21
Orthopedic Management of the Shoulder
1. Identify and describe methods, management, and rehabilitation for subacromial rotator cuff impingement.
2. Identify and describe methods of management and rehabilitation for tears of the rotator cuff.
3. Describe methods of management and rehabilitation for glenohumeral instability.
4. Discuss methods of management and rehabilitation for adhesive capsulitis.
5. Identify and describe common injuries of the acromioclavicular joint.
6. Describe common methods of management and rehabilitation for injuries of the acromioclavicular joint.
7. Identify and describe common fractures of the scapula, clavicle, and proximal humerus.
8. Outline and describe methods of management and rehabilitation of fractures around the shoulder.
9. Describe methods of management and rehabilitation after shoulder arthroplasty.
10. Describe common manual exercise techniques for the shoulder.
SUBACROMIAL ROTATOR CUFF IMPINGEMENT
A common cause of shoulder pain and dysfunction in laborers, athletes, and persons who do repetitive overhead lifting is subacromial rotator cuff impingement. In this disorder, the tendons of the rotator cuff are crowded, buttressed, or compressed under the coracoacromial arch, resulting in mechanical wear, stress, and friction.15,20,23 Clinically, distinction must be made between primary and secondary impingement because there are important differences in treatment related to the specific cause of impingement.15,20
Primary shoulder impingement refers to mechanical compression of the rotator cuff tendons, primarily the supraspinatus tendon, as they pass under the coracoacromial ligament between the acromion and coracoid process.15,32
Secondary shoulder impingement is related to glenohumeral instability that creates a reduced subacromial space because the humeral head elevates and minimizes the area under the coracoacromial ligament.20 This mechanical instability is the result of impairment of muscle coordination and weakness of the scapular stabilizers.
Age-related degenerative changes also can result in a decreased subacromial margin between the rotator cuff and coracoacromial arch. Bony osteophyte formation can occupy space under the anteroinferior surface of the acromion, which consequently reduces the available space. A reduction in available space in the shoulder is known as anatomic crowding. The supraspinatus tendon is the most common structure involved with rotator cuff impingement; the vascularity of the supraspinatus tendon is causative.20,32 An area just proximal to the insertion on the greater tuberosity is hypovascular and is commonly referred to as a watershed zone, critical zone, or critical portion. This area of relative transient hypovascularity occurs with repeated arm motions from abduction to adduction, which compromises the blood supply to the area. The combination of reduced blood supply to the supraspinatus tendon and mechanical wear, stress, and friction as a result of repeated overhead motions can lead to primary impingement, supraspinatus tendinitis, and ultimately tears within the rotator cuff.27,32
The various stages of rotator cuff impingement are related to age and degenerative changes in the cuff itself. Neer35 has identified three specific stages of impingement (tendinitis):
 Stage I: Occurs in younger patients (usually younger than 25 years of age), but can occur at any age. Clinical features are edema and hemorrhage. Pain is worse with shoulder abduction greater than 90°.2–5 It is essentially a reversible lesion that responds to conservative physical therapy interventions.37
Stage I: Occurs in younger patients (usually younger than 25 years of age), but can occur at any age. Clinical features are edema and hemorrhage. Pain is worse with shoulder abduction greater than 90°.2–5 It is essentially a reversible lesion that responds to conservative physical therapy interventions.37
 Stage II: The fibrosis and tendinitis stage, which usually affects patients between the ages of 25 and 40 years.1 It is classified as irreversible because of long-term repeated stress, wherein the supraspinatus tendon, biceps tendon, and subacromial bursa become fibrotic. Pain is the predominant feature and occurs with daily activities; it frequently causes the patient difficulty at night.
Stage II: The fibrosis and tendinitis stage, which usually affects patients between the ages of 25 and 40 years.1 It is classified as irreversible because of long-term repeated stress, wherein the supraspinatus tendon, biceps tendon, and subacromial bursa become fibrotic. Pain is the predominant feature and occurs with daily activities; it frequently causes the patient difficulty at night.
 Stage III: Affects patients more than 40 years of age. It is characterized by tendon degeneration, rotator cuff tears, and rotator cuff ruptures. Usually associated with a long history of repeated shoulder pain and dysfunction, as well as significant muscle weakness and atrophy.
Stage III: Affects patients more than 40 years of age. It is characterized by tendon degeneration, rotator cuff tears, and rotator cuff ruptures. Usually associated with a long history of repeated shoulder pain and dysfunction, as well as significant muscle weakness and atrophy.
Various clinical tests can be used to identify the presence of pain related to specific maneuvers of the shoulder. During the initial evaluation performed by the physical therapist (PT), tests are used to elicit impingement signs. One of these is the Neer painful arc test, in which pain is reported while the shoulder goes through elevation with internal rotation. This test elicits impingement secondary to compression of the rotator cuff against the coracoacromial arch.10 The Hawkins-Kennedy test is performed by elevating the shoulder to 90° in the scapular plane with internal rotation over pressure (Fig. 21-1). In most cases, elevation of more than 80° or 90° elicits pain. Therefore exercise and all activities that require the shoulder to elevate or abduct past 80° or 90° must be strictly avoided until all symptoms of pain have been eliminated.
Rehabilitation of Primary and Secondary Rotator Cuff Impingement
Kamkar and colleagues20 have identified scapular weakness as leading to “function scapular instability,” which affects scapular position during activities that cause a “relative decrease in the subacromial space.” This secondary impingement requires the scapulothoracic muscles to be strengthened and stabilized before specific rotator cuff weakness can be addressed. Scapula thoracic articulation is known to many clinicians as the true core of the upper extremity. To effectively stabilize the humeral head so that it does not migrate superiorly, causing “winging” or “tipping,” the scapular muscles (serratus anterior; upper, middle, and lower trapezius; levator scapulae; and rhomboid muscles) must be strengthened.17,20,42 Thein42 describes the clinical features of humeral head migration (secondary impingement) as possibly confusing the typical impingement picture. She reports, “If the supraspinatus is overworked trying to stabilize the humeral head, then it is unable to effectively function to depress the humeral head. The resultant upward movement decreases the subacromial space and irritates the subacromial soft tissues, thus perpetuating the impingement process.”
