22
Orthopedic Management of the Elbow
1. Identify and describe the principles for common overuse and soft-tissue injuries of the elbow.
2. Discuss common methods of management and rehabilitation of overuse, soft-tissue injuries of the elbow.
3. Identify and describe intercondylar fractures, radial head fractures, olecranon fractures, and fracture-dislocations of the elbow.
4. Describe methods of management and rehabilitation of various fractures and fracture-dislocations of the elbow.
5. Describe techniques to improve range of motion of a stiff elbow including common joint mobilization techniques.
SOFT-TISSUE INJURIES OF THE ELBOW
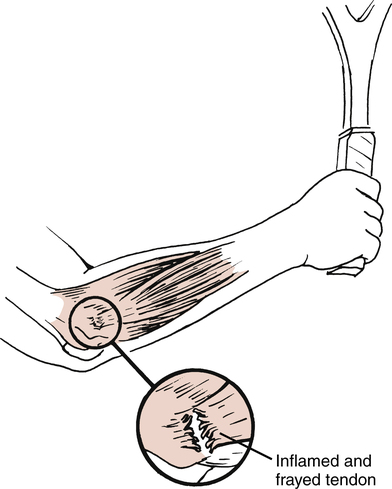
Lateral Epicondylitis
Commonly referred to as tennis elbow, lateral epicondylitis affects the common wrist extensor origin of the extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, and extensor digiti minimi.8,29 The repetitive overuse of this area leads to tendinitis of the origin of the extensor carpi radialis brevis tendon (Fig. 22-1).9,29
Interestingly, lateral epicondylitis can affect anyone involved with repetitive activities of the wrist extensors.28 Thus persons involved with the use of hand tools (e.g., hammer, screwdriver, or pliers) and various activities involving wrist rotation, pulling, extending, and hand grasping can be affected by lateral epicondylitis.28
Generally the patient suffering from lateral epicondylitis has pain with palpation of the lateral epicondyle, with active or resisted wrist extension, and occasionally with grasping of the affected hand.8,23,28 Because this is a chronic overuse tendinitis, the intense inflammatory response in the affected area of the lateral epicondyle is “an attempt to increase the rate of tissue production to compensate for the increased rate of tissue microdamage.”28
Management of Lateral Epicondylitis
Initial acute management focuses on resolving pain and swelling with the judicious use of ice massage directly over the affected area, phonophoresis or iontophoresis, physician-prescribed analgesics and nonsteroidal antiinflammatory drugs (NSAIDs), rest, and protection of the area from unwanted stress to allow for healing.8,23,28
Relative rest rather than strict immobilization is used. A wrist cock-up splint can be used in severe cases to minimize stress on the inflamed wrist extensor tendons. The patient is allowed to remove the splint as needed to participate in controlled motion exercises that do not produce pain. Long-term, rigid immobilization is not indicated, because treatment goals are to not only reduce pain and swelling but also to encourage proper collagen alignment and scar tissue maturation.23 Without early protected motion, excessive tissue scarring and random collagen fiber alignment would severely limit normalized motion and function of the elbow and wrist.
During the initial healing stage, the PTA must encourage the patient to avoid any and all motions that may adversely affect healing. Short-term modifications in activities of daily living (ADLs), sports, and job-related activities must be addressed to provide a pain-free environment for healing. When this initial program fails to bring significant relief of symptoms, some physicians elect to inject the area with a steroid to reduce the inflammation.20,23
In addition, active gentle static stretching is advised for the wrist extensors to produce normalized, pain-free wrist flexion and extension (Fig. 22-2). Although specifically addressing treatment for the elbow, active motion and resistance exercises for the elbow and shoulder can be initiated if no wrist motion occurs to increase symptoms.

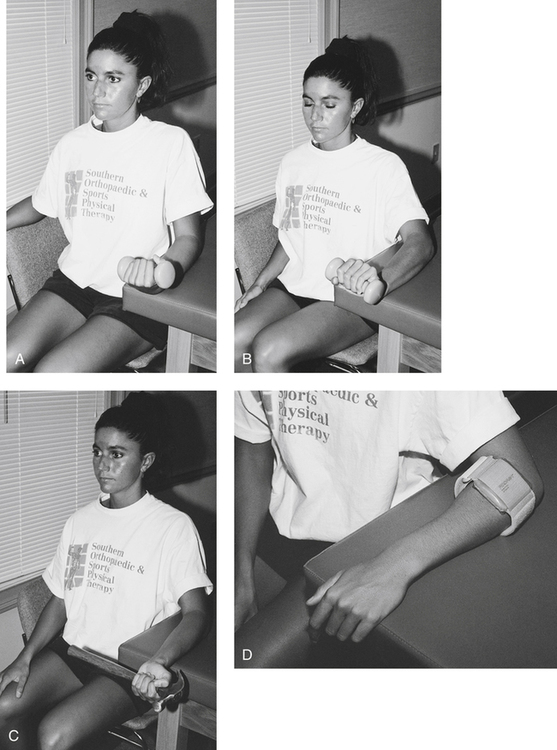
The PTA must carefully instruct the patient to perform all exercises within a pain-free range of motion (ROM). Throughout all phases of recovery, the patient must avoid stressful, pain-producing activities to prevent the exacerbation of the inflammatory condition. Progressive motion exercises and increased resistance exercise are the foundation for a return to functional activities. Concentric and eccentric muscle contractions are added once the patient can demonstrate increased quality of multiangle isometric contractions. Care must be taken when initiating both concentric and eccentric resistance exercises because frequently these contractions produce symptoms. Light resistance is advocated when having patients perform these exercises for the first time. An important component for all resistance exercises used with lateral epicondylitis is the performance of slow, controlled eccentric contractions. Eccentric muscle contractions produce greater tension than either concentric or isometric exercise. In addition, energy use involving adenosine triphosphate (ATP) is less for eccentric exercise than for either concentric or isometric exercise. Eccentric muscle contractions are, in fact, advocated by Curwin and Stanish8 for the treatment of tennis elbow, and the rationale for the performance of eccentric exercise is described by Reid and Kushner24 as, “Exercising the muscle eccentrically allows it to withstand greater resistance and prevent injury, which occurs by eccentrically loading an inflexible muscle.”24
