19
Orthopedic Management of the Hip and Pelvis
1. Identify common hip fractures.
2. Outline and discuss common methods of management and rehabilitation of ordinary hip fractures.
3. Identify and describe common methods of management and rehabilitation after hip arthroplasty.
4. Identify and describe common soft-tissue injuries of the hip.
5. Outline and describe common methods of management and rehabilitation of soft-tissue injuries of the hip.
6. Identify common fractures of the pelvis and hip.
7. Discuss methods of management and rehabilitation for fractures of the pelvis and acetabulum.
HIP FRACTURES
The clinical significance of hip fractures is reflected in the annual rate of fractures and the financial burden to the economy that hip fractures produce.10,16 Goldstein10 states that more than 300,000 fractures occur annually with an associated cost of $10 billion. Other authorities4,16 report that 267,000 fractures occur annually, with a price tag of $33.8 billion.4 Although fractures in general occur to all age groups, hip fractures are most common among elderly women.4,16,17 Hip fractures in women can be attributed in part to the higher incidence of osteoporosis in this group17; with regard to age, hip fractures represent the most common acute orthopedic injury in the geriatric population.16
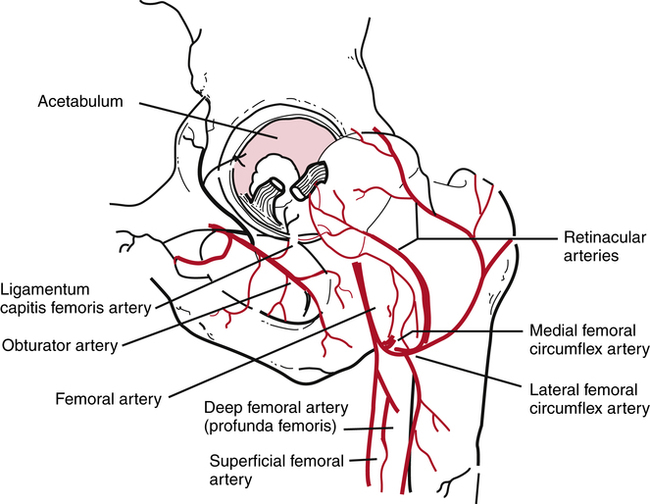
The classification of hip fractures is clinically significant for the PTA because the severity and location of the fracture profoundly affect surgical management and physical therapy interventions. The vascular supply to the femoral head and neck may be significantly compromised with certain fracture patterns and levels of severity (Fig. 19-1).17 LeVeau17 states, “The extent of the supply of blood to the head of the femur determines remodeling and healing after femoral neck fracture or hip dislocation.”
Generally, hip fractures can be classified by location and described by severity (simple or comminuted).9 Fractures of the hip can be located in the following areas:
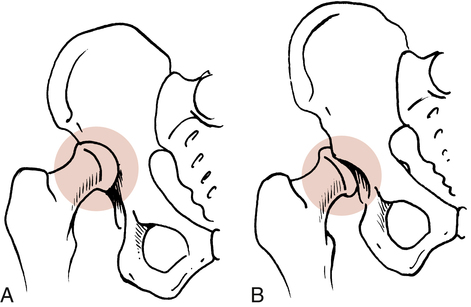
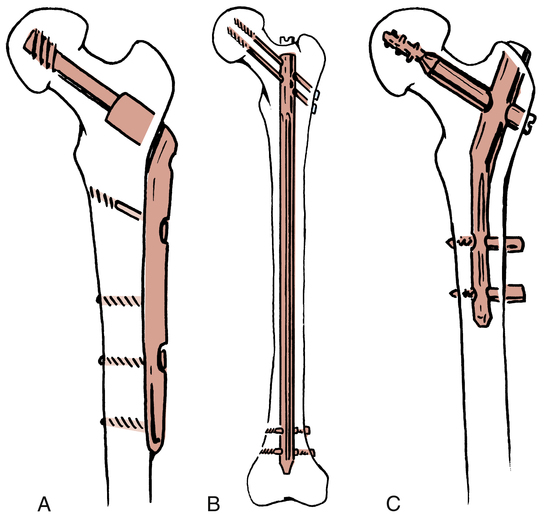
 Extracapsular or intertrochanteric9,10,21 (Fig. 19-2, A)
Extracapsular or intertrochanteric9,10,21 (Fig. 19-2, A)

 Femoral neck or subcapital areas11 (intracapsular) (Fig. 19-2, B)
Femoral neck or subcapital areas11 (intracapsular) (Fig. 19-2, B)
 Proximal femoral shaft or subtrochanteric areas (Fig. 19-2, C)11
Proximal femoral shaft or subtrochanteric areas (Fig. 19-2, C)11
Secondary to the location and severity of hip fracture, the most significant complication is related to osteonecrosis and the loss of blood supply to the femoral head leading to avascular necrosis (AVN). Gross and associates11 affirm, “any fracture of the neck (femoral) can disrupt this tenuous blood supply. As a result, there is an exceedingly high incidence of avascular necrosis of the femoral head after hip fractures.” LeVeau17 states, “avascular necrosis may occur after hip fracture in about 65% to 85% of the patients.”
Three main clinical complications are noted with subtrochanteric fractures: malunion, delayed union, and nonunion avascular necrosis.18 Two factors associated with malunion and nonunion of subtrochanteric hip fractures are:
 The subtrochanteric area of the proximal femur is cortical bone, which has a decreased blood supply.
The subtrochanteric area of the proximal femur is cortical bone, which has a decreased blood supply.
 The subtrochanteric area is prone to large biomechanical stresses that can lead to loosening of various fixation devices.18 This complication must be considered by the PTA when treating patients with this type of fracture.
The subtrochanteric area is prone to large biomechanical stresses that can lead to loosening of various fixation devices.18 This complication must be considered by the PTA when treating patients with this type of fracture.
Many options are available in treating hip fractures: The choice depends on the patient’s age, location of the fracture, quality of bone, severity of the fracture (simple, displaced, or comminuted), activity level of the patient, associated soft-tissue injuries, and specific goals for the patient’s return to activity. Generally, hip fractures are managed surgically with an open reduction with internal fixation (ORIF) procedure that secures the fracture fragments with various rods, nails, pins, screws, and plates.9,10,16 Some hip fractures can be managed conservatively with bed rest, traction, and protected weight bearing.18 For example, in a fractured greater trochanter where the displaced fracture fragment is less than 1 cm (as evaluated by the physician radiographically), the treatment could be bed rest for several days, range of motion (ROM) exercises, and limited weight bearing for 4 weeks.18
With an isolated lesser trochanteric fracture (most common in adolescents), the physician bases treatment on the amount of fragment displacement. If the fracture is displaced more than 2 cm, the physician could perform an ORIF procedure; if the fragments are in closer apposition, the physician may elect rest, protected weight bearing, and limited exercise for 3 to 4 weeks.18 Figure 19-3 depicts common fixation devices used to secure fracture fragments using an ORIF procedure.
