17
Orthopedic Management of the Ankle, Foot, and Toes
Walter L. Jenkins and D.S. Blaise Williams
1. Identify common foot and ankle ligament injuries.
2. Describe intervention methods for common foot and ankle ligament injuries.
3. Identify and describe common lower leg, ankle, and foot tendon injuries.
4. Outline and describe common methods of intervention for lower leg, ankle, and foot injuries.
5. Identify common foot and ankle fractures.
6. Discuss common methods of intervention for foot and ankle fractures.
7. Identify and describe common methods of intervention for toe injuries.
8. Describe common mobilization techniques for the ankle, foot, and toe.
LIGAMENT INJURIES OF THE ANKLE
Injuries to the lateral ligament complex (the anterior talofibular ligament, fibulocalcaneal ligament, and posterior talofibular ligament) account for approximately 14% to 25% of all sports-related injuries.34,62 Therefore inversion ankle sprains are among the most common sports and orthopedic injuries.31,32,91 Studies report that approximately 95% of all ankle sprains occur to the lateral ligament complex.92 Additionally, injuries to associated structures including articular cartilage and the synovial membrane have been identified on arthroscopy in individuals who had recurrent or recalcitrant lateral ankle sprains.59 Untreated ankle sprains may lead to chronic pain, muscular weakness, and instability.32 Ankle joint osteoarthritis has been observed in patients with chronic ankle instability.108
Lateral Ligament Injuries (Inversion Ankle Sprains)
Mechanisms of Injury
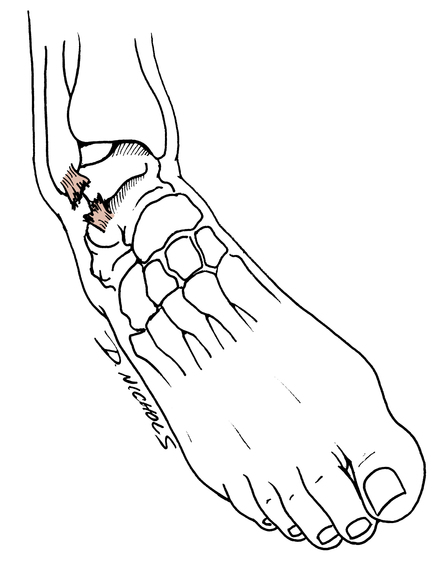
Ligament sprains of the lateral aspect of the ankle usually are caused by plantar flexion, inversion, and adduction of the foot and ankle (Fig. 17-1).97 Large forces are not needed to produce an ankle sprain. Stepping off a curb, stepping into a small hole, or stepping on a rock can produce sudden plantar flexion and inversion motions. During athletic competition, stepping on an opponent’s foot is a common occurrence that leads to lateral ligament sprains of the ankle. Most commonly ankle sprains occur with the foot is in an unloaded or non–weight-bearing (NWB) position before the injury.104
Classification of Sprains
Classifying inversion ankle sprains can be difficult and confusing.97 The standard classification of ligament injuries (e.g., first-, second-, and third-degree sprains) requires elaboration when applied to inversion ankle sprains, specifically addressing grades, degrees, and descriptive severity of the injury (mild, moderate, or severe). A classification model described by Leach64 is contrasted with the common standard classification of ankle sprains as a means of comparison and to illustrate the potential for confusion about classification of inversion ankle sprains.
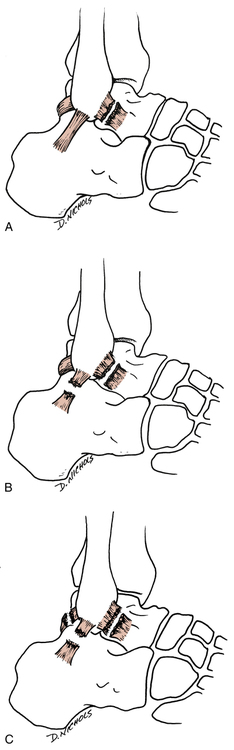
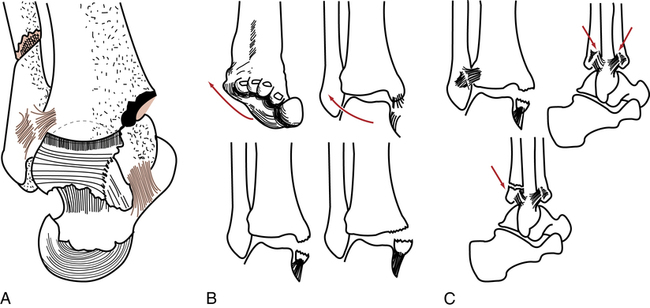
 First-degree sprain: Single ligament rupture.64 The anterior talofibular ligament is completely torn. In the standard classification of ligament sprains a complete tear or rupture of a ligament is called a grade III, or third-degree sprain (Fig. 17-2, A).
First-degree sprain: Single ligament rupture.64 The anterior talofibular ligament is completely torn. In the standard classification of ligament sprains a complete tear or rupture of a ligament is called a grade III, or third-degree sprain (Fig. 17-2, A).
 Second-degree sprain: Double ligament rupture.64 Both the anterior talofibular ligaments and fibulocalcaneal ligaments are completely torn. The standard classification describes a partially torn single ligament as a grade II sprain (Fig. 17-2, B).
Second-degree sprain: Double ligament rupture.64 Both the anterior talofibular ligaments and fibulocalcaneal ligaments are completely torn. The standard classification describes a partially torn single ligament as a grade II sprain (Fig. 17-2, B).
 Third-degree sprain: All three lateral ankle ligaments (anterior talofibular, posterior talofibular, and fibulocalcaneal) are completely torn.64 In the standard classification, a single ligament that is completely torn is defined as a grade III ligament sprain (Fig. 17-2, C).
Third-degree sprain: All three lateral ankle ligaments (anterior talofibular, posterior talofibular, and fibulocalcaneal) are completely torn.64 In the standard classification, a single ligament that is completely torn is defined as a grade III ligament sprain (Fig. 17-2, C).
Clinical Examination
Testing
Ankle stability tests are used by the physician and the physical therapist (PT) to identify and quantify the integrity of the lateral ligament complex. Injury to the anterior talofibular ligament can be assessed clinically by performing the anterior drawer test (Fig. 17-3).97 The patient must be in a relaxed seated or semirecumbent position with the involved leg flexed 90° at the knee and the involved ankle slightly plantar flexed. Stabilize the distal tibia and support it with one hand, while using the other hand to gently but firmly grasp the calcaneus and attempt to translate or pull the ankle forward. No excessive motion is seen or felt if the ligament is intact. However, the ankle demonstrates excessive forward or anterior motion if the anterior talofibular ligament is torn.
The talar tilt test or inversion stress test examines the ankle ligament’s resistance to maximal inversion stress (Fig. 17-4).97 The patient is in the same position used for the anterior drawer test, and the ankle is gradually stressed by exertion of constant pressure over the lateral aspect of the foot and ankle while counter pressure is applied over the inner aspect of the lower leg until maximal inversion is reached.10 The severity of ligament injury should be graded according to the classification system used by the physician or the supervising PT.