Resistive exercises emphasizing the eccentric phase are described in Figure 22-3, A-B. A hammer is an effective strengthening tool for the treatment of lateral epicondylitis. However, when instructing the patient to perform pronation and supination of the forearm for the first time, the PTA should have the patient hold the hammer close to its head (Fig. 22-3, C). As the patient gains strength and can control the resistance of the hammer eccentrically, the patient should gradually hold the hammer at the midshaft. As strength improves further, the patient should be allowed to hold the hammer at the end of the shaft, which requires greater eccentric muscle control, strength, and torque. In the same manner, strength can be gained for radial and ulnar deviation through use of the hammer. With a gradual return to functional activities, some physicians and therapists advocate the use of a counterforce brace to help dissipate the “overload forces” on the common origin of the wrist extensors (Fig. 22-3, D).8,20,28
Surgery is rarely necessary for this condition because physical therapy management frequently is effective. In rare instances when conservative means fail to reduce pain and improve function, the surgeon may elect to surgically excise the “angiofibroblastic tissue at the origin of the extensor carpi radialis brevis muscle.”29
Medial Epicondylitis
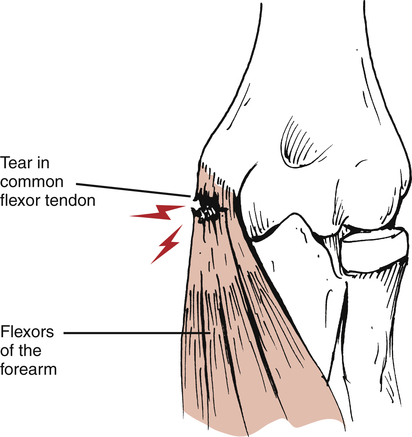
Medial epicondylitis, an overuse condition, affects the origin of the pronator teres, flexor carpi radialis, flexor digitorum sublimis, and flexor carpi ulnaris at the medial epicondyle of the elbow.23 Although it occurs less often than lateral epicondylitis (the ratio of lateral epicondylitis to medial epicondylitis is 7:1),28 it is no less incapacitating to the patient. Again the dominant feature is pain with palpation over the medial epicondyle, active motion, and particularly with resisted wrist flexion and full passive wrist extension (Fig. 22-4).23,24
Management of Medial Epicondylitis
The acute management phase of this inflammatory overuse condition, also referred to as golfer’s elbow, concentrates on the management of pain and swelling. Usually the physician prescribes NSAIDs, ice (protect the ulnar nerve), phonophoresis or iontophoresis, relative active rest (not immobilization), protection, and gentle active motion exercises. The criteria-based treatment plan parallels that for lateral epicondylitis, although it obviously focuses on the wrist flexors. Static low-load, long-duration stretching3,4 can proceed as pain allows. The PTA must encourage the patient to avoid repetitive flexing of the wrist and pronating of the forearm if these motions produce pain. Modifications in lifting, twisting, pulling, or turning of the wrist and forearm must accompany each phase of recovery to avoid stress on the medial structures. Moist heat and ultrasound can be applied to the medial epicondyle before stretching once motion has improved without pain. Resistance training can then begin with submaximal isometrics, progressing to higher-quality isometric multiangle contractions, and ultimately to concentric and eccentric isotonic and isokinetic resistance exercises. The patient is instructed in the active use of the shoulder of the affected limb and strongly encouraged to follow a conditioning program to maintain or enhance cardiovascular fitness, strength, and flexibility throughout the rehabilitation process.
Although the resolution of pain and swelling is paramount for active use of the wrist and forearm, regaining lost motion caused by pain and muscular dysfunction is critical for function and a return to normal daily activities. The normal elbow ROM is 0° to approximately 145° of flexion.29 However, most daily activities can be carried out within a functional ROM of 30° to 130° of flexion.24,29 In addition, normal pronation of 75° and supination of 85° exceeds the functional arc of motion of 50° needed to carry out most ADLs. Therefore the PTA must encourage pain-free early protected motion to facilitate the collagen fiber alignment needed for both functional scar maturation and purposeful motion to perform ADLs.
Medial Valgus Stress Overload
Injuries to the elbow often occur in the overhead athlete. The repetitive overhead motion involved in throwing is responsible for unique and sport-specific patterns of injuries to the elbow. These are caused by chronic stress overload or repetitive micro-traumatic stress observed during the overhead pitching motion as the elbow extends at over 2300°/s, producing a medial shear force of 300 N and lateral compressive force of 900 N.11,32 In addition, the valgus stress applied to the elbow during the acceleration phase of throwing is 64 N·m,11,32 which exceeds the ultimate tensile strength of the ulnar collateral ligament.10 Thus the medial aspect of the elbow undergoes tremendous tensile (distraction) forces and the lateral aspect is forcefully compressed during the throwing motion.