While treating patients with hip fractures, the PTA must be aware that venous thrombosis is a potentially critical complication after hip surgery. Without prophylactic medications to minimize thrombosis, statistics show that 40% to 90% of patients develop this condition after hip surgery.18 Venous thrombosis is the most common complication after hip fracture in the elderly population of patients.18
Hip fractures and dislocations can occur in combination, as well as isolated events. Usually hip dislocations are either anterior or posterior (Fig. 19-4). Isolated hip dislocations generally are treated conservatively with bed rest, traction, and protected limited weight bearing for up to 12 weeks.18 For example, with an anterior hip dislocation, bed rest with traction is prescribed, with specific precautions to strictly avoid extreme hip abduction and external rotation to prevent redislocation. Usually protected weight bearing is allowed when the patient can achieve painless hip ROM around 3 to 4 weeks after the incident.18 Conversely an isolated posterior hip dislocation is treated with bed rest and traction in abduction with precautions to prevent hip abduction, flexion, and internal rotation to protect the joint from dislocation.18
Rehabilitation after Hip Fractures
The patient’s overall preoperative physical and mental condition is a predictor of postoperative success. Patients with major cardiovascular or pulmonary disease processes, obesity, osteoporosis, dementia or poor upper body strength are at increased risk for postoperative complications. Overall mortality rates of 20% after 1 year, 50% at 3 years, 60% at 6 years, and 77% after 10 years have been reported.7
Although the overall goal of rehabilitation is to restore patients to preinjury level, this may not be realistic. Only 20% to 35% of patients regain their preinjury level of independence. As many as 15% to 40% require institutionalized care for more than 1 year after surgery. Many (50% to 83%) require devices to assist with ambulation.14
The progression from maximum to minimum protection closely follows the rate of bone healing. However, other factors are considered in safely and effectively providing an environment for the return to functional activities. In the maximum-protection phase of recovery (phase 1 to 21 days postoperatively, as described by Goldstein9), the fracture site is protected; pain and swelling are reduced; and isometric exercises, gentle protected ROM, and limited weight bearing begin.9,17
The general goals of recovery are to increase muscular strength specific to the surgery, improve overall conditioning, increase ROM of the affected hip, enhance aerobic fitness, increase local muscular endurance, reduce pain and swelling, reestablish normalized gait mechanics, and protect the healing structures from internal and external forces that can impede healing.9,17
Goldstein9 identified a few major complications that occur, particularly during the maximum-protection phase of recovery. Generally, no combined diagonal or rotary forces are used in exercises during this phase. Hardware loosening and delayed healing may occur if increased torque is placed through the healing fracture site by excessive unwanted forces.9 No active straight-leg raises or supine hip bridges should be performed during the first 6 to 8 weeks after surgery. Goldstein states, “The power generated by the massive hip muscles is so great during those exercises that there is a danger of displacing the fractured segments.”9
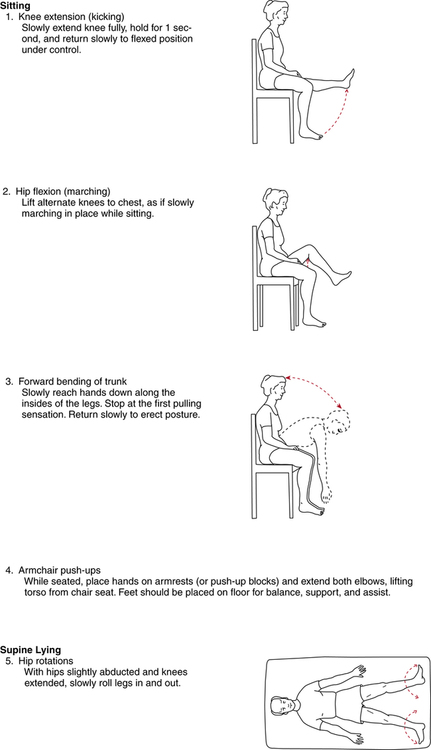
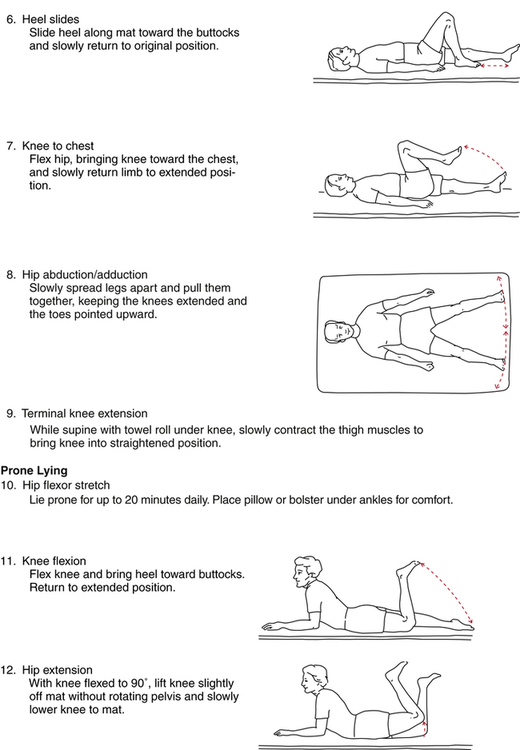
In addition to rudimentary isometric quadriceps sets, gluteal sets, ankle pumps, and gentle hip-motion exercises, authorities advocate adding the exercises described in Figure 19-5 progressively during the first 3 weeks after surgery,9 although exercises number 3 (forward bending of trunk) and 12 (hip extension in prone) are not advocated by the author of this chapter.
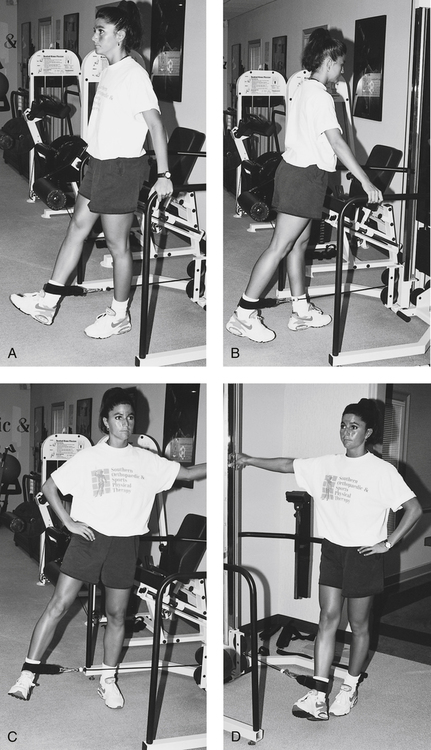
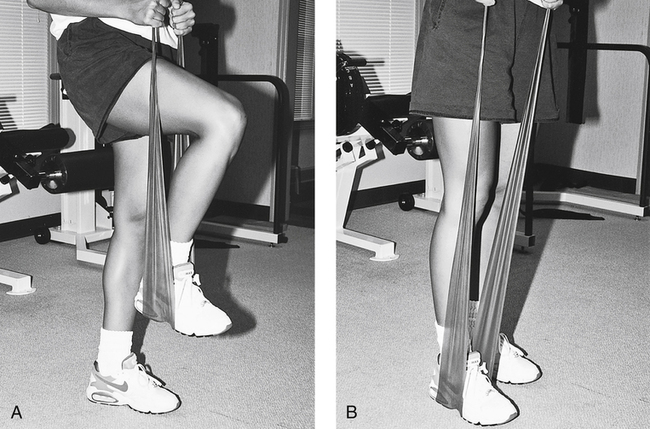
The moderate-protection phase, defined as 3 to 6 weeks after surgery,9 provides for more challenging exercises directed at regaining hip and knee motion, improving quadriceps and hamstring strength, and increasing strength to the hip extensors, abductors, and adductors. Standing four-position hip strengthening can be achieved initially without any resistance until a proper pattern of movement is achieved. Advancing this exercise can be accomplished using a cable system (Fig. 19-6), lower levels of Thera-Band, or ankle weights. The initiation of limited ROM leg presses can commence during this phase as well.
