18
Orthopedic Management of the Knee
Kenneth Bush, Justin Rossetter, Matthew Smith and Michael Allen
1. Identify common ligament injuries of the knee.
2. Discuss general methods of management and rehabilitation of common ligament injuries of the knee.
3. Identify and describe common meniscal injuries of the knee.
4. Discuss common methods of management and rehabilitation of meniscal injuries of the knee.
5. Discuss surgical and postoperative management of articular cartilage injuries.
6. Describe common methods of management and rehabilitation of patellofemoral disease of the knee.
7. Identify and describe common patella, supracondylar femur, and proximal tibia fractures.
8. Describe common methods of management and rehabilitation of fractures around the knee.
9. Identify and describe methods of management and rehabilitation after knee arthroplasty and high tibial osteotomy.
LIGAMENT INJURIES
 Grade I: An incomplete stretching of collagen ligament fibers resulting in minimal pain, minimal or no swelling, no loss of joint function, and no clinical or functional instability.
Grade I: An incomplete stretching of collagen ligament fibers resulting in minimal pain, minimal or no swelling, no loss of joint function, and no clinical or functional instability.
 Grade II (second degree): A partial loss of ligament fiber continuity. A few collagen ligament fibers may be completely torn; however, most of the ligament remains intact. This degree of sprain is characterized by moderate pain, moderate swelling, and some loss of joint function and stability.
Grade II (second degree): A partial loss of ligament fiber continuity. A few collagen ligament fibers may be completely torn; however, most of the ligament remains intact. This degree of sprain is characterized by moderate pain, moderate swelling, and some loss of joint function and stability.
 Grade III (rupture): The entire collagen ligament fiber bundles are completely torn. There is no continuity within the body of the ligament. This is usually characterized by profound pain, intense swelling, loss of joint function, and instability.
Grade III (rupture): The entire collagen ligament fiber bundles are completely torn. There is no continuity within the body of the ligament. This is usually characterized by profound pain, intense swelling, loss of joint function, and instability.
Anterior Cruciate Ligament Injuries
The anterior cruciate ligament (ACL) primarily resists anterior tibial translation on the femur; it also prevents hyperextension and extreme varus, valgus, and rotational movements around the knee.71 The cruciate ligaments are intracapsular structures, which can produce a joint effusion when injured. This anatomic relationship is contrasted with the medial and lateral collateral ligaments, which are extracapsular structures. When the medial collateral ligament (MCL) is sprained, there is generally less swelling and no intraarticular effusion because the resultant bleeding from the injured tissues can evacuate the area and the fluid is not restrained within the joint capsule.
Etiology
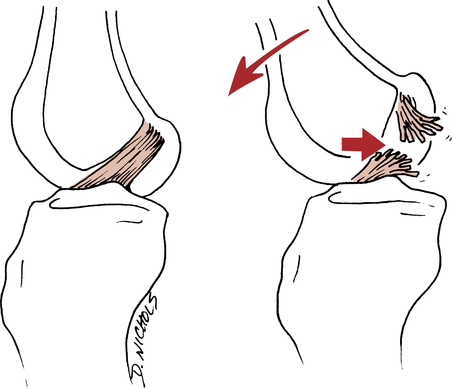
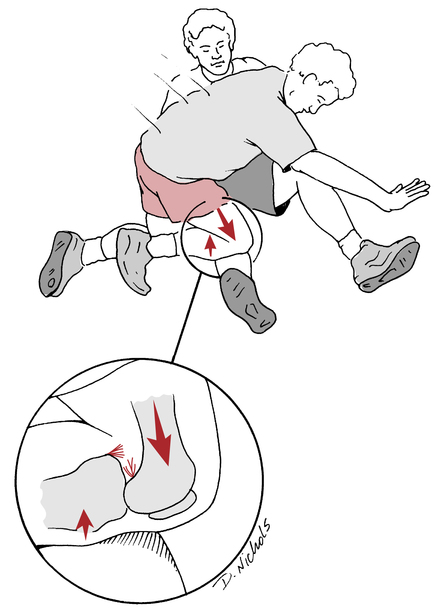
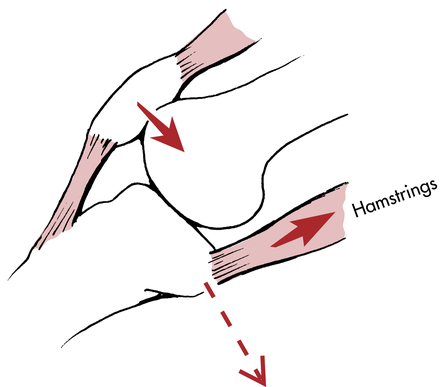
It is well published that female athletes tear their ACLs at a higher rate than their male counterparts.1 The common mechanism for both contact and noncontact injuries results in a combined force of external rotation of the hip, valgus stress at the knee joint, and internal tibial rotation with or without knee hyperextension while the affected foot is planted (Fig. 18-1).24,73,74,77,91,97
Clinical Evaluation
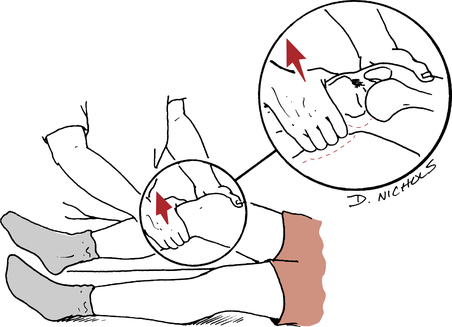
Perhaps the most common, specific, and clinically useful ligament stability test for the ACL is the Lachman examination (Fig. 18-2).47 The patient is supine on an examining table with the affected knee flexed to approximately 25° to 30°. One hand is used to stabilize the distal femur, and the other hand grasps the proximal tibia. An anterior and posterior force is gently directed to the proximal tibia. The integrity of the ACL should be observed, and the degree of anterior tibial translation should be noted.
The anterior drawer test (Fig. 18-3) is another clinical examination used to approximate the degree of anterior tibial translation relative to the fixed femur. This examination is a less sensitive test to challenge the integrity of the ACL, and is instead thought to assess the meniscotibial ligaments and the mobility of the menisci on the tibia.47 The examination is performed with the patient supine and the affected knee flexed to approximately 90°. Stabilize the affected limb by sitting on the patient’s foot. Both hands should be used to grasp the proximal posterior tibia, with the thumbs on the anterior joint line of the knee. An anterior and posterior force should be exerted to the proximal tibia, and the amount of joint separation of the tibia relative to the femur should be observed.
Other relevant tests for the stability of the ACL incorporate multidirectional rotation examinations to acknowledge the presence of anterolateral rotator instability (ALRI), anteromedial rotatory instability (AMRI), posteromedial rotatory instability (PMRI), and posterolateral rotatory instability (PLRI). ALRI is the more common multiplanar instability encountered.47,91 The Hughston jerk test and pivot shift test are commonly used examinations to sublux and reduce the tibia relative to the femur.47
Throughout the performance of the examination, complete muscle relaxation of the hamstrings, quadriceps, and gastrocnemius–soleus muscle group must be maintained. Swelling, intraarticular effusion, and muscle spasm falsely stabilize the knee, rendering the examination meaningless.51
Operative Management
An autograft reconstruction uses tissue from the body of the patient. Various tissues are used for grafts, including the gracilis tendon, fascia lata, semitendinosus tendon, and quadriceps muscle tendon. The bone–patellar tendon–bone (BPTB) autograft is a commonly used graft because of its boney anchor points. The BPTB and bundled gracilis and semitendinosus autografts have all been shown to have greater tensile strength to sheer forces than the original ACL.20,72 An allograft refers to biologic tissue taken from a human cadaver. The major risks of using allograft involve disease transmission and problems with effective sterilization procedures that do not weaken the graft.28
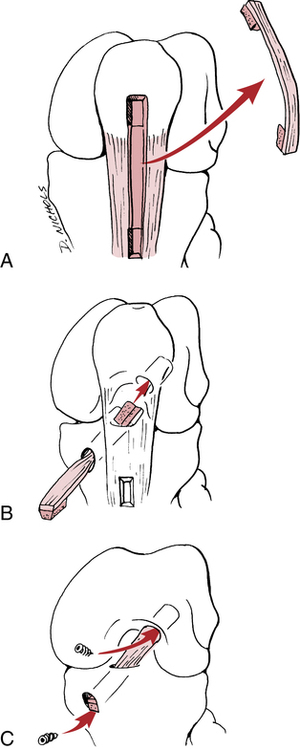
The arthroscopic central one-third BPTB autograft procedure involves harvesting the graft from the involved knee (Fig. 18-4, A) and surgically routing this structure through tunnels placed in the femur and tibia in a way that duplicates normal ACL anatomy, then securing the graft to the bone to allow for stable healing (Fig. 18-4, B-C). A small incision is made in the knee, and a small diameter drainage tube is inserted to help evacuate the joint of residual bleeding, which may increase the risk of arthrofibrosis if allowed to accumulate. This small drain is usually removed after a few days when the bleeding is controlled. Even with the placement of the drain, postoperative arthrofibrosis is a clinically significant problem that can occur.45 Sterile bandages are placed over the incisions, and the patient’s leg is often placed in a hinged brace locked in 0° of flexion.
Healing of the graft after surgery
Ligament healing processes and revascularization of graft material are vital concerns in the prescribed rehabilitation program designed by the supervising PT. The appropriate progression of the rehabilitation program depends on the PTA’s awareness of the various stages of healing after an autograft procedure. Once the graft is harvested and surgically routed within the knee, it begins a gradual process of avascular necrosis over the first 6 to 8 weeks.28 The graft gradually loses strength and is quite fragile during the first 2 months after surgery, so excessive loads and forces that would compromise the healing of the graft must be avoided during this time period. The graft slowly revascularizes, and at approximately 3 months the tensile strength of the graft is less than 50% of its original strength.28,75 Graft strength may take as long as a year to mature and may never reach preoperative tensile strength after the graft cell death and subsequent revascularization process.