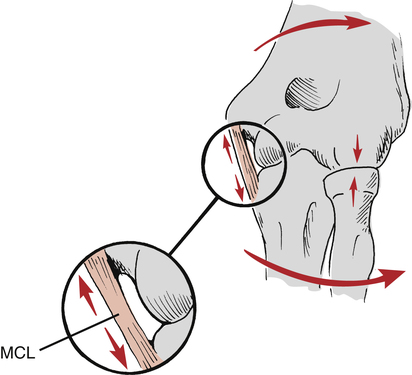
Medial valgus stress overload, also known as valgus extension overload (VEO) occurs commonly among patients who participate in repetitive throwing and racquet sports such as javelin throwing, baseball, racquetball, and tennis.9,21,23 The overhead athlete is susceptible to these specific elbow injuries. A number of forces act on the elbow during the act of throwing,11,32 including valgus stress with tension across the medial aspect of the elbow. These forces are maximal during the acceleration phase of throwing. Compression forces are also applied to the lateral aspect of the elbow during the throwing motion. The posterior compartment is subject to tensile, compressive, and torsional forces during acceleration and deceleration phases. This may result in valgus extension overload within the posterior compartment, leading to osteophyte formation, stress fractures of the olecranon, or physeal injury.1,35 These stresses approach the ultimate failure load of the ligament with each throw. The repetitive nature of overhead throwing activities such as baseball pitching, javelin throwing, and football passing further increase the susceptibility of medial elbow injuries including ulnar collateral ligament (UCL) injuries, by exposing the ligament to repetitive micro-traumatic forces. Clinical differences exist between medial valgus stress overload and medial epicondylitis. Although medial epicondylitis represents a chronic overuse syndrome affecting the soft-tissue musculotendinous origin of the wrist flexors and pronators, medial valgus stress overload occurs to the capsuloligamentous structures (medial [ulnar] collateral ligament) as a result of repetitive valgus stress to the elbow (Fig. 22-5).9,21,23
Patients usually complain of pain over the medial aspect of the elbow and the posterior aspect of the olecranon.21,23 During the physical therapist’s (PT) initial evaluation, the PTA may observe the performance of ligament stability tests to confirm the presence of UCL laxity. The affected arm is held in 20° to 30° of flexion while the humerus is held in full external rotation to unlock the olecranon process from the olecranon fossa. A medial or valgus stress then is applied to the elbow to assess the stability of the UCL (Fig. 22-6).21,23
Management of Medial Valgus Stress Overload
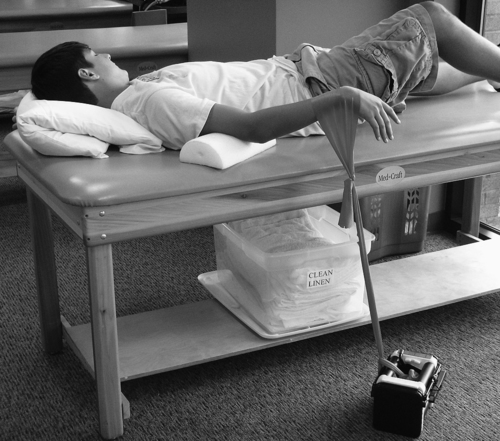
The elbow is predisposed to flexion contractures due to the intimate congruency of the joint articulations, the tightness of the joint capsule, and the tendency of the anterior capsule to develop adhesions following injury.33 The brachialis muscle also attaches to the capsule and crosses the elbow joint before becoming a tendinous structure. Injury to the elbow may cause excessive scar tissue formation of the brachialis muscle as well as functional splinting of the elbow.33 Gentle low-load static stretching begins as soon as pain allows. Therefore the stretching regimen focuses on all wrist motions, forearm pronation and supination, and elbow flexion and extension as long as no symptoms of pain occur with these activities. If the patient continues to have difficulty achieving full extension using ROM and mobilization techniques, a low-load, long duration (LLLD) stretch may be performed to produce a deformation (creep) of the collagen tissue, resulting in tissue elongation.12,27,30,31 This technique is extremely beneficial for regaining full elbow extension. The patient lies supine with a towel roll or foam placed under the distal brachium to act as a cushion and fulcrum. Light resistance exercise tubing is applied to the wrist of the patient and secured to the table or a dumbbell on the ground (Fig. 22-7). The patient is instructed to relax as much as possible for 10 to 15 minutes per treatment. The amount of resistance applied should be of low magnitude to enable the patient to perform the stretch for the entire duration without pain or muscle spasm. This technique should impart a LLLD over a prolonged period of time to achieve maximal benefits. Patients are instructed to perform this stretch technique several times per day, equaling 60 minutes of total end range time. Patients may perform a 15 minute stretch, 4 times per day.16 This program has been extremely beneficial for patients with a stiff elbow.