PROXIMAL FEMORAL OSTEOTOMY
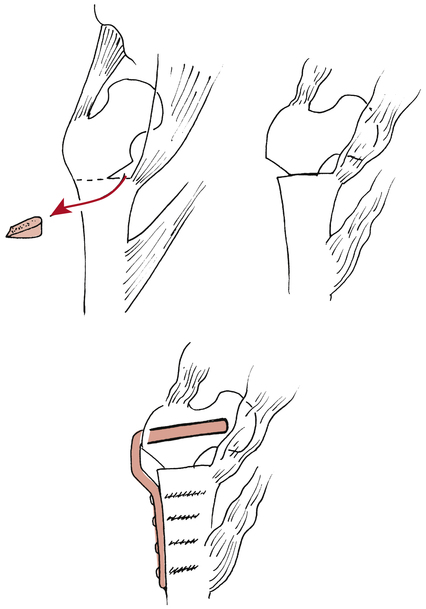
Intertrochanteric osteotomy may be performed when degenerative joint disease (DJD) is extensive and results in hip pain associated with subchondral bone erosion, articular cartilage fibrillation and fissuring, and hip joint incongruity.15 The goal of this surgical procedure is to reduce pain and improve function related to advanced osteoarthritis by surgically changing the femoral neck-shaft angle so that healthy cartilage is exposed, thus “improving joint surface congruity.”15 Figure 19-7 illustrates this procedure and shows the changed neck-shaft angle relationship, reduced ligamentous and muscular tension, and improved joint articulation occurring after surgery.15
Rehabilitation after Proximal Femoral Intertrochanteric Osteotomy
Weight-bearing status is highly individualized but generally is progressed according to the rate and quality of bone healing. Typically, a walker or crutches reduces compressive loads through the hip during TDWB, PWB, and non–weight bearing (NWB) gait techniques. In most cases, protected weight bearing is strictly enforced for 8 to 12 weeks after this procedure.15
HEMIARTHROPLASTY OF THE HIP
For femoral head osteonecrosis or severe femoral head fractures, hemiarthroplasty is used to eliminate pain and improve function. This procedure replaces the damaged femoral head with a bipolar prosthesis. Because hemiarthroplasty requires a normal acetabular surface,15,22 it is rarely used for arthritis.22 This is considered a conservative procedure15 when compared with a total hip replacement. Hemiarthroplasty can be converted at a later date to total hip replacement if symptoms persist and the joint degenerates.22 The term bipolar refers to two separate snap-fit components of one femoral prosthetic unit. A bipolar prosthesis is usually a large-diameter femoral head component that snap-fits snugly onto a smaller diameter femoral head, which is part of the total prosthetic unit.9,15 A unipolar femoral prosthesis is a self-contained femoral head and shaft without additional components. The bipolar prosthesis usually produces less wear caused by friction and reduced impact loading of the acetabulum.20
FIXATION OF PROSTHETIC HIP COMPONENTS
As discussed in Chapter 9, the method of fixation of various prosthetic components directly affects the short- and long-term course of rehabilitation after hip arthroplasty. Both femoral and acetabular components usually can be secured to the bone with a cement, polymethylmethacrylate (PMMA), which is not actually an adhesive, but rather provides a strong interference fit between the prosthesis and the bone.20 Or the components can be secured with a noncemented biologic tissue ingrowth prosthesis. Miller22 recommends that cemented femoral stems be used only for patients older than 65 years of age, and that noncemented prostheses be used for younger patients. Weight-bearing precautions are related to the specific type of fixation procedure used to secure the prosthesis. Weight bearing generally is deferred for longer periods of time with a noncemented biologic tissue fit prosthesis so that the bone can grow into the porous coated femoral stem. Weight bearing with cemented devices can progress at a slightly faster rate. However, in either case, rotational forces (torque) must be strictly avoided to minimize the loosening of components.
TOTAL HIP REPLACEMENT
 Osteoarthritis (both femoral head and acetabulum)
Osteoarthritis (both femoral head and acetabulum)
 Juvenile rheumatoid arthritis (the most common indication for THR in adolescents)20
Juvenile rheumatoid arthritis (the most common indication for THR in adolescents)20
 Significant alterations in activities of daily living (ADLs)22
Significant alterations in activities of daily living (ADLs)22
Surgeons must select a proper femoral head size for each patient. In theory, a large-diameter femoral head may provide for greater ROM and inherent stability.20,22 This makes sense because greater forces are necessary to dislocate a large-diameter head from the acetabulum. In practice, large-diameter femoral head components do not reduce the incidence of dislocation after surgery. Therefore the most commonly used head size is moderate (26 to 28 mm) rather than overly large (32 mm).20,22
One of the most common complications related to THR, using a noncemented femoral stem component, is persistent thigh pain with an antalgic gait (painful limp-gait) pattern. This thigh pain may last for 1 or 2 years after surgery and is reported in approximately 20% of all patients with this fixation type.20,22
The most significant complication after THR, with the highest mortality, is thromboembolic disease.20 The entire rehabilitation team (PT, PTA, physician, etc.) must be concerned with this complication and monitor for this continually. While many of the signs of thromboembolitic disease after THR are the same as with any other lower extremity injury or surgery, some specific signs post THR would be localized tenderness and swelling along the distribution of the deep venous system of the hip, specifically the femoral vein along the anterior thigh.
Because the method of fixation is directly related to the initiation and progression of weight bearing after surgery with uncemented components, some authorities recommend TDWB on the second day postoperatively, gradually progressing to FWB by 8 weeks postoperatively.9 With a cemented (PMMA) prosthesis, Goldstein9 suggests TDWB 2 days after surgery, progressing to FWB by the third week postoperatively. These timetables for weight bearing are directed by the biologic rate of bone healing and the wishes of the physician and are applied under the direction of the PT. A cemented component generally allows earlier motion and weight bearing than an uncemented prosthesis.
Loosening of the components has been estimated at 10% to 40% by 10 years postoperatively.22 Loosening is more common among younger, more active patients, obese patients, patients with rheumatoid arthritis, and patients with previous hip surgery.22 The PTA must be acutely aware of these factors when treating THR patients and recognize the increased potential for component loosening.