Postoperative rehabilitation
In general terms, ACL reconstruction rehabilitation can be organized into three broad, interconnecting phases91:
1. Maximum-protection phase: From the first day postoperatively to approximately the sixth week after surgery.
2. Moderate-protection phase: From approximately the 7th to the 12th weeks after surgery.
3. Minimum-protection phase: From the 13th week after surgery until return to activity.
Maximum-protection phase (0-8 weeks)
Control of swelling is important throughout each phase of rehabilitation. Postoperative swelling can have a profound negative effect on the progress of the patient, even with suction drains inserted at the time of surgery. Swelling inhibits muscle contractions, contributes significantly to pain, limits joint motion, and can stimulate arthrofibrosis.85 Cryotherapy, elevation of the limb, and the use of a compression wrap help to minimize swelling.
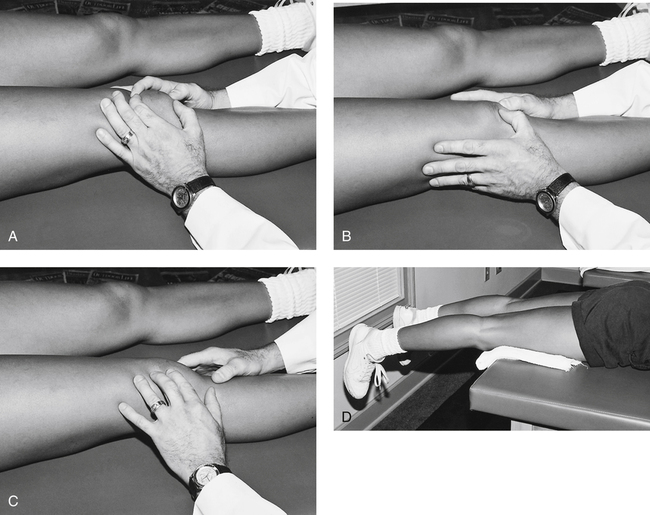
The patient’s ability to achieve early active range of motion (AROM) is an essential component of the maximum-protection phase. Patellar motion (caudal, cephalic, medial, and lateral glide) must be an immediate goal for the restoration of knee motion. Scarring from the graft harvest site and the suprapatellar pouch typically inhibits free patellar motion and full knee ROM.85 Initially the PTA must provide gentle stretching of the patella (Fig. 18-5, A–C) and instruct the patient to perform these stretches two to three times daily. Generally, full knee extension is achieved soon after surgery; if not, passive prone or supine knee extension stretches can be used judiciously to gradually increase knee extension (Fig. 18-5, D). In addition to active and passive knee flexion and extension, some authors advocate the use of a continuous passive motion (CPM) device for a limited time very early in this phase.28,76,91 The use of a CPM device has been suggested to help maintain a normal articular surface as well as to help evacuate synovial joint hemarthrosis and aid in the prevention of joint contracture.28,76,91 The use of CPM generally is limited to the period immediately after hospitalization.28
Weight-bearing status remains a controversial subject in the literature. In general, weight bearing with crutches is allowed as tolerated immediately after surgery, and patients should be full weight bearing somewhere between 2 and 6 weeks from surgery.21,28,91
The primary focus of strengthening the postoperative ACL patient during the maximum-protection phase is to encourage quadriceps control and hamstring strength. Strengthening exercises during the maximum-protection phase focus on isometric co-contractions of the quadriceps and hamstrings. Hamstring strengthening is emphasized during this phase of maximum protection because they act as dynamic stabilizers to limit anterior tibial shearing forces.28,63,76,77,91 Both standing leg curls and supine leg curls can be initiated during this phase if a brace is used.
Exercises that do not strain the ACL include10:
 Isometric hamstring muscle contraction exercises at 15°, 30°, 60°, and 90°
Isometric hamstring muscle contraction exercises at 15°, 30°, 60°, and 90°
 Isometric quadriceps contractions at 0° and 90°
Isometric quadriceps contractions at 0° and 90°
 Simultaneous contraction of the quadriceps and hamstring muscles at 60° and 90°
Simultaneous contraction of the quadriceps and hamstring muscles at 60° and 90°
 Active flexion-extension motion of the knee from 60° to full flexion81
Active flexion-extension motion of the knee from 60° to full flexion81
 Passive flexion-extension motion of the knee without muscle contraction
Passive flexion-extension motion of the knee without muscle contraction
Open kinetic chain (OKC) active knee extension, with or without resistance, causes an anterior tibial translation force relative to the femur that stresses the new graft. The largest anterior tibial translational forces occur between the knee flexion angles of 30° to 50°.81 This stated knee range of motion (ROM) should be completely avoided when performing OKC knee extension exercise in the early rehabilitation phases of ACL reconstruction.
Moderate-protection phase (6-12 weeks)
To advance to this level the patient must be FWB and should be able to demonstrate proper gait mechanics. Immobilization is generally discontinued around the fifth or sixth week postoperatively.21 Control of pain and swelling with the use of cryotherapy, compression, and elevation continues as indicated.
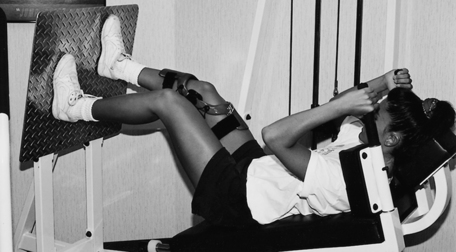
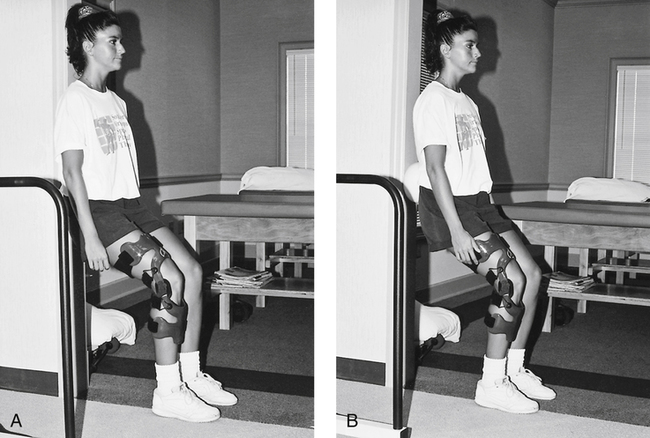
Closed kinetic chain (CKC) exercises are a system of interdependent articulated links in which motion at one joint produces motion at all other joints in the system in a predictable manner. CKC exercises and progressive proprioceptive tasks (to stimulate the afferent neural input system) are initiated and progressed throughout this phase. Gradual CKC progressive loads are essential to encourage functional muscle control, confidence in the use of the affected limb, and help stimulate neuromuscular coordination. Initial instruction in CKC exercises begins with the patient braced to protect the healing graft. Standing and shifting of body weight from the nonaffected limb to the affected limb is a safe and appropriate introduction to CKC exercises. Once the patient demonstrates confidence, muscle control, and stability, the brace is removed (with prior consultation and concurrence from the supervising PT) and the patient is allowed to shift weight without braced support. The leg press is used as a CKC exercise in a short-arc motion early in the moderate-protection phase while the patient is braced (Fig. 18-6). Progressive ROM exercises are allowed as tolerated. Standing wall slides also are introduced during the moderate-protection phase if the affected limb is braced and the tibia is kept vertical to avoid an anterior tibial translation force (Fig. 18-7). The short-arc step-up is an excellent exercise used to stimulate quadriceps control and strength. A biofeedback system can be used in conjunction with step-ups to encourage appropriate quadriceps firing patterns (Fig. 18-8).
Stationary cycling should be progressed with added time and resistance throughout this phase. The stationary bicycle is used initially to encourage ROM, but during the middle and later stages of this phase the bicycle can be used as an aerobic conditioning tool if the patient has achieved the required ROM, strength, and stability to perform endurance activities. Stair-steppers and inclined walking can also be introduced during this phase if the ROM and intensity of the resistance on the apparatus are modified and controlled initially to allow for protected joint motion (Fig. 18-9). To stimulate greater strength and local muscular endurance of the quadriceps, the patient can be instructed to perform the stair-stepper in a reverse manner.
Criteria that must be met by the patient before progressing to the next phase include the following:
Minimum-protection phase (12-24 weeks)
The minimum-protection phase signals the return to more normalized activities and the introduction of more challenging functional activities. Isolated knee ligament stability tests (e.g., Lachman test, anterior drawer test, and pivot shift test) are performed at the discretion of the PT and physician, usually during the moderate-protection and minimum-protection phases of rehabilitation. Ongoing documentation of the stability of the affected limb is essential to justify progression to more challenging exercises and quantify the clinical results of the surgery. The use of isokinetic testing of the involved limb is also left to the judgment of the PT and physician. Generally, isokinetic examinations are reserved for the moderate-protection and minimum-protection phases. Certain precautions must be taken to minimize the tibial translation forces produced with isokinetic testing and training to protect the healing graft. Positioning the pad proximally on the tibia helps to protect the reconstructed ACL against excessive anterior tibial translation forces.91
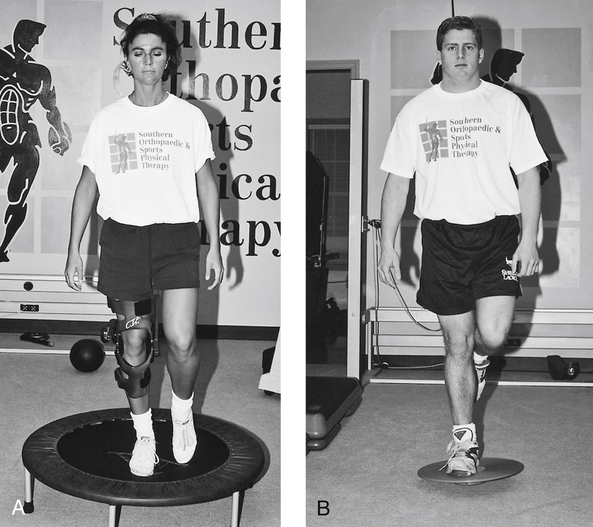
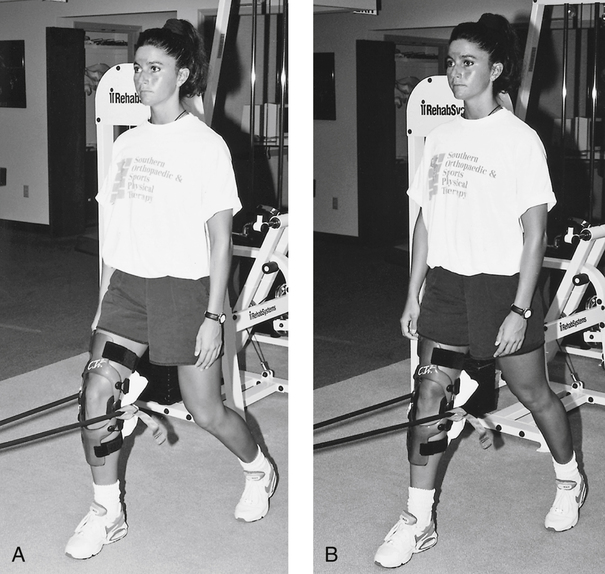
More progressive proprioceptive exercises can be initiated when clinical testing demonstrates improved strength, neuromuscular control, and stability of the ligament. The use of a balance board and minitrampoline further challenges the mechanoreceptor system (Fig. 18-10). Standing knee extension with resistance provided by elastic tubing is an excellent CKC exercise that encourages quadriceps control in more functional positions (Fig. 18-11).
