13
Orthopedic Pharmacology
1. Discuss pharmacokinetic concepts, including absorption, distribution, metabolism, excretion half-life, and duration of action, and their relationship and significance to rehabilitation therapies.
2. Discuss pharmacodynamic concepts including the dose–response relationship, therapeutic window, adverse drug reactions, toxicity, tolerance, withdrawal, and addiction.
3. List the general principles of safe medication use and the physical therapist assistant’s role in optimizing patient safety.
4. Discuss general principles of treatment and prevention of orthopedic infection including why such infections are difficult to treat and importance of antibiotic compliance.
5. Discuss the analgesics best suited for different types of pain.
6. Discuss how opioids work differently from antiinflammatory analgesics in the treatment of pain.
7. Discuss common side effects and precautions associated with opioids, acetaminophen, nonsteroidal antiinflammatory drugs, cyclooxygenase-2 inhibitors, and corticosteroids.
8. Discuss the risk of acetaminophen overdoses during pain management.
BASIC PRINCIPLES OF PHARMACOLOGY AND SAFE MEDICATION USE
Pharmacokinetics
Simply put, pharmacokinetics is a term used to describe what the body does to a medication. The four pharmacokinetic phases are (1) absorption, (2) distribution, (3) metabolism, and (4) excretion.7
Absorption describes how the medication moves from its site of administration into the systemic circulation (into the bloodstream). Some common routes of administration are shown in Table 13-1. Most medications must move from the site of administration into systemic circulation to be effective. Others, such as topical creams or inhalers, may provide therapeutic benefits through a localized effect. Although systemic absorption may not be necessary for effectiveness of topically applied medications, it can occur and result in side effects. For example, high dose, long-term use of inhaled corticosteroids to treat asthma has been shown to result in enough systemic absorption to increase the risk of developing osteoporosis.12,15
Table 13-1
List of Common Routes of Administration
| Route | Description | Example Medication(s) |
| Oral (PO) | Swallowed; uses the gastrointestinal tract | Most commonly used route of administration in U.S.; tablets, capsules, oral liquids |
| Sublingual (SL) | Under the tongue; medication rapidly absorbs into systemic circulation | Nitroglycerin tablets for chest pain |
| Rectal | Administered through the rectum; some absorb into systemic circulation, others provide a local laxative effect |
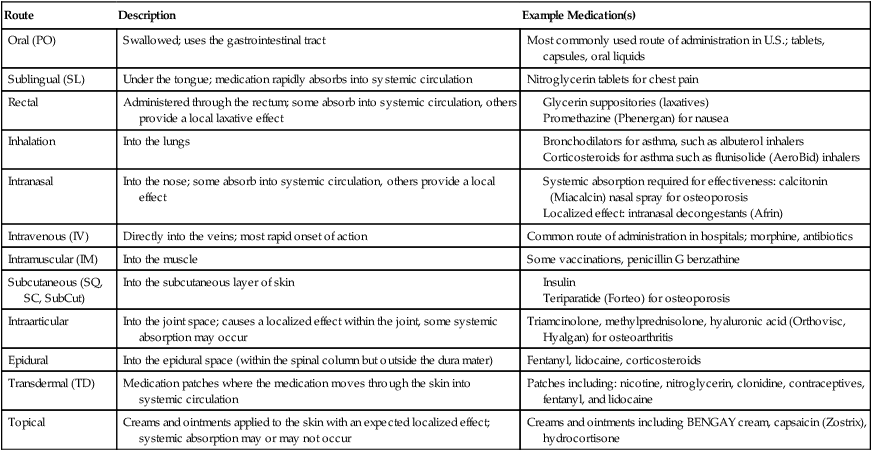
The rate and extent of drug absorption through the skin can be dramatically increased by application of heat; therefore heat generating modalities (e.g., heating pads, ultrasound, infrared lamps, and warm hydrotherapy) should not be applied near transdermal medication patches. Electromagnetic (e.g., ultraviolet radiation, lasers, and diathermy) and electrical current modalities (e.g., transcutaneous electrical nerve stimulation [TENS]) should also not be used near medication patches because many patches have metallic backings that conduct electric currents, leading to significant heat generation and burns.3
Medications are cleared from the body through metabolism, excretion, or both. Metabolism is the biotransformation or chemical alteration of the medication. The byproduct of drug metabolism is called a metabolite. Through metabolism, some medications are inactivated, whereas others remain active (active metabolite) but are more water soluble for easier elimination by the kidneys. Generally, metabolism takes place in the liver but it can occur through enzymatic processes in the kidneys, lungs, and bloodstream. Differences in drug response, side effects, and safe dose can be greatly affected by genetic differences in drug metabolism.21
Pharmacodynamics
Simply put, pharmacodynamics is a term used to describe what the medication does to the body. It is a study of the relationship between the amount of drug in the body and the response observed.7 Pharmacodynamics include a wide variety of principles, such as the dose–response relationship, therapeutic window, adverse reactions, and toxicity.