Postoperative dislocation of the hip after THR is another clinically significant complication occurring at rates between 1% and 4%.22 These dislocations are multifactorial, requiring an awareness of the basic concepts of hardware design, fixation procedures, and surgical approaches and patient compliance with specific total hip precautions to avoid dislocation. The most immediate concern during the recovery from THR is teaching and reinforcing precautions to the patient, nursing staff, family, and other caregivers.
 Avoid hip adduction. This is usually accomplished by using an abduction wedge or pillow.
Avoid hip adduction. This is usually accomplished by using an abduction wedge or pillow.
 Avoid hip internal rotation. The affected limb can be supported medially with pillows or a wedge to maintain the limb in neutral or slight external rotation.
Avoid hip internal rotation. The affected limb can be supported medially with pillows or a wedge to maintain the limb in neutral or slight external rotation.
 Avoid hip flexion greater than 90°.
Avoid hip flexion greater than 90°.
 Avoid the combination (simultaneous performance) of hip flexion, internal rotation, and adduction for up to 4 months after surgery.9
Avoid the combination (simultaneous performance) of hip flexion, internal rotation, and adduction for up to 4 months after surgery.9
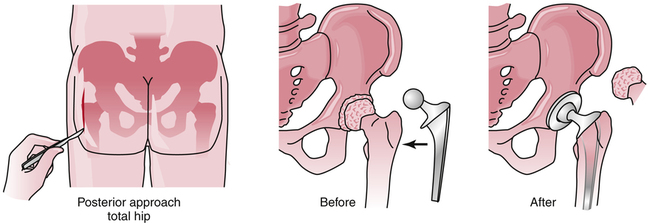
The preceding precautions apply when a posterior (Fig. 19-8), posterolateral, or lateral approach is used. If an anterior surgical approach is used, combined hip extension and external rotation should be avoided.9 Again, this variation is needed because the surgeon had to extend and externally rotate the limb to dislocate the hip and gain exposure for replacement.
Rehabilitation after Total Hip Replacement
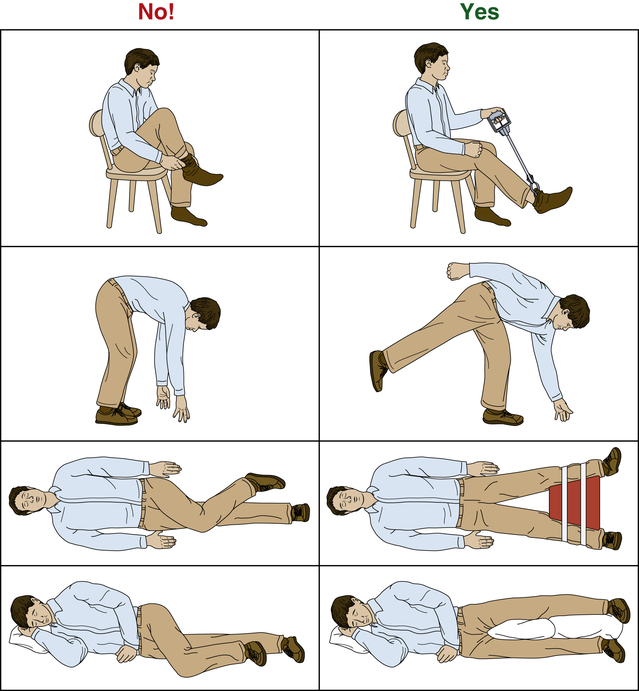
In the maximum-protection phase of recovery, the patient is instructed in bilateral ankle pumps, isometric quadriceps sets, gluteal isometrics, and active knee flexion (being careful to avoid excessive hip flexion) exercises. The contralateral limb can be exercised with active straight-leg raises, quadriceps sets, hamstring sets, ankle pumps, and full knee and hip mobility exercises. To ensure primary healing, all universal hip precautions must be enforced. (Avoid hip flexion, adduction, and internal rotation with a posterior, posterolateral or lateral surgical approach, and avoid hip extension and external rotation with an anterior approach.) In addition, the patient should be strongly cautioned to avoid the following positions and actions (Fig. 19-9), as outlined by LeVeau17:
Transfer training and bed mobility must be addressed immediately after surgery. The affected limb should be maintained in a stable, secure position during all transfers from bed to commode or wheelchair. A raised toilet seat is a basic requirement during the early phase of recovery. In addition, a raised and rigid (although padded) seat cushion is necessary to eliminate the sling effect of the wheelchair seat, which places the hip in an internally rotated position.9
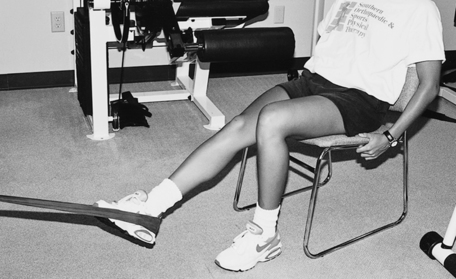
The moderate-protection phase can begin when the patient has demonstrated improved quadriceps control, active knee flexion, reduced pain, compliance with all precautions and exercises, independent bed mobility and transfers, and improved gait (with necessary weight-bearing precautions). Moderate protection does not imply reduced THR precautions in any way. During this phase, more challenging exercises are added to more closely approximate functional activities. Light resistance exercises for quadriceps strengthening in a semirecumbent position and elastic tubing (Thera-Band) also can be used to strengthen the hamstrings and hip extensors in a semirecumbent or seat-elevated position (Fig. 19-10). Standing exercises stress active hip motion (straight-plane motions, no combined rotational forces, THR precautions strictly enforced) and strengthening.
To enhance aerobic fitness, a recumbent bucket-seat bicycle ergometer or a UBE can be used. Increases in weight bearing are added as determined by component fixation, tissue healing constraints, and the wishes of the physician. Closed-chain functional activities begin between 3 and 8 weeks postoperatively10 for cemented prostheses, with increased weight bearing orders by the physician. These activities can include sit-to-stand exercises with an elevated seat, partial supported knee bends (for concentric and eccentric quadriceps control), weight-shifting exercises, treadmill walking, mini step-ups, and standing resisted hip and knee extension (Fig. 19-11). For an uncemented prosthesis, closed-chain functional activities are deferred for 2 or 3 weeks longer than for cemented prostheses. However, standing straight-plane resistance exercises (hip extension, adduction, abduction, and flexion) are allowed between 3 and 8 weeks postoperatively.
The minimum-protection phase is classically characterized by a return to normalized gait patterns without assistive devices, and by instruction in balance, coordination, proprioception, and advanced closed-chain functional activities that duplicate the patient’s specific ADLs. Most patients recover most of their hip motion during the first year after surgery.20 Therefore at this phase of recovery (approximately 4 months after surgery) the patient may still demonstrate decreased motion, but must be reassured that more time is needed before assessing the ultimate degree of hip motion attainable.
Returning to higher level activities, including sport activity, should be a team approach discussion with the physician, PT, PTA and patient. Multiple factors should be considered, not the least of which would be presurgical activity level, experience in the activity/sport the patient wants to return to, strength, balance, proprioception, mobility status, and so on. A list of recommendations of activities and their level of recommendation is given in Box 19-1.