Scapular stabilization exercises are only one component of a successful rehabilitation program.9 In general a comprehensive rehabilitation program to address rotator cuff impingement, rotator cuff tendinitis (supraspinatus tendinitis), and degenerative tears of the rotator cuff tendons include modification of activities, local and systemic methods to control pain and swelling (nonsteroidal antiinflammatory drugs [NSAIDs], corticosteroid injections, ice, ultrasound, iontophoresis, phonophoresis), stretching and strengthening exercises, and a return to normal function after reevaluation by the PT and with continued maintenance of protective positions and general conditioning.13,15
Throughout phase I, stretching exercises are performed to increase blood flow and contractility15 and improve motion. The PTA must pay particular attention to performing all stretching activities, because many generalized shoulder stretches involve full forward shoulder elevation and abduction maneuvers. All phase I stretching should encourage nonballistic, slow, controlled, pain-free motion at less than 80° to 90° of elevation. Capsular mobility has been shown to be very helpful in increasing motion and preparing the surrounding muscles to assist in shoulder elevation in all planes of motion.26,34 However, once symptoms are managed the patient can perform all stretches involving elevation and abduction if these stretches do not produce symptoms. Depending on the initial evaluation data gathered by the PT, the patient may be instructed in two specific stretches that authorities15 suggest are effective in addressing posterior capsular tightness. Shoulder adduction across the chest (cross-body stretching) and internal shoulder rotation are used cautiously to improve posterior capsular tightness and overcome the limitations on motion of internal rotation of the shoulder. The effective use of the sleeper stretch to increase posterior capsular mobility has been reported. The concept of anterior capsular mobility has been presented as important for shoulder mobility to treat or prevent impingement while regaining horizontal abduction to prepare for tri-plane overhead motion.25
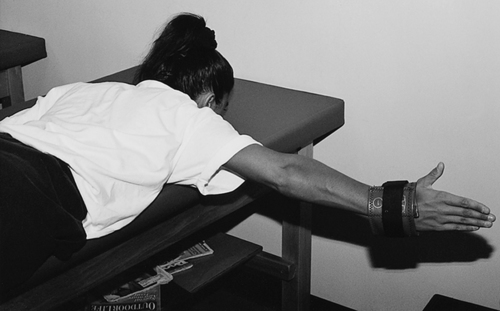
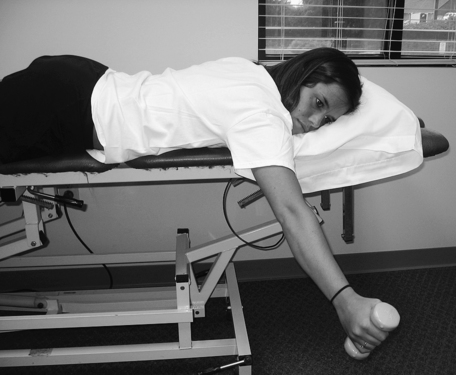
Initial strengthening activities that can begin during phase I generally include scapula stabilization exercises and light rotator cuff strengthening. The use of closed kinetic chain loading such as wall push-ups can be an effective pain-free low level muscle recruitment exercise. Closed kinetic chain (CKC) exercises will provide co-contraction and tri-plane stabilization with lower muscle contraction load than open kinetic (OKC) chain exercises.5,46 Once the patient demonstrates improved motion and can do ADLs without pain, a progression through a series of OKC muscle strengthening can begin. Prone extension to the hip, side-lying external rotation, and scaption elevation without pain are some recommended exercises for rotator cuff recruitment toward strengthening (Fig. 21-2).38 Specific rotator cuff strengthening exercises should focus on the supraspinatus muscle.38 Studies demonstrate that the supraspinatus, infraspinatus, subscapularis, deltoid, latissimus dorsi, and pectoral muscles are effectively strengthened by arm elevation in the transverse plane, shoulder elevation with neutral rotation in the plane of the scapula (Fig. 21-3), prone horizontal shoulder abduction with external rotation (Fig. 21-4), and seated press-ups.30

Phase II, return to function, progresses with advanced scapular stabilization exercises that are encouraged as part of a comprehensive glenohumeral and scapulothoracic strengthening program. This phase of program uses progressive resistive strengthening via increased resistance while using OKC exercises. Electromyographic studies33 have identified four basic scapular stabilization exercises that strengthen the upper, middle, and lower trapezius; the levator scapula; the rhomboid major; the pectoralis minor; and the middle and lower serratus anterior muscles.8 The exercises are rowing, scapular plane elevation (scaption), press-ups, and push-ups followed by scapular protraction. As strength improves and when motion increases, a gradual return to normal function signifies the beginning of phase III, return to activity.44
The process of functional recovery is slow and must be done cautiously; overhead activities are introduced incrementally as the patient is able to demonstrate pain-free motion and the ability to perform strengthening activities. Some advanced return to activity phase exercises can include oscillatory training (Bodyblade) using tri-plane positioning (Fig. 21-5).40
Surgical Management of Shoulder Impingement and Rotator Cuff Tears
When physical therapy interventions fail to provide long-lasting relief and in cases of rotator cuff tears (Neer’s stage III impingement, tendon degeneration, and cuff tears), various surgical procedures can be used to correct the underlying pathologic condition. With subacromial impingement not involving a specific rotator cuff tear, subacromial decompression (SAD) can be used to eliminate or diminish the abnormality causing the impingement between the humeral head and the undersurface of the acromion, allowing freer movement of the tendons without irritation. Acromioplasty includes beveling or reshaping of the acromion with detachment of the coracoacromial ligament. Distal clavicle excision (DCE) may also be involved.39 If there is an associated rotator cuff tear (small tear less than 1 cm, medium tear less than 3 cm, large tear greater than 5 cm), a SAD procedure is used in conjunction with direct repair of the rotator cuff defect. The SAD procedure can be performed as an open arthrotomy or as an arthroscopic procedure.39
Rehabilitation after SAD or rotator cuff repair closely parallels nonoperative rehabilitation of rotator cuff impingement. However, time must be allowed for healing of the soft tissues and bone after surgery. Some clearly identified differences exist between rehabilitation procedures used for decompression and small cuff tears (less than 1 cm) and repairs of medium (less than 2 to 3 cm) and large (greater than 4 to 5 cm) cuff tears with SAD.39 With a small cuff tear repaired in conjunction with a decompression procedure, active motion and pain-free exercise can begin as soon as the patient can tolerate these activities.39,44 However, if the rotator cuff tear is between 2 and 5 cm, tissue protection must be longer to allow for extensive soft-tissue healing. If full active range of motion (AROM) is allowed too early, healing of the rotator cuff may be compromised because of the stresses placed on the repaired tissues. The type of surgical procedure used, mini-open procedure or arthroscopic approach; the healing constraints must be considered for proper beginning of successful rehabilitation. Large cuff tears may require longer periods of time for recovery to achieve improved healing.15
Generally, recovery after SAD with or without rotator cuff repair follows a prescribed three-phase rehabilitation program.42,44 Phase I, the prefunctional phase, lasts approximately 3 to 4 weeks39,44 and focuses on control of pain and swelling with NSAIDs, oral analgesics, ice packs, ultrasound, phonophoresis (if needed), infrared therapy, and various degrees and durations of manual range of motion (ROM), depending on the extent of tissue injury. The concept of early protected manual motion applies depending on the precise nature of the injury and which surgical procedure is used. The prefunctional phase should include increasing ROM, scapula stabilization beginning with retraction, and adding protraction when the patient has pain-free arm control.