Frequently, other structures are injured along with the ACL. The rehabilitation plan outlined does not account for possible injury to the meniscus, posterior cruciate ligament (PCL), MCL, lateral collateral ligament (LCL), or joint capsule; associated fractures; or impaired neurovascular structures. The complex nature and vast array of combined injuries dictates modifications at each level of rehabilitation and prolongs the healing process. Common injuries associated with an ACL rupture include a concomitant MCL sprain with a lateral meniscus tear.6,84 In regard to an injured MCL, or débrided meniscus, there will not be a large alteration to the rehabilitation process. In the case of a meniscus repair, it is common for the ACL reconstruction and the meniscal repair to be staged at different times ranging from 3 to 5 months apart. This is done to individually maximize the rehabilitation outcomes of the two surgeries. It has been found that surgical repair of both the ACL and meniscus at the same time yields poorer outcomes than staging the surgeries at separate healing intervals.14
Nonoperative Rehabilitation
The PTA also must be aware that isolated ACL injuries may dictate a nonsurgical course of treatment. The physician must decide if the patient is best suited for surgery or should be treated nonoperatively. If the patient is treated nonoperatively, the rehabilitation program progresses at a faster pace, although the injured knee must still be protected and allowed to heal from the trauma of the initial injury. The maximum-protection phase should range from 2 to 4 weeks, moderate-protection phase should range from 3 to 12 weeks, and minimum-protection phase ranging from 10 to 16 weeks from injury. The aforementioned time frames are approximate and should be based on each individual patient’s prior level of function and current goals with rehabilitation. It is suggested that returning to running after an ACL injury treated nonoperatively should be approximately 12 weeks.21
Posterior Cruciate Ligament Injuries
The primary function of the PCL complex is to restrict posterior tibial translation. It acts as a secondary restraint to tibial varus, valgus, and external rotations.100 Isolated PCL injuries occur less often than ACL injuries.7,17,22 PCL injuries are most commonly the result of some sort of trauma to the knee. Although high-velocity knee injuries often result in PCL tears in combination with other ligamentous injuries, this chapter will deal only with isolated PCL injuries.100
Etiology
The most common mechanism of PCL injury is a fall on a hyperflexed knee that results in a posterior translation of the tibia on the femur (Fig. 18-12).22,47,100 Other mechanisms include a dashboard injury from a motor vehicle accident that also causes the tibia to translate posteriorly on the femur. Hyperextension injuries can also tear the PCL, however this commonly will result in a concomitant ACL injury.100
Clinical Evaluation
Clinical examination of the PCL may be very complex and begins with a careful history to determine the mechanism of injury. When eliciting a history from a patient with an acute, isolated PCL tear, unlike with an ACL tear, the patient will often not report feeling a pop or tear.100 Patients with acute PCL tears will typically have mild to moderate knee effusion, a slight limp, pain in the back of the knee, and will often lack full flexion of the knee. More instability is experienced with combined injuries than with isolated tears. Patients with chronic PCL tears may complain more of disability, having difficulty doing things such as walking up or down inclines secondary to increased tibial movement on the femur.100
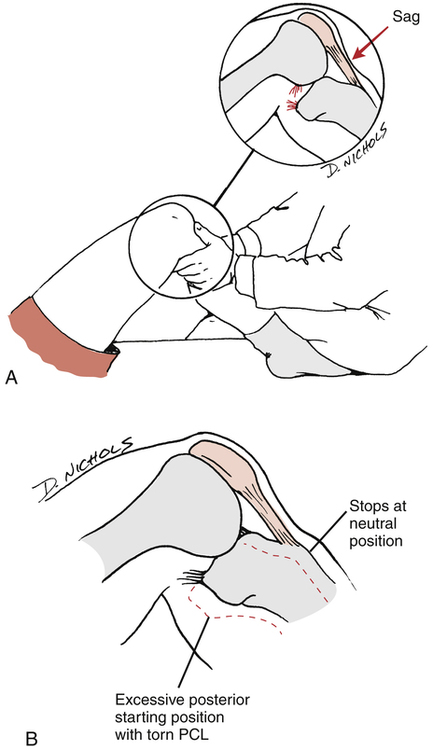
The most accurate test for the integrity of the PCL is the posterior drawer test.100 This test is performed with the patient supine, the knee at 90° flexion, and the tibia in neutral, external, and internal rotations. As seen in Figure 18-13, A, a positive posterior drawer test is observed when the tibia sags, or subluxes, posteriorly relative to the femur. In cases of isolated PCL tears, there is less posterior tibial translation with internal tibial rotation because the MCL and posterior oblique ligament contribute to this as a secondary restraint. Therefore there will be greater posterior tibial translation with the tibia in external rotation when the MCL and posterior oblique ligaments are not compromised. The examiner may produce a false-positive anterior drawer sign, where the posterior tibial sag actually is being reoriented to the neutral position rather than a true anterior translation occurring (Fig. 18-13, B).
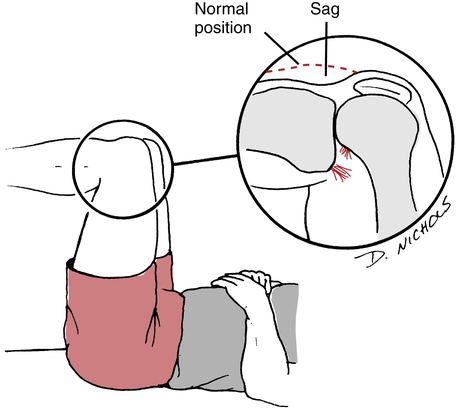
Another PCL laxity test is the Godfrey posterior tibial sag test. The patient is supine with the hip and knee of the affected limb held at 90°. Hold the heel of the affected limb and allow the tibia to translate, sublux, or sag posteriorly by gravity (Fig. 18-14).
Operative Management
Current surgical indications for PCL injuries include combined ligamentous injuries involving the PCL, symptomatic grade III laxity, and bony avulsion fractures.100 There are a number of graft options for patients seeking a PCL reconstruction. Autologous tissues that are available include BPTB and hamstring and quadriceps tendons, of which the BPTB is the most frequently used. To decrease harvest site morbidity and surgical time, the Achilles allograft is an alternative to the autografts just listed.22,29,100
Postoperative rehabilitation
Postoperative treatment may begin as quickly as the day after surgery. Patients may present with use of a knee immobilizer or hinged knee brace most often locked in full extension and use of crutches to decrease stress placed through the surgically repaired knee. Weight-bearing restrictions after PCL reconstruction vary from immediate full weight bearing to partial weight bearing (PWB) for 4 to 6 weeks.22,29
Maximum protection phase
Early physical therapy will include quadriceps setting, multiplane straight leg raises, patella mobilization, and ROM exercises to gain full extension. Hamstring isometrics at angles greater than 30° have been shown to increase strain on the PCL, and therefore should be avoided in the maximum-protection phase.63 Minimizing full knee flexion from 60° to 90° is necessary early in the rehabilitation to protect the healing PCL graft. Generally, full knee flexion ROM can be achieved by 2 months after surgery.22
Moderate and minimum protection phases
These phases of rehabilitation are similar to that of the postoperative ACL in terms of goals and time frames. Considered an agonist of the PCL, the quadriceps should be emphasized more than when rehabilitating a patient from an ACL reconstruction.63 The goal of the moderate protection phase (6 to 12 weeks from surgery) of rehabilitation is to restore full ROM and progress strength of the affected leg. The minimum protection phase consists of progressing strengthening exercises from bilateral to unilateral. Running and plyometric exercises for the athletic patient should be progressed in a similar fashion to that of rehabilitating the postoperative ACL. Return to sport can range from 6 to 9 months from surgery.