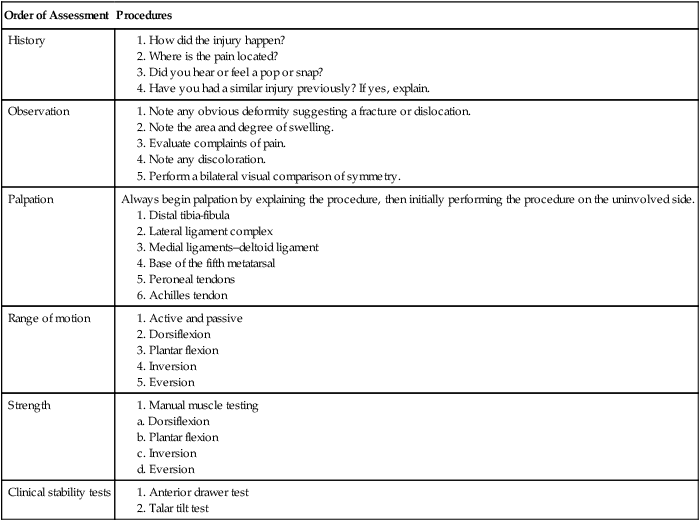
Order of procedures
Table 17-1 outlines the procedure for evaluation of inversion ankle sprains. The mechanism of injury that produces an inversion ankle sprain also may cause other conditions that must be differentiated by the physician91,97 and PT, such as fracture of the base of the fifth metatarsal, malleolar fractures, osteochondral fractures, osteochondritis dissecans, midfoot ligament sprains, and subluxing peroneal tendons.
Table 17-1
Physical Therapist Initial Evaluation Outline for the Clinical Assessment of Inversion Ankle Sprains
| Order of Assessment | Procedures |
| History |
Intervention
The specific rehabilitation program used to treat inversion sprains depends on the severity of sprain (first-, second-, or third-degree). Generally first- and second-degree sprains can be effectively managed nonoperatively with a supervised rehabilitation program.98
Initial management of acute inversion ankle sprains calls for rest, ice, compression, and elevation (RICE). Rest is a relative term used to define avoidance of unwanted stress; it does not necessarily require complete avoidance of all stress. The application of ice, compression, and elevation is directed at minimizing and reducing intense inflammatory response, hemorrhage, swelling, pain, and cellular metabolism to provide the most conducive environment for tissue healing.91
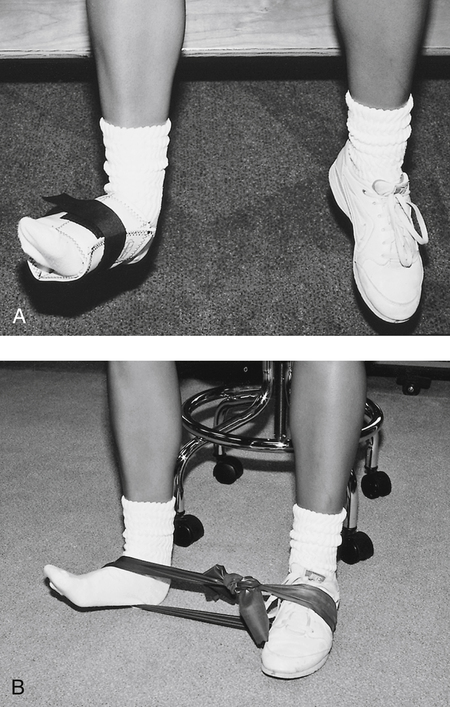
The moderate-protection phase can begin once the patient can bear weight on the injured limb without crutches, perform all ROM and isometric exercises without undue complaints of pain, and control the swelling. This phase encourages the use of the RICE principle, full weight bearing (FWB), and continued ligament support with the use of braces or tape. More progressive exercises are initiated, including concentric and eccentric contractions (Fig. 17-5) (with ankle weights or latex bands), heel cord stretching (Fig. 17-6) (towel stretch, wall stretch, or prostretch), and standing toe and heel raises.

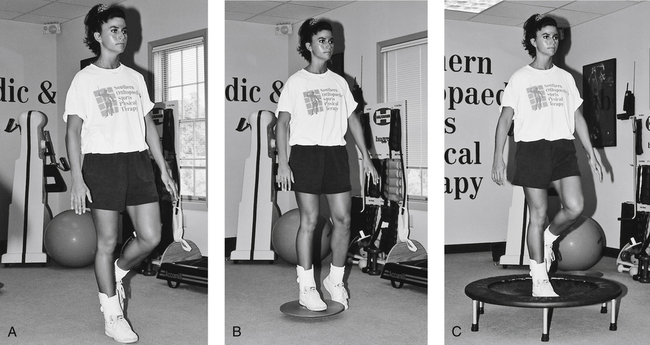
Proprioception exercises are commonly initiated during the moderate-protection phase. Protection of the ligament must be encouraged during these challenging exercises. Balancing on the injured limb on a flat surface is slowly progressed to a balance board, and then to a minitrampoline—all excellent exercises that stimulate balance, coordination, and muscular endurance (Fig. 17-7).
The minimum-protection phase can begin once the patient can perform all resistive exercises, (ankle weight, Thera-Band, and manual resistance) ambulate without pain or limping, and swelling is reduced. Although proprioception training is commonly used in practice there are few articles outlining its effectiveness in rehabilitation.115
From 4 to 8 weeks after injury, new collagen formation allows almost-normal stresses to be applied.91 At this point, more functional activities are allowed, including straight-line jogging, large figure-of-eight running, jumping drills, and cutting activities.
The minimum-protection phase does not imply removal of all supportive devices. Maturation of the injured ligaments can take as long as 6 to 12 months.91 Therefore it is critical to encourage patient compliance with the use of either tape or a semirigid brace during all running activities.
Box 17-1 outlines a general three-phase rehabilitation program for an inversion ankle sprain. In all instances, if pain, swelling, or irritation persists, the patient is not taken to the next phase until he or she is pain free in the present phase. The ankle must be securely taped or braced when running, jumping, or otherwise performing aggressive, ballistic motions.
The treatment of grade III ankle sprains (using the standard classification) is somewhat controversial.91,98 At this time there are few, if any outcome studies that outline differences in conservative and surgical treatment for acute grade III injuries. Kerkhoffs and associates56 concluded that “there is insufficient evidence available from randomized controlled trials to determine the relative effectiveness of surgical and conservative treatment for acute injuries of the lateral ligament complex of the ankle.” Some authors10,12,103 report that surgery is needed because “surgical exploration often reveals that the torn ends of the fibulocalcaneal ligament are so widely separated that simple immobilization alone is not sufficient to allow the ligament to heal in a stable position.”10 However, other authors have found that “early controlled mobilization (functional treatment) was the method of choice and provided the quickest recovery in ankle mobility and the earliest return to work and physical activity without compromising the late mechanical stability of the ankle.”91 Therefore depending on the physician’s choice of treatment, a grade III sprain can be treated either surgically or with early controlled motion and supervised physical therapy. A good to excellent long-term prognosis can be expected in 80% to 90% of patients with grade III ankle sprains regardless of the intervention.54 However, if inadequate treatment is performed, chronic instability may occur leading to injuries to associated structures.31 Secondary to the possibility of chronic instability Ferran and Maffulli31 have proposed that athletes with acute grade III injuries be surgically treated.