Tolerance occurs when the reaction to a drug diminishes over time. Tolerance can occur to both the benefits of a medication (making it less effective over time) and the ADRs (making it better tolerated over time).4 Withdrawal symptoms indicate physical dependency and are expected to occur with certain medications when used over a prolonged period. Withdrawal symptoms are generally the opposite of the pharmacologic effects of the medication. For example, one withdrawal symptom of a medication used to lower blood pressure would be hypertension.
Psychological dependency, also called addiction, occurs with certain medications such as opioid analgesics, amphetamines, and benzodiazepine sleep aids, as well as other substances with abuse potential, including cocaine, heroin, alcohol, caffeine, and nicotine. Withdrawal symptoms do contribute to the development of addiction in that the patient continues to use the substance to avoid the unpleasantness of the withdrawal symptoms; but having withdrawal symptoms alone does not meet the definition of addiction. It is important to understand the difference between physical and psychological dependency.4 Psychological dependency and addiction involve strong cravings and desires for the drug that overwhelm daily life. There is a loss of control over its usage and use continues despite its negative impact on quality of life.4,6 Drug addiction is most strongly associated with medications that rapidly distribute into the CNS causing high levels of euphoria and dysregulation of the neurotransmitters involved in the body’s natural reward and pleasure centers.
Principles of Safe Medication Use
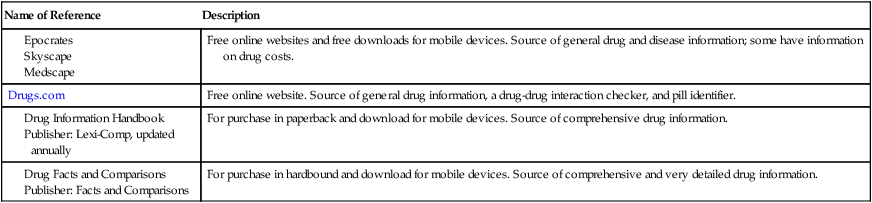
Although PTAs are not involved in the decision-making process regarding prescription and over-the-counter (OTC) medication use, having a general understanding of commonly used medications and knowing where to look for more information can help the PTA identify medication-related problems that should be brought to the attention of the prescriber or other health care team members. PTAs often spend more time with patients during therapy sessions than a prescriber spends with the patient during a typical office visit. This may provide opportunities to identify problems with compliance, lack of medication knowledge, ADRs, and lack of drug effectiveness. A variety of drug information resources exist that can be helpful in providing information, such as mechanism of action, dosing, therapeutic uses, and ADRs. See Table 13-2 for a list of helpful drug information resources. Although such resources exist, the PTA must be cautious about providing specific information to the patient that would be considered outside the PTA’s scope of practice.
Table 13-2
The following general principles of safe medication use can be provided to any patient:
 Keep a current list of all medications including prescription, OTC, and herbal
Keep a current list of all medications including prescription, OTC, and herbal
 Keep medications in their original containers
Keep medications in their original containers
 Never take some else’s medication
Never take some else’s medication
 Take medications exactly as directed
Take medications exactly as directed
 Do not start or stop medications without consulting the prescriber
Do not start or stop medications without consulting the prescriber
 Report any new symptoms to the prescriber
Report any new symptoms to the prescriber
 Don’t chew, crush, or break any capsules or tablets unless instructed
Don’t chew, crush, or break any capsules or tablets unless instructed
 When measuring liquid medications, use only the measuring device provided
When measuring liquid medications, use only the measuring device provided
MEDICATIONS TO TREAT AND PREVENT ORTHOPEDIC INFECTIONS
Antibiotic use in the treatment and prevention of orthopedic related infections is common. Antibiotics are medications with the ability to kill or inhibit growth of bacteria. Common examples of antibiotics used in the hospital and outpatient orthopedic settings are listed in Table 13-3. Orthopedic infections can result in slowed recovery, permanent joint damage, amputation, nonunion in cases of fracture, removal of implanted hardware, and death due to sepsis. Appropriate antibiotics are selected, taking into account the type of documented or suspected bacterial pathogens, the drug’s ability to distribute adequately to the site of infection, patient allergy history, side effects, and cost. Because the risk of infection following orthopedic surgeries is high, antibiotics are routinely administered before the procedure to reduce the risk of infection-related complications. The use of antibiotics to prevent an infection is referred to as prophylaxis.