Nonoperative Rehabilitation
Nonoperative treatment is indicated for patients with acute, isolated grade I or II PCL tears.100 Patients may present with a knee immobilizer or hinged knee brace, along with crutches. Patients will begin physical therapy immediately to focus on decreasing inflammation, maintaining quadriceps tone, and restoring knee ROM. Rehabilitation exercises will include quadriceps isometrics, multiplane straight leg raises, and ROM. CKC strengthening may begin after 2 to 4 weeks as swelling, pain, and ROM improve. As mentioned previously, quadriceps strengthening should be emphasized because of the agonistic nature they have with the PCL to prevent posterior tibial translation.26,63 Stationary bike, elliptical, or pool work may be implemented to increase cardiovascular fitness. Plyometric and sport specific training may be implemented once adequate strength is demonstrated and the patient shows no signs of pain or swelling. Typical return to sport is approximately 6 to 8 weeks with low grade PCL sprains.100
Medial Collateral Ligament Injuries
Etiology
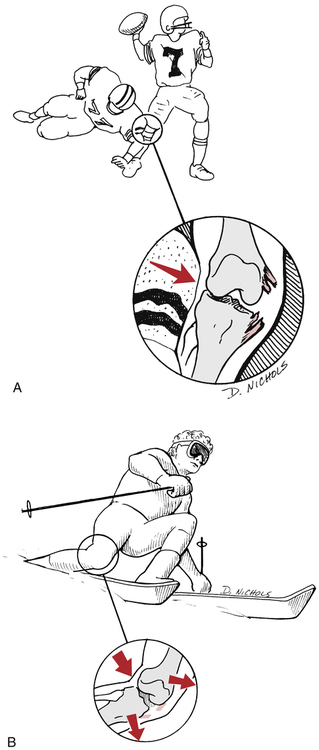
Injuries to the MCL are the most common ligament injuries seen in the knee.31,58,98 The MCL can be injured by direct contact to the lateral knee resulting in a valgus stress to the knee (Fig. 18-15, A). Uncommonly, a noncontact valgus or rotational stress to the knee can produce an isolated tear of the MCL when the lower leg is fixed and the tibia rotated externally (Fig. 18-15, B). Upon injury, patients may feel or hear a pop, but more commonly state they felt a tearing or pulling on the medial aspect of the knee. Patients will often present with swelling, and more severe sprains may present with ecchymosis. Patients will also walk with a limp; as they will be very hesitant to fully extend the knee because of increased stress and pain.
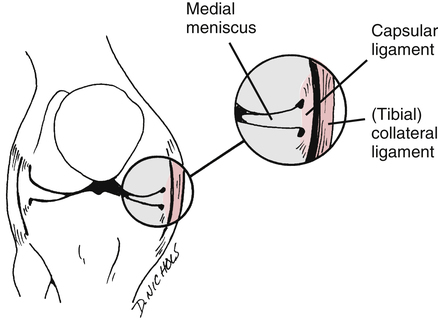
Literature shows the higher the grade of MCL lesion, the higher the incidence of an associated ligament injury; with grade III MCL injuries commonly associated with an ACL lesion.30 Because of a high rate of associated injuries to an MCL sprain, one must also bear in mind the anatomical relationship between the MCL and medial meniscus of the knee. The MCL and medial meniscus are attached to one another (Fig. 18-16), which helps in understanding how a blow to the lateral aspect of the knee may also injure the medial meniscus. O’Donoghue73 is credited with describing the unhappy triad as a combined injury to the MCL, ACL, and medial meniscus. However, as time has passed the more clinically common triad includes the MCL, ACL, and lateral meniscus.6,25,67,84
Clinical Evaluation
The most sensitive clinical test to describe the severity of an MCL sprain is the valgus stress test. This test is performed with the patient supine on an examining table while the examiner stands to the side of the affected limb at the level of the distal tibia and the affected knee flexed to 30°. The medial aspect of the distal tibia is firmly grasped with one hand, while the other hand is used to apply a valgus force to the lateral proximal joint line. The examiner’s valgus force will cause the medial joint line to gap, or open, and place stress through the MCL. Gapping with the knee in full extension suggests there may be significant injury to multiple structures including the MCL, ACL, PCL, and posterior capsule.47
Rehabilitation
Consensus is that isolated grade I-III MCL injuries can be treated nonoperatively.4,42,49,68 Patients will initially present with the use of crutches and a hinged knee brace to decrease valgus and rotational forces. In this early maximum-protection phase, the goal is to decrease inflammation, restore ROM, and increase quadriceps tone. Exercises will consist of knee ROM exercises, quadriceps setting, and multiplane straight leg raises without creating unnecessary valgus stress across the affected knee. Patients may progress to FWB within 1 to 2 weeks from injury as pain and quadriceps strength allows.
If normal gait mechanics exist and strength and ROM allow, a running progression may start as early as 6 weeks from injury. Plyometric strengthening may start at the same time, progressing through different planes of movement as discussed previously. General return to sport will happen between 8 and 12 weeks from injury. A functional brace may be suggested to further protect the injured MCL when return to sport is permitted.24
MENISCUS INJURIES
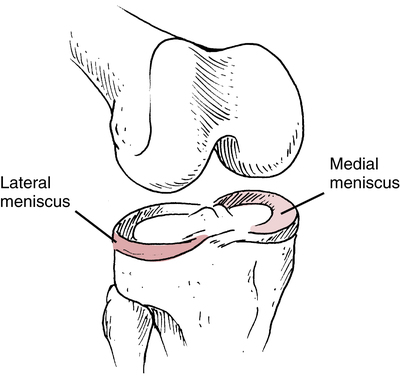
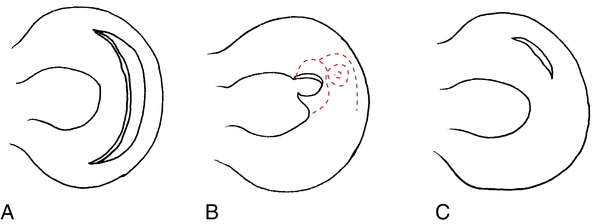
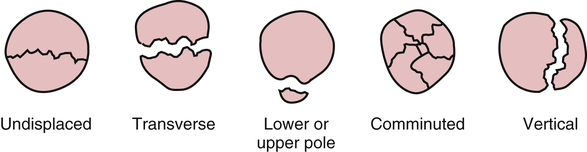
The menisci are C-shaped or semicircular fibrocartilaginous structures with bony attachments at the anterior and posterior aspects of the tibial plateau, which contain primarily (90%) type I collagen.3,37 The medial and lateral menisci of the knee serve as extensions of the tibia and provide for reception of the femoral condyles onto the surface of the tibia (Fig. 18-17).3 The menisci are important in many aspects of knee function, including stability, shock absorption, load transmission, nutrition, lubrication, joint stress reduction, increased congruity, and contact area.15,37,40,44,48 Injury to the meniscus can result in many patterns of tears (Fig. 18-18). Five main types have been identified,32 as follows:
The most common tears are flap (oblique) or vertical longitudinal, which occur in nearly 81% of meniscus tears. Vertical longitudinal tears can be complete (bucket handle tears) or incomplete and most often occur in younger individuals. Complex or degenerative tears are more common in individuals older than 40 years of age. Transverse or radial tears are often seen in isolated meniscus injuries or in conjunction with other meniscus tears. Lastly, horizontal tears are thought to be the result of shear forces generated by axial compression. They are very common in the lateral meniscus with runners.37
Etiology
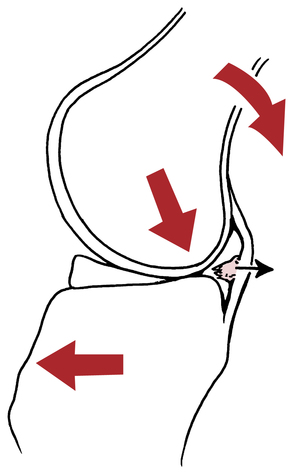
The meniscus can be injured by sudden trauma or gradual degeneration.3,15,32,44 As mentioned, traumatic meniscus injuries are most common in a younger population, whereas degenerative tears occur more frequently to individuals older than 40 years of age.3,37 Noncontact, weight-bearing injuries to the meniscus usually involve combined forces of knee flexion, rotation, compression, and shear (Fig. 18-19).3,15,32 Degenerative tears can be subtle and do not usually involve a history of sudden overt trauma. Generally with degenerative tears, some type of insignificant activity (squatting or getting out of a car) precedes the symptoms of pain, swelling, and locking of the knee.
Clinical Examination
Apley compression and distraction test is used to determine if the injury is ligamentous or meniscal.83 To perform this test, the patient is prone with the affected knee flexed to 90°. The distal femur is stabilized with a strap or hand. The free hand is used to grasp the distal tibia and provide a distraction and internal-external rotation force to the tibia. Pain signifies the possibility of a ligament tear. The compression component of this examination is performed in the same manner, except that the free hand applies a compression and rotational force to the distal tibia. Pain with compression and combined internal and external rotation on the flexed knee suggests the presence of a meniscal lesion.
The McMurray test also is used to reproduce symptoms of a torn meniscus.32,83 The patient is supine with the hip and knee of the affected limb fully flexed. To test for the presence of a medial meniscus lesion, a valgus force to the knee is applied with one hand while an external rotation force is applied and the knee is extended by holding the distal tibia with the other hand. To test for a lateral meniscus tear, a varus force with internal tibial rotation is provided. With either internal or external rotation of the knee, if a tear is present, the patient may experience pain and an audible or palpable snap or pop may occur.