Generally joint protection lasts longer with grade III ankle sprains than with grade I and II sprains. When these injuries are treated surgically, and postoperative immobilization is used, deleterious effects on muscle, bone, cartilage, tendons, and ligaments can be expected.1
Deltoid Ligament Sprains (Medial Ligament)
Acute isolated sprains of the deep and superficial layers of the deltoid ligament are rare, occurring in only 3% to 5% of all ankle sprains.91,92 It is clinically important to recognize that “complete deltoid ligament ruptures occur in combination with ankle fractures.”91
However, according to Hintermann and associates,43 sprains of the deltoid ligament appear to be more frequent than commonly recognized, leading to problems with posterior tibialis tendon dysfunction and chronic medial ankle instability. Fractures of the medial or lateral malleolus may cause disruption of the deltoid ligament.43
Intervention
Partial tears of the deltoid ligament are managed nonoperatively with physical therapy. Because complete ruptures occur with fractures, many authorities advocate surgical repair and fixation of the fracture fragments.14,20 However, some authors recommend casting, NWB for 6 weeks, then progressive weight bearing and physical therapy.38 In either case, rehabilitation focuses primarily on joint protection and the use of a semirigid orthosis.
High Ankle Sprain or Ankle Syndesmosis Injury
When the ankle is forced into dorsiflexion or rotation with the foot in a weight-bearing position, injury to the ankle syndesmosis commonly occurs. This mechanism of injury is prevalent in skiing, football, soccer, and other sport activities.68 Injury to the structures supporting the ankle syndesmosis, the anterior and posterior tibiotalar ligaments, the interosseus membrane, interosseus ligament, and the deltoid ligament, can result in an unstable distal tibiofibular articulation.68,86,89 Diagnostic testing for the high ankle sprain include the external rotation and squeeze tests, and various forms of diagnostic imaging.
Intervention
Treatment of these injuries may include immobilization, limitation of weight bearing, and surgery.68,86,89 A conservative approach to treatment and rehabilitation is necessary secondary to weight bearing being disruptive to the healing process for these ligaments. Chronic instability and arthritis commonly occur when this injury is mismanaged.89
Chronic Ankle Ligament Instabilities
The PTA, as an integral part of the rehabilitation team, must be aware of certain short- and long-term complications that may arise from acute or chronic ligament injuries of the ankle. Complications after surgical repair or conservative treatment of ankle sprains are common. Renstrom and Kannus91 report that 10% to 30% of patients have chronic symptoms of weakness, swelling, pain, and joint instability after inversion sprains. There are two types of instabilities associated with chronic ankle sprains: mechanical and functional.
Mechanical Instabilities
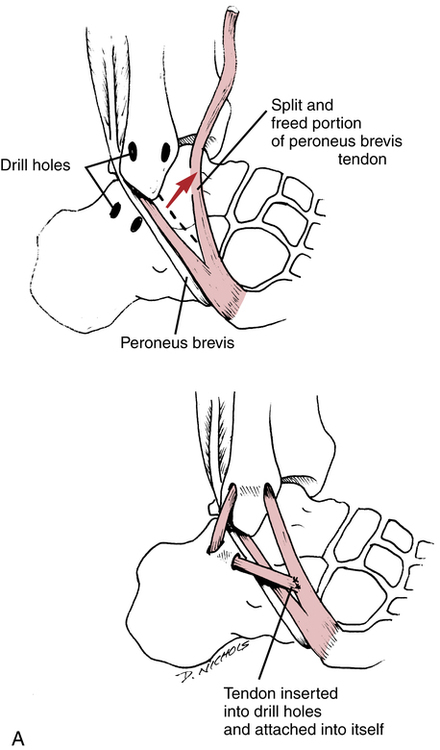
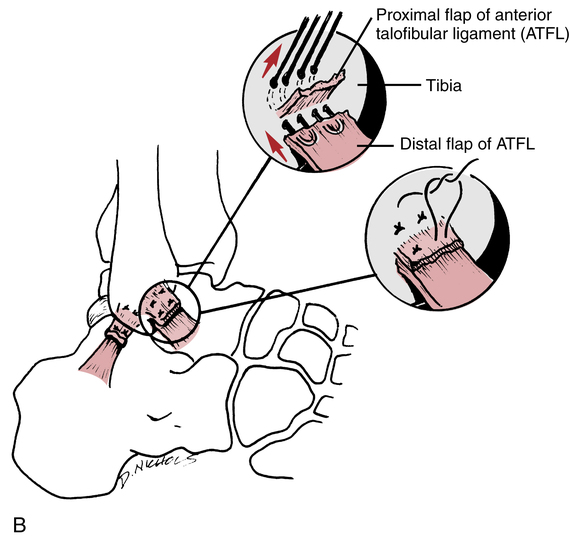
Mechanical instability is defined as laxity of the ankle ligaments. With mechanical instabilities, surgery may be necessary to stabilize the ankle joint.6 The Watson-Jones,117 Evans,30 Chrisman–Snook,17 and Elmslie17 procedures are common reconstructive surgical procedures used to help stabilize the lateral ligament complex of the ankle. In general, the peroneus brevis muscle is rerouted through a surgically constructed tunnel in the distal fibula (Fig. 17-8, A). The rerouting of the peroneus brevis dynamically stabilizes the lateral aspect of the ankle. Another method used to help stabilize chronic ligament laxity is a delayed anatomic repair of the ligaments. The ligaments are surgically cut, shortened, and reattached to the bone with this method (Fig. 17-8, B). Surgical repair has been gaining popularity among foot and ankle surgeons because of the failure of most reconstruction procedures to correct preinjury ankle biomechanics.44,70
Ankle arthroscopy has also been gaining popularity among foot and ankle surgeons secondary to the need to identify and treat intraarticular lesions at the time of surgery.21,59,70 In particular, articular cartilage lesions can be identified and treated with arthroscopy.
Functional Instabilities
Functional instability refers to a subjective feeling of giving way without affecting ligament laxity. Unlike mechanical instability, functional instability involves a host of factors, including strength, proprioception, and ligament stability. McVey and colleagues77 report that up to 40% of patients with lateral ankle instability have functional instability.
Intervention
The primary components of rehabilitation for chronic functional instabilities are closed-chain resistance exercises, proprioception maneuvers, dynamic muscular exercises (concentric and eccentric loads), and bracing for support. Single-leg support proprioception exercises with external resistance (Fig. 17-9) provide dynamic support and balance training. Balance board activities, heel-toe walking, and minitrampoline activities are the cornerstones of proprioception exercises for the ankle throughout all phases of rehabilitation for functional ankle instabilities.
