Orthotics: evaluation, intervention, and prescription
HEIDI TRUMAN, CPO and WALTER RACETTE, CPO
After reading this chapter the student or therapist will be able to:
1. Identify and analyze the force systems produced by the use of an orthosis.
2. Comprehend the prescription rationale gained from an orthotic evaluation for individuals with neuromuscular dysfunctions.
3. Identify and differentiate the variables considered by the orthotist to optimize outcomes during orthotic intervention.
Overview
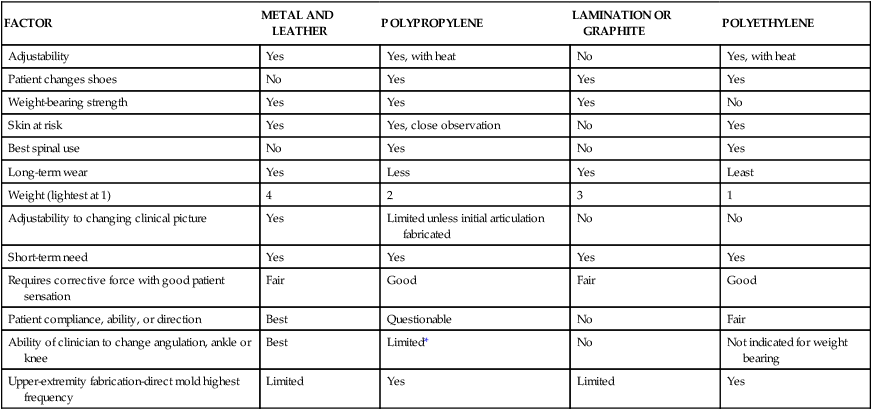
An orthosis is an external device that produces a force that biomechanically affects the body to correct, support, or stabilize the trunk, the head, and/or an extremity. The goals in patient care with orthotic use vary from temporary application to permanent usage to maintain improvement. Orthoses are named by the sections of the body to which they are applied. For example, an orthosis that controls and covers the ankle and foot is called an ankle-foot orthosis (AFO). The abbreviations for the device are used by professionals in clinical documentation. Many factors enter into the decision regarding use and type of orthosis, and these will be discussed later. It is essential that the least complicated and most cost-effective orthosis be applied to the patient. The rehabilitation team must build a priority list of desired outcomes and accept that sometimes all of the items on the list may not be achieved by either the orthosis or the patient-team combination. At the very least, care must be attempted in stages because the patient’s condition changes or other medical concerns may arise. For example, an excessive number of custom-made and custom-fit plastic AFOs have been issued because they are “more cosmetic and lighter” than AFOs made of metal and leather material. There are times when all higher-priority goals can be achieved so that down the list the goals of cosmesis and light weight can be considered (Table 34-1). However, in the case of neuropathy of the foot, significant risk would be incurred by providing a total contact AFO made of plastic to keep it lightweight. A double-upright metal AFO with a well-fitting extra-depth shoe with a custom accommodative insert would fit the patient’s needs and take into consideration the sensory and motor changes within the lower extremity. Effective coordination and communication between health professionals in development of patient goals is essential during the evaluation process. For example, a design criteria omission as simple as placing a loop closure on the side that the patient cannot reach will prohibit the use of the orthotic device. A sound understanding of biomechanical and orthotic principles as well as skilled patient management techniques must be used to be successful with patients who require orthoses.
TABLE 34-1 
COMPARISON OF METAL AND PLASTIC ORTHOSES
| FACTOR | METAL AND LEATHER | POLYPROPYLENE | LAMINATION OR GRAPHITE | POLYETHYLENE |
| Adjustability | Yes | Yes, with heat | No | Yes, with heat |
| Patient changes shoes | No | Yes | Yes | Yes |
| Weight-bearing strength | Yes | Yes | Yes | No |
| Skin at risk | Yes | Yes, close observation | No | Yes |
| Best spinal use | No | Yes | No | Yes |
| Long-term wear | Yes | Less | Yes | Least |
| Weight (lightest at 1) | 4 | 2 | 3 | 1 |
| Adjustability to changing clinical picture | Yes | Limited unless initial articulation fabricated | No | No |
| Short-term need | Yes | Yes | Yes | Yes |
| Requires corrective force with good patient sensation | Fair | Good | Fair | Good |
| Patient compliance, ability, or direction | Best | Questionable | No | Fair |
| Ability of clinician to change angulation, ankle or knee | Best | Limited* | No | Not indicated for weight bearing |
| Upper-extremity fabrication-direct mold highest frequency | Limited | Yes | Limited | Yes |
*Use in combination with metal joints produces best results.