Table 13-3
Common Antibiotics Used to Treat and Prevent Various Types of Orthopedic Infections∗
| Drug Class | Specific Antibiotics |
| Penicillins |

MEDICATIONS TO TREAT PAIN AND INFLAMMATION
The Joint Commission has emphasized pain treatment as a responsibility of health care providers and a patient’s right by requiring routine pain assessment as the “fifth vital sign.” It is recommended that regular assessment and documentation of pain severity, functional ability, progress towards achieving therapeutic goals, and presence of ADRs occur in both children and adults.1,6
Types of Pain
Neuropathic pain results from damage to or dysfunction of nerves. Examples include nerve compression, fibromyalgias, diabetic neuropathy, postherpetic neuralgia, spinal cord injuries, and phantom pain following amputation. Neuropathic pain is relatively resistant to opioids, acetaminophen, and antiinflammatory agents, although they may be helpful in certain cases. The most effective medication to treat neuropathic pain will vary by patient. The medications that tend to be most effective in treating neuropathic pain are medications that slow or block nerve conduction. Antidepressants such as duloxetine (Cymbalta), amitriptyline (Elavil), desipramine (Norpramin), venlafaxine (Effexor), and others are commonly used, as are anticonvulsants such as pregabalin (Lyrica), gabapentin (Neurontin), carbamazepine (Tegretol), and others. Effective topical products include lidocaine (Lidoderm) patch and capsaicin (Zostrix) cream.13,19,20 The opioid analgesic, tramadol (Ultram), is also often used to treat neuropathic pain because it is an opioid analgesic with additional antidepressant-like properties on nerve conduction.
Acute pain occurs following injury to the body and generally disappears when the injury heals. Chronic pain continues past the normal time of expected healing, which is assumed to be about 3 months.6,11 Persistent pain, whether acute or chronic, generally responds better to around-the-clock dosing rather than on demand dosing (also called prn dosing or as needed dosing). Many types of inflammatory pain as well as neuropathic pain are chronic rather than acute. Opioids, acetaminophen, and NSAIDs have quick onsets of action, within minutes to hours, whereas drugs for neuropathic pain, such as antidepressants and anticonvulsants, generally are not effective for several weeks. Ideally, when treating persistent chronic pain, patients are prescribed medications with a long duration of action and/or sustained release products to prevent the need for frequent daily administration. Patients may then take a shorter-acting analgesic or immediate release product for breakthrough pain. Breakthrough pain is pain that occurs despite the use of regularly scheduled pain medications.6
Opioid Analgesics
Opioid analgesics are all chemically related to opium. Commonly used prescription opioid medications include morphine, oxycodone, hydrocodone, and codeine. See Appendix A for others. Opioid analgesics work within the CNS to block the transmission of pain and create a feeling of euphoria. It is important to note that although pain is relieved, the underlying disease process or cause of the pain is not altered. Opioids are the most powerful medications available for treatment of nociceptive pain; they are also effective for some patients with neuropathic pain. IV opioids are more commonly used for inpatient settings for moderate to severe acute pain. Oral agents can be used for mild, moderate, or severe acute or chronic pain in any setting. Opioids are sometimes administered epidurally to provide highly effective pain control directly upon the spinal cord. Fentanyl (Duragesic) is available as a transdermal patch that provides control of severe, chronic pain.
Side effects of the opioid analgesics include nausea and vomiting (take with food to minimize risk), allergic reactions, sedation, drowsiness, dizziness, constipation, hypotension and orthostatic hypotension, slowed heart rate, slowed respiration, impaired judgment, physical dependence, and addiction.14 Several of these side effects reduce the patient’s safety and may increase risk of falls and injury. Constipation caused by chronic opioid use is extremely common but can be treated and prevented with over-the-counter stool softeners and mild laxatives including senna, docusate (Colace), and bisacodyl (Dulcolax) tablets.