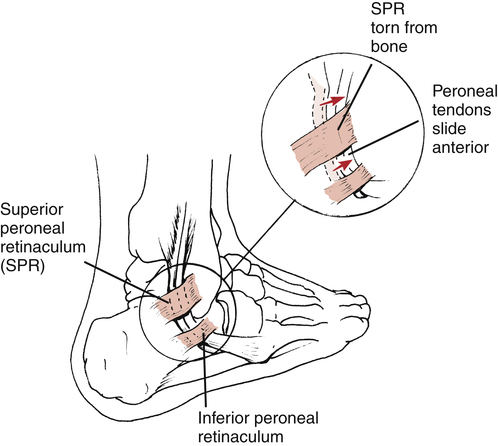
SUBLUXING PERONEAL TENDONS
The PTA must recognize that certain anatomic variations and acute injuries can result in instability of the peroneal tendons and ultimate disability. This injury is classified as acute or chronic. The mechanism of injury involves passive dorsiflexion with the foot slightly everted.27,73 Acute subluxation of the peroneal tendons can be misdiagnosed as a lateral ankle sprain because of the close anatomic proximity of the tendons to the lateral ligament complex (Fig. 17-10). Patients suffering with peroneal tendon subluxation commonly describe posterior ankle pain and may complain of a popping sensation in the lateral ankle. Active dorsiflexion with eversion of the ankle may reproduce the symptoms.41
Some patients who suffer dislocation of the peroneal tendons have a loose retinaculum (which supports the tendon within the peroneal groove) and also may have a very shallow peroneal groove.33 Acute injuries to the ankle ligaments (grades I, II, and III, using the traditional classification of sprains) may also result in injury to the peroneal retinaculum. Misdiagnosis of an ankle sprain is quite common.33 When subluxation occurs the peroneal tendons normally dislocate anteriorly over the lateral malleolus with ankle dorsiflexion.27,33,73
Intervention
Acute injuries usually are treated initially with conservative measures, including rigid-cast immobilization and NWB gait for approximately 6 weeks.33,105 Ferran and associates33 report that conservative management is successful in approximately 50% of cases. However, in some cases, patients ultimately require a surgical repair to correct the disability.55,105 Many authorities still recommend cast immobilization and NWB for 6 weeks for acute injuries, but operative care is the treatment of choice for cases involving recurrent or chronic subluxing peroneal tendons.55 Keene55 reports the five basic types of surgical repair procedures for correction of chronic subluxing peroneal tendons:
Postoperative Interventions
The postoperative care of subluxing peroneal tendons requires excellent communication among the PTA, PT, and surgeon. The exact procedure performed should be explained to the PT, who should articulate the key points of the surgery to the PTA and outline the indications and contraindications for rehabilitation. Usually postoperative care involves the use of immobilization for a few weeks and instruction in weight bearing as tolerated (WBAT). Keene55 recommends plantar flexion and dorsiflexion exercises 3 weeks after surgery. Heckman and colleagues41 suggest that patients remain non–weight bearing for 2 weeks followed by 2 to 4 weeks of immobilization in a cast or walking boot. ROM exercises are commonly initiated at 4 to 6 weeks postoperatively.
Initially, limited ROM dorsiflexion strengthening exercises should be used. As pain, swelling, and strength improve, greater degrees of dorsiflexion motion can be added. Proprioception exercises on a flat surface can be initiated soon after immobilization ends. Progression to balance board activities and minitrampoline exercises depends on the patient’s tolerance. Keene55 recommends that a running program can begin when ROM has been achieved and the involved limb reaches 80% of the strength of the noninvolved limb.
ACHILLES TENDINOPATHY
Achilles tendinopathy is an overuse injury resulting from repetitive microtrauma and accumulative overloading of the tendon (Fig. 17-11).55 The primary feature of Achilles tendinopathy is localized pain at the midportion, distal third, and insertion on the calcaneus. It should be distinguished from other similar posterior foot and ankle disorders such as retrocalcaneal bursitis and Haglund disease.101
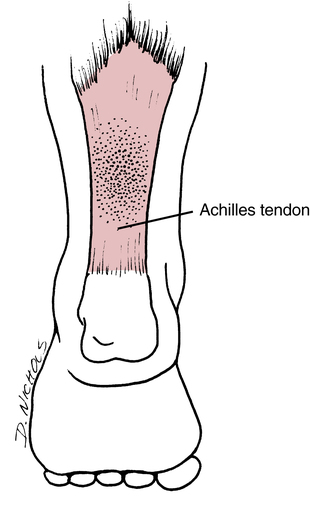
Many intrinsic and extrinsic factors can lead to Achilles tendinopathy. Decreased vascularity, malalignment of the hindfoot or forefoot, and issues with gastrocnemius–soleus flexibility are common intrinsic factors.55,101 Extrinsic factors include variations in training, running surface changes, and poor or inappropriate footwear. The general features of Achilles tendinopathy include soft-tissue swelling, pain, and crepitus.
Intervention
Ultrasound also can be used to help reduce pain and assist with collagen synthesis.50 Generally, ultrasound can be used immediately before an exercise program to improve circulation, enhance relaxation of the soft tissues, and reduce pain. Occasionally phonophoresis (ultrasound used with a topical hydrocortisone cream) is used in cases of severe pain.
Flexibility exercises are used to increase dorsiflexion motion and reduce the effects of scarring in prolonged cases of Achilles tendinopathy. Researchers have pointed out that a lack of dorsiflexion is a common denominator for patients suffering from Achilles tendinopathy.63
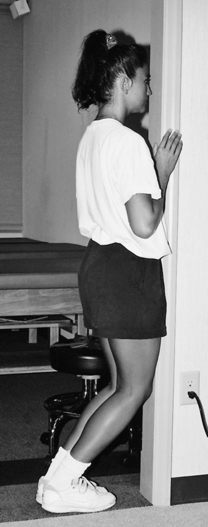
Standing heel cord stretches can be performed on a small block or with a commercial appliance to produce greater dorsiflexion motion. A soleus stretch is also used for Achilles tendinopathy. The patient faces a wall with his or her knees touching the wall while keeping the heels on the floor (Fig. 17-12).
Curwin and Stanish23 advocate eccentric strength training exercises for treatment of many types of tendinopathy. When strengthening the gastrocnemius–soleus muscle group, standing heel raises are a preferred form of exercise. The patient is instructed to rise up on the balls of the feet using the uninvolved limb, then before the descent phase, body weight is transferred to the involved limb and slowly lowered using the ipsilateral gastrocnemius–soleus muscle. Several authors have strongly advocated the use of an eccentric only strength training program for Achilles tendinopathy.3,58 Alfredson and associates3 describes excellent clinical outcomes following a 12-week eccentric strength training program for Achilles tendinopathy. In their study subjects who performed the eccentric program were able to resume running in 12 weeks, whereas those who performed a more standard concentric rehabilitation program were not able to return to running during this same time frame.3 Knobloch58 reports that “daily eccentric training for Achilles tendinopathy is a safe activity without any evidence of adverse effects in either mid-portion and insertional Achilles tendinopathy.”
In some severe cases of Achilles tendinopathy, physicians may prescribe rigid cast immobilization of the ankle for 10 days.63 The entire program of rehabilitation after cast immobilization progresses at a slightly slower rate because of the ROM and strength loss associated with immobilization. In all cases of Achilles tendinopathy, the patient is instructed in a general body fitness program. Aerobic exercise can be achieved with an upper body ergometer (UBE), seated bicycle ergometer with the seat height corrected to prevent plantar flexion, or a swimming program. Upper- and lower-body stretching and strengthening exercises are encouraged as long as the tendon suffers no undue stress or pain.