At the end of this phase, the initial use of the upper body ergometer (UBE) may be introduced. The early use of CKC activity with double-arm wall push-ups may be helpful for low level recruitment of shoulder muscles.44,46 With increased arm control strength and motion, phase II, the return to function phase, can begin. It generally lasts from weeks 5 through 12 after surgery. During this phase, progressive motion can be used, although with caution for repetitive shoulder abduction and forward elevation above 90°. The use of Thera-Band strengthening of the rotator cuff should be performed in a short-arc pattern of motion, normally in the standing positions.18,44 In addition, dumbbell isotonic concentric and eccentric exercises for recruitment of the humeral head decompression (rotator cuff) may begin using short-arc pain-free ROM. This program is known as positional recruitment for the purpose of low-level strengthening and progresses according to the tolerance of the patent and demonstration of arm control.44 During phase II, progressive strengthening exercises for elevation in scaption are performed in allowing for what is known as shoulder hike. Prone positional exercise, such as prone extension to hip (Fig. 21-6) and short-arc prone scaption at 100°, and eccentric training of scaption has been very useful in treating shoulder hike.30,38,44 Progressive resistive exercises (PREs) are a major part of the return to function phase. With some patients, based on good pain-free response to all rotator cuff exercise, advanced scapula stabilization and oscillatory training such as the Bodyblade may begin (see Fig. 21-5).

Phase III, the return to activity phase, can begin once the patient can demonstrate normal motion without symptoms and with improved strength. This phase lasts approximately from week 12 to beyond. Return to activity always includes the continuation of PREs. This aspect of rehabilitation is for the long haul.44 Advanced CKC exercises such as single-arm wall push-ups on an uneven surface may be introduced. For the advanced patient, plyometric activity with plyo-toss exercise may be used (Fig. 21-7).
During the return to activity phase the core rotator cuff strengthening exercises of forward elevation, scaption, prone horizontal abduction with external rotation, and press-ups, as well as scapular stabilization exercises of seated rows, prone scaption at 120° (Fig. 21-8), scaption, and press-ups for scapular protraction (push-ups with a plus)20,33,38,44 form the foundation of improving strength that eventually leads to full functional recovery.
The prefunctional phases and periods of passive or manual control motion are extensive for rehabilitation after surgical repair of massive rotator cuff tears. Generally, no active shoulder motion or active concentric or eccentric strengthening is allowed for 2 to 3 months after surgery.11 Extensive soft-tissue healing must proceed unabated to foster the recovery of functional motion and strength.
Initially the patient is placed in abduction pillow or shoulder immobilization after surgery to allow the repaired tissues of the rotator cuff and deltoid to be placed in a shortened position. Early active muscle strengthening and active motion are avoided to allow for appropriate healing. Generally, manual control passive ROM with full motion restriction is allowed during the first several weeks of recovery. AAROM activities, can begin 2 months after surgery.11
Submaximal isometrics and scapular stabilization exercises must be added cautiously 4 to 12 weeks after surgery.11,44 Specific rotator cuff strengthening exercises11 performed isotonically with dumbbells, Thera-Band, and similar devices are reserved until 3 months after surgery to accommodate the healing constraints of the tendons and muscles of the rotator cuff and deltoid. Full functional recovery of motion and strength may take up to several months after the repair of massive rotator cuff tears.11,44
GLENOHUMERAL JOINT INSTABILITY AND DISLOCATION
Dislocations and subluxations (partial dislocation) of the glenohumeral joint (the articulation between the humeral head and glenoid fossa of the scapula) frequently occur after indirect trauma with the arm abducted, elevated, and internally rotated (posterior dislocation).16 The shoulder is the most commonly dislocated joint in the body,16 and dislocation occurs in men more often than in women. Anterior dislocations occur more frequently than posterior dislocations.16 Also, rotator cuff tears of various dimensions (small, less than 1 cm; medium, less than 3 cm; and large, greater than 5 cm) occur with relative frequency. Strege41 reports that rotator cuff tears occur 30% of the time with acute anterior dislocations in patients older than 40 years of age and 80% of the time in patients older than 60 years of age.