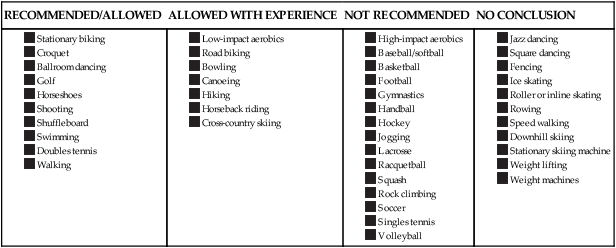
From Healy WL, Iorio R, Lemos M: Athletic activity after total joint replacement, Am J Sports Med 29:377–388, 2001.
HIP OSTEOARTHRITIS
Hip osteoarthritis (OA) is defined as the focal loss of articular cartilage with variable subchondral bone reaction. The prevalence of OA ranges from 7% to 25% in adults aged 55 years and older in the white European population.24 Although specific characteristics of hip OA have not always correlated with radiographic features, joint pain and functional impairment seem consistent.
Conservative interventions that have demonstrated success in those patients with hip OA include gait and balance training, manual therapy techniques, and systematically progressed therapeutic strengthening.2
Regarding the use of manual therapy techniques, it was recommended that clinicians should consider the use of manual therapy procedures to provide short-term pain relief and improve hip mobility and function in patients with mild hip OA. Distractive techniques are particularly helpful to the patient with hip OA. Manual therapy techniques were also found to be superior in terms of relief of pain and improvement in function as compared with therapeutic exercise in all patients with hip OA, except those with highly limited function, high pain levels, and limited ROM.13
LEGG-CALVÉ-PERTHES DISEASE
In 1910, three researchers identified a hip condition that usually affects children between the ages of 4 and 8 years (the range is 2 to 12 years of age with the most common age being 6 years).3 This condition, which is referred to as Legg-Calvé-Perthes (LCP) disease or coxa plana, is characterized as a noninflammatory, self-limiting (can heal spontaneously with or without specific treatment) syndrome in which the femoral head becomes flattened at the weight-bearing surface11 as a result of disruption of the blood supply (AVN) to the femoral head in the growing child.11,17 The long-term complications of the flattened femoral head lead to an incongruous joint surface and advanced DJD (Fig. 19-12).11,17,19

Throughout the management of this disease, the primary focus is on maintaining the femoral head within the confines of the acetabulum, regaining motion, and reducing pain and dysfunction.11,17,19 In the acute or maximum-protection phase, reducing pain and dysfunction is generally accomplished using physician-prescribed nonsteroidal antiinflammatory drugs (NSAIDs), bed rest, and traction to take the load off the hip and restore motion in abduction.
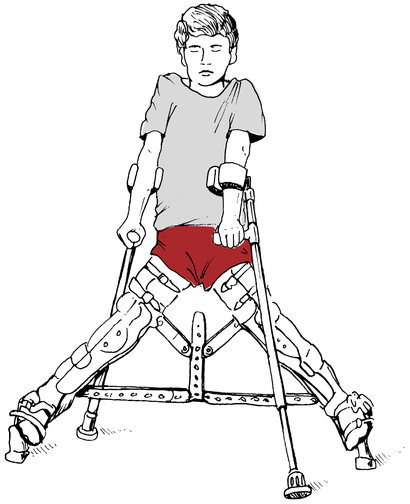
Keeping the femoral head seated within the acetabulum can be accomplished using an abduction orthosis (Fig. 19-13).11,17 To aid healing and reduce unwanted stress on the affected hip, the abduction orthosis can be worn as long as 2 years.17 During this time, the brace can be removed for short periods each day to exercise the limb and attend to personal hygiene.17 With the brace removed, the patient must maintain hip abduction during ROM exercises for the knee (flexion and extension), internal rotation of the hip, quadriceps strengthening, hip abduction, and hip extension strengthening exercises (gluteus medius and gluteus maximus).17
OSTEITIS PUBIS
Examination findings include tenderness over the symphysis and proximal adductors, pain with adduction against resistance, and restricted hip rotation with pelvic obliquity and sacroiliac dysfunction.8 A bone scan of the area may assist in differential diagnosis of this dysfunction versus pubalgia and athletic pubalgia (sports hernia).
SOFT-TISSUE INJURIES OF THE HIP
Bursitis
Trochanteric bursitis is a common soft-tissue injury affecting the hip in an active population of patients. The greater trochanter of the femur is most commonly affected. The trochanteric bursa may become irritated and inflamed because of excessive compression and repeated friction as the iliotibial band (ITB) snaps over the bursa while lying superior to the greater trochanter (Fig. 19-14).

Two other areas of bursitis commonly affecting the hip are ischial bursitis and iliopectineal bursitis. Ischial bursitis (Fig. 19-15) has also been termed Weaver’s bottom and is characterized by pain over the ischial tuberosity underlying the gluteus maximus. It can be caused by direct contusion of the ischial tuberosity or extended periods of sitting.11,23 Occasionally this condition can mimic a hamstring strain at the origin of the muscle at the ischial tuberosity.11,23 This condition tends to affect thinner people and cyclists. Management is similar to other forms of bursitis: rest from the aggravating activity, ice packs, NSAIDs, and a judiciously applied program of stretching exercises that do not aggravate the symptoms. Generally, hamstring stretches are encouraged along with quadriceps-strengthening exercises. Somewhat unique to this particular bursitis is the use of a padded seat cushion as an intervention method because of the bursa location. Occasionally, conservative care fails and the physician may elect to inject the area with corticosteroids.11

Iliopectineal bursitis is characterized by either local tenderness over the iliopsoas muscle and tendon or diffuse radiating pain into the anterior thigh (Fig. 19-16).23 Because the iliopectineal bursa lies deep to the tendon of the iliopsoas muscle, tightness of the iliopsoas alone and in conjunction with excessive hip extension can cause compression and frictional wear of the iliopectineal bursa. Pain may also be noted with passive hip flexion and adduction at the end range. Specific care centers on reducing pain and irritation using a program of rest, ice, antiinflammatory medications, and physical therapy interventions such as thermal agents, stretching, and strengthening exercises.

Muscle Strains
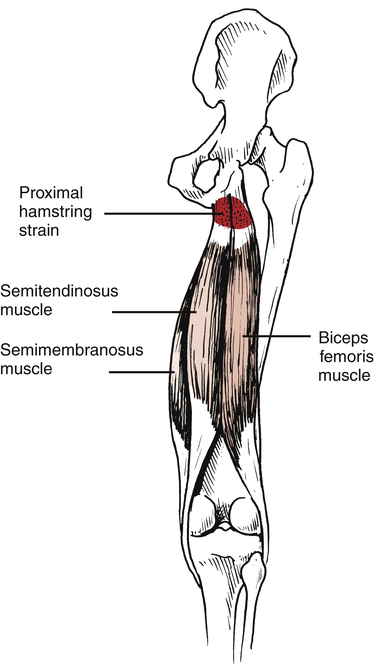
Most acute injuries affecting the hip are musculotendinous strains of the hamstrings, iliopsoas, adductors, and rectus femoris.11,23 Injuries to the hamstrings at the origin (ischial tuberosity) can be caused by sudden, forceful contraction of the hamstrings or by decelerating the lower leg against the concentric contraction of the quadriceps during running as the hamstrings contract eccentrically (Fig. 19-17).