The bounce home test is designed to determine if a torn meniscus is preventing knee extension.83 The patient is supine with the affected knee flexed and supported by the examiner’s hand. The knee is passively extended to full extension. If the meniscus is torn, the knee may not fully extend because the torn tissue blocks extension and creates a rubbery, springy end-feel.61
The Thessaly test has been shown to be the most accurate clinical test to detect a meniscus tear.52 The patient stands on the affected limb with the knee flexed 5° or 20°. The examiner supports the patient’s outstretched arms while the patient rotates their knee internally and externally three times. Joint line discomfort or a sense of catching or locking of the knee is considered a positive test.52
Management
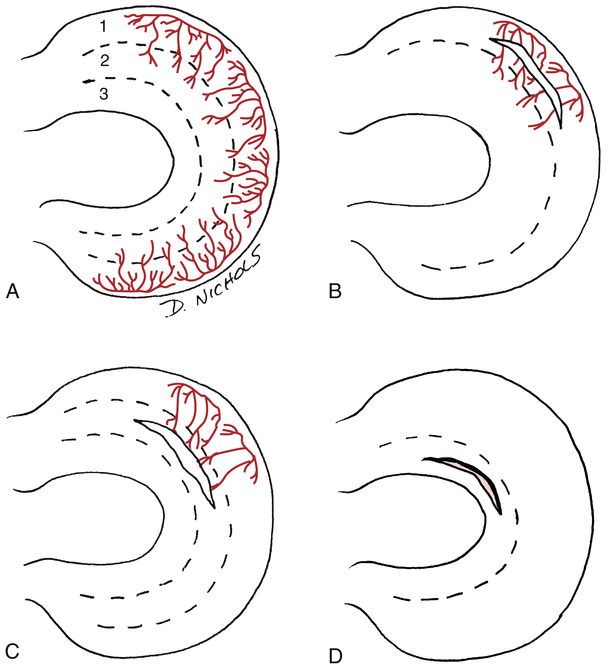
The rationale for treatment options is directly related to the location of the tear in the meniscus and the ability of the meniscus to repair itself. The vascular anatomy of the medial and lateral meniscus is reserved for the peripheral 10% to 30% of its width (Fig. 18-20, A).3 The remaining portions are relatively avascular and aneural. Researchers and surgeons recognize a zone classification of injury related to the vascular supply of the meniscus.3,40,44,83 The injured meniscus may or may not heal or repair itself, depending on the location of the tear. A zone I tear is recognized as red-on-red because the location of the tear is vascular on both sides (Fig. 18-20, B). Injuries in this area may heal better than those in other areas because of the blood supply. Because of this blood supply in the red-on-red area, some surgeons elect a nonsurgical course of treatment. A zone II tear is located in the red-on-white area of the meniscus (Fig. 18-20, C). A tear in this area has a vascular supply on only one side. These tears also may heal because of the communication with a blood supply. A zone III tear is located in the nonvascular central body of the meniscus called the white-on-white area (Fig. 18-20, D). An injury in this area does not heal because there is no blood supply to support the healing process.
Surgical indications for arthroscopic treatment of meniscal pathology include the following: (1) symptoms of meniscus injury that affect activities of daily living, work, or sports; (2) positive finding from clinical examination; (3) failure to respond to nonsurgical treatment; and (4) absence of other causes of knee pain identified in clinical examination or imaging studies.66 The age of the patient, the stability of the knee, the location of the tear, and the integrity of the meniscus should all be considered when deciding on the course of treatment.32
Surgical Procedures
Although infrequent today, total meniscectomy was once a common procedure for meniscus injury. Joint space narrowing and osteophyte formation are common problems that have led to a decrease in total meniscectomy surgeries.3,32,38,83 Current treatment of meniscal injuries is to maintain as much viable tissue as possible by avoiding total meniscectomy and investigating the possibility of surgical repair.
Subtotal or partial meniscectomy
To avoid the long term affects of total meniscectomy, partial meniscectomy is advised when a meniscus repair is not feasible. Preservation of the load-bearing functions of the meniscus is the foundation for a partial meniscectomy. The long-term consequences of subtotal meniscectomy must be clearly understood when addressing functional activities and return to athletics. Early degenerative changes are seen with both total and partial meniscectomy, and include narrowing of the tibiofemoral joint space, formation of bone spurs (osteophytes), and degeneration of the femoral articular surface on the side of the surgery.3,32 Counseling and education of the patient focus on modifying their activities of daily living (ADLs) related to stair climbing and repetitive vertical compressive loading.
Meniscal repair
Multiple surgical options are available when considering meniscal repair, which include nonfixation healing enhancement (meniscal trephination or synovial abrasion), open repair, arthroscopic repair (inside-out, outside-in, all inside suture techniques), and nonsuture techniques (biomaterial). A review of the literature showed that meniscal repairs demonstrated greater potential for healing under the following conditions: (1) repairs involve the lateral meniscus; (2) meniscal injuries are acute; and (3) repairs are performed in conjunction with ACL reconstruction.38,90
Postoperative rehabilitation
Physical therapy often begins in the maximum protection phase (weeks 0 to 6) with protective weight bearing, the use of a brace locked into extension, and restricted ROM to 90° flexion. Delaying FWB status until 4 to 6 weeks is recommended to avoid vertical compression forces into the repaired tissue.48 Exercises include patella mobility, knee ROM limited to 90° of flexion, quadriceps setting, straight leg raises, and gait training. If the patient will be non–weight bearing, (NWB) it is important to include open-chain multiplane hip strengthening and ankle and foot strengthening. Progression of exercises into closed-chain strength training will be dependent upon the weight-bearing restrictions, which may remain until 4 to 6 weeks after surgery.
Meniscal transplantation
In an effort to restore normal knee anatomy and biomechanics, meniscal allografts can be used to replace the damaged meniscus. When surgical indications are adhered to, studies have shown excellent results in pain relief and improved function.18 Surgical indications for meniscal allograft transplantation include prior meniscectomy, continued pain with intact articular cartilage, normal anatomic alignment, and joint stability.18,38 Specific age limits are not available, but generally patients who are older than 50 to 55 years already have a degree of arthritis that would contraindicate the procedure. Other contraindications include inflammatory arthritis, obesity, and previous infection.18
Meniscus transplantation can be performed as either an open or arthroscopic technique. Other procedures that may be performed in conjunction with meniscal transplantation are high tibial osteotomy to provide improved alignment, or reconstruction of the ACL to increase joint stability. Success rates of meniscus allograft transplants vary depending on the criteria used to determine success. It has been shown that knees with advanced arthrosis have a greater risk for graft failure.18
Postoperative rehabilitation
In rehabilitation of allograft meniscal transplantation a conservative approach is recommended. Patients will present postoperatively as NWB and with ROM limitations of 0° to 90° flexion. Postoperative rehabilitation will vary widely, but should closely resemble the rehabilitation of a meniscal repair. Most surgeons will provide a program that allows running at 4 to 6 months and full activities at 6 to 9 months.18
ARTICULAR CARTILAGE LESIONS
Articular cartilage is known to protect the subchondral bone and to reduce friction of the joint.62 It is suggested that isolated chondral lesions may progress to symptomatic degeneration of the knee, and therefore surgical intervention may be warranted to provide pain relief and restore normal joint congruity.18,60 Surgical options include arthroscopic débridement, microfracture, osteochondral grafting, and autologous chondrocyte implantation (ACI).
Operative Management
The microfracture procedure involves several holes being punctured into the subchondral bone, which creates a bleeding response of marrow into the area of the chondral lesion.87 The marrow formulates into a fibrocartilaginous clot to protect the underlying subchondral bone.55,80,87 Osteochondral grafting is a procedure in which cylindrical osteochondral grafts are harvested from the NWB surface of the femoral condyles and strategically placed within the area of the chondral lesion.41 ACI involves two surgical procedures. The first procedure is an arthroscopic evaluation of the chondral lesion as well as a chondrocyte biopsy from the articular cartilage from a small section of a femoral condyle. Those chondrocytes are then cultured for a approximately 3 weeks and then injected back into the area of the chondral lesion (see Fig. 10-6). The injected chondrocytes are held in place by either a periosteal patch from the patient’s tibia or a synthetic collagen patch.19,33,62 Variables such as patient age, weight, activity level, chondral lesion size, and other concomitant knee pathology dictate which procedure is best for each patient.
Postoperative Rehabilitation
Rehabilitation progression for microfracture, osteochondral grafting, and ACI procedures are quite similar. Most authors agree to minimize weight bearing if the resurfacing technique was performed on the weight-bearing surface of the tibia or femur. The patient may be NWB for 2 to 8 weeks after surgery.33,39,56,80,87 If the surgery was for the patellofemoral joint, the patient may start weight bearing soon after surgery with their knee immobilized or in a hinged brace allowing up to 20° of flexion.39,87 A CPM machine may be prescribed because this has been shown to be beneficial for tissue repair.39 Primary goals throughout this time are to protect the healing tissue, initiate patella mobilization, minimize joint swelling, restore ROM, and to begin isometric exercises as discussed previously.33,39 Cardiovascular fitness should be promoted with the use of a stationary bike with minimal resistance, or the use of an upper body ergometer (UBE).
Authors seem to agree that returning to sport should happen between 6 and 12 months after surgery.33,39,56 Low-impact activities such as skating and cycling may begin by 6 months after surgery. Basic agility work as well as pool running may also begin at this time. Roughly 8 months after surgery, the patient should start an interval running program on land as well as a plyometric exercise progression. High impact sports such as tennis and basketball should not start until close to 12 months out from surgery.33
PATELLOFEMORAL PATHOLOGIC CONDITIONS
Etiology
Pathology of the patellofemoral joint is one of the most common disabilities of the knee joint in orthopedic and sports medicine.94 Several authors have speculated differences in flexibility, strength, and neuromuscular control to be causes of patellofemoral pain (PFP). What seems to be consistent is that people with PFP have decreased gastrocnemius and soleus flexibility78 and decreased hip external rotation and abduction strength78,89; they also tend to demonstrate increased hip internal rotation with CKC activities such as running.89 Most patients with PFP will complain of anterior knee pain with prolonged sitting (theater sign), stair ambulation, and squatting motions.