The advancements in and access to medical technology have had a profound effect in the field of orthotics. The evolution of plastic, composite, and metals fabrication technology has dramatically improved the ability to control, support, and protect all areas of the human body. Today, patients are fit for custom and prefabricated orthotic devices that provide a variety of functions in both a timely and cost-effective manner. These factors have led physicians to routinely prescribe orthoses for a wide range of medical conditions, whereas in prior decades lack of availability and shortage of experienced orthotists restricted patient access and narrowed the use of orthoses.1 Orthoses are important options for postoperative management, acute fracture management, and adjunct treatment, in addition to more traditional uses. For many, the proliferation of the prefabricated orthosis signaled a dilution of quality orthotic care, but in reality it has had the opposite effect. These readily available, cost-effective orthoses have not taken orthoses out of the hands of the orthotist but rather have moved them into the minds of treating professionals. There has been continued growth of new and improved orthoses and expansion into other areas of treatment previously lacking in orthotic management. For example, positional and corrective orthoses can be used for premature and newborn infants, and a wide range of sizes of orthoses that previously were made only in adult sizes have become available for pediatric patients. As with any new technological advancement, there has been incorrect application and use. It is not that many of these prefabricated orthoses are difficult to apply; rather, there has been lack of a clear understanding of the indications, contraindications, and limitations these devices present to the orthotist and other health professionals such as occupational and physical therapists.
Advancements in technology have allowed the use of lighter, stronger materials in the fabrication of lower-extremity orthotics. Specifically, the substance called preimpregnated carbon is a graphite fabric with an exact amount of resin and catalyst already incorporated into the material. With the fibers properly directed over a model, it can be formed with heat. Graphite in other forms has been used in both prosthetics and orthotics for years. However, it had limited acceptance in orthotics because it did not significantly reduce the weight of the orthosis compared with other materials. It also lacked the properties to enable modification of the orthosis after the lamination process. The preimpregnated graphite has a dramatically reduced weight, still maintains its strength, and gives the orthotist the opportunity to use the dynamics of loading and response during the gait cycle. This allows for assistance in both the swing and stance phases of gait (Figure 34-1). A clinical example at the end of this chapter demonstrates this need in patient management.
Another significant advancement in component technology has been the introduction of weight-activated orthotic knee joints. Although available in prosthetics for decades, the development of a lightweight, compact knee joint that would allow a patient to have knee stability during stance2 and clearance during swing phase has been elusive until recently. Before this, the available knee joints for knee-ankle-foot orthoses (KAFOs) involved some type of locking mechanism that remained locked throughout the gait cycle. The joint provided stabilization of the weak quadriceps musculature during stance but kept the knee in a fully extended position, making advancement of the limb in swing more difficult for the patient. There are specific indications and contraindications for stance control KAFOs, but early results are promising. This feature can significantly reduce energy output,3 as it is not necessary to raise the center of gravity to clear the locked knee during swing phase. This improves patient safety when walking on uneven surfaces. New technology for externally powered knee orthoses has just entered the market. These “bionic legs” are robotic aids worn during therapy sessions for gait training. They assist and augment the strength of the patient’s muscle and are most typically used in post–cerebrovascular accident (CVA) rehabilitation. Once the patient has achieved functional improvements, the use of the orthosis is discontinued.