Two associated injuries may occur as a result of acute glenohumeral dislocation and instability. Because the shoulder is the most mobile joint in the body, bony restrictions do not provide substantial restraint. Rather, the fibrocartilaginous glenoid labrum deepens the articulation between the humeral head and bony glenoid fossa. Injury to the labrum can occur if forces are great enough to dislocate the humerus from its confines within the glenoid. This injury is referred to as a Bankart lesion3,36,41,42,44 and is defined as “an avulsion of the capsule and glenoid labrum off of the anterior rim of the glenoid resulting from traumatic anterior dislocation of the shoulder.”21,41
The head of the humerus is subject to injury as a result of anterior shoulder instability. A Hill-Sachs lesion is a compression or “impaction fracture”36 of the posterolateral aspect of the humeral head as a result of anterior shoulder instability.3,36,41,42 This lesion results from instability and is not the essential cause of glenohumeral instability.36,45
As stated, anterior dislocations are more prevalent than posterior dislocations. However, shoulder instability can be defined as multidirectional, wherein the humeral head may sublux or dislocate anteriorly, inferiorly, and posteriorly.36,41
Nonoperative Management
The initial management of acute shoulder dislocations (anterior and posterior) calls for a period of protection lasting for up to 4 to 6 weeks.16,36 All positions that may reproduce the mechanism of dislocation are avoided. In some cases immobilization is needed to promote healing.
Management of pain and swelling is addressed with physician-prescribed NSAIDs, analgesics, ice packs, electrical stimulation, or other physical agents such as ultrasound and infrared. During the protection period, the hand, wrist, and elbow of the affected shoulder must receive active motion and strengthening exercises that do not compromise the shoulder. Also, a general conditioning program of strength, flexibility, and endurance activities can begin. With an anterior shoulder subluxation (spontaneous reduction of the humeral head) or dislocation, the patient must avoid shoulder abduction and external rotation to allow proper capsular scarring and soft-tissue healing to occur. It is interesting to note that patients older than age 40 years who are not at significant risk of recurrent dislocation because of a relatively sedentary lifestyle may only need minimal protection for a couple of weeks before rehabilitation can begin and motion can be regained.16,36
Initial strengthening begins with submaximal isometric exercises that can be safely started while the patient’s shoulder is placed in the neutral humeral position. Isometric shoulder adduction and abduction, internal and external rotation, and elevation and extension can be performed at a pain-free level. Once the patient can demonstrate an increase from submaximal isometric contractions to near-maximal contractions, progressive internal and external rotation can begin with the affected shoulder in a minimal degree of abduction. When the symptoms of pain are reduced and the intensity and quality of muscle contractions are improved, the patient may increase ROM activities to forward elevation, extension, scapular mobility, and internal and external rotation and abduction. As the patient progresses to the return to function phase, combined shoulder abduction and external rotation are avoided. In fact, some authorities recommend avoiding extremes of shoulder abduction and external rotation for 3 months after removal of the sling.16,36 The hallmark of the return to function phases of recovery after anterior shoulder dislocation or subluxation is progressive strengthening of the rotator cuff, anterior shoulder muscles, and scapular stabilizers, with particular attention given to eccentric strengthening of the posterior rotator cuff (infraspinatus and teres minor).22,42,44 Thera-Band and handheld dumbbell weights are effective because of the wide variety of motions that can be addressed and can carry over to home exercises. Please refer to the previous section on rotator cuff exercises for a recommended home program.
Synchronous shoulder motion, or scapulohumeral rhythm, must be addressed before and throughout recovery from a shoulder dislocation. The 2:1 ratio of motion between the scapula and glenohumeral joint (meaning that for every 2° of glenohumeral flexion or abduction after the first 30° of shoulder motion, the scapula must rotate upwardly 1°)24 must be addressed early to prevent the facilitation of abnormal motions between the scapula and glenohumeral joint during strengthening activities. This can be accomplished adequately by focusing on normalized scapular motion and stabilization exercises during the return to function phase as long as symptoms of pain and harmful glenohumeral joint positions are avoided.
Throughout each phase of recovery, various tissues that contain the humeral head in the glenoid fossa (glenoid labrum, capsule, and ligaments; superior, middle, and inferior glenohumeral ligaments; and musculotendinous rotator cuff) can be stressed or torn. By definition, glenohumeral instability identifies ligamentous and capsular restraints as being “attenuated”27,28; therefore the appropriate progressive application of strengthening activities for the rotator cuff and scapulothoracic muscles becomes central to the recovery of motion and function.
One way the PTA can address functional motions and stimulate the afferent neural input system is through CKC activities. CKC activities can enhance proprioception and promote dynamic joint stability.16,28 Rhythmic stabilization through manual exercises and progression to other oscillation training such as the Bodyblade may be helpful.
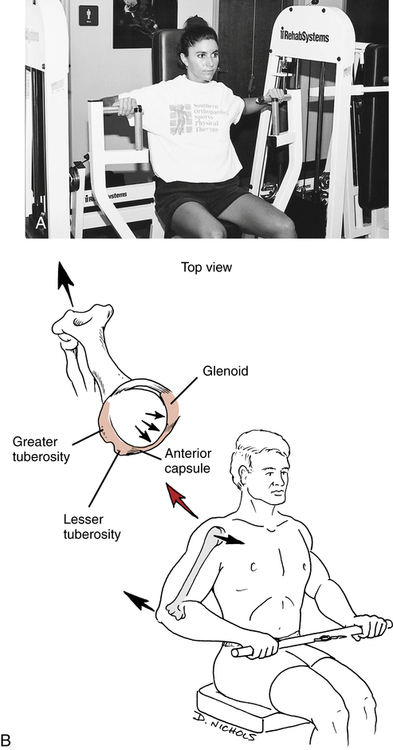
Isotonic resistance exercises are quite challenging and stressful to the glenohumeral joint; consequently, many appropriate exercises must be modified to accommodate limitations of motion, pain, and the provocative positions of abduction and external rotation. The seated or supine chest press is an example of isotonic exercise that promotes anterior shoulder strength. However, this particular exercise can place the shoulder in a horizontally abducted position that stresses the anterior shoulder capsule, causing the head of the humerus to translate forward within the glenoid (Fig. 21-9). Progressive positional recruitment for strengthening using the PRE method is always continued throughout this phase of recovery.