Surgery is considered if conservative treatment fails to restore function and eliminate pain. Degenerative changes, which are usually present in the adult, must be addressed surgically.21,24 In general, an osteotomy is performed to remove osteophytes (bone spurs) and fibrotic, degenerated tissue.21,24
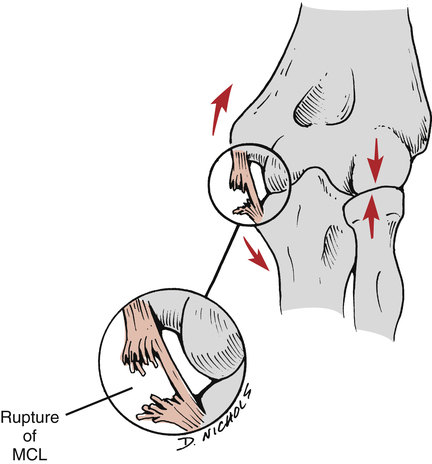
Acute rupture (grade III ligament rupture) of the medial (ulnar) collateral ligament can occur in skeletally mature adults if valgus stress is applied suddenly with sufficient force (Fig. 22-8).
If early active protected joint motion and progressive resistance exercise have been used, authorities suggest that the injured patient can resume throwing activities approximately 3 months after injury.21 However, surgery may be necessary to stabilize the joint if the patient does not demonstrate improved valgus stability and continues to have dysfunction.
Generally if the ulnar collateral ligament is ruptured midsubstance, a direct repair is carried out and a reconstructive procedure is performed. The palmaris longus or gracilis graft source is taken and passed in a figure-of-eight pattern through drill holes in the sublime tubercle of the ulna and the medial epicondyle.2 A subcutaneous ulnar nerve transposition is performed at the time of reconstruction. Some surgeons are presently performing UCL reconstruction utilizing the docking procedure, as described by Rohrbough and colleagues.26
Postoperative rehabilitation begins immediately, with the patient’s affected limb immobilized in a brace to protect against valgus stress. Instructions are given to perform hand, wrist, and shoulder exercises to maintain motion. Usually by the third week postoperatively, ROM should approach at least 20° of extension while slowly progressing to 110° of elbow flexion.9 The continuous use of ice and therapeutic agents (e.g., ultrasound, transcutaneous electrical nerve stimulation, and galvanic stimulation)24 are prescribed as necessary. Progressive resistance concentric and eccentric contractions are used for the wrist of the involved limb, whereas submaximal isometrics can begin for elbow flexion and extension.
Shoulder strengthening and flexibility exercises also can begin during the third week of recovery.9 However, care must be taken to avoid external shoulder rotation exercises because this motion produces valgus stress on the elbow.9
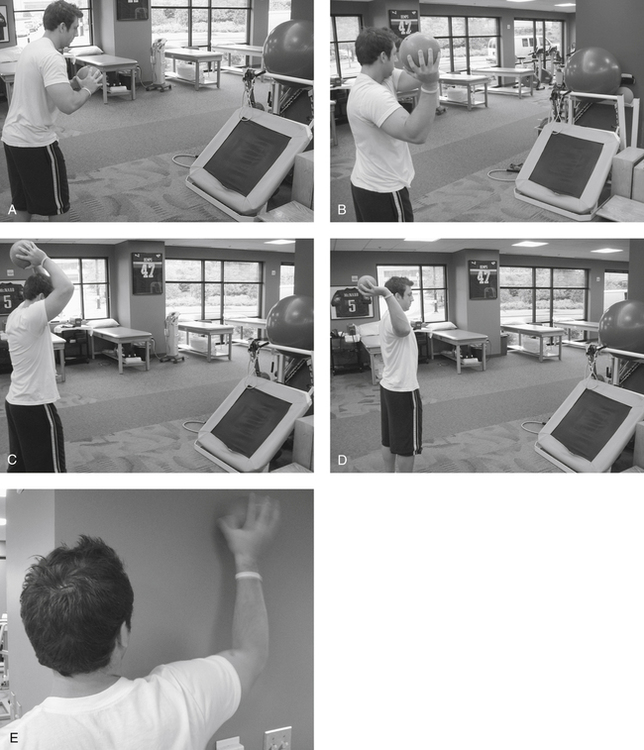
Usually by 4 to 6 weeks after surgery, ROM should be 0° to 130°.9 In addition, concentric and eccentric resistance exercises for elbow flexion and extension are added progressively as tolerated. Gentle forearm pronation and supination exercises also can be made more challenging. From 2 to 4 months after surgery, functional training can begin with an emphasis on shoulder, elbow, and wrist strengthening, motion exercises, and plyometrics. Plyometric drills can be an extremely beneficial form of functional exercise for training the elbow in overhead athletes.33,34 Plyometric exercises are performed using a weighted medicine ball during the latter stages of this phase to train the shoulder and elbow to develop and withstand high levels of stress (Fig. 22-9). Plyometric exercises are initially performed with two hands performing a chest pass, a side-to-side throw, and an overhead soccer throw. These may be progressed to include one hand activities such as 90/90 throws, and wall dribbles. For patients returning to sports that involve the upper extremity, such as golf, tennis, javelin, baseball, and softball, these patients are placed on an interval sport program as described by Reinold and colleagues.25 Ultimately, it takes 10 to 12 months after elbow reconstruction and rehabilitation for valgus instability before a functional return to overhead, competitive sports is allowed.21
Lateral Collateral Ligament Injury
Stability of the elbow occurs mainly through the osseous configuration but secondarily through the medial and lateral collateral ligaments (LCLs). In particular, the lateral ligament complex prevents rotational instability between the distal humerus and the proximal radius and ulna. However, disrupting the soft-tissue constraints through a traumatic onset often results in subluxation or dislocation. The elbow is the second most commonly dislocated large joint after the shoulder.14,15 In children younger than the age of 10 years, elbows are the most commonly dislocated joint.