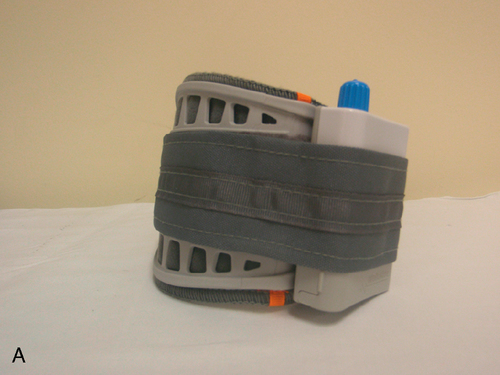
Other advancements in orthotic technology include the development of neuroprosthetic devices. These devices act through circuitry and programming to substitute for a deficit in the neural system. Functional electrical stimulation (FES) is a method of applying low-level electrical currents to motor nerves to restore function. In the 1960s the application of FES for foot drop was demonstrated by using a simple single channel to stimulate the common peroneal nerve to activate the ankle dorsiflexors. FES has widespread applications in many other neuroprosthetic devices such as cardiac pacemakers, cochlear stimulators, bladder stimulators, and phrenic nerve stimulators. Until recently, FES devices to provide ambulation assistance were large, unreliable, complex, and restricted to use in a therapy setting. The FES used in neurological rehabilitation attempts to unmask existing voluntary control (if any) and/or initiate dormant activity of the nerves and muscles. For FES to be used, the patient must have an upper motor neuron lesion. This means the nerve-to-muscle pathway is intact and the reflex arc is undamaged. Goals of FES address many rehabilitative outcomes. FES can reduce spasticity, synergy patterns, swelling, and blood clot formation as well as maintaining range of motion (ROM). FES used in gait can improve overall walking abilities by dorsiflexing the foot during swing to provide foot clearance, control initial contact, increase safety, decrease energy expenditure, and retrain muscles. FES has some application in the upper extremity as well, although at this time it is purely in a therapeutic setting. Currently, there are several FES units for foot drop on the market. These devices are used by patients in their daily lives and are not limited to the rehabilitation setting. The WalkAide from Innovative Neurotronics (Figure 34-2) and NESS L300 from Bioness (Figure 34-3) both function to provide dorsiflexion during the swing phase by stimulating the peroneal nerve. An ideal candidate for these devices must have an upper motor neuron lesion, good control of the knee joint, and drop foot. Common neurological conditions in which these devices are used are CVA and multiple sclerosis (MS). Both devices involve some sort of sensor to determine when the patient is initializing the swing phase of the gait cycle and send an electrical stimulus to the nerve to dorsiflex the foot. Advantages of functional FES over traditional orthotic management for foot drop are that it shifts an orthotic device from being a passive support to providing active assistance. FES stimulates the patient’s muscles to lift the foot, rather than acting as a passive splint to hold the foot.

 The NESS L300 Foot Drop System.
The NESS L300 Foot Drop System.Basic orthotic functions
Alignment
Alignment of the extremities and spine is a common function in orthotic prescription. The orthosis can provide either temporary or permanent function. A TLSO may be prescribed for stabilizing alignment after spinal fusion in the case of an unstable spinal cord injury (refer to Chapter 16). A supramalleolar orthosis (SMO) is commonly prescribed to hold the foot in proper alignment. When the goal of orthotic intervention is to correct alignment to a position well tolerated by the overlying soft tissue and/or the malalignment is a result of a muscle weakness, the new position should stabilize the joint. Clinicians need to remember that aligning one joint may result in the proximal or distal joint being placed in malalignment. An example of this is a genu valgum knee, which may seem easily corrected. However, changes in alignment result in adjustments by the other joints up and down the kinetic chain. Questions such as “Does the subtalar joint have the mobility to pronate?” must be asked and answered.