RUPTURES OF THE ACHILLES TENDON
Complete ruptures of the Achilles tendon can occur with sudden eccentric-concentric contraction of the gastrocnemius–soleus (Fig. 17-13).101 These ruptures usually involve the area “3 to 4 cm proximal to its insertion on the calcaneus, within the area of decreased vascularity” and occur mostly in men 20 to 50 years old.55,101 Racquet sports and other activities requiring a deceleration to acceleration mechanism are often the mechanism of injury. Approximately 50% of Achilles tendon ruptures are secondary to degenerative changes in the tendon.101 Corticosteroid injections or fluoroquinolone antibiotics are also responsible to weakening the tendon and predisposing an individual to rupture.101
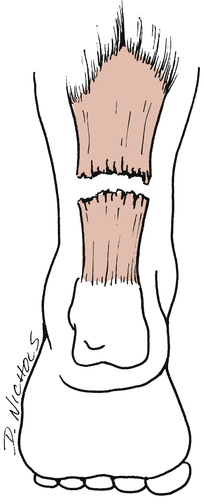
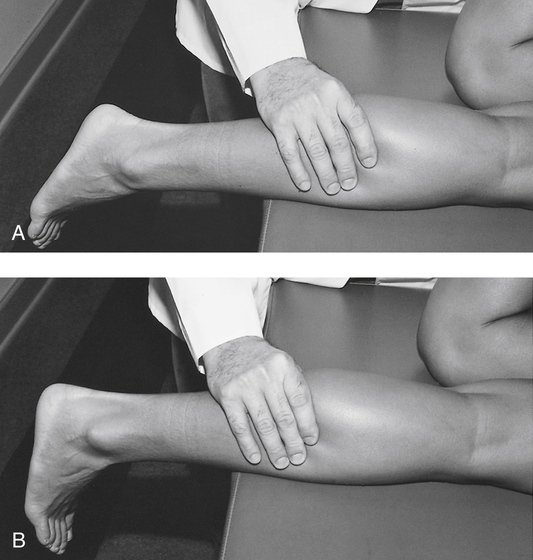
In acute Achilles tendon rupture, palpation reveals a defect or gap in the continuity of the distal third of the tendon. The Thompson test clinically assesses the integrity of the Achilles tendon. To perform this simple test, the patient lies prone on an examining table with the feet extending off the end. The entire lower leg is exposed, from knee to toes. The belly of the calf of the uninvolved limb is grasped and squeezed so that the foot plantar flexes. If the tendon is ruptured on the involved limb when the calf is squeezed, no plantar flexion motion results (Fig. 17-14).
Intervention
A ruptured Achilles tendon can be treated surgically or with cast immobilization.57,101 Nonoperative treatment of Achilles tendon ruptures requires the patient to be immobilized for as long as 8 weeks.55,57,101 However, with nonoperative treatment, researchers have documented rerupture rates of 8% to 39%.9,30,52,57 In addition, there is a greater loss of strength, power, and endurance compared with surgically repaired tendons.9,49,52,55 Surgically repaired Achilles tendons have a much lower rate of rerupture (0% to 5%), and there is a significant increase in the ultimate recovery of muscular strength, power, and endurance.57 However, Nistor85 reports only minor differences between surgical and nonsurgical management. Some surgeons85 prefer nonoperative management because there are fewer complications related to surgery, reduced complaints, no hospitalization, and no significant differences in function compared with surgically treated patients. There are numerous surgical techniques used to repair acute Achilles tendon ruptures, including end-to-end primary repair and direct repair and augmentation with tendon or synthetic grafts.∗
Regaining full dorsiflexion and plantar flexion motion is an exceedingly slow process after cast removal. Gentle active dorsiflexion and plantar flexion exercises are initiated immediately. Typically, a small heel-lift is used in everyday shoes to minimize stress on the healing tendon. Because the tendon was not surgically repaired, the process of regaining tensile strength and collagen alignment must be approached cautiously. Progressive active motion is an essential component for full return to function. However, if the tendon is stressed too soon or vigorously, it may rerupture. The heel-lift is commonly worn for 3 to 4 weeks and gradually reduced in size to prevent sudden excessive stress on the tendon.55
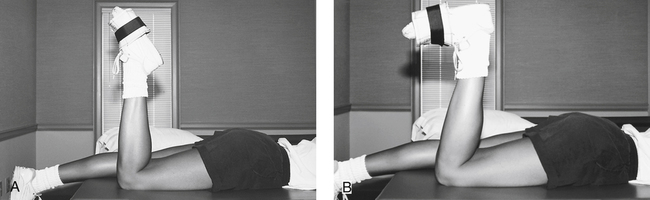
Progressive plantar flexion and dorsiflexion exercises using a latex band are encouraged as pain and motion allow. Proprioception exercises can be employed early, depending on the patient’s tolerance. Generally, proprioception exercises begin with the patient in a seated position (Fig. 17-15) and progress as tolerated. If rerupture occurs, it is usually within 4 weeks after immobilization.55 During this maximum-protection phase, the patient is encouraged to avoid sudden forceful plantar flexion or dorsiflexion motions.
Weight-bearing plantar flexion can begin gradually once the patient has successfully completed the prescribed program of ROM and strengthening exercises without complications. Standing plantar flexion is initiated without a block to stand on. The patient is instructed to gradually rise up on the toes using primarily the uninvolved limb, then lowers himself or herself using both feet. As strength improves, the patient gradually uses more of the involved limb to rise up on the balls of the feet. Adding a small block of wood on which to rise adds greater dorsiflexion stress and motion. Seated calf raises can be performed by modifying a leg extension machine (Fig. 17-16). The seated position may be more comfortable initially.
Rehabilitation following surgical repair or reconstruction of the Achilles tendon is quite variable. Secondary to the large number of procedures available, the timing of the surgery (acute vs. chronic), stability of the repair/reconstruction, and intrinsic patient variables the rehabilitation progression may be different from surgeon to surgeon, and patient to patient. In particular the surgical variations are numerous with each having differing needs for immobilization and restriction of weight bearing during the immediate postoperative period. Variables such as ROM, weight bearing, and initiation of strength training are determined by the surgeon. Therefore each individual should be rehabilitated independently.∗
Generally, rehabilitation following Achilles tendon repair or reconstruction follows a criteria-based rehabilitation program as described previously. Following a period of immobilization a gradual progression of weight bearing and ROM is pursued. Normally plantar flexion is less restricted than dorsiflexion during the early postoperative period. Strength training can begin as early as 2 to 4 weeks postimmobilization.55
Secondary to the large differences in Achilles tendon surgery and rehabilitation programs the return to full activity is also variable. At least one author believes that successful outcomes are dependent on tendon elongation. Kannas and Renstrom54 report that improved outcomes occur when less elongation of the Achilles tendon occurs. Therefore symmetric ankle dorsiflexion ROM is a goal of treatment, and increased dorsiflexion beyond the contralateral side is discouraged. Generally most patients are able to return to full activity within 6 to 9 months. Surgical complications following Achilles tendon repair or reconstruction include sural nerve dysfunction, infection, skin sensitivity, adhesions, rerupture, and tendon necrosis.57,61 The vast majority of patients appear to be satisfied with their results.2,29,48,57,88
COMPARTMENT SYNDROMES
Compartment syndromes of the lower leg are defined as either acute or chronic elevated tissue pressure within a closed fascial space, resulting in occlusion of vessels and compromised neuromuscular function.4,35,93
Acute compartment syndromes of the leg are most commonly associated with tibial fractures, direct trauma to the area, muscle rupture, muscle hypertrophy, and circumferential burns.62,91 Acute elevated intracompartmental pressure within the lower leg is considered a medical emergency.35
Chronic compartment syndromes also are referred to as exertional compartment syndrome or exercise-induced compartment syndrome. Muscular contractions and exertion have been shown to cause increases in muscle size, leading to increased intracompartmental pressure.62,91 This results in ischemia and reduced neuromuscular function. To understand this series of events, it is necessary to review pertinent anatomy of the lower leg.
There are four well-defined compartments of the leg, divided by nonyielding fascia.4,93 The anterior compartment of the lower leg contains the tibialis anterior muscle, anterior tibial artery and vein, and foot and toe extensor muscles. The lateral compartment contains the superficial peroneal nerve and short and long peroneal muscles. The superficial posterior compartment contains the soleus muscle and plantaris and gastrocnemius tendons. The deep posterior compartment contains the posterior tibialis muscle, the peroneal artery and vein, tibial nerve, and posterior tibial artery and vein. If swelling occurs in one or more of these compartments, reduced capillary blood perfusion results in neurovascular and muscular dysfunction.