Management of Lateral Collateral Ligament Injury
Operative management
The reconstruction technique is intended to recreate the ulnar aspect of the LCL complex. O’Driscoll22 recommends first repairing the avulsed origin of the lateral ligament complex to its isometric origin on the lateral epicondyle if possible. This is typically followed by augmentation of the repair with graft choices ranging from the palmaris longus, lateral triceps tendon, semitendonosus allograft or autograft, or even a plantaris allograft. The physician’s preference will often dictate which graft is used during the reconstruction.
By week 8, the patient may progress to the advanced strengthening phase. The goals of this phase are to increase strength, power, and endurance while maintaining full elbow ROM. Aggressive strengthening exercises involving eccentric and plyometric contractions are also included, usually at 10 weeks postoperative. These sport-specific activities are progressed through increasing the number of repetitions, increasing the weight of the medicine ball or increasing the timed bouts of the activity to improve endurance. Beyond week 16, the patient is reassessed to determine strength levels before progressing to an interval sports program. Sufficient strength, generally within 15% of the contralateral side, and full ROM indicate the patient is ready to begin an interval program.25
FRACTURES OF THE ELBOW
Fractures of the Distal Humerus (Supracondylar Fractures)
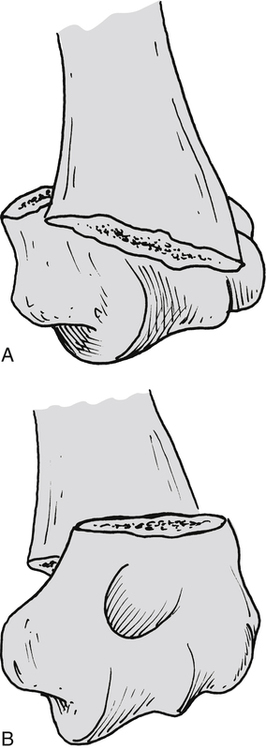
By definition a supracondylar fracture is a transverse fracture of the distal third of the humerus.17 These frequent injuries usually occur in children.17,21,28 Supracondylar fractures generally are of two types.7,17,29 Type I is the most common and refers to an injury that occurs as a result of a fall on an extended, outstretched arm in which the distal humerus fragment is displaced posteriorly and is maintained in that position because of the strong pull of the triceps (Fig. 22-10, A).7,29 Type II is considered a flexion injury and occurs after direct trauma to the posterior aspect of the elbow in which the distal humeral fragment lies anterior to the humerus (Fig. 22-10, B).7,29
The most common treatment of these fractures is by closed reduction and immobilization for 4 to 6 weeks. The affected arm is held in a flexed position to allow the triceps to help maintain the fracture in a stable position.17,29
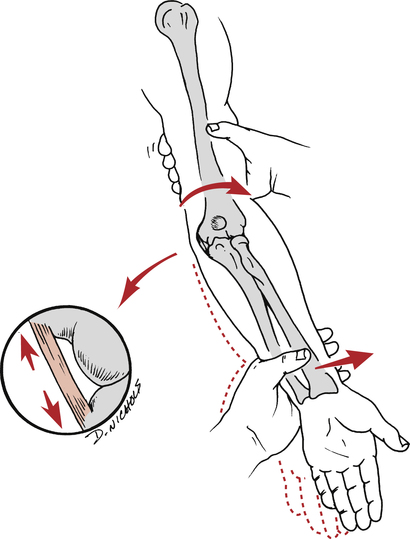
Complications arising from supracondylar fractures18 include nonunion, malunion, and joint contracture. Perhaps the most disastrous complication results from vascular compromise.7,17,18,29 As the fracture fragments are displaced, hemorrhage beneath the deep fascia produces an ischemic injury that creates an arterial and venous obstruction (usually affecting the brachial artery), leading to a Volkmann ischemic contracture (Fig. 22-11).7,18,28 What is most important is that the clinical signs and symptoms of ischemic obstruction may not be noticed until the end of immobilization.7 The symptoms of Volkmann ischemic contracture can occur throughout each phase of recovery after a supracondylar fracture.
Stralka and Brasel28 outline six symptoms authorities define as indicating vascular obstruction:
 Severe pain in the forearm muscles
Severe pain in the forearm muscles
 Limited and extremely painful finger movement
Limited and extremely painful finger movement
 Purple discoloration of the hand with prominent veins
Purple discoloration of the hand with prominent veins
 Initial paresthesia followed by loss of sensation
Initial paresthesia followed by loss of sensation
Restoration of elbow function after supracondylar fractures initially focuses on motion exercises that do not stress the fracture site. Therefore passive stretching is contraindicated during the early healing phase.17 Gentle active exercises for the upper arm, wrist, and shoulder, of course, should be performed to the patient’s tolerance. Resistance exercises consisting of submaximal isometrics and progressing to concentric and eccentric muscle contractions are allowed, pending confirmation of secure union of the fracture fragments.