Evaluation
During evaluation, review of the diagnosis and gathering of patient history are extremely valuable. A complete medical diagnosis will indicate important information to the team. For example, if a patient with poliomyelitis is to be seen, the orthotist is aware that it is a lower motor neuron lesion and that proprioception is intact (see Chapters 17 and 35). These patients have the benefit of skeletal balance in standing and ambulation and therefore require durable orthotic construction. Compare this with a similar result in muscle testing and ROM assessment for an individual with T12 level paraplegia. Assuming this is a complete lesion, patients with this upper motor neuron lesion lack proprioception. They require other means to get feedback about standing balance and require a lightweight orthosis, as they rarely use orthoses as a major means of locomotion. Although gathering patient history is a vital part of the evaluation, it is, more importantly, an opportunity to establish a productive patient management environment. Patients and family members have important information regarding the initial injury, previous medical care, reasons they sought additional care, and desired outcomes of new treatment. Most of this information can be gathered efficiently as either the therapist or the orthotist begins other professional evaluations. These are important patient and family management skills. One must hear from the patient or family why they came to see the health care professional and their expectations of care. The therapist should not assume the family’s goals without asking, as often patient and family goals are higher than the clinicians’ expectations. Communicating at a level that is understandable both is vital and demonstrates to the patient and family that the therapist is a concerned professional, thereby engendering trust and confidence. Complete and timely documentation of these findings is becoming increasingly vital to the evaluation and treatment plan. Whether communicating with others on the rehabilitation team, insurance carriers, or legal professionals, documentation and building medical justification are essential in treating all patients.
Evaluation of the upper extremities
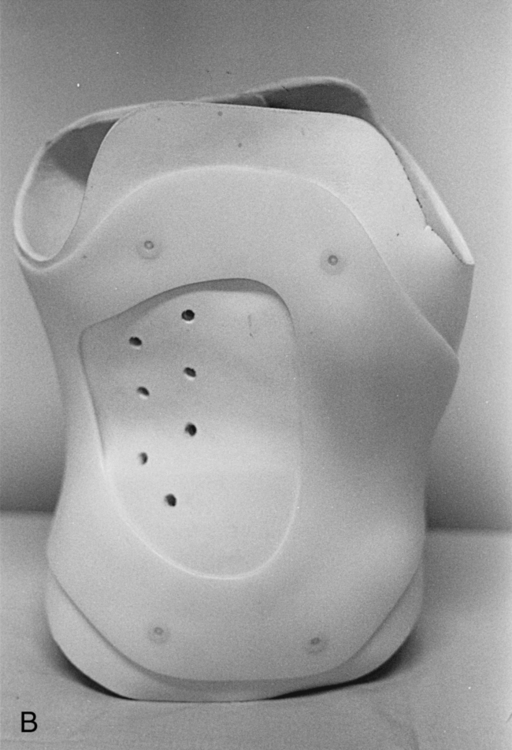
Evaluation of the upper extremities requires multiple inputs from health care professionals, patients, family, and teachers because of the wide range of specific functions an individual performs daily. Unique to the upper extremity, multiple functions generally require multiple orthotic devices for activities of daily living (ADLs). Typical functions of orthoses of the upper extremity include maintenance of functional wrist and hand position, reduction of contracture or tone, transfer of force available in one area to another, and support of subluxations resulting from denervation. It is common for the neurologically impaired patient to require several orthoses with different functions for use throughout the day. Strength, ROM, condition of soft tissues, and sensation are all important evaluation factors. In addition, ambulatory status, bilateral or unilateral condition, status of vision, and condition of the spine and head must be factored into the indications and contraindications in assessment of the orthotic needs of the patient. Much more critical muscle tests must be performed in the upper extremity as opposed to the lower extremity, as minor increases or decreases in strength will dramatically alter orthotic need. For example, the C5 quadriplegic has the ability to function with a wrist-hand orthosis by providing enough wrist extension to use the tenodesis effect, which can produce a three-jaw-chuck type of grip. The difference between a functioning and nonfunctioning orthosis is minor, not only because there is limited muscle strength, but also because minor inefficiencies in the tenodesis splint (from friction or malalignment) could reduce function to below acceptable levels. Patients with unilateral involvement have far different needs than the bilaterally involved. The patient with a CVA with unilateral involvement may have an intervention of a positional wrist-hand orthosis to prevent contracture and injury and a supportive shoulder orthosis to prevent shoulder subluxation (Figures 34-4 and 34-5). In these cases the other extremity becomes dominant, and there is little need to fabricate complex orthoses for the use of the affected extremity. The patient with bilateral involvement presents a much different picture. Consideration for grooming, feeding, mobility, and so on must be factored into the desired expectation during evaluation. The case of the patient with neurological impairments who requires orthotic intervention is complex, as this patient typically has involvement in the trunk, head, and lower extremity. These patients require specialized wheelchairs and seating systems. Evaluation is most effective with all rehabilitation team members present to establish a treatment plan. Orthotic treatments maximize what limited muscle strength and ROM the patient may have. Orthoses that are used during the day to maximize function are often replaced with positional orthoses at night to preserve gains and prevent decline in ROM. The occupational therapist provides most of the functional and positional orthoses for the upper extremity. In today’s rehabilitation environment, many occupational therapists work directly with orthopedic hand specialists and trauma physicians. They use low-temperature materials to mold custom devices specifically designed for protecting surgical reconstruction or promoting or maintaining ROM or for use as assistive devices.