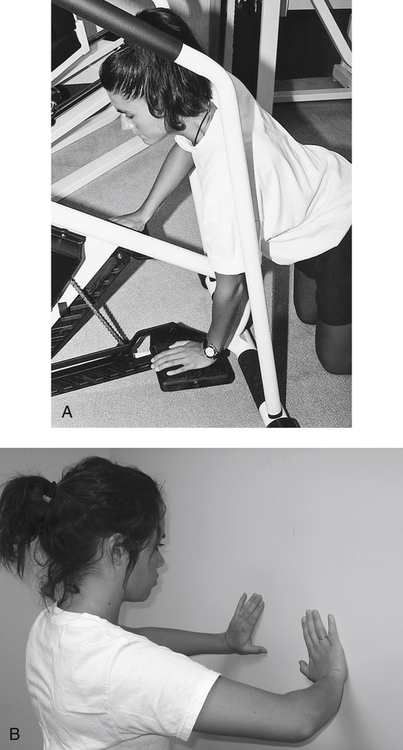
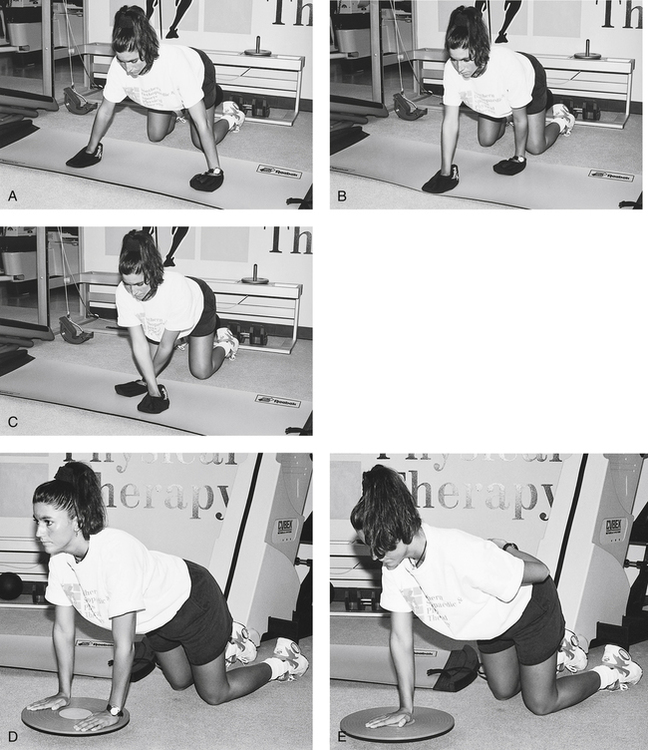
Local muscle endurance activities are done using an UBE, CKC exercise with the use of hands on the stair-stepper (Fig. 21-10, A).44 Weight-bearing closed-chain exercises such as wall push-ups (Fig. 21-10, B) for tri-plane strengthening can be introduced. These exercises provide proprioceptive stimulation to the mechanoreceptor system. Gradually, more challenging weight-bearing activities that demand progressive control of the glenohumeral joint in multiplane and diagonal motions are added (Fig. 21-11, A–C). A balance board also can help train the shoulder muscles to respond and fire quickly for sufficient stabilization (Fig. 21-11, D-E).
Cable systems offer various exercises and positions that duplicate functional activities. Cable systems are particularly useful in athletic patients, because sport-specific tasks can be reproduced with this equipment. In addition, a plyo-toss (plyometric) exercise for stabilization is part of the return to activity phase. Plyometric ball toss against a rebounder is an excellent exercise for advanced patterns (Fig. 21-12).4
The process of recovery after shoulder dislocation matches the degree of injury. Full functional recovery is not always possible. In some cases, minor stress causes the shoulder to dislocate again after acute traumatic dislocation. With repeated episodes of shoulder dislocation or subluxation, recurrent anterior instability can result.12,16 If patients fail to respond to an aggressive physical therapy program, the physician may choose one of several operative procedures to correct the instability. Patients with recurrent dislocations may receive an anterior capsulolabral reconstruction.7 Patients with multidirectional instability may require a procedure known as a capsular shift.23
Operative Management and Rehabilitation
Because posterior shoulder dislocations account for only 2% to 4% of all shoulder dislocations,36 this discussion focuses on repairs and rehabilitation procedures to enhance joint stability and promote function in patients with anterior glenohumeral instability. Surgical procedures for shoulder instability can be classified as open or arthroscopic techniques.7,23,36
Patients with anterior shoulder instability corrected via arthroscopy normally experience less postoperative pain and reduced soft-tissue damage.44 Rehabilitation after open or arthroscopic stabilization for anterior glenohumeral instability requires a prefunctional phase of rehabilitation that emphasizes protected ROM. Slow and protective external rotation is performed up to 12 weeks postoperative to ensure healing of all soft tissue. A recommended external rotation incrimination is as follows:
Initial postoperative care begins with a period of immobilization in a shoulder immobilizer to allow for appropriate soft-tissue healing.7 During this period, medications for pain and swelling may be prescribed by the physician. Frequently, ice packs are applied to the shoulder for 20 minutes, three to five times daily, as part of the home program to control postoperative pain and swelling. Also the patient can actively perform finger, hand, wrist, and elbow mobility exercises. In addition, submaximal isometric exercises can be initiated while the arm is still in the immobilizer. These must be performed pain free.
The degree and direction of shoulder motion allowed are specific to the surgical procedure, the wishes of the physician, and the direction of the PT. Generally, scapular protraction and retraction, manual control ROM, and assisted ROM exercises are performed to increase motion. The initiation of motion exercises is important because faulty scapulothoracic and glenohumeral mobility can be affected early. Care must be taken to encourage scapular motion, as well as glenohumeral mobility, and to identify any limitations affecting normal scapulohumeral rhythm. Progressive elevation and scapula control is recommended early in this phase of rehabilitation. Elevation is normally progressed to 135° to tolerance after 6 weeks postoperative. Slow progression of abduction is recommended. Therefore the PTA must be aware of the exact rationale behind limiting early active or passive shoulder abduction and external rotation.44
Progressive motion and strengthening exercises are allowed as the patient progresses to the return to function phase. Progressive shoulder strengthening must address both the glenohumeral and scapulothoracic joints. To recover functional mobility of the shoulder, a program of positional recruitment is suggested. Because the scapula forms the base of support for glenohumeral motion, stabilization exercises must be advanced. As the patient demonstrates improved mobility without complaints of pain, the quality of muscle contraction (from submaximal to maximal) must be encouraged gradually. PREs using a Thera-Band, dumbbells, or both within an active, pain-free ROM can begin, along with more challenging flexibility exercises, between 6 and 8 weeks after surgery.7
The eccentric contraction phase of each exercise must be encouraged. Applying this concept during the return to function phase involves emphasizing the eccentric loading phase of all internal rotation, abduction, external rotation, adduction, and shoulder elevation exercises.4 Local muscle endurance also must be considered once the patient has achieved improved motion and strength. Usually an UBE or some other form of low-intensity, high-repetition shoulder-specific activity is appropriate. Functional activities, proprioception, and CKC exercises, are necessary for functional recovery.