Intercondylar T or Y Fractures
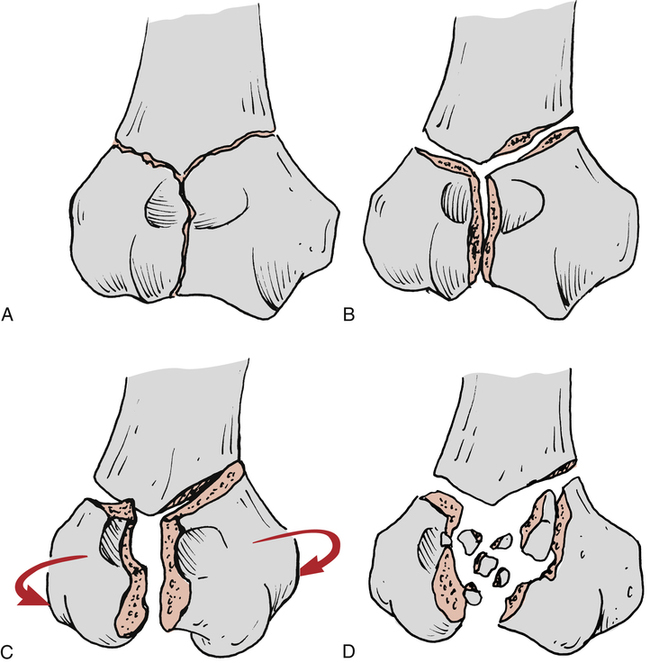
In addition to nondisplaced or displaced transverse supracondylar fractures, potentially more significant fracture patterns can occur with falls or direct trauma to the elbow. Intercondylar fractures describe injuries that extend between the condyles of the distal humerus and involve the articular surfaces of the elbow joint.7,17,18,29 According to Strege29 and Miller,18 there are four classifications of intercondylar fractures that display a T or Y configuration7,17,21:
 Type I: A nondisplaced fracture that extends between the two condyles (Fig. 22-12, A)
Type I: A nondisplaced fracture that extends between the two condyles (Fig. 22-12, A)
 Type II: A displaced fracture without rotation of the fracture fragments (Fig. 22-12, B)
Type II: A displaced fracture without rotation of the fracture fragments (Fig. 22-12, B)
 Type III: A displaced fracture with a rotational deformity (Fig. 22-12, C)
Type III: A displaced fracture with a rotational deformity (Fig. 22-12, C)
 Type IV: A severely comminuted fracture with significant separation between the two condyles (Fig. 22-12, D)
Type IV: A severely comminuted fracture with significant separation between the two condyles (Fig. 22-12, D)
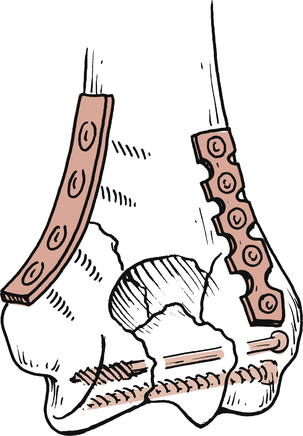
The type of fracture dictates a course of treatment that parallels the significance of the injury. With a type I nondisplaced fracture, treatment can be immobilization for approximately 3 weeks, followed by progressive, gentle active motion. Resistance exercises are deferred until secure bone union has been confirmed radiographically. With types II and III displaced fractures, the treatment is open reduction with internal fixation (ORIF) with the use of Kirschner wires, side plates, and lag screws to secure and stabilize the displaced fracture fragments (Fig. 22-13).17,18,29 Type IV comminuted intercondylar fractures are treated differently for adults and elderly patients with poor bone quality (osteoporosis).18,29 Adult patients are usually treated with an ORIF procedure to stabilize the fragments. However, in elderly patients with generally poor bone quality (osteopenic bone), a treatment procedure referred to as the bag of bones technique is used.17,18,29 This technique calls for the use of a “collar and cuff” sling, with the affected elbow flexed as far as the limits of swelling and circulatory compromise allow.29 With the elbow flexed and able to hang freely within the sling, gravity is used to help obtain possible reduction of the fracture fragments (Fig. 22-14).18,29
During the early postimmobilization period, no passive manipulation or passive stretching can be performed.29 Strege29 reports an appreciable risk of joint ankylosis when passive stretching and manipulation are performed during early postinjury elbow rehabilitation.
