckbill (i.e., duckling or punch biopsy) (Fig. 9-7). Release proceeds laterally to the lateral edge of the brachialis, indicated by a strip of fatty tissue surrounding the radial nerve (see Fig. 9-7D). The capsule is excised proximally on the medial side and centrally with the shaver disconnected from suction (see Fig. 9-7E and F). The remaining lateral capsule is divided with a fine, pointed scissors or other suitable instrument, and the proximal portion is excised (see Fig. 9-7G and H). I prefer to make the capsulotomy distally, where the interval between brachioradialis and extensor carpi radialis longus is readily identifiable, and I then excise the whole capsule. Some surgeons wisely recommend cutting the capsule more proximally, where the radial nerve is farther away. In either case, a small triangle of capsule may be left intact over the interval between the brachioradialis and extensor carpi radialis longus to protect the radial nerve. The capsular release must go right down to the collateral ligaments on each side for complete release.
PEARLS& PITFALLS
OUTCOMES
My experience has been that for the proper indications, the results are among the most reliable and gratifying for the patient and physician of any shoulder or elbow operation performed. Data should be available in the peer-review literature in the future.
1. O’Driscoll SW. Arthroscopic osteocapsular arthroplasty. In: Yamaguchi K, King G, McKee M, O’Driscoll S, editors. Advanced Reconstruction Elbow. 1st ed. Rosemont, IL: American Academy of Orthopedic Surgeons; 2007:59-68.
2. O’Driscoll S. The arthroscopic treatment of the stiff elbow. In: Celli A, ed. Treatment of the Elbow Lesions: New Aspects in Diagnosis and Surgical Techniques. New York, NY: Springer; 2008:211-219.
3. O’Driscoll SW, Savoie FH3rd. Arthroscopy of the elbow. In: Morrey BF, ed. Master Techniques in Orthopedic Surgery: The Elbow. 2 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:27-45.
4. Jones GS, Savoie FHIII. Arthroscopic capsular release of flexion contractures (arthrofibrosis) of the elbow. Arthroscopy. 1993;9:277-283.
5. Ward WG, Anderson TE. Elbow arthroscopy in a mostly athletic population. J Hand Surg Am. 1993;18A:220-224.
6. Redden JF, Stanley D. Arthroscopic fenestration of the olecranon fossa in the treatment of osteoarthritis of the elbow. Arthroscopy. 1993;9:14-16.
7. O’Driscoll SW. Arthroscopic treatment for osteoarthritis of the elbow. Orthop Clin North Am. 1995;26:691-706.
8. Ogilvie-Harris DJ, Gordon R, MacKay M. Arthroscopic treatment for posterior impingement in degenerative arthritis of the elbow. Arthroscopy. 1995;11:437-443.
9. Savoie FH 3rd, Nunley PD, Field LD. Arthroscopic management of the arthritic elbow: indications, technique, and results. J Shoulder Elbow Surg. 1999;8:214-219.
10. Cohen AP, Redden JF, Stanley D. Treatment of osteoarthritis of the elbow: a comparison of open and arthroscopic debridement. Arthroscopy. 2000;16:701-706.
11. Krishnan S, Pennington S, Burkhead W. Arthroscopic ulnohumeral arthroplasty for degenerative arthritis of the elbow in patients under the age of 50. Tech Shoulder Elbow Surg. 2005;6:208-213.
12. Adams JE, Wolff LH 3rd, Merten SM, Steinmann SP. Osteoarthritis of the elbow: results of arthroscopic osteophyte resection and capsulectomy. J Shoulder Elbow Surg. 2008;17:126-131.
13. O’Driscoll S. Valgus extension overload and plica. In: Levine WN, editor. Athlete’s Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2008:71-83.
14. Miller C, Jobe C, Wright M. Neuroanatomy in elbow arthroscopy. J Shoulder Elbow Surg. 1995;4:168-174.
15. Gallay SH, Richards RR, O’Driscoll SW. Intraarticular capacity and compliance of stiff and normal elbows. Arthroscopy. 1993;9:9-13.