Clinical symptoms of acute compartment syndrome include pain, palpable swelling or tenseness, and paresthesias.4,93 The skin may be warm, shiny, and tense. Passive stretching of the muscles of the lower leg may produce severe pain.
Intervention
Acute compartment syndrome is treated with a surgical procedure called a fasciotomy.4,93 When nerve and muscle ischemia last longer than 12 hours, severe and irreversible damage occurs.4 If, however, the ischemia can be reduced in less than 4 hours, usually no permanent damage occurs.4
A surgical fasciotomy is designed to relieve intracompartmental pressure by opening or releasing the fascial compartment, thus allowing the pressure to be reduced. It is interesting to note that the surgical incision is sometimes left open and is managed with sterile dressings.4 Recently, less invasive techniques such as endoscopy have been utilized.120 Immediately after surgery, ice packs and leg elevation are necessary to reduce swelling. Walking as tolerated and active and passive gentle ROM of the ankle and knee are begun 2 days after surgery. Early ROM is crucial in order to prevent contractures. Treatment with ice and leg elevation is continued after exercise. A general conditioning program can begin with strengthening exercises and aerobic exercises using a single-leg ergometer or UBE. Once the patient shows improved motion and reduced pain and swelling, light resistance exercises can begin for the involved leg. Close attention should be paid to foot structure because contractures may develop postsurgery, resulting in varying levels of equinus deformity in the foot.109 However, very light resistance should be encouraged because heavy and intense exercise, which leads to muscular hypertrophy, is contraindicated after fasciotomy for acute compartment syndromes.
The management of chronic exercise-induced compartment syndromes is similar to that of acute compartment syndromes. However, chronic compartment syndromes do not always represent a surgical emergency. Conservative management should include relative rest, antiinflammatory drugs, stretching and strengthening of the involved muscles, and foot orthotic devices (if appropriate).118 Subcutaneous fasciotomy should be used only when pain and symptoms affect function. The postoperative management of fasciotomy after chronic compartment syndromes parallels the rehabilitation program outlined for acute compartment syndromes.
ANKLE FRACTURES
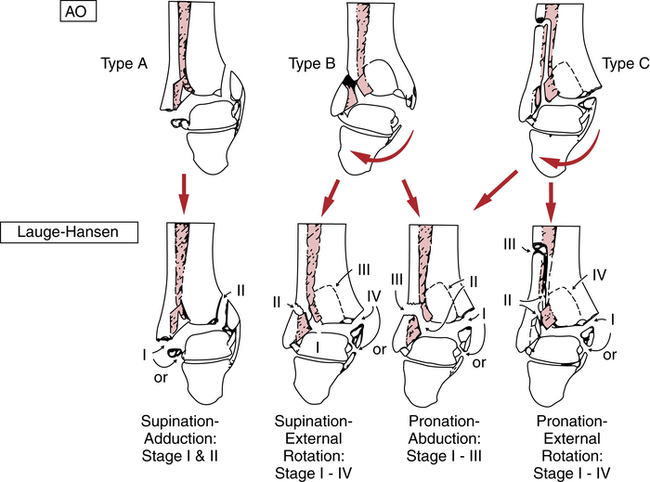
The most widely accepted classification of ankle fractures is called the Lauge–Hansen classification.76 Another type of classification, called AO, is based on principles, which are similar to, though slightly different from, the Lauge-Hansen (Fig. 17-7). The organization and classification of ankle fractures frequently involve the direction of force, which results in specific patterns of injury. For example, a Lauge–Hansen pronation-abduction or pronation–lateral rotation injury may result in a malleolar or bimalleolar fracture of the ankle (Fig. 17-18).
Ankle fractures include lateral malleolar fractures, medial malleolar fractures, bimalleolar fractures (combined medial and lateral malleolar fractures), and trimalleolar fractures (bimalleolar fractures plus the posterior margin of the tibia). Though simple malleolar fractures are managed initially with immobilization, many fractures are managed with an open reduction with internal fixation (ORIF) procedures. Typically, these fractures are fixed with various screws and plates to hold the fragments in place (Fig. 17-19).
A walking cast is applied once the patient achieves full plantar flexion and dorsiflexion ROM. Before casting, the surgical wound must be fully closed, sutures removed, infection absent, and no drainage present. A general full-body conditioning program is prescribed throughout immobilization. Both aerobic fitness and strengthening exercises are advocated also. Further, strengthening of the uninjured limb has shown beneficial crossover results in strength of the injured limb.114
Distal Tibia Compression Fractures (Pilon Fractures)
Distal tibia compression fractures (pilon fractures) occur as a result of vertical or axial loads that drive, or compress, the tibia into the talus. The initial management of these injuries usually involves an ORIF procedure, external fixation, or skeletal traction with a calcaneal pin.76 If the fracture was managed with external fixation, special attention should be given to these individuals because malunion is more common with this type of fixation.90 Because of the nature of these fractures, weight-bearing activities usually are deferred for as long as 12 or more weeks. Weight bearing creates vertical compression and compromises the natural course of healing needed for a stable outcome. Secondary osteoarthritis is a common complication with severe multifragmented compression fractures.76 Typically throughout immobilization, a general conditioning program is allowed as long as no weight bearing occurs.
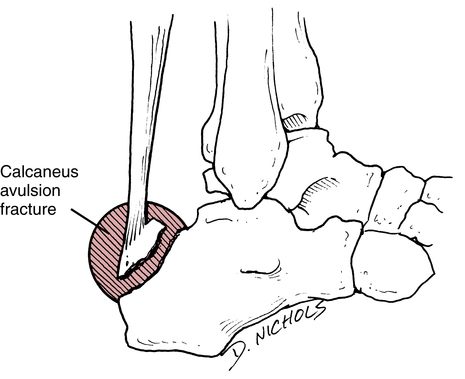
Calcaneal Fractures
Calcaneal fractures are intraarticular depression fractures usually caused by falls from a height and resulting in compression of the calcaneus from the talus (Fig. 17-20). McRae76 describes seven common patterns of calcaneal fractures:
1. Vertical fractures of the calcaneal tuberosity
3. Fractures of the sustentaculum tali
4. Anterior calcaneal fractures
5. Fracture of the body of the calcaneus without involvement of the subtalar joint
6. Calcaneal fractures with lateral displacement and involvement of the subtalar joint
Each calcaneal fracture type has individual characteristics that allow the physician to determine the treatment options and the rehabilitation progression. Both conservative (casting) and surgical (ORIF) procedures are used with calcaneus fractures.76 As with all fractures, specific rehabilitation procedures should be cleared by the physician before initiation. When possible early ROM activity is used in rehabilitation to reduce stiffness and prevent long-term ROM loss. Weight-bearing status; active, passive and resisted ROM; and functional progression should be determined by the physician throughout rehabilitation. Supportive measures to control pain and swelling are used as necessary.
In the long term, the cornerstone in recovering from a calcaneal fracture lies in regaining motion and strengthening the plantar flexors. Multiangle isometric plantar flexion can be initiated and progressed to full ROM manual resistance dorsiflexion and plantar flexion. The use of latex rubber tubing and bands for plantar flexion in a long-seated position is an appropriate and challenging calf-strengthening exercise during the moderate-protection phase of rehabilitation. Strengthening of the soleus can be achieved by having the patient lie prone with the affected leg flexed 90° at the knee and placing ankle weights around the foot of the affected leg (Fig. 17-21).