Health care providers and patients alike may overestimate the risk of developing addiction when managing pain with opioids. This misperception can lead to inadequate pain control through underprescribing or underdosing, and patients skipping doses or “taking as little as possible.” The actual risk of developing opioid addiction following chronic use for medical management of pain is difficult to assess, but has been estimated at approximately 0.2% (2 in 1000) for persons with no prior history of substance abuse, and 3.3% (33 in 1000) for the general population.8
Tolerance and physical dependency are likely to occur with chronic use and are not equivalent to addiction. Although certain behaviors may seem like warning signs of addiction, the PTA should not make assumptions. Behaviors such as aggressively complaining about pain, occasionally taking more than prescribed, drug hoarding during periods of reduced pain, openly acquiring similar drugs from other medical resources, reporting unintended psychiatric effects, and resistance to changes in therapy are not necessarily signs of addiction. These behaviors are equally likely to occur in nonaddicted patients experiencing tolerance, an increase in pain level, poorly controlled pain, and anxiety related to a return of pain.18 Prescribers must balance the legitimate medical need for opioids in patients with chronic pain with the possibility of addiction and abuse.6
Acetaminophen
Acetaminophen is the most commonly used OTC fever reducer and analgesic. It is effective for a variety of noninflammatory, mild to moderate, acute, and chronic types of pain, including headaches, toothaches, sinus pain, back pain, osteoarthritis, and many others. Its mechanism of action is somewhat unclear but likely involves inhibition of prostaglandins and cyclooxygenase (COX) and some CNS activity.2 Although it affects prostaglandins and COX, it does not have strong antiinflammatory properties and is not an NSAID.
Many oral opioids also contain acetaminophen. Acetaminophen tablets come in regular strength (325 mg per tablet) and extra strength (500 mg per tablet). Per OTC package instructions, the typical adult dose is two tablets every 6 hours.14 For the regular strength tablets, this dose will equal 2600 mg/day; for the extra strength tablets, this dose will equal 4000 mg/day.
Acetaminophen has a strong record of safety when used at normal doses in healthy people. As compared to NSAIDs, acetaminophen is the safest OTC analgesic in patients with a history of gastrointestinal bleeding, congestive heart failure, hypertension, and patients taking the oral anticoagulant, warfarin (Coumadin). The major health concern with chronic acetaminophen use is hepatotoxicity (liver toxicity). Analysis of various national databases estimates that acetaminophen overdoses cause 56,000 emergency department visits, 26,000 hospitalizations, and 460 deaths annually in the United States, and the number of fatalities is growing rapidly.16 In 2009, the US Food and Drug Administration (FDA) convened a special meeting to discuss how to address this growing public health problem.17
The cause of liver toxicity involves its metabolism. When used at normal dosages, the majority of acetaminophen is metabolized into a nontoxic metabolite and only 5% is metabolized into a liver toxic metabolite. Under normal circumstances, the body is able to quickly detoxify this metabolite and no liver damage occurs. When used in excessive dosages or in the presence of preexisting liver impairment, the body cannot detoxify quickly enough.7
Patients taking acetaminophen chronically should be asked about alcohol use. Package instructions state: “If you consume three or more alcoholic drinks per day, ask your doctor whether you should take acetaminophen or other pain relievers/fever reducers.”14 The reason for this warning is that heavy, chronic alcohol use shifts the metabolism of acetaminophen, resulting in a higher percentage of toxic metabolite production. Again, the body cannot detoxify quickly enough and the risk of liver damage increases.
To minimize the risk of liver toxicity, dosages should not exceed 4 gm/day (4000 mg/day) for most healthy adult patients. This maximum “safe” dose may be too high for frail older adults, persons who chronically use alcohol, and those with impaired liver function.17
Nonsteroidal Antiinflammatory Drugs
Four NSAIDs are available OTC: aspirin, ibuprofen, naproxen, and ketoprofen. The others are available by prescription only. Two NSAIDs are available in injection form, ketorolac and ibuprofen. NSAIDs are very commonly used OTC as fever reducers and analgesics. NSAIDs are effective for a variety of noninflammatory, mild to moderate, acute and chronic pain, including headaches, back pain, and osteoarthritis, and are especially effective for inflammatory pain, including rheumatoid arthritis, carpal tunnel syndrome, acute gout, lateral and medial epicondylitis (tennis elbow and golf elbow), and bursitis.5,7 NSAIDs can be found in a variety of OTC products, including cough and cold products and some sleep aids (e.g., Advil PM). A few prescription opioid analgesics contain ibuprofen or aspirin (see Appendix A).