Physical Examination
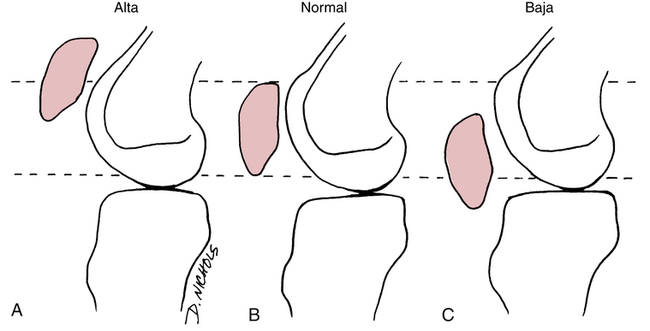
In general, the patella is referenced to the femur in three positions (Fig. 18-21). A patellar posture that is more superior than normal is referred to as patella alta50,67,96 and is associated with greater patellar instability.67 Excessive hamstring tightness can increase patellofemoral compression because patellar excursion through knee extension is resisted by hamstrings, requiring more quadriceps force and causing increased compression forces of the patella into the femur (Fig. 18-22).50 Testing for rectus femoris and iliotibial band (ITB) inflexibility should also be performed, because these structures have been linked to decreased PFP if flexibility is restored to normal.94
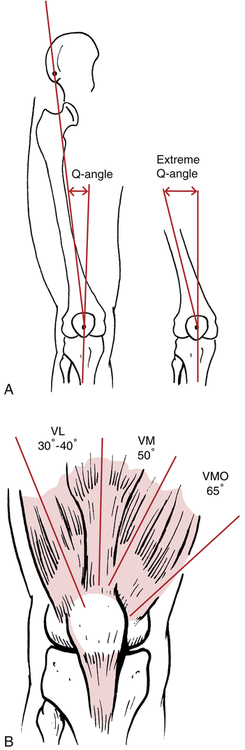
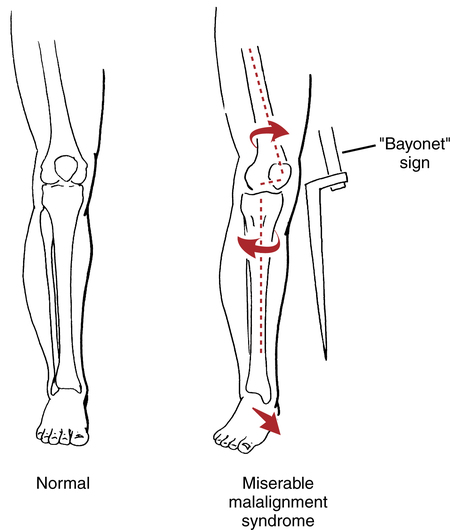
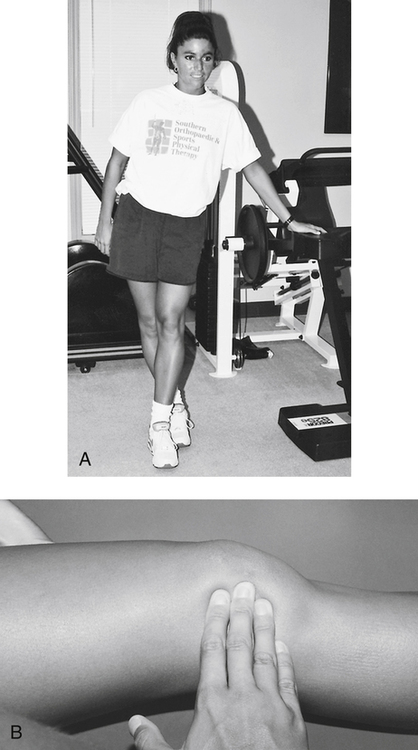
In addition to patellar posture and muscle stiffness, the quadriceps angle (Q angle) is a clinical assessment that relates to patellar tracking deviations and variations in the line or angle of pull of the quadriceps on the patella.67 The Q angle refers to a line drawn from the anterior superior iliac spine (ASIS) through the center or axis of the patella and distally to the insertion of the patellar tendon on the tibial tubercle (Fig. 18-23, A). The Q angle can be increased by proximal tibial external rotation or distal tibia varus.50,96 Figure 18-23, B, shows the various angles of muscular pull on the patella and how an increased Q angle can affect the tracking mechanisms of the patella during flexion and extension. Miserable malalignment syndrome (Fig. 18-24) is assessed with the patient in the standing position and provides objective data for the physician and PT about the entire lower extremity kinetic chain, patellar tracking dysfunction, and pain.50,67,96 This syndrome is characterized by femoral anteversion (internal femoral rotation), “squinting” patellae (patellae facing toward each other), proximal external tibial torsion (which results in what is called the bayonet sign), and foot pronation.9,96 Miserable malalignment syndrome results in an increased Q angle and can result in lateral tracking of the patella. It has been suggested that the Q angle is not just a valuable tool as a static measurement; it should also be observed during CKC activity, such as a single leg squat.79
Nonoperative Rehabilitation of Anterior Knee Pain
Strengthening of the quadriceps muscle group is initiated by introducing isometric sets that do not produce pain. In some instances, submaximal isometric quadriceps sets are necessary at the beginning of the program to accommodate pain. The vastus medialis oblique (VMO) is the focus of attention when addressing the quadriceps strengthening because of its ability to stabilize the patella superiorly and more importantly, medially.9 The superior-medial pull of the vastus medialis muscle directly counteracts lateral tracking syndromes. Equally important, is to perform isolated strengthening exercises of the hip abductors, external rotators, and extensors.
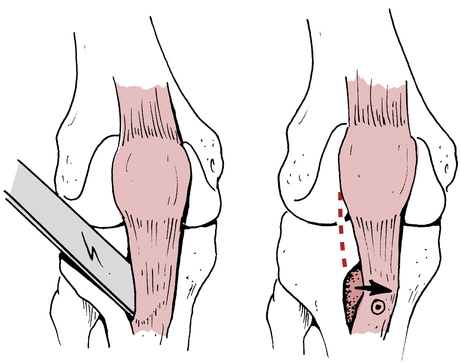
In conjunction with quadriceps and hip strengthening, tight lateral structures that act to pull the patella laterally must be treated manually and with appropriate stretching. Stretching the hamstrings and ITB (Fig. 18-25, A) and performing manual patellar-stretching exercises (Fig. 18-25, B) are essential to counteract anterior knee pain that results for a lateral tracking patella.94,95 Also, quadriceps, gastrocnemius, and soleus inflexibility should be addressed in the initial phase of rehabilitation.
Once acute inflammation has subsided, CKC strengthening exercises are introduced to promote higher level functional strengthening. Multiplane hip strengthening, leg press, squats, walls squats, and step-ups are all appropriate progressions. ROM, resistance, and step height may all need to be modified to allow the patient to perform without pain. It is important to understand that significant increases of patellofemoral joint stress are shown to happen between 0° and 30° of knee flexion with open-chain exercises, and between 60° and 90° with closed-chain exercises.88 Biofeedback units used on the VMO during CKC is an excellent way to emphasize proper muscular activation. CKC exercises should be progressed from bilateral to unilateral as pain and strength allow. Emphasis should be placed on alignment as the exercises progress. Encouraging joint stacking, where the patient controls hip adduction and internal rotation, will reduce valgus angulation across the knee and in turn will help reduce PFP.64,99
Supportive devices can help dynamically stabilize the patella and promote normal tracking throughout this phase of rehabilitation. Commercially available patellar stabilizing sleeves provide a lateral buttress support to the patella to minimize lateral tracking. Various taping methods can be incorporated for dynamic stability as well. The use of foot orthotics in patients with increased pronation has shown to be useful in decreasing pain by improving lower extremity alignment.12 These devices may be necessary for the patient to progress through CKC strengthening without pain.
It is important to incorporate pain-free cardiovascular exercise to build muscular endurance and promote patellofemoral joint health. Elevated treadmill walking, both forward and backward, may be most beneficial for muscle activation while minimizing stress to the patellofemoral joint.16,57 Swimming and using a stationary bike and elliptical trainer are all appropriate nonimpact cardiovascular modalities as long as they are pain free for the patient.
When considering return to sport and discharge criteria for patients with PFP it is important for the clinician to thoroughly evaluate lower extremity mechanics as it relates to alignment with running, jumping, and cutting activities. Lower extremity jumping mechanics appear to be consistently different among individuals with PFP.99 Conservative treatment programs that include kinematic retraining may improve patient outcomes and prevent recurrence of this common orthopedic condition.64,79,99
Operative and Postoperative Management for Patellofemoral Pain
Surgical management of patellofemoral disorders can be classified as proximal realignment procedures, distal realignment procedures, and procedures to address articular cartilage abnormalities.96
Proximal Realignment
The basic goal of operative management for anterior knee pain related to lateral patellar tracking disorders is to reestablish appropriate extensor mechanism function and reduce patellofemoral contact forces.35
Proximal realignment procedures involve lateral retinacular release with or without VMO advancement.93 Rehabilitation after proximal realignment procedures is essentially the same as for nonoperative treatment of anterior knee pain. However, pain and swelling after surgery, as well as specific tissue healing and time constraints, must be addressed carefully. Therefore the initial course of management after proximal realignment procedures is focused on the use of ice, lateral patellar compression, limb elevation, temporary immobilization, weight bearing as tolerated, and NSAIDs as prescribed by the physician. Control of pain and swelling is essential to reduce the quadriceps inhibition they produce.
Distal Realignment
The goal behind distal realignment surgeries is to reduce severe patellofemoral compression loads and significant patellar subluxation by surgically removing the extensor mechanism’s insertion (patellar tendon attachment on the tibial tubercle) and reattaching the tibial tubercle to a more mechanically advantageous site to improve the pull of the quadriceps (Fig. 18-26).9
Individual circumstances and surgical procedures dictate variations in this initial management plan. Significant modifications in rehabilitation are necessary with distal realignment procedures based on bone and soft-tissue healing and promotion of quadriceps strength. Generally, immobilization with a hinged range-limiting brace is used for 4 to 6 weeks.9,96 Crutches are encouraged for about 6 weeks, with initial NWB progressing to toe-touch weight bearing and then to FWB over the full 6 weeks of immobilization.9,96 Gradual progression of flexion ROM is advised; achieving approximately 100° of knee flexion for the first 2 weeks and progressing to 120° by 6 weeks.9 Isometric quadriceps sets and straight-leg raises are encouraged once pain, swelling and tissue healing allow. With extensor mechanism repair, as well as radical distal realignment procedures, a few weeks’ delay is necessary before initiating quadriceps sets and straight-leg raises so as not to endanger the surgical repair site. Many remedial quadriceps strengthening exercises can be performed in the brace during the early phases of recovery. The moderate protection phase after 6 weeks from surgery will be a similar progression of exercises as those mentioned with nonoperative rehabilitation.
Articular Cartilage Procedures
Arthroscopic procedures are used to directly address the condition of the articular cartilage on the undersurface of the patella and the femoral condyles in cases of anterior knee pain. The term chondromalacia describes retropatellar articular cartilage degeneration or softening. The diagnosis of chondromalacia only can be made at the time of surgery because visualization of the articular surface is necessary.67,96
Various surgical procedures are used to smooth rough articular surfaces and stimulate an inflammatory response to enhance healing. Perforation or abrasion of subchondral bone (chondroplasty, microfracture and abrasion arthroplasty) stimulate a communication between the damaged articular surface and vascular supply of subchondral bone.9 Acute postoperative management includes ice, elevation, compression, NSAIDs, protected weight bearing and possible use of a CPM at home. The PTA must pay close attention to complaints of pain and objective signs of swelling with all exercise progressions. Progression of exercises has been discussed in the articular cartilage section of the chapter.