Fractures of the Talus
The talus can be fractured by falling from a height and landing on the foot in a crouched position.76 This produces an axial compression load between the talus and calcaneus. There are four classifications of talar fractures76:
 Type I: Talar neck fracture without displacement
Type I: Talar neck fracture without displacement
 Type II: Talar fracture with subtalar subluxation (the incidence of avascular necrosis is as high as 50%)76
Type II: Talar fracture with subtalar subluxation (the incidence of avascular necrosis is as high as 50%)76
 Type III: Talar fracture with further subtalar subluxation (the incidence of avascular necrosis is as high as 85%)76
Type III: Talar fracture with further subtalar subluxation (the incidence of avascular necrosis is as high as 85%)76
 Type IV: The talar head dislocates from the navicular in association with a type III injury
Type IV: The talar head dislocates from the navicular in association with a type III injury
STRESS FRACTURES OF THE FOOT AND ANKLE
The development of stress fractures can be viewed in part as resulting from a linear progression or continuum of excessive external forces that lead to intrinsic reactions of muscle, bone, and periosteum. For example, with increased muscular forces resulting from continued and excessive use (marathon running, recreational jogging, aerobic dance, or occupations that require standing or walking all day) there is an associated increased rate of bone remodeling around the area of increased stress.102 If the stress is not removed, this increase in bone remodeling is followed by a greater rate of bone resorption. If the stress continues, the bone eventually responds by developing microfractures, periosteal inflammation, and resultant stress fractures.102 If stressed further, and the bone and soft tissues are not allowed to recover fully and heal properly, the development of linear fractures and ultimately displaced fractures can occur.102
There are certain stress fractures that pose a greater risk of delayed union, nonunion, and displacement than others.74 The base or proximal diaphysis of the fifth metatarsal is described as “no-man’s-land” and is “at risk” for delayed union or nonunion after a stress fracture.74,91 Usually, complete rigid-cast immobilization is indicated for 6 to 8 weeks when conservative, relative rest has failed to arrest symptoms of pain.74,91,92 Other stress fractures termed at risk22 are tarsal navicular fracture, sesamoid fractures, and all intraarticular fractures.
The management of not-at-risk74 stress fractures of the foot and ankle can be effectively rehabilitated with activity modification; relative rest; therapeutic agents to relieve pain and swelling; and specific leg, ankle, and foot stretching and strengthening exercises. Low-impact aerobic exercise is useful in athletic patients who are extremely active. For example, instead of running, the patient can use a stationary cycle, recumbent cycle, elliptical trainer or run in a NWB manner under water.
For stress fractures of the foot and ankle that are at risk74 (fifth metatarsal, navicular, sesamoids, and intraarticular fractures), more caution is necessary during the advancement of closed-chain activities to protect the healing bone from unwanted forces. With at-risk stress fractures, some form of external support can be used to brace the area. Usually some type of bracing, padding, casting, or orthosis is applied to control stress and forces to the healing bone.74 The application of therapeutic exercises must be approached cautiously. Submaximal isometric exercises are encouraged initially. AROM and light concentric and eccentric loads are added as pain allows. Obviously, vertical compressive loads and shearing forces (i.e., jumping, running, cutting) are strictly prohibited to allow proper healing. Modifications in aerobic activity and general physical conditioning can allow the patient to continue to participate in strenuous physical conditioning, provided no stress is applied to the healing tissues. The initiation of closed-chain functional activities must be deferred until radiographic confirmation by the physician documents stable bone healing.
MEDIAL TIBIAL STRESS SYNDROME
Musculoskeletal overuse injuries of the lower leg involving the distal third of the posterior medial border of the tibia have historically been referred to as shin splints. This term has no place in orthopedic management and should be discarded as a nonspecific term used to describe any pain occurring in the lower leg.4 A more precise and descriptive term is medial tibial stress syndrome (MTSS), which describes pain over the distal and middle thirds of the tibia along the posterior medial border.10 Differential assessment by the physician and PT includes stress fractures of the tibia and fibula, ischemic disorders, and deep compartment syndromes of the lower leg.
The predominant feature of MTSS is tenderness over the distal, posteromedial tibia.80 Traditionally a number of different structures are thought to cause these symptoms. Musculotendinous inflammation, periosteal inflammation of the muscle–tendon–bone interface at the posterior medial border of the tibia, injury to the tibia bone, the posterior tibialis muscle, and the medial origin of the soleus muscle have been identified as a primary source of pain in patients with MTSS.4,7,25,78 More recent work has noted that a primary source of symptoms with MTSS is the tibial bone.72,80
Several studies have attempted to determine the etiology of MTSS.8,28,46,80,112,121 Intrinsic factors for MTSS include overpronation of the foot, female sex, high body mass index, hip ROM (internal and external rotation), and ankle ROM loss (dorsiflexion). Hubbard and colleagues46 report that a previous history of MTSS, previous history of stress fracture, and less than 5 years of experience in a sport predispose an athlete to MTSS. Runners, basketball and volleyball players, tennis players, and military recruits have a greater incidence of MTSS.28,80 Diagnosis of MTSS is primarily made on physical exam, but diagnostic imaging including plain film radiographs, bone scans, dual energy x-ray absorptiometry (DEXA) scans, and magnetic resonance imaging (MRI) are also used.72,80
Because pain is the predominant feature of MTSS, it is helpful to classify and describe the severity of pain related to the patient’s ability to perform activities.51 Grade I describes pain that is experienced after activities. Grade II defines pain felt both during and after activities that does not affect the actual performance of activities. Grade III pain is felt before, during, and after activities and affects the patient’s ability to perform activities. Grade IV pain is so significant that no activities can even be attempted.
Currently there is evidence to support the use of relative rest, foot orthotic devices, and stretching to improve symptoms in patients with MTSS.80,112 However, a multimodal approach utilizing mechanical and therapeutic approaches appears to be most beneficial with this disorder.28
PLANTAR FASCIITIS (HEEL SPUR SYNDROME)
Chronic inflammation of the plantar aponeurosis, with or without an associated calcaneal heel spur, is called plantar fasciitis (Fig. 17-22). Leach and co-workers65 describe plantar fasciitis as repetitive microtrauma leading to injury, attempted repair, and chronic inflammation. Brody13 describes plantar fasciitis as an “inflammatory reaction due to chronic traction on the plantar aponeurosis (fascia) at its insertion into the calcaneus.”
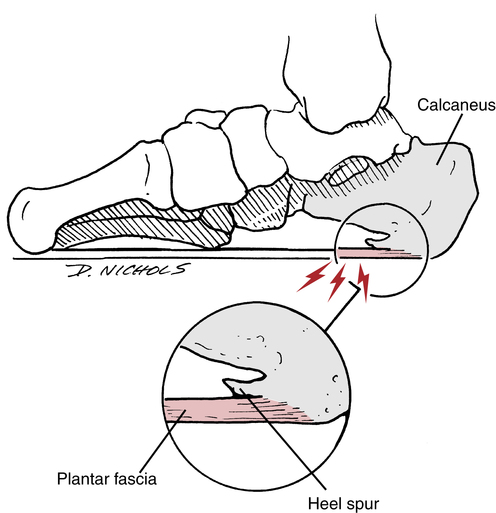
Although most authors and clinicians believe this pathology is an inflammation of the plantar fascia there are several authors who describe this disorder as a plantar fasciopathy or plantar fasciosis.67,94 These authors believe that the pathology can be degenerative as well as inflammatory in nature, depending on the chronicity of the pathology. The same issue has been discussed with other overuse tendon injuries.