 Resting hand splint.
Resting hand splint.Orthotic intervention
Several factors play key roles in the success of orthotic intervention. To improve function without complication or patient risk, the clinician must be sure to address the patient’s major complaint; the reason the patient and family came to see the therapist or orthotist must be clearly established to ensure compliance with orthotic intervention. It is important to establish a baseline of function so that results of intervention are measurable. In some situations the patient benefit is clear and immediate, whereas in others, concentrated instruction, orthotic modification, and time are required before improved function can be observed or measured. The process of donning and doffing the orthosis as independently as possible enhances the overall goal for the patient and family and must be well thought out by the experienced clinician. The clinician must be conservative in setting these expectations. It is important to remember that what happens in the clinical setting may not be easily reproducible in the home situation. The orthotic interventions must be kept as simple as possible: what is the least amount of orthotic intervention that will provide the expected goal? Although an obvious statement, the balance between too much and not enough can challenge the clinician’s skill and experience. The use of trial orthoses can provide valuable information during the evaluation, and these are generally available commercially for short periods. Various types of heat-moldable plastics have been beneficial for many individuals. At times, however, their use adds risk and complication without improvement compared with traditional AFOs fabricated with metal and leather attached to the patient’s shoe. For example, if the patient requires ankle and knee stability yet lacks sensation in the foot and ankle, the double-upright metal orthosis attached to the patient’s shoe creates much less risk for possible skin breakdown than a rigid total contact plastic orthosis (see Table 34-1). With a plastic orthosis, the family must find a shoe big enough to easily fit the orthosis. Technological advancements have led to a number of additions to the arsenal of orthotists. Prefabricated orthoses with better sizing and materials have given the clinician additional tools for evaluation and for devising permanent orthoses. Preimpregnated graphite AFOs are now available in multiple sizes and provide toe pickup during swing phase and some knee-stabilizing characteristics during stance phase. Although very lightweight, these orthoses provide dynamic stance phase control. Introduction of biomechanical forces to the extremities may cause unwanted movements or restrictions, and careful selection of components is essential to keep the focus on the orthotic plan. For example, a patient with a CVA may need more anterior lever force to provide knee stability, so one would plantar flex the orthotic ankle joint. However, this knee-stabilizing effect in stance phase would cause a toe drag during swing phase. A simple fix is to provide the opposite side with a ¼-inch heel and sole lift for additional clearance during swing phase of the affected extremity (Table 34-2).