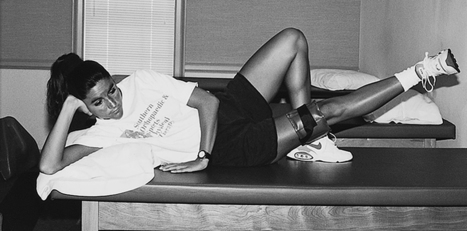
Initial injury management involves the application of cold packs for 20 minutes, three to five times daily. Wrapping the affected limb with a compression bandage also can help relieve stress on the limb. Motions that produce pain and interfere with the healing process should be avoided. Two motions should not be attempted during the acute or maximum-protection phase of recovery: full knee extension combined with forward trunk flexion and full leg flexion.3,4
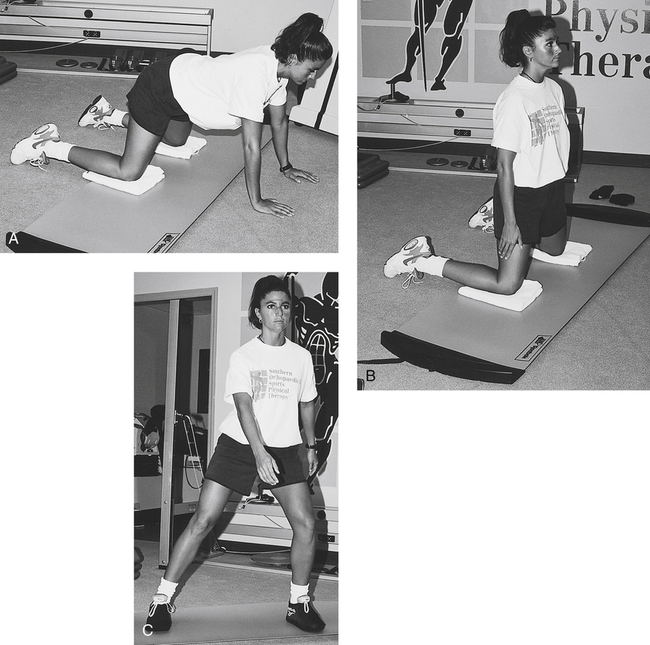
An adductor muscle strain is termed a groin pull. A classic program of protection, ice, compression bandaging, crutches, and protected weight bearing during the acute or maximum-protection phase should be followed. As with other muscle and tendon strains, early aggressive stretching should be avoided. Once pain subsides, active hip flexion, gentle hip abduction and adduction motion, and knee ROM exercises should begin. Specific hip abduction stretching can be initiated, instructing the patient to perform the seated butterfly stretch, with a strong caution to proceed slowly without pain. Some authorities suggest waiting 3 to 6 weeks before instructing the patient in progressive resistance exercises.11 However, resistance exercises can begin earlier, depending on the severity of the strain. To specifically strengthen the hip adductors, submaximal isometrics (Fig. 19-18) can give way to proximally placed resistance in various positions (Fig. 19-19).
Progression to more dynamic strengthening exercises depends on the specific goals established by the patient and PT. For example, in a young athletic population of patients eager to return to sports activities, a slide board can be an effective tool to introduce dynamic hip adduction and abduction motions (Fig. 19-20).
An iliopsoas muscle strain also is referred to as a hip flexor pull. This injury can occur from sudden, forceful extreme hip extension or by forced hip flexion against resistance.23 A standard program of protection, rest, ice, and compression bandages with crutches and limited weight bearing is encouraged in the acute phase. Sleeping comfort can be enhanced by sleeping supine with pillows under the knees to reduce hip extension. Gentle, active hip flexion and extension exercises are begun once the initial healing phase has ended and the patient no longer complains of pain. A prolonged period of time may be needed to avoid hip extension (e.g., push-off during gait running or hip extension past neutral) and encourage healing. Gentle active stretching of the hip flexors can begin with the patient supine and the nonaffected knee and hip flexed. In addition, a hurdler’s stretch can be initiated once the patient demonstrates improved hip extension motion without pain. The PTA should strongly encourage the patient to perform these stretches in a slow, static fashion without pain. Very close supervision is needed to guard against any ballistic, forceful, or violent motions that could impede healing and reinjure the affected limb.
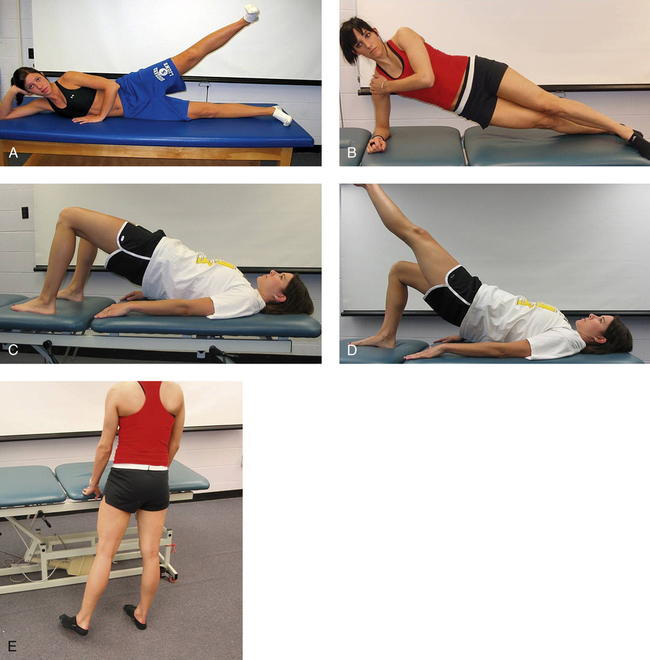
 Side-lying hip abduction (gluteus medius: 42% ± 23%)1: patient lies on contralateral side with shoulder, hip and ipsilateral heel in contact with wall. Patient lifts ipsilateral lower extremity 6 to 12 inches in frontal plane, while keeping contact with wall throughout the motion (Fig. 19-21, A). As the patient increases strength and requires less stabilization, he or she can move away from wall to perform this exercise as the PTA monitors compensation of abducting anterior to frontal plane.
Side-lying hip abduction (gluteus medius: 42% ± 23%)1: patient lies on contralateral side with shoulder, hip and ipsilateral heel in contact with wall. Patient lifts ipsilateral lower extremity 6 to 12 inches in frontal plane, while keeping contact with wall throughout the motion (Fig. 19-21, A). As the patient increases strength and requires less stabilization, he or she can move away from wall to perform this exercise as the PTA monitors compensation of abducting anterior to frontal plane.
 Side bridge (gluteus medius: 74% ± 30%)5: patient lies on ipsilateral side with ipsilateral forearm directly below shoulder and lifts bilateral hips off table as demonstrated (Fig. 19-21, B).