Once wound closure has occurred after an ORIF procedure, the use of a whirlpool bath may aid local circulation, removal of waste, reduction in soft-tissue congestion, and enhancement of soft-tissue relaxation in preparation for protected active motion. Elbow flexion and extension, as well as forearm pronation and supination, are encouraged as prescribed by the physician and directed by the PT. Stable union of the fracture signifies more active involvement with progressive motion exercises and the initiation of resistance exercise training to regain strength. If the patient demonstrates loss of motion, the physician and PT may decide to perform specific joint mobilization techniques once bone union is secure. This does not conflict with the mentioned contraindication for passive manipulation and stretching immediately after immobilization. Some patients ultimately may have residual loss of motion. However, functional activities can be performed with flexion and extension of 30° to 130° and pronation and supination of 50°.29
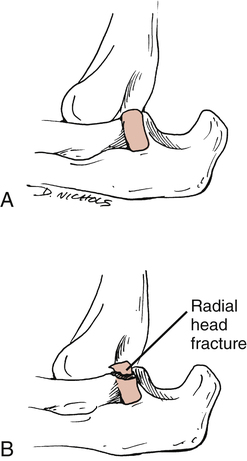
Radial Head Fractures
Another common fracture that occurs as a result of a fall on an outstretched arm is a radial head fracture. These fractures represent approximately one third of all elbow fractures and nearly 20% of all elbow trauma.13
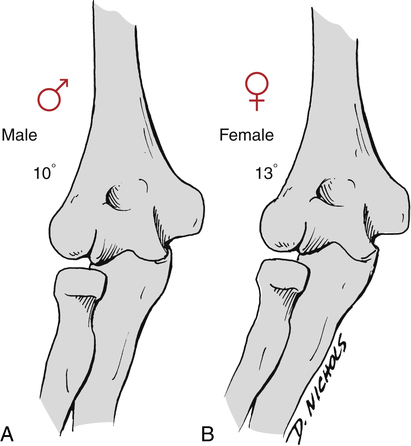
The definition of the “carrying angle” of the elbow and the difference noted between men and women are important in understanding radial head fractures. The carrying angle is formed between the intersection of the long axis of the humerus and the axis of the ulna, with the elbow joint in full extension.29 A normal carrying angle for men is 10° of valgus; in women, it is 13° of valgus (Fig. 22-15).29 The clinical relevance is that a fractured radial head can lead to an increased valgus deformity and the varus elbow malalignment called a gunstock deformity.13
Radial head fractures generally are classified into four types, as follows (Fig. 22-16):
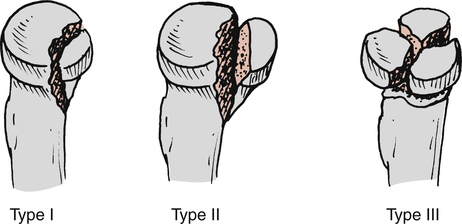
 Type I: A nondisplaced fracture
Type I: A nondisplaced fracture
 Type II: A marginal fracture with displacement
Type II: A marginal fracture with displacement
Treatment options parallel the significance of the injury and dictate the course of rehabilitation. Patients with type I nondisplaced radial head fractures usually need a period of immobilization ranging from 5 to 7 days up to 3 to 4 weeks.17,29 Usually, early active motion is allowed as soon as pain subsides. Because these fractures generally are stable (nondisplaced), healing occurs with very good results.17 Terminal elbow extension may be recovered many months after type I radial head fractures.17
With a type II displaced fracture, the radial head can be excised or stabilized with an ORIF procedure. With a type III comminuted radial head fracture, the fractured area is excised.13,17,18,29
Rehabilitation after an ORIF or radial head excision usually calls for immobilization in a hinged splint to protect the healing bone and surrounding soft tissues. As noted, excision of the radial head can lead to increased varus or valgus deformity. In either case, migration of the radial shaft may occur after excision and place stress on the distal ligamentous radioulnar articulation.13,17,18 Therefore any discomfort expressed by the patient at the distal radioulnar joint after excision of the radial head usually results from added stress on this area created by the disrupted proximal radial segment.13,17,18 When the patient is immobilized, the hand, wrist, and shoulder of the affected limb are exercised as tolerated. The patient also is encouraged to participate in a general conditioning program of aerobic exercise, strength training, and flexibility exercises. Pain and swelling usually are managed satisfactorily by placing ice packs directly over the painful area. Early active ROM exercises are advocated 3 to 5 days postoperatively by some or deferred for up to 3 weeks by others.13,29 Restoration of motion is the cornerstone for recovery after radial head fractures. As noted, joint restrictions secondary to arthrofibrosis and contractures can occur, with pronation and supination most commonly affected after radial head fractures.
Olecranon Fractures
Olecranon fractures commonly result after a fall on the point of the elbow (olecranon process) or indirectly from forceful contraction of the triceps.17 Generally, they are classified as either nondisplaced or displaced fractures. Displaced fractures of the olecranon have four subclassifications18:
The treatment for nondisplaced olecranon fractures requires immobilization for 6 to 8 weeks,7,17 although as little as 3 weeks or less is used in some cases (particularly in older patients).18,29 The position in which nondisplaced olecranon fractures are immobilized is somewhat controversial, in that some authorities advocate placing the affected arm in extension or slight flexion,5,7,13,17 whereas others recommend placing the affected arm in 45° to 90° of flexion.18,29 The rationale for placing the elbow in 45° of flexion is the likelihood of the loss of flexion after immobilization.29 In addition, Strege29 suggests that immobilization should not exceed 45° because of the risk of displacing fracture fragments.