TABLE 34-2 
INDICATIONS FOR COMMON ORTHOTIC MODIFICATIONS AND ADDITIONS
| MODIFICATION OR ADDITION | DESCRIPTION |
| SACH modification | This modification is done by cutting out a triangular wedge in the heel of the shoe and inserting a softer material. The solid ankle cushion heel (SACH) modification is used to dampen the effect of the heel or posterior lever arm at heel strike. This force produces an anterior force to destabilize the knee, which may be undesirable. |
| Heel and sole buildup | Adding a ¼-inch heel and sole buildup to the unaffected side can create additional swing clearance needed on the affected side. This modification is indicated if additional dorsiflexion of the orthotic joint creates knee instability or if the patient lacks dorsiflexion range of motion. |
| Rocker-bottom heel and sole modifications | There are several different styles of rocker-bottom buildup. Although the roll built into this modification may differ, the basic results are the same—to add motion and translate the center of gravity forward when the ankle and/or knee joint is locked. |
| Long tongue stirrup, extended steel shanks | A stirrup is the metal attachment to the shoe. The use of a long tongue (a steel extension that goes distally between the bottom of the shoe and the heel and sole) is necessary to transfer the force created by restriction of ankle motion. Without this type of fabrication, the force produced at midstance will not be controlled. A steel shank produces the same control but is not part of the stirrup and may be used in combination with a rocker bottom. |
| Medial or valgus control T-strap; lateral or varus control T-strap | These straps, leather on traditional double-upright orthoses or plastic or padding control T-strap modifications on plastic AFOs, produce a force to reduce valgus (a medial T-strap) or varus (a lateral T-strap). A medial T-strap attaches to the shoe medially, and the beltlike strap goes around the lateral upright and is tightened. The lateral T-strap attaches to the lateral side of the shoe and applies a medially directed force by being tightened around the medial upright of the AFO. |
| Heel buildup | A heel buildup is used to accommodate heel cord tightness. The tibia must be at least 90 degrees to the floor for safe balance and ambulation. Common signs of the need to build up the heel are genu recurvatum and the heel slipping out of the shoe. The amount of heel buildup must be matched with the same heel and sole buildup on the opposite side for balance. |
| Instep or figure-of-8 straps | This orthotic modification is used to keep the heel seated in the shoe or plastic ankle-foot orthosis when a tight heel cord is present. These straps fit across the dorsum of the foot with a posterior attachment point. |
| Swedish knee orthosis | This prefabricated knee orthosis is an effective method to prevent genu recurvatum. It is typically indicated after a CVA for the patient who lacks proprioception and whose knee hyperextends, creating pain and slackening the knee ligaments. It can be used temporarily as a training orthosis or on a more definitive basis when persistent pain and instability are present. |
Clinicians need to set realistic, manageable patient-centered treatment goals. All too often, treatment plans are only in the minds of the clinicians and are either never or too poorly communicated with the patient and family. Clinicians should assume that the patient and family members will expect benefits of the intervention that will far exceed what the therapist knows are possible. The time to address those gaps is certainly before treatment, not when the patient and family realize that expectations regarding functional gains may not be realistic. If failure is the reason a patient recognizes that the intervention was wrong, the therapists have lost the patient’s trust and the potential for future intervention guidance. Discussing realistic achievable goals of treatment, after assessing all factors, the home situation, and individual motivation, with the patient and family in language they understand is critical if successful orthotic intervention is to be achieved. The goal of orthotic care for a patient with CVA is to provide safe standing balance for transfer and minimal ambulation in the home. Patients and their families will realize the major benefit this will have on the home situation. However, without this identified as the goal before orthotic care, they may leave the therapeutic environment wondering why the patient cannot walk normally and participate in life activities that require longer distance ambulation skills.4 This clinical error is an all too frequent patient management mistake. Integrating orthoses with physical and occupational therapy motor relearning and neuroplasticity should help optimize functional recovery.
To provide a cost-effective orthosis in a timely manner with today’s vast number of orthotic devices, the orthotist must stay abreast of the wide array of choices at his or her disposal to meet the needs of the patient. The reality of cost containment is not a recent event in the orthotic profession, as funding for these devices has always been challenged. This has necessitated the development of more cost-effective alternatives, such as the prefabricated orthosis. The introduction of heat-moldable plastics into orthotics in the late 1960s and early 1970s on a custom basis replaced, to a large extent, the need to mold leather and/or metal to fabricate an orthosis (see Table 34-1). This improved the total contact fit and dramatically reduced the time and skill level required for manufacturing. Today’s orthotist has a multitude of devices from which to choose to meet the needs of the patient. Options range from custom-made devices using a patient mold to prefabricated custom-fit devices. A thorough understanding of the indications and contraindications for each of these devices is essential in order to meet patient needs. A lack of understanding of biomechanical principles, of the limitations of prefabricated orthoses, and of custom fitting can lead to failure and increase the impairment problems existing within the patient environment. All orthoses produce a force field, some desirable and some undesirable. It requires an experienced clinician to make the most appropriate choices, as too often the failure of treatment is blamed on an orthosis. Usually such failure is the result of an inappropriate initial selection of orthotic components, lack of discernment between custom-made and custom-fit devices, or misidentification of the patient as an orthotic candidate. Prefabricated custom-fit orthoses are cost-effective only if they produce the desired goal over time. As a general rule, one should consider prefabricated custom-fit orthosis for patients who have an anatomically “normal” biomechanical structural environment and who will use the orthosis for only a short time. Custom-made orthoses for extremities or the spine are usually prescribed for patients who have deformity or unusual size or who must use the device indefinitely.