During the return to activity phases of recovery, in order to stimulate the mechanoreceptor system, a complete program of advanced CKC exercises, plyo-toss (plyometrics) and sports specific training is designed. Generally the total length of rehabilitation after surgical stabilization of the glenohumeral joint ranges from 3 to 5 months.7
ADHESIVE CAPSULITIS
Adhesive capsulitis, which is also referred to as frozen shoulder, is characterized by decreased shoulder ROM, pain, inflammation, fibrous synovial adhesions, and reduction of the joint cavity.1,3,6 Adhesive capsulitis occurs more commonly in females and affects patients between 40 and 60 years of age.6 The two distinct classifications of frozen shoulder are primary and secondary adhesive capsulitis. Primary idiopathic frozen shoulder is the most common lesion and occurs spontaneously from unknown causes. Secondary adhesive capsulitis generally occurs after trauma or immobilization.6,52
Among older patients, secondary adhesive capsulitis can develop because of limited immobilization for as little as 1 or 2 days.5,14 In the early stages of this disabling condition, pain occurs both at rest and during activity.5,6,14 However, as the condition progresses, pain gradually subsides, then spontaneously disappears. Severely restricted motion and profound loss of function remain.5,6,14 During the acute painful phase, treatment is focused on controlling inflammation and symptoms of pain. Physician-prescribed analgesics, NSAIDs, and intraarticular steroid injections can provide some pain relief.6
Physical therapy interventions during this acute painful stage include the judicious use of ice, heat, ultrasound, phonophoresis, and infrared. Also central to this initial management phase is the stimulation of pain-free motion and relaxation of muscle guarding of the glenohumeral joint, cervical area, and scapulothoracic muscles.19 Passive, active, and active assisted motion exercise must occur within a pain-free ROM to stimulate removal of metabolic waste, increase local blood flow, and assist in the reduction of edema in the local tissues. Both wand and rope and pulley systems can be used early if they are performed in a slow, controlled, pain-free ROM. For severely restricted glenohumeral motion, the PT may prescribe the application of specific joint mobilization techniques to help modulate pain and reduce muscle guarding.1,3,5,14,19,44 As addressed, grades I and II low-amplitude physiologic and accessory oscillations can help encourage relaxation while reducing pain.19,44
If the scapula is not stable and free from restriction while the patient attempts to regain shoulder motion and function, normal scapulohumeral rhythm cannot be obtained. Therefore early scapular stabilization exercises3,37,44 can be employed as long as pain does not inhibit the correct performance of the exercise. Normalized motion must precede specific strengthening activities to avoid developing faulty shoulder mechanics.
The complete restoration of glenohumeral joint mobility is the goal of treatment for the late stage of adhesive capsulitis. The PT must identify the appropriate application of increased joint mobilization techniques to address specific capsular restrictions and initiate more challenging progressive resistance exercises.48 When the patient demonstrates improved glenohumeral motion and appropriate scapulohumeral rhythm, strengthening exercises can begin for the deltoid, scapular muscles, rotator cuff, and upper-arm muscles.9,44
Although control of pain and inflammation is the primary feature of early physical therapy management, submaximal isometric exercise can be used to initiate strengthening if pain is not increased with exercise. Progressing from submaximal isometrics to maximal isometrics usually precedes the use of a Thera-Band or dumbbells for concentric and eccentric exercises. A comprehensive series of rotator cuff exercises38,43 and scapular stabilization exercises3 can be encouraged as early as pain and motion allow. To address normalized function, the patient does closed-chain resistance exercises and overhead loading along with proprioception exercises (e.g., balance board, slide board, and Plyoball) in a sequential, orderly fashion once sufficient strength, improved motion, and scapulohumeral rhythm have been established. Local muscle endurance activities focus on purposeful, functional movements that duplicate ADLs.
ACROMIOCLAVICULAR SPRAINS AND DISLOCATIONS
Ligamentous sprains of the AC joint usually result from a fall on the acromion (direct force) or when force is transmitted from a fall on an outstretched arm proximally to the AC joint (indirect force).50 AC joint sprains and dislocations are graded according to the degree of injury to specific ligamentous structures (AC and coracoclavicular ligaments), as well as the position of the clavicle in complete rupture of both the AC and coracoclavicular ligaments, as follows50:
 First-degree, grade I AC joint sprain: Characterized by partial tearing of the AC ligaments, with resultant joint tenderness over the AC joint, no joint instability or laxity of the ligament, and minimal loss of function.31
First-degree, grade I AC joint sprain: Characterized by partial tearing of the AC ligaments, with resultant joint tenderness over the AC joint, no joint instability or laxity of the ligament, and minimal loss of function.31
 Second-degree, grade II AC sprain: Complete rupture of the AC ligaments with partial tearing of the coracoacromial ligaments.31,50 The patient has moderate pain, some dysfunction (reduction in shoulder abduction and adduction), and a palpable gap between the acromion and the clavicle.1,30,31
Second-degree, grade II AC sprain: Complete rupture of the AC ligaments with partial tearing of the coracoacromial ligaments.31,50 The patient has moderate pain, some dysfunction (reduction in shoulder abduction and adduction), and a palpable gap between the acromion and the clavicle.1,30,31
 Third-degree, grade III AC ligament injury: Dislocation between the acromion and clavicle where both the AC and coracoclavicular ligaments are ruptured and the distal clavicle becomes displaced superiorly. Patients demonstrate marked pain and severe limitation of shoulder motion. Three additional classifications have been proposed that describe the degree of vertical, posterior, and inferior separation of the clavicle in grade III AC dislocation.31
Third-degree, grade III AC ligament injury: Dislocation between the acromion and clavicle where both the AC and coracoclavicular ligaments are ruptured and the distal clavicle becomes displaced superiorly. Patients demonstrate marked pain and severe limitation of shoulder motion. Three additional classifications have been proposed that describe the degree of vertical, posterior, and inferior separation of the clavicle in grade III AC dislocation.31
Rehabilitation and management of grade I AC sprains focus on symptomatic relief. Typically, pain is controlled with the use of ice packs, NSAIDs, analgesics, and rest. Because the AC ligaments have been partially torn, the AC joint must be protected from further direct or indirect forces that may stress the AC ligaments. The patient may be allowed to resume activities within 2 weeks and usually does not require a rehabilitation program of significant duration.1,31
Grade II AC sprains require more direct attention to approximate the torn AC ligaments and allow for secure ligament healing. Usually this injury is managed nonoperatively using a shoulder immobilizer as needed for the short-term, and early ROM and stabilization exercises begin.31 Again, modalities of choice may be used as needed.