Side bridge (gluteus medius: 74% ± 30%)5: patient lies on ipsilateral side with ipsilateral forearm directly below shoulder and lifts bilateral hips off table as demonstrated (Fig. 19-21, B).
 Bilateral lower extremity bridge (gluteus medius: 28% ± 17%; gluteus maximus: 27% ± 13%; hamstrings: 35% ± 21%)5,6: patient lies supine with bilateral feet flat on table. Patient lifts bilateral hips off table to neutral spine position (Fig. 19-21, C).
Bilateral lower extremity bridge (gluteus medius: 28% ± 17%; gluteus maximus: 27% ± 13%; hamstrings: 35% ± 21%)5,6: patient lies supine with bilateral feet flat on table. Patient lifts bilateral hips off table to neutral spine position (Fig. 19-21, C).
 Single lower extremity bridge (gluteus medius: 47% ± 24%)5: patient starting position as with bilateral bridge exercise. Patient lifts contralateral lower extremity with knee extended as patient lifts bilateral hips with ipsilateral lower extremity to neutral spine position (Fig. 19-21, D).
Single lower extremity bridge (gluteus medius: 47% ± 24%)5: patient starting position as with bilateral bridge exercise. Patient lifts contralateral lower extremity with knee extended as patient lifts bilateral hips with ipsilateral lower extremity to neutral spine position (Fig. 19-21, D).
 Standing hip abduction without weight (gluteus medius: 33 ± 23%)1: patient stands on contralateral lower extremity and abducts ipsilateral lower extremity 6 to 12 inches (Fig. 19-21, E).
Standing hip abduction without weight (gluteus medius: 33 ± 23%)1: patient stands on contralateral lower extremity and abducts ipsilateral lower extremity 6 to 12 inches (Fig. 19-21, E).
Muscle Contusions
The most common contusion affecting the hip and pelvis involves the subcutaneous tissues of the iliac crest and is commonly termed a hip pointer.12 Typically this injury can occur in one of two ways:
1. The iliac crest is contused by direct contact from an external force or falling on the exposed iliac crest.
2. There is a sudden forceful contraction or overstretching of the muscles attached to the iliac crest.12 This seemingly minor injury can be severe, causing extreme pain and dysfunction.
FRACTURES OF THE PELVIS AND ACETABULUM
General principles dealing with pelvic fractures and their classification with acetabular fractures dramatically show the PTA the extensive and potentially life-threatening nature of these injuries.11,21,22 This discussion outlines the profound complications that may occur with pelvic fractures, giving the PTA a better understanding of the long-term rehabilitation needed in many cases of severe fractures.
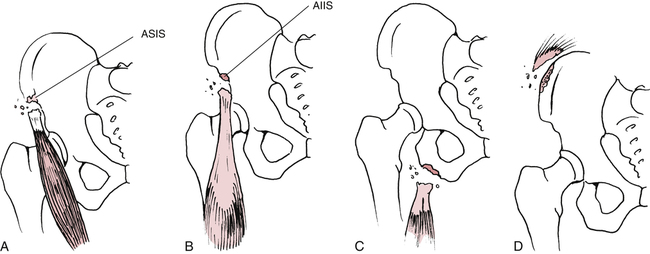
The most basic classification of pelvic fractures refers to the injury as either stable or unstable.11,21,22 Stable fractures include avulsion-type fractures of the anterior superior iliac spine, anterior inferior iliac spine, ischial tuberosity, and iliac crest (Fig. 19-22).11,21 Avulsion fractures of the pelvis can be treated conservatively with rest, protected weight bearing, crutches, and avoidance of premature stretching and resistive exercises, which may delay bony union (usually within 6 weeks).11
McRae21 advocates an ORIF procedure with avulsion fractures of the ischial tuberosity and fragment separation greater than 2 cm by saying, “Non-union is an appreciable risk, and if this occurs there may be problems with chronic pain and disability.” Usually avulsion fractures of the ischial tuberosity can be treated with rest, keeping the hip extended and externally rotated to avoid continued stress on the healing bone, and enforcing protected weight bearing for approximately 6 weeks.21 Once secure bone healing has been established, the PT may direct the assistant to carry out a gentle, progressive flexibility program to regain hip flexion. Strengthening exercises are added when the physician confirms radiographic evidence of secure union of the avulsion.
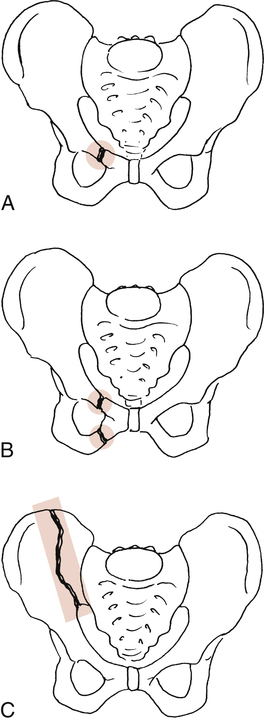
Other stable pelvic fractures include fractures of the superior pubic ramus, superior and inferior pubic rami on one side, and ilium (Fig. 19-23).21 In general, stable fractures of the pelvis are treated nonsurgically with protection, bed rest (2 to 3 weeks),21 and progressive motion and exercise once stable bone union has been confirmed.
Unstable pelvic fractures usually can be defined as either rotationally unstable but vertically stable, or rotationally and vertically unstable.21 These severe injuries can be treated with an external fixator, ORIF procedure, or extended convalescence involving bed rest.11,21,22 The PTA must be aware of complications after unstable pelvic fractures that can influence the time to begin rehabilitation procedures and can require protracted periods of recovery before physical therapy interventions. Box 19-2 outlines complications associated with these potentially life-threatening injuries.
The rehabilitation program employed after pelvic fractures is individualized and specific to the type and severity of fracture and the methods used to stabilize the fracture (ORIF, external fixator, and long-term convalescence). Because of the fragile hemodynamic nature of significant pelvic fractures, weight bearing of any kind is deferred for 8 weeks or longer.21
The classification system used to identify specific patterns of acetabular fractures is defined by Loth18 as the Letournel classification model (Fig. 19-24). Generally, these fractures are treated according to the severity of the fracture, usually with an ORIF procedure or, conservatively, with bed rest and traction to reduce compression of the joint.21 Conservative management of acetabular fractures is reserved for severely fragmented acetabular floor fractures in which surgery cannot realign the fragments to anatomically reconstruct the articular surface.21 An ORIF procedure is used to stabilize the fracture in all other cases.18
COMMON MOBILIZATION TECHNIQUES FOR THE HIP
Reduced motion secondary to pain and fibrosis after fractures, soft-tissue injuries, and various hip arthroplasty techniques may warrant mobilization in conjunction with thermal agents, strengthening, stretching, and functional activities. The techniques presented here are identified by the PT as appropriate techniques to use based on pathology, the presence of pain, or defined limitations of movement. As with all mobilization techniques, the PT selects which techniques to use and the direction of force, amplitude, grades, velocity, and distractions (see Chapter 15).