Clinical examples
Paraplegia
Orthotic intervention for a patient with paraplegia is generally considered for the lower extremities at the T12 level in the complete lesion.5 Complete lesions higher in the cord leave the patient without enough trunk stability to use bilateral orthoses effectively. Although a thoracic extension can be added to bilateral KAFOs, this addition greatly increases the difficulty of donning the orthosis independently, and most patients will have great difficulty getting from sitting to standing.
The most appropriate orthoses for a T12 complete paraplegic are bilateral KAFOs. The patient generally uses a swing-to or swing-through gait, and successful use of orthoses requires excellent standing balance. There are three significant design requirements for these KAFOs: shallow thigh and calf bands, bail or French knee locks, and double-adjustable ankle joints. A double-adjustable ankle joint has channels on the anterior and posterior sides of the joint. This allows the orthotist to easily adjust dorsiflexion and plantarflexion position and ROM, or even provide dynamic assistance via a spring added to the channel of the joint (Figure 34-6). The shallow bands force the center of gravity forward, inducing lordosis so the patient can rest on the iliofemoral or Y ligaments of the hip. The knee joint locks are automatic because the patient requires the upper extremities for standing. The bail or French joint will lock as the patient stands and bends over the rigid ankle joint, forcing the knee joints into extension. The lock then can catch on the back of a wheelchair seat or other chair to release the lock and bend at the joint when the patient sits. The foot-ankle complex forms the basis for balance. A few degrees of adjustment at the double-adjustable ankle joint can make the difference between safe standing balance and limited standing balance. The long tongue stirrup extends at least to the heads of the metatarsals and farther if the patient is taller and heavier than normal (see Table 34-2). The use of a strutter bar from the upright of the stirrup extending to a transverse bar at the heads of the metatarsals with a long tongue stirrup (Scott-Craig design, Figure 34-7) ensures that the necessary rigidity is provided. A point between effective standing balance and ambulation is reached after training and ankle adjustment. Patients must have full ROM at the hips, knees, and ankles for use of these devices to be successful.
Hemiplegia
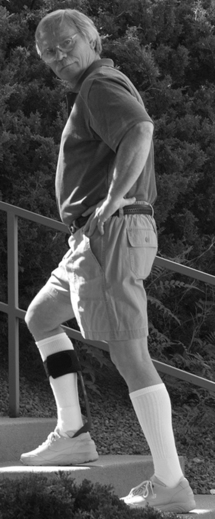
Patients who have had a CVA can vary widely in their need for orthotic intervention, from a simple AFO to assist toe clearance, to an AFO to stabilize both ankle and knee, to an orthosis used temporarily for training purposes.6,7 The use of a KAFO in the patient with hemiplegia is rarely indicated. Even though the more affected patient does not have knee stability, he or she rarely ambulates with a heel strike that would destabilize the knee and therefore can use an AFO with an anterior limited-range ankle joint. In addition, patients cannot don the KAFO with the use of only one upper extremity. With hip flexor weakness and knee instability on the affected side, the orthotic intervention may be to assist in transfers rather than to facilitate gait. As a general rule, orthotic intervention for the client with a CVA ranges from a static toe pickup orthosis to a double-adjustable ankle joint with the ankle locked. The use of dynamic components is not effective, because they will initiate spasticity. The lack of ROM into dorsiflexion or even to neutral causes the most significant problems for these patients. An ankle that lacks dorsiflexion ROM prevents advancement of the center of gravity and produces a lever arm that induces genu recurvatum and pain, and either the heel comes out of the shoe or the ankle rolls into varus. Because these patients lack proprioception, this constant force directed posteriorly will, over time, be significant. The patient will develop pain in the knee and not ambulate, the heel cord will shorten more, and the cycle will continue. Heel cords rarely gain length after the patient has been discharged from the rehabilitation setting, and one must consider the family and home situation. Heel buildups on the affected side are used to bring the tibia into 90 degrees. Buildups of 1 to 1½ inches are not uncommon. Remember to balance the opposite shoe. When selecting between different orthotic components, it is best to choose the more stable orthosis. The use of trial orthoses during evaluation is invaluable and helpful initially. As the patient improves, he or she may require less orthotic management or no orthosis at all. A three-point pressure orthosis for the knee, such as a Swedish knee cage (Figure 34-9), is also a valuable training orthosis and, in the case of some post-CVA patients, is used daily when the degree of recurvatum exceeds the patient’s ability to control the posteriorly directed force. The stirrup (the metal attachment to the patient’s shoe) of the AFO must be firm and extend under the sole and heel to the heads of the metatarsals. Although this adds weight to the orthosis, it is necessary to transmit knee-stabilizing forces. Stirrups attached under the heel will only allow undesirable motion and will not provide the required stability.