FRACTURES
Patellar Fractures
Etiology
Fractures of the patella can occur with direct or indirect trauma. 96 The most common injury involves the patella making contact with a hard surface. Less frequently the patella can be fractured by a violent contraction of the quadriceps. 65,96 Avascular necrosis (AVN) can result if a transverse fracture occurs, because the vascular supply to the patella is reserved for the central portion of the distal pole, leaving the proximal segment of the transverse fracture prone to AVN.65
Nonoperative Rehabilitation
Rehabilitation management of nondisplaced patellar fractures treated with immobilization and limited weight bearing is primarily supportive throughout the literature. Nondisplaced patellar fractures are often treated conservatively with immobilization of the affected limb in full extension for 4 to 6 weeks. 59,65,96 The unaffected limb can maintain strength and flexibility using quadriceps strengthening exercises. Aerobic fitness can be enhanced with the use of single leg stationary cycling or an UBE. Ankle pumps are encouraged for the affected limb throughout immobilization. Quadriceps sets, short-arc knee extensions and straight leg raises are introduced gradually once sufficient bone healing has occurred. If quadriceps strengthening exercises and knee flexion exercises are initiated too soon, the force of muscle contraction and knee flexion stretching may separate and stress the fracture site, slowing the healing process and leading to fracture displacement.
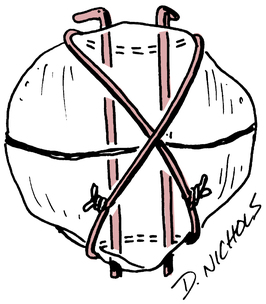
Operative Management
Surgery for displaced patella fracture is indicated when the bone fragments exceed 3 to 4 mm in separation.59 Stabilization of displaced patellar fractures is best accomplished with an open reduction with internal fixation (ORIF) procedure. Figure 18-27 portrays various patellar fracture patterns. The most common fixation devices are tension band wiring and cerclage wiring (Fig. 18-28). The tension band wire is a dynamic compression device that approximates and compresses the patellar fragments. The additional use of cerclage wiring adds to the stability of the repair and allows early joint motion without redisplacing the fracture fragments.96
Supracondylar Femur Fractures
Operative Management
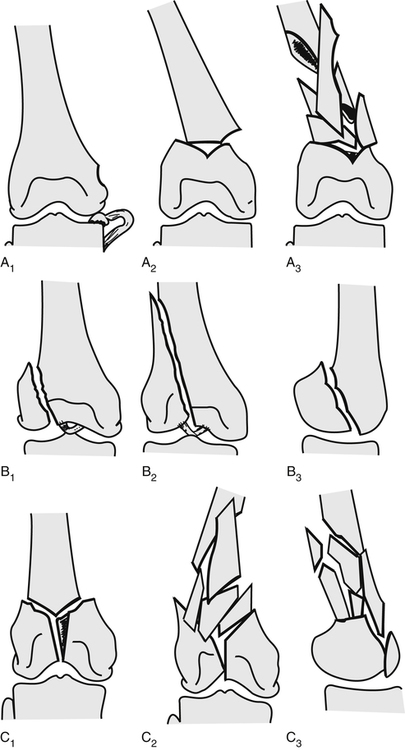
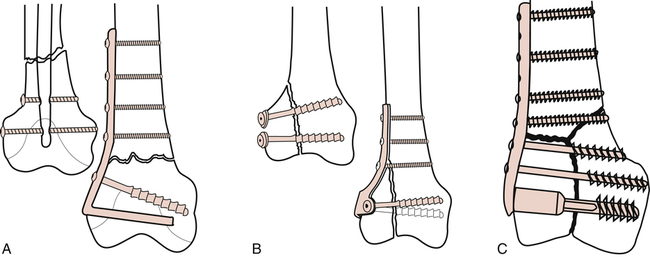
Distal femur fractures generally are classified as extraarticular, unicondylar, or bicondylar65,67 (Fig. 18-29). These fractures are usually managed with an ORIF procedure. Figure 18-30 demonstrates fixation devices used for transverse supracondylar fractures, unicondylar fractures, and type C (T– and Y-pattern) fractures. The method of fixation focuses on fracture site stabilization and fragment apposition while minimizing the pull on the fracture site by the quadriceps, hamstrings, and calf muscles.59,65
Proximal Tibia Fractures (Tibial Plateau Fractures)
Operative Management
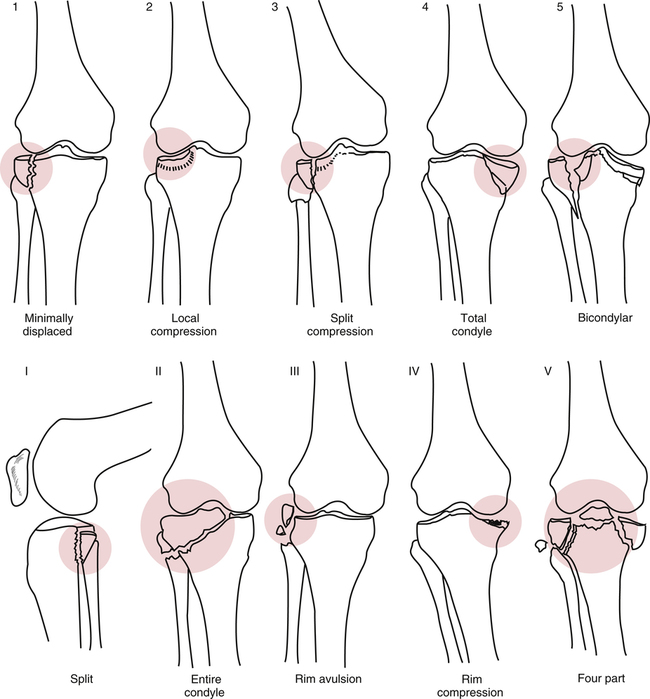
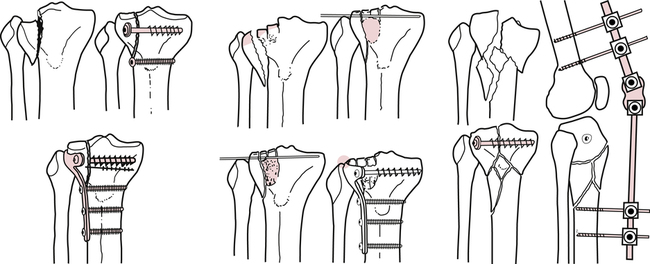
Displaced proximal tibial fractures are treated with an ORIF procedure. Figure 18-31 illustrates the different types of tibial plateau fractures. Various internal fixation devices used with different fracture patterns are illustrated in Figure 18-32. Postoperative management and rehabilitation of tibial plateau fractures follow the course of bone and soft-tissue healing. First, the patient is placed in a leg immobilizer or fracture brace in full extension. Active quadriceps sets are performed and the patient is generally NWB or partial weight bearing, depending on the severity of the fracture. After initial surgical wound healing has occurred, knee flexion exercises can begin based on the patient’s tolerance.
Nonoperative and Postoperative Management of Supracondylar and Tibial Plateau Fractures
Physicians usually treat nondisplaced distal femur and proximal tibial fractures nonoperatively with closed reduction of the fragments and tibial traction for approximately 8 to 12 weeks.59 Physical therapy management of supracondylar and tibial plateau fractures is guided extensively by the healing process of bone and associated soft tissue. Generally, patients have limited weight bearing for 8 to 12 weeks. NWB is followed strictly until subsequent radiologic assessment determines secure bone healing. Arthrofibrosis and quadriceps adhesion to the bone are frequent problems, with significant bleeding and associated tissue damage in distal femur fractures. Therefore early postoperative management focuses on patellar mobility (within the confines of the knee brace or immobilizer), active quadriceps-strengthening exercises (quadriceps sets and straight-leg raises), and active knee flexion to minimize knee contractures. It is imperative to encourage strengthening and flexibility exercises for the uninvolved limb and instruct the patient in a general fitness program that does not compromise the healing of the injured limb.