Other general rules of mobilization for the hip joint that should be implemented include:
 Warming of the tissues and body through exercise is advisable.
Warming of the tissues and body through exercise is advisable.
 Both the patient and the PTA must be in the correct position, relaxed and at ease.
Both the patient and the PTA must be in the correct position, relaxed and at ease.
 All techniques must be modified to suit both the PTA and the patient.
All techniques must be modified to suit both the PTA and the patient.
 Whenever possible, have the patient’s body weight serve as a means of stabilization to prevent unwanted movement.
Whenever possible, have the patient’s body weight serve as a means of stabilization to prevent unwanted movement.
 Hand placement for mobilization should be as close to the joint as possible, with firm but comfortable grasp.
Hand placement for mobilization should be as close to the joint as possible, with firm but comfortable grasp.
 Visualizing the joint surface, its direction, and contour will assist the PTA in correctly performing the technique.
Visualizing the joint surface, its direction, and contour will assist the PTA in correctly performing the technique.
 Whenever possible on hip joint mobilizations, the forearms should be positioned in line with the direction of the mobilization force to be applied.
Whenever possible on hip joint mobilizations, the forearms should be positioned in line with the direction of the mobilization force to be applied.
 The PTA must use the minimum of force consistent with achieving the objective.
The PTA must use the minimum of force consistent with achieving the objective.
Distraction
 Patient position: Supine with the leg positioned over the clinician’s shoulder, hip in resting position.
Patient position: Supine with the leg positioned over the clinician’s shoulder, hip in resting position.
 PTA position: Standing to side of the leg to be mobilized facing the patient’s hip.
PTA position: Standing to side of the leg to be mobilized facing the patient’s hip.
 Stabilization: The rest of the body on the table serves as stabilizing force. A belt may be wrapped around the patient’s pelvis and the treatment table to help stabilize the pelvis.
Stabilization: The rest of the body on the table serves as stabilizing force. A belt may be wrapped around the patient’s pelvis and the treatment table to help stabilize the pelvis.
 Mobilization: Position both hands on anterior and medial surfaces of the proximal thigh. Both hands move the femoral head away from the acetabulum at a 90° angle.
Mobilization: Position both hands on anterior and medial surfaces of the proximal thigh. Both hands move the femoral head away from the acetabulum at a 90° angle.
 Direction of force: Impart a caudal/inferior and lateral force to the hip joint by leaning back away from the patient (Fig. 19-25).
Direction of force: Impart a caudal/inferior and lateral force to the hip joint by leaning back away from the patient (Fig. 19-25).

Inferior Glide (Long Axis Distraction)
 Patient position: Supine on table, lumbar spine side-bent away from side to be mobilized.
Patient position: Supine on table, lumbar spine side-bent away from side to be mobilized.
 PTA position: Standing at the patient’s foot facing the patient’s hip.
PTA position: Standing at the patient’s foot facing the patient’s hip.
 Stabilization: The rest of the body on the table serves as stabilizing force, especially with the lumbar spine side-bent away. A belt may be wrapped around the patient’s pelvis and the treatment table to help stabilize the pelvis.
Stabilization: The rest of the body on the table serves as stabilizing force, especially with the lumbar spine side-bent away. A belt may be wrapped around the patient’s pelvis and the treatment table to help stabilize the pelvis.
 Mobilization: Grab patient’s leg proximal to the knee (supracondylar ridges of femur) with both hands. Distraction force in caudal direction imposed via both hands. PTA can lean back and use entire body for more aggressive mobilization if prescribed by PT.
Mobilization: Grab patient’s leg proximal to the knee (supracondylar ridges of femur) with both hands. Distraction force in caudal direction imposed via both hands. PTA can lean back and use entire body for more aggressive mobilization if prescribed by PT.
 Direction of force: Directly inferior and along longitudinal axis from hip joint imparted via PTA body leaning back.
Direction of force: Directly inferior and along longitudinal axis from hip joint imparted via PTA body leaning back.
Posterior Glide
 Patient position: Supine with arms relaxed. Patient’s dysfunctional side is flexed so that the foot is placed on the table just lateral to the noninvolved knee.
Patient position: Supine with arms relaxed. Patient’s dysfunctional side is flexed so that the foot is placed on the table just lateral to the noninvolved knee.
 PTA position: Standing on side opposite of dysfunction, directly facing the patient.
PTA position: Standing on side opposite of dysfunction, directly facing the patient.
 Stabilization: Patient resting on table serves as stabilization. The dysfunctional lower extremity is placed in a position of flexion, adduction, and internal rotation such that the foot is placed on the table as stated above.
Stabilization: Patient resting on table serves as stabilization. The dysfunctional lower extremity is placed in a position of flexion, adduction, and internal rotation such that the foot is placed on the table as stated above.
 Mobilization: PTA places bilateral hands on top of the knee on the dysfunctional side.
Mobilization: PTA places bilateral hands on top of the knee on the dysfunctional side.
 Direction of force: Mobilization is imparted to the posterolateral hip and capsule through the long axis of the femur. Mobilization force is via PTA’s body through his or her hands (Fig. 19-27).
Direction of force: Mobilization is imparted to the posterolateral hip and capsule through the long axis of the femur. Mobilization force is via PTA’s body through his or her hands (Fig. 19-27).

Anterior Glide in Flexion, Abduction, and External Rotation
 Patient position: Prone on table with dysfunctional hip in a position of flexion, abduction, and external rotation.
Patient position: Prone on table with dysfunctional hip in a position of flexion, abduction, and external rotation.
 PTA position: Standing on side of dysfunction. Contact the proximal femur just distal the greater trochanter.
PTA position: Standing on side of dysfunction. Contact the proximal femur just distal the greater trochanter.
 Stabilization: Patient’s body resting on table serves as stabilizing force. A belt may be wrapped around the patient’s pelvis and the treatment table to help stabilize the pelvis.
Stabilization: Patient’s body resting on table serves as stabilizing force. A belt may be wrapped around the patient’s pelvis and the treatment table to help stabilize the pelvis.
 Mobilization: Mobilizing force is imparted to the hip through the proximal femur using passive accessory glides from posterior to anterior.
Mobilization: Mobilizing force is imparted to the hip through the proximal femur using passive accessory glides from posterior to anterior.
 Direction of force: Passive accessory glides imparted from posterior to anterior (Fig. 19-28). Direction may also be imparted anterior-medial dependent on direction of restriction. Consider joint surface with mobilization.
Direction of force: Passive accessory glides imparted from posterior to anterior (Fig. 19-28). Direction may also be imparted anterior-medial dependent on direction of restriction. Consider joint surface with mobilization.
GLOSSARY
Comminuted fracture Any fracture with more than two fracture fragments.
Displaced fracture Any fracture in which there is loss of contact between surfaces.
Hip osteoarthritis The focal loss of articular cartilage with variable subchondral bone reaction.
Osteitis pubis A disorder characterized by pain and bony erosion of the symphysis pubis.
Osteonecrosis Subchondral bone necrosis secondary to vascular insufficiency.
Simple fracture A fracture in which the skin and soft tissues overlying skin are intact.