Usually, nondisplaced olecranon fractures are allowed gentle active ROM exercises after 3 weeks of immobilization. Flexion of the affected arm should not exceed 90° for the first 6 to 8 weeks after injury so that fracture fragments can heal.13,29
Displaced or comminuted fractures of the olecranon can be treated with an ORIF procedure to secure the fragments. With severely comminuted fractures, excision of as much as 80% of the olecranon can occur without loss of joint stability.18,29
Progressive flexion and extension movements must proceed cautiously and slowly to prevent displacement of the fragments. In addition, the patient must be carefully instructed to initially perform resistance exercises well within the limits of pain and motion restrictions to allow for proper bone healing. The strong contractions of the biceps during flexion and the triceps during extension activities are effective to gradually overcome most motion limitations observed early after injury or surgery. Full recovery after olecranon fractures may take 6 months to 1 year.13
Fracture-Dislocations
A fall on an extended outreaching arm causes isolated elbow dislocations and combined fracture-dislocations (Fig. 22-17).9,17,19,24,28 Conwell7 reports that “with the exception of the shoulder, the elbow is the most frequently dislocated joint in the body.” This injury occurs most often in men, with the nondominant arm representing about 60% of these injuries.19
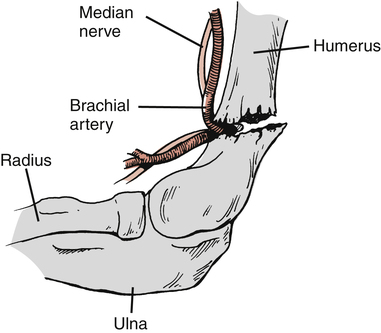
Posterior elbow dislocations are the most common, whereas anterior dislocations represent 1% to 2% of all elbow dislocations.19 Associated fractures of the radial head occur in approximately 10% of elbow dislocations.19,28 In addition, associated neurovascular injuries can occur with either isolated elbow dislocations or with fracture-dislocations.17,19,28,29 Injuries involve the median, radial, and ulnar nerves, as well as the brachial artery with elbow dislocations.19,29
Isolated posterior elbow dislocations are managed with closed reduction and immobilization.7,9,17–19,28 The elbow is placed in 90° of flexion in a splint for 3 to 6 weeks.7,17,29 During this period, hand and shoulder motion is allowed if no offensive stress is applied to the elbow. Early active ROM exercises can begin during the first week after reduction.29 However, no passive ROM or stretching is allowed because of the risk of myositis ossificans,17,28 which results from aggressive passive stretching and mobilization. Active motion is not believed to cause this condition.28 Therefore gentle active flexion and extension exercises are added as pain, swelling, and soft-tissue healing dictate. Because this injury represents a hyperextension trauma that significantly affects the joint capsule, muscle, tendon, and frequently ligamentous restraints, extensive soft-tissue healing is necessary for a stable, functional joint. The joint capsule of the elbow may require 8 to 10 weeks to heal satisfactorily.9 Restoration of elbow extension therefore must proceed cautiously because the mechanism of injury is usually elbow hyperextension. Resistance exercises can begin as soft-tissue healing progresses. Eccentric and concentric resistance exercises for the biceps can be emphasized to reduce hyperextension forces.9 Resistance-type exercises are deferred for at least 3 weeks to allow for acute symptoms to subside. However, aggressive elbow extension must be prevented until 8 to 10 weeks have elapsed.9,19
The most common complication after elbow dislocation is loss of extension.19,28,29 Ten weeks after dislocation, a 30° flexion contracture is common, and a 10° flexion contracture is typically observed 2 years after injury.19 However unacceptable this loss of motion may be, it does not represent an “overwhelming functional deficit.”29
The treatment of fracture-dislocations centers on the appropriate management of the fracture (most commonly the radial head) and reduction of the elbow. In most cases, radial head excision is performed to minimize the development of myositis ossificans.28 Therefore with radial head excision, proximal migration of the radius can result in stress and pain to the distal radioulnar ligamentous articulation.17,18,29
Rehabilitation after fracture-dislocation of the elbow focuses on early protected active motion. Passive stretching again is strictly avoided during the early recovery phases of healing. With radial head excision, a loss of 25° to 30° of pronation and supination can be expected if postoperative immobilization lasts longer than 4 weeks.28 As with isolated dislocation, loss of full elbow extension is not uncommon.
MOBILIZATION OF THE ELBOW
The rationale for specific joint mobilization is to avoid joint restrictions or hypomobility, which can limit the normal joint arthrokinematics.6 In many instances, arthrofibrosis occurs as a result of immobilization and internal fixation methods used to stabilize fracture fragments.
The PT determines if mobilization is indicated after injury, surgery, or immobilization based on tissue healing constraints, the nature of the joint restriction (hypomobility of noncontractile tissue or articular surface dysfunction),6 and whether passive motion is indicated for the treatment of joint limitations. The PT must clearly define the specific indications for mobilization with reference to the exact technique to be employed, rate of movement, amplitude of force, and direction of the force applied to the elbow. To obtain relaxation, the PTA must place the patient in a comfortable position, with specific attention paid to the support and stability of the shoulder, elbow, and arm of the patient. Before joint mobilization is applied, thermal agents are employed to reduce tissue congestion, aid in the removal of wastes, improve tissue extensibility, and enhance relaxation of the patient and the affected joint.
Injuries to the elbow that require mobilization should increase in flexion, extension, or both. Wooden36 outlines three techniques used to enhance general motion, flexion, and extension of the elbow.
To enhance general mobility of the elbow, the patient should be supine with the affected elbow flexed to 90°. The shoulder of the affected limb is held at the patient’s side or in an abducted position. The PTA places both hands at the proximal aspect of the forearm, and directs a straight lateral distraction force that directs the forearm away from the humerus (Fig. 22-18).

Humeral-ulnar abduction is employed to promote elbow extension.36 The patient should be supine with the affected arm abducted and the elbow slightly flexed. The PT sits to the patient’s affected side with one hand stabilizing the distal lateral humerus and the other hand firmly grasping the ulnar aspect of the distal forearm. In this position, the PT directs a valgus or abduction force to the elbow (Fig. 22-19).36

An adduction technique is applied to increase elbow flexion.36 The patient remains supine with the affected arm abducted. The PT sits to the patient’s affected side and stabilizes the distal humerus on the medial aspect with one hand, while placing the opposite hand on the distal radial aspect of the forearm. In this position, the PT directs a varus or adduction force to the elbow (Fig. 22-20).