High Tibial Osteotomy
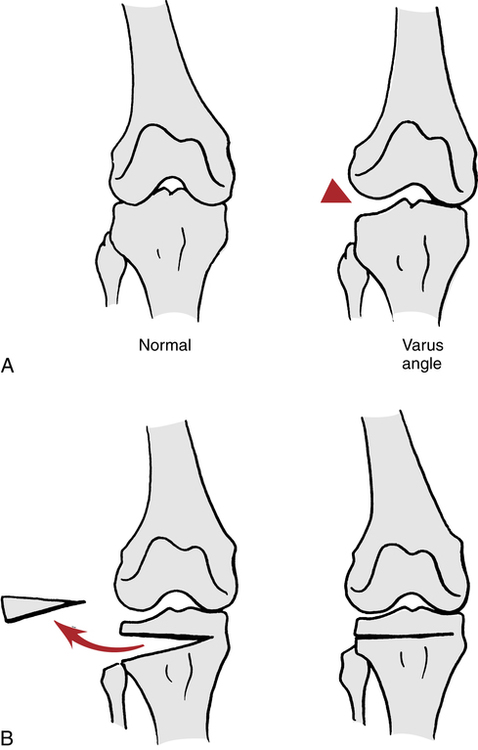
A tibial osteotomy procedure can be performed on patients who demonstrate advanced degenerative joint disease (DJD) of one compartment of the knee.67 Most commonly, this is the medial compartment and is characterized by a varus (bow-legged) deformity that creates abnormal loads on the medial aspect of the tibiofemoral joint.72 Less frequently, the lateral compartment is involved and creates a valgus deformity (knock-knees) (Fig. 18-33). This procedure is generally considered a temporary solution, approximately 10 years, before a total knee replacement (TKR) is considered.67 Patients younger than 50 years of age with greater than 120° flexion have a higher probability of success with a high tibial osteotomy (HTO).70
HTO attempts to realign the tibiofemoral joint by surgically creating a wedge in the proximal tibia or distal femur, depending on varus or valgus deformity, and redistributing the forces and compressive loads more evenly across the joint (Fig. 18-34). In valgus deformity associated with lateral tibiofemoral compartment destruction, a distal femur (supracondylar) closing-wedge osteotomy is performed and is stabilized with a plate.67,86 Depending on the wishes and training of the surgeon, some patients use CPM immediately postoperatively to facilitate early flexion motion.86
Postoperative Rehabilitation for High Tibial Osteotomy
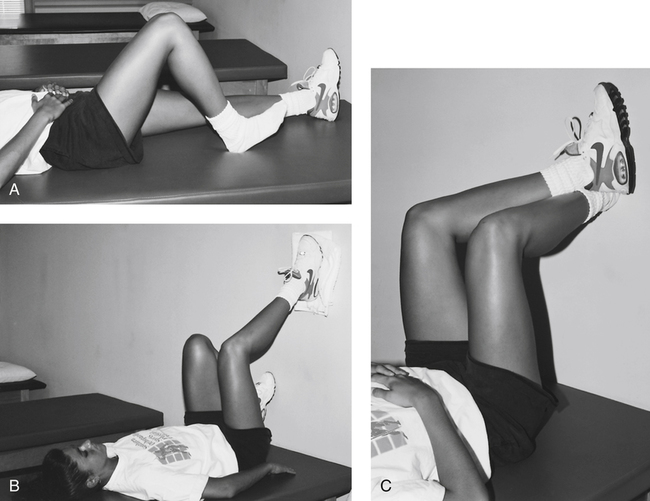
Usually the knee is placed in an immobilizer in full extension with a suction drain inserted to help evacuate the excessive accumulation of blood. Initially, strengthening exercises (quadriceps sets, straight-leg raises in the splint, and gluteal sets) are performed and advanced from the first day postoperatively. Manual patellar stretching is encouraged once initial surgical wound healing has occurred, especially with distal femoral wedge osteotomy (preoperative valgus deformity caused by lateral joint compartment disease) because the procedure involves extensive invasion of the quadriceps.86 If CPM is not used, the patient is allowed out of the immobilizer several times a day to perform active knee flexion exercises (Fig. 18-35). As patellar mobility (caudal-cephalic motion) improves, progressive knee flexion ROM exercises are added with the patient in a sitting position to allow gravity to influence the flexion range of the affected limb. Care must be taken to manually assist the affected limb from sudden flexion and encourage quadriceps relaxation.
Weight-bearing status after HTO is guided primarily by the time constraints of bone healing.86 Usually touch-down weight bearing (TDWB) is allowed after surgery with the aid of crutches or a walker for up to 12 weeks.86 Progressive resistive exercises for the quadriceps and hamstrings are initiated gradually within the first 3 to 4 weeks after surgery. Usually ankle weights, Thera-Band resistance, seated isotonic quadriceps and hamstring exercises, and cables and pulleys can be added cautiously during the moderate-protection phase of recovery (7 to 12 weeks).91 Knee flexion ROM improvement is encouraged by using supine wall slides, seated knee flexion, prone knee flexion, and stationary cycling.
Total Knee Replacement
Knee Arthroplasty
The indications for TKR are primarily to eliminate or reduce pain and improve functional activities in severely disabled patients.34,36,67 Osteoarthritis (DJD) and rheumatoid arthritis contribute significantly to unicompartmental (medial or lateral), bicompartmental (both medial and lateral joint compartments), and tricompartmental (medial, lateral, and patellofemoral compartments) pain and dysfunction.34,36,67,92
Basic contraindications for TKR are active or recent septic arthritis, a “nonfunctioning extensor mechanism or severe neurologic dysfunction that prevents extension or control of the knee,” and a neuropathic joint.59,67
TKR generally involves removing the degenerated articular surfaces of the tibia, femur, and patella, and replacing these structures with metal, plastic, or a combination of each. The goals are to relieve pain, uniformly transmit forces across the joint, create a horizontal joint in the stance phase of gait, restore anatomic and mechanical axes, provide adequate stability, and improve function.34,36,67,92
Prosthetic implants vary in their design by being constrained, nonconstrained, mobile-bearing, or fixed-bearing. Constrained, or conforming implants, sacrifice the cruciate ligaments (ACL, PCL, or both) and rely on the conformity between the components for stability. Nonconstrained (cruciate-sparing) implants retain the cruciate ligaments.36,67,92 Fixed- bearing prostheses have a polyethylene (plastic) component fixated on the tibial tray. Mobile-bearing prostheses have a polyethylene platform which articulates between the metallic femoral prosthesis and tibial implant. The mobile polyethylene platform allows for better load-sharing throughout the polyethylene and theoretically reduces the wear of this implant.13 Studies show similar outcomes with regard to ROM and function with these four implants,11,46,82 however the prevalence of osteolysis was found to be slightly higher with the mobile-bearing implants.46
Prostheses can be secured with or without bone cement. The cementless prosthesis is porous-coated and allows the surrounding bone to grow into and adhere to the prosthesis, creating a direct biologic fixation.36 Cemented implants have been shown to have better survival at 15 years than cementless implants.5
Although the most common approach used to perform a TKR is through an anterior medial parapatellar incision, some surgeons are using a minimally invasive approach that spares cutting through the quadriceps. Several authors have shown improved function and a shorter inpatient stay2,27,54 as well as decreased use of narcotics for pain management with the minimally invasive approach.54
Rehabilitation after Total Knee Joint Replacement
Weight bearing may be restricted longer in the noncemented group to allow for firm bone growth to the component.36 Cemented components demonstrate a more secure fit earlier than the noncemented group, thus allowing earlier progression in weight bearing.
Immediate postoperative care uses a compression dressing with a knee immobilizer in full extension with the involved limb elevated 30° to 40° to minimize swelling and to prevent a knee flexion contracture. The maximum-protection phase of recovery focuses on reducing unwanted stresses that may loosen the prosthesis, while stimulating muscle strength, increasing ROM, and reducing pain and swelling. Remedial exercises that are initiated immediately after surgery include quadriceps, hamstring, and gluteal isometrics, ankle pumps, active assisted straight-leg raises, short-arc terminal knee extensions and knee flexion ROM exercises. Some authors report that CPM may be beneficial in regaining knee flexion34,36; however, other studies suggest standard physical therapy exercises without the use of CPM result in the same quality of function and ROM after TKR.8,23 The knee immobilizer can be removed to perform supine heel slides and supine hip and knee flexion exercises. Supine wall slides and active-assisted wall slides can be added as pain allows. As the midline surgical incision heals, the patella should be mobilized in a caudal-cephalic motion to reduce patellofemoral adhesions. The appropriate time to begin weight bearing depends on the fixation used, but generally the patient is instructed in a PWB gait with a walker or crutches within a day after surgery.34 An ambulatory assistive device is retained for support until a normalized gait is achieved.
With the primary goal after TKR being to restore ROM, the secondary goal is to restore strength. Quadriceps strength is highly correlated with functional performance, and therefore should be a focus throughout rehabilitation.69 Once the patient is able to start an outpatient rehabilitation program, continued efforts of progressing knee ROM and general lower extremity strengthening can be started, as summarized in Table 18-1.
Table 18-1
Outpatient Rehabilitation Program after Total Knee Arthroplasty
Quad sets, straight leg raises (with full knee extension), hip abduction (side lying), standing hamstring curls, seated knee extension, standing terminal knee extension from 45° to 0°, step-ups (5- to 15-cm block), wall slides to 45° knee flexion; 1-3 sets of 10 reps for all strengthening exercises
Criteria for progression: exercises are to be progressed (e.g., weights, step height) once the patient can complete the exercise correctly and feels maximally fatigued at the end of each set
Progression: 0.5- to 1.0-kg weights added to exercises, step-downs (5- to 15-cm block), front lunges, and wall slides toward 90° knee flexion
Ambulation training with assistive device as appropriate with emphasis on heel strike, push-off at toe-off, and normal knee joint excursions
Emphasis on heel strike, push-off at toe-off, and normal knee joint excursions when able to walk without assistive device
Stair ascending and descending step-over-step when patient has sufficient concentric and eccentric quadriceps strength
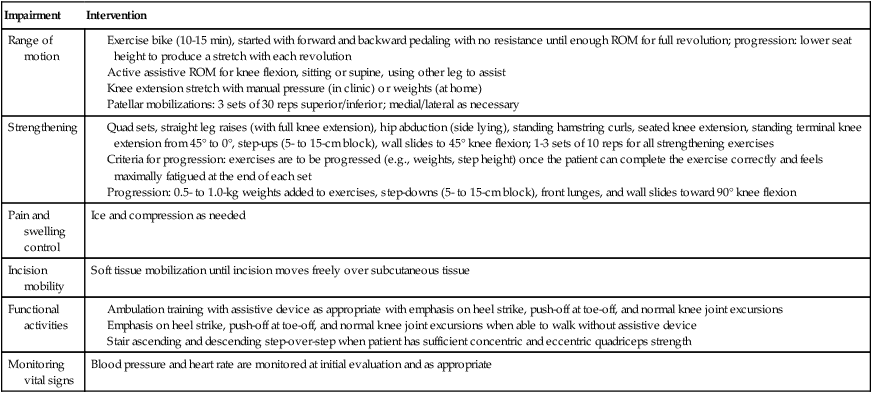
ROM, Range of motion; reps, repetitions.
From Mizner RL, Petterson SC, Snyder-Mackler S: Quadriceps strength and the time course of functional recovery after total knee arthroplasty, J Orthop Sports Phys Ther 35:424-436, 2005.
The PTA should expect the greatest amount of functional gain in the first 3 months of rehabilitation; however, improvements up to a year from surgery may be expected.53 After TKR it is generally understood that participating in high-impact activities, such as jogging, basketball, football, and soccer, is not recommended.43