Aspirin is an NSAID, although it is often described separately because its therapeutic uses and side effect profile are somewhat different from the other NSAIDs. Aspirin should not be used in children because it can cause a rare, but potentially fatal illness of childhood known as Reye syndrome. Aspirin has strong antiplatelet effects, and is therefore used in low dosages, 81 to 325 mg/day, to prevent ischemic strokes. Higher dosages (650 mg/dose) are required to achieve analgesic benefits.14
The mechanism of action of NSAIDs involves inhibition of prostaglandins and cyclooxygenase type 1 and COX-2. Because of side effects, NSAIDs are not appropriate for all patients. NSAIDs should be avoided in persons with difficult to control hypertension, congestive heart failure, kidney disease, stomach ulcers, bleeding disorders, alcoholism, and patients taking anticoagulants (e.g., warfarin).7,14
Cyclooxygenase-2 Inhibitors
Currently, celecoxib (Celebrex) is the only COX-2 inhibitor on the market. Available by prescription only, celecoxib is used to treat the same types of pain as NSAIDs but with a lower risk of certain side effects. Like the NSAIDs, celecoxib also inhibits the production of prostaglandins by inhibiting the COX enzyme; however, it inhibits COX-2 but not COX-1. Inhibition of COX-2 results in the same antiinflammatory benefits as the NSAIDs and side effects related to fluid accumulation (avoid in persons with hypertension, congestive heart failure, and kidney disease). Because celecoxib does not inhibit COX-1 to a large degree, it has fewer bleeding-related and stomach-related side effects, so it is safer than other NSAIDs in persons at risk for gastrointestinal bleeding, including persons over 65 years of age, with bleeding disorders, alcoholism, and taking anticoagulants.5 Because of potential cross-sensitivity, persons allergic to sulfonamide antibiotics (e.g., sulfamethoxazole/trimethoprim [Bactrim and Septra]) should not be prescribed celecoxib.
Corticosteroids
Corticosteroids (also called glucocorticoids) are produced naturally by the adrenal cortex and are involved in regulating metabolism of carbohydrates, proteins, and fats; inflammation; immune function; wound healing; and a wide number of other body systems. When used medically, corticosteroids have powerful antiinflammatory and immunosuppressant effects, making them useful in treating conditions such as rheumatoid arthritis, osteoarthritis, carpal tunnel syndrome, acute gout, lateral and medial epicondylitis, bursitis, and systemic lupus erythematosus (SLE). Corticosteroids may be administered orally, intravenously, or intraarticularly (into the joint). Commonly used corticosteroids are listed in Appendix A.
Intraarticular injections of corticosteroids (mainly methylprednisolone and triamcinolone) can provide excellent pain relief for joints with the advantage of local drug delivery and possibly fewer systemic side effects. After injection, the patient should minimize activity and stress on the joint for several days. Pain generally begins to decrease within 24 to 72 hours after injection, with maximum benefits in about 1 week. The analgesic and antiinflammatory benefits from a single injection may last for up to 4 to 8 weeks.7 The most commonly injected joint is the knee. Other joints may include the shoulder, wrist, temporomandibular joint, ankle, and elbow. Even localized drug delivery results in some systemic absorption.9 Side effects from intraarticular administration are similar to those seen with oral and intravenous administration, but are less frequent and also include local side effects, such as osteonecrosis (loss of blood supply to the bone, resulting in tissue death), tendon rupture, and skin atrophy at the injection site.7,9
Corticosteroids can increase blood glucose (sugar) levels, especially in persons with diabetes or at high risk of diabetes. Because of their effects on metabolism of carbohydrates, proteins, and fats, high-dose corticosteroids can cause muscle myopathy, manifested as muscle weakness as well as abnormal fat distribution to the abdomen (potbelly), face (moon face), and upper back (buffalo hump). Other corticosteroid side effects include edema, cataracts, glaucoma, stomach ulcers, insomnia, risk of infection, mood changes, and even serious psychiatric disturbance.7,9,14