As noted, there is usually a palpable step-off between the acromion process and distal clavicle with grade II AC sprains. This deformity represents a permanent loss of joint continuity because of lost ligamentous support between acromion and clavicle.31
The treatment of grade III AC sprains (dislocation of the distal clavicle and acromion process) may include surgical intervention. Although many surgeons advocate open surgical repair, others favor closed reduction, immobilization, and progressive rehabilitation. The nonoperative treatment of grade III AC sprains is centered on reducing the dislocation and maintaining the reduction.31 The goals of the initial course of treatment in physical therapy is to minimize pain and swelling, with the modalities of choice, physician-prescribed NSAIDs, analgesics, and protection of the AC joint from unwanted stress, To ensure proper healing of the ligaments, the rehabilitation team must continuously reinforce compliance using the immobilizer for the recommended period prescribed by the treating physician.
SCAPULAR FRACTURES
Most scapular fractures result from direct, severe trauma.29,50 Therefore there is a high incidence of significant associated injuries, including other fractures, glenohumeral dislocations, pneumothorax, and neurovascular injuries.29,41,50 Interestingly, fractures of the scapular body are the most common (49% to 89%)50 and demonstrate the highest incidence of associated injuries (35% to 98%).41 However, the treatment of fractures to the scapular body is conservative if associated injuries have not occurred, using ice and shoulder immobilization for 2 to 3 weeks.29,41,50 During the immobilization period, hand, wrist, and elbow exercises can be initiated for the affected arm along with a general conditioning program. Early manual control ROM exercises for the shoulder begin as the pain and swelling subside.
Isometric exercises performed submaximally also can be initiated early if the patient remains pain free. As pain and swelling subside, strengthening exercises can be added within a pain-free ROM. Nonunion and malunion of this fracture are rare and usually are not associated with a loss of function or clinical symptoms.41,50
The second most common scapular fracture occurs to the glenoid neck. Williams and Rockwood50 suggest that if the fracture is extraarticular, healing can occur at 6 weeks and that management involves conservative symptomatic care. Glenoid fractures also can be intraarticular, where the fracture extends through the glenoid fossa. The treatment of these fractures depends on whether there is associated glenohumeral instability. If no instability is present, these fractures are treated with shoulder immobilization and a return to motion and strength.50 However, if there is glenohumeral instability associated with an intraarticular glenoid fracture, then surgical repair is needed to stabilize the fragments.50 Usually an internal fixation device is inserted into the fracture fragments; therefore immobilization is needed to minimize stress at the fracture site. Manual control exercises can be initiated soon after surgery to minimize postoperative joint stiffness. Although gentle manual control shoulder elevation and external rotation are initiated 2 to 3 weeks postoperatively, active stretching and resistance exercises must be deferred for up to 6 to 8 weeks to allow for secure bone healing.50
CLAVICLE FRACTURES
Fractures of the clavicle occur as a result of direct or indirect trauma. These injuries are common and primarily affect men younger than 25 years of age.52 Care is focused on achieving reduction of the fracture fragments, maintaining the reduction, and minimizing the immobilization of the glenohumeral joint of the affected arm.52 Usually the patient is placed in a commercially available figure-of-eight bandage to maintain proper alignment of the area. The duration of immobilization varies, but authorities suggest that healing takes 4 to 6 weeks or longer.52
During the initial period of immobilization, with the figure-of-eight bandage, the hand, wrist, and elbow of the affected arm are exercised with active motion and resistance exercises. Unwanted stress to the fracture site is avoided during this period. In addition, the patient may perform submaximal isometrics for the shoulder and scapula once pain has been controlled. Manual exercises to the scapula is recommended before beginning OKC strengthening.44
Active shoulder elevation must not be greater than 50° to 70° until after 4 weeks (although patients may be encouraged to perform gentle active shoulder motion no greater than 60° when pain free).50 As the healing process continues and when bone healing is confirmed radiographically (approximately 4 to 6 weeks), greater degrees of shoulder motion are allowed, with PREs added as tolerated.
If the fracture is located at the distal end of the clavicle, ORIF may be more appropriate, because these fractures tend to be unstable and do not maintain proper alignment with a figure-of-eight bandage.41 The fragments of a displaced distal clavicle fracture usually are secured with an intramedullary fixation pin.41
PROXIMAL HUMERUS FRACTURES
Proximal humerus fractures usually are classified according to a four-part classification.29,41 The four parts are the humeral head, lesser tuberosity, greater tuberosity, and humeral shaft.41
Physical therapy management of humerus fractures depends on the severity and complexity of the fracture, as well as the means used to secure fixation of the fracture site. Generally with nondisplaced one-part fractures (the most common type), the affected arm is placed in a immobilizer for a period of time and the patient is given analgesics and encouraged to apply ice liberally to minimize pain and swelling. Within the first 2 weeks, gentle active motion is allowed, as well as active motion of the elbow, wrist, and hand of the affected arm.29 In fact, the patient may be allowed to remove the immobilizer for active motion exercises a few times each day.29
Submaximal shoulder isometrics are initiated as early as pain allows. Perhaps the most salient aspect of physical therapy care in proximal humerus fracture is the functional restoration of glenohumeral motion and strength after protracted periods of immobility to allow for appropriate bone healing. Early scapular motion exercises minimize the restriction of scapular mobility. Submaximal scapular stabilization exercises44 also can be encouraged early, as pain allows, to provide a stable base for glenohumeral motion exercises. Manual glides for mobility of the scapula maybe helpful. Manual glides to the glenohumeral joint may be needed if hypomobility is a side effect of prolonged immobilization. Progressive motion and resistance exercises for the deltoid, rotator cuff, and upper arm muscles closely parallel bone healing and the patient’s ability to demonstrate improved motion without pain.