Spastic diplegic cerebral palsy
The goals of orthotic intervention in the patient with cerebral palsy are to control tone, prevent contractures, and provide a secondary support after a surgical procedure.8 Orthotic intervention for these individuals varies from region to region. As a general rule, the orthosis used to prevent contracture should be different from the orthosis used for ambulation. Some of the new designs incorporate modules that can key into one another or be used separately. This feature allows flexibility, assists in donning (especially in a patient with spasticity), and meets several treatment objectives. Modular articulating joints with various settings and functions to use with thermoplastic orthoses greatly increase the options that are available today. With the goals of orthotic intervention stated earlier, total contact–type orthoses are generally the desired option. As with any total contact orthosis and hypersensitive or hyposensitive skin, a cautious balance between correction or holding and skin tolerance must be reached. The fitting of and follow-up for these types of orthoses require experience, knowledge, and patience. Combinations of padding, wedging, straps, and heat relief methods are often necessary to enable the patient to wear the orthosis for a significant amount of time on a daily basis. A patient with spastic diplegic cerebral palsy relies heavily on her or his orthosis and wears it out faster than most other orthotic patients. In the case of a child, she or he may grow out of the orthosis before it wears out. This should be considered in the design and fabrication.
Multiple sclerosis
As MS progresses and further demyelination occurs, increased interruption of normal nerve impulses creates deficiencies in muscle control, vision, balance, sensation, and mental functions. Orthotic considerations for a patient with MS can vary as the patient’s symptoms fade, recur, and change over the years with the disease. Clinical presentation may vary from month to month. Fatigue plays a major role in the symptoms, and the patient’s expectations and willingness to use orthotic devices ebb accordingly. Typical patient reaction is reluctance to use any form of ambulatory aid or orthosis until safety is a major issue. Patients and family usually seek help when falls become more frequent. Lack of toe clearance during swing phase and poor knee stability and push off in stance phase are the most common problems that can benefit from orthotic intervention. Because of the nature of symptom fade and recurrence and the increase with fatigue, the weight and simplicity of orthotic intervention must be major considerations. In many instances the evaluation will indicate the need for a KAFO, but this will be rejected by the patient because of its weight and complexity. The benefit of the KAFO for knee stability and foot and ankle control is counteracted by the patient’s inability to advance the limb during swing phase and control the extremity, as well as a perception that he or she does not need that type of control. Most patients also will reject the use of a double-upright, double-adjustable metal orthosis for the same reason, and although their strength varies from day to day, they will judge need when they are at their strongest rather than their weakest. Traditionally, plastic AFOs are used to control foot drop and provide some medial and lateral ankle control. These orthoses also can provide some knee stability if the plastic is robust enough and if the medial and lateral trim lines are advanced anteriorly past the malleoli. This anterior force stops the center of gravity’s forward progression at midstance, and, again, many patients reject this type of orthosis. The recent development of prefabricated AFOs made of graphite has met the needs of many of these patients (Figure 34-14). This ultralight orthosis fits inside the patient’s shoe. It will provide toe clearance during swing phase and some dynamic knee stability and push off during stance phase.