Avascular necrosis (AVN) may be a risk with some significant fractures (displaced fractures of the anatomic neck).29 For example, in an older population of patients with advancing osteoporosis who have four-part proximal humerus fracture, internal fixation may be poor because of the osteopenic bone. A prosthetic humeral head, known as hemiarthroplasty, may be more appropriate in this case.41
Total Shoulder Arthroplasty
With severe four-part fractures of the proximal humerus, AVN of the humeral head, osteoporosis, rheumatoid arthritis, and advanced osteoarthritis, the proximal humerus may be replaced with a prosthesis, or a total shoulder arthroplasty may be indicated.14,41 The condition of the rotator cuff is a significant feature in patients receiving a hemiarthroplasty or total shoulder arthroplasty. Goldstein14 reports that in patients suffering from rheumatoid arthritis, as many as 38% have a torn rotator cuff. If a rotator cuff tear is repaired in addition to the arthroplasty, postoperative immobilization may be as long as 4 to 6 weeks, with the affected arm held in an abduction splint to allow for healing of the repaired cuff.2,14,47 When a patient has a massive rotator cuff tear or has had a revision of failed arthroplasty with rotator cuff tear a reverse prosthesis procedure may be needed. This procedure requires the surgeon to place the humeral component in the glenoid socket and the glenoid component into the proximal humerus. The rehabilitation objectives are usually the same as a regular arthroplasty,6 but in some cases the progress will be slower.47
Thus a rotator cuff repair added to shoulder arthroplasty guides the course of rehabilitation and dictates the need for protective of limited motion, which leads to a longer program of rehabilitation.5 In terms of restoration of shoulder motion, if the rotator cuff is not repaired, progressive range of motion though goal setting of the PT is carefully guided to regain functional motion.49
The prefunctional phase of rehabilitation after shoulder arthroplasty usually allows for early manual control assisted ROM and isometric exercises. Slow return toward external rotation is used to protect the healing of the subscapularis.44 Isometric exercise may depend on soft-tissue healing and patient tolerance. Usually during the first postoperative week, the patient is allowed active exercise of the wrist, hand, and elbow of the affected shoulder. The postoperative immobilizer also is frequently removed for hygiene and exercises.14 By the end of the first week, the immobilization device may be removed and manual control exercises initiated and AAROM exercises are continued. At the end of the second postoperative week, the patient is introduced to scapular motion and stabilization exercises while the quantity and quality of isometric exercises and motion exercises are progressed.14 The assistant must encourage compliance with a comprehensive home exercise program of motion and strength. Wand-assisted exercises and pulley systems can be used as part of the home ROM program. Return to function phase will include light resistive strengthening, and more advanced scapula stabilization Thera-Band exercises are useful for the home exercise program. This usually begins between 4 and 6 weeks. Because the subscapularis has been taken down as part of this procedure, precaution is taken to protect against a return of external rotation that is too rapid. Additionally, early strengthening of the subscapularis is avoided to allow adequate heading of this muscle.44
If the patient has received a rotator cuff repair or neural prosthesis, the sequence of care and initiation of resistance exercise and active shoulder motion may be delayed. Functional use of the affected arm can be expected around 4 months postoperatively. However, Goldstein14 suggests that for optimal results, the patient should participate in an active home exercise program long after discharge of rehabilitation.
MOBILIZATION OF THE SHOULDER
Mobilization of the Scapulothoracic Joint
While the patient is in a side-lying position on the unaffected side, the scapula can be effectively mobilized in a superior and inferior direction, as well as distracted from the thorax. To distract the scapula, the PTA should stand facing the patient. The PTA should firmly grasp the medial or vertebral border of the affected scapula and purposefully distract the scapula away from the thorax (Fig. 21-13). To glide the scapula superiorly and inferiorly, the PTA should assume the same position and support the inferior border of the scapula. The PTA should use the hand on the inferior border to direct a force to glide the scapula in a superior direction, then use the hand on the superior border to direct a force to glide the scapula in an inferior direction.21,44 In the same position the PTA can perform a lateral scapula glide. This technique is helpful to loosen subscapular soft tissue that may have become hypomobile during the postoperative or prefunctional phase of rehabilitation.

Mobilization of the Glenohumeral Joint
Anteroposterior glide of the glenohumeral joint can be accomplished with the patient supine. The PTA should sit near the affected shoulder. Wooden51 recommends putting towels under the elbow of the affected shoulder in this position, to place the humerus in a more horizontal position. The humeral head should be grasped firmly with the thumb and fingers of one hand while the scapula is actively stabilized with the other hand. If the glenohumeral joint is stiff and motion is applied to the joint without stabilizing the scapula, the glenohumeral joint and scapula will move as a single unit. While stabilizing the humerus with one hand, the other hand is used on the humeral head to provide an inferiorly or posteriorly directed force (Fig. 21-14).
Lateral distraction of the humeral head can also be achieved while the patient is supine. The PTA should sit near the affected shoulder, then abduct the affected shoulder to 45° and the arm is supported by the PTA’s hands. The PTA can use one or both hands to grasp the proximal humerus and direct a straight lateral force, effectively translating the humeral head from the glenoid (Fig. 21-15). Mild inferior glides of the glenohumeral joint may be helpful in regaining motion due to superior migration of the head of humerus.44
GLOSSARY

Glenohumeral joint Greatest range of motion and least stable of any joint. Center core of motion.