Patients with plantar fasciitis frequently complain of pain along the medial border of the calcaneus on the plantar surface. Many patients report that pain is worse in the morning when the foot contacts the floor in getting out of bed. Palpation of the plantar fascia usually reveals tenderness at the medial tuberosity of the os calcis or throughout the entire course of the fascia.4 Palpation is performed with the toes flexed, which reduces tension on the fascia, or with the toes extended, which increases tension on the fascia.11 Dorsiflexion of the ankle may also provoke symptoms.16
Intervention
Many patients respond well to conservative physical therapy procedures.83,94 Relative rest, stretching, manual therapy, exercise, iontophoresis, arch taping, and foot orthotic devices have been shown to improve symptoms and function in patients with plantar fasciitis.∗ A specific physical therapy approach where the clinician treats impairments, functional limitations, and disabilities with interventions designed to improve each item observed in the examination appears to have the greatest impact on patients with plantar fasciitis.75
Specifically addressing ROM deficits at the ankle joint (dorsiflexion) with manual therapy and stretching exercises appears to be helpful in these patients. If indicated, both the gastrocnemius and soleus muscles should be stretched. However, if stretching of the gastrocnemius or soleus is painful in the area of the plantar fascia the clinician may want to decrease this activity.16 In the author’s experience if arch taping is helpful in reducing symptoms use of an over-the-counter foot orthotic device may be helpful. Custom-made foot orthotic devices may also be used in selected patients. In particular those patients who have a large arch deformity and did not respond favorably to an over the counter device may be good candidates for a custom-made foot orthoses.
Strength training for the musculature in the foot and lower leg may be indicated if specific weaknesses are observed during the examination. Inversion, eversion, dorsiflexion, and/or plantar flexion strength training is necessary when weakness occurs. Strength training for the intrinsic musculature in the foot may also be necessary. Activities such as toe curls, picking up marbles with the toes, or gripping a towel can be used to strengthen the foot intrinsic musculature (Fig. 17-23).
Extracorporeal shockwave therapy has been used for several years to assist in the healing process in patient with plantar fasciitis. This modality attempts to break up adhesions and improve soft tissue extensibility of the plantar fascia. Several authors have shown good results with this form of treatment.94,110,116
With some patients who do not respond to conservative therapy, the physician may decide to correct the problem surgically. Surgical options include plantar fascia release (fasciotomy) and partial plantar fascia release. Rompe94 states that conservative management is the first and best option, and should last approximately 6 months before other forms of treatment. If conservative management fails, then surgery is the next option.
ARCH DEFORMITIES (PES PLANUS AND PES CAVUS)
Pes planus (flatfoot) is a congenital or acquired deformity of the foot where the medial longitudinal arch of the foot is reduced, causing the medial border of the foot to contact the ground when a person is standing.71 The usual cause of acquired pes planus is muscular weakness, laxity of ligaments that support the medial longitudinal arch, paralysis, or a pronated foot.71 Pes planus deformity can be classified as mild, moderate, or severe.81
During the initial evaluation, the PT measures the degree of hindfoot and forefoot alignment in NWB. The hindfoot alignment is defined as the longitudinal bisection of the calcaneus relative to the long axis of the lower leg, and the forefoot alignment is defined as the metatarsal alignment relative to the perpendicular of the longitudinal bisection of the calcaneus. If the plantar surface of the distal segment is medial relative to the proximal segment, this is defined as a varus alignment. If the plantar surface of the distal segment is lateral relative to the proximal segment, this is defined as a valgus alignment. In addition, the PT assesses the deformity in a weight-bearing position.92 With a rigid pes planus deformity, the foot appears to have an abnormally low arch in both weight-bearing and NWB positions.92 With a flexible pes planus deformity, the foot appears to have a normal arch in a NWB position, but an abnormally low or flat arch in weight bearing.
No specific therapeutic interventions are necessary if there is no associated pain or dysfunction. However, because the area is a terminal component of the closed kinetic chain during weight bearing (the arch can affect the knee, hip, and spine in a closed kinetic chain), treatment that is specific to the arch may be indicated if associated pain and dysfunction are experienced in other joints along the kinetic chain. For example, pes planus can affect the normal neutral-to-pronation sequence of the foot during the gait cycle. Because the foot is already pronated (with pes planus), the reduced normalized motion from neutral to pronation is affected during gait. Therefore the knee and other joints along the kinetic chain must compensate for this reduced motion. If pain and resultant dysfunction occur in one or more of these associated joints, then corrective action is necessary to place the foot in a more neutral position to enhance the normal physiologic motion of the entire kinetic chain. Injuries common to those with pes planus occur more often to medial soft tissue structures of the knee.119
Usually the use of a custom-fabricated foot orthotic device is indicated to create a more normal mechanical arch. Materials used to fabricate foot orthotic devices include cork, leather, rubber, foam, felt, and plastic.18 The rationale for the use of a custom-molded foot orthotic device to correct a symptomatic pes planus is supported in the literature.24 Further, successful treatment of other lower extremity injuries commonly attributed to pes planus have been documented.37 However, individual consideration should be given to each patient for prescription foot orthoses as lower extremity overuse injuries are always multifactorial.84
Pes cavus, on the other hand, describes an abnormally high arch.71,91 Pes cavus usually is a result of neurogenic pathologic processes, muscle imbalances, and congenital abnormalities; both medial and lateral longitudinal arches can be affected. Clinically, patients may complain of painful calluses beneath the metatarsal heads because of the mechanical friction and pressure that occur with metatarsal heads. Osteoarthritic changes are not uncommon in the tarsal area because of the altered biomechanics of the foot. Mechanical compensation at proximal joints in the lower extremity is also common with injuries being more common to lateral bony structure of the foot and lower leg.119
Treatment for pes cavus is much more challenging than for pes planus and should be focused on pain and shock attenuation. Recent evidence supports the effectiveness of custom-made foot orthoses for treatment of pain related to pes cavus. 40 No treatment is indicated if no symptoms exist, although the PT may document this deformity during a lower-quarter evaluation.
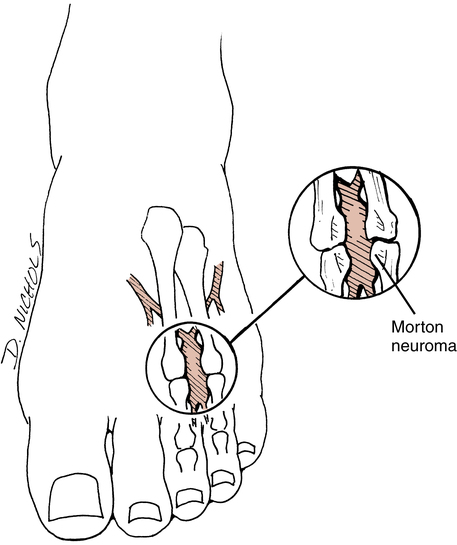
MORTON NEUROMA (PLANTAR INTERDIGITAL NEUROMA)
Patients with a neuroma may complain of diffuse, occasionally radiating pain into the toes and proximally to the dorsal or plantar surface of the foot.22 A neuroma usually occurs at the 3-4 interspace and less frequently at the 2-3 interspace (Fig. 17-24).79 Morton neuroma occurs bilaterally only 15% of the time, with the patient complaining of a burning, cramping, or catching sensation.22,79 A painful mass can be palpated in approximately one third of the cases.79
Intervention
Conservative care calls for the use of a metatarsal pad; change of footwear to a wider, softer shoe; and local corticosteroid injections. Surgical excision of the neuroma may be necessary when all attempts at conservative care fail to relieve pain. However, success of the surgical technique is around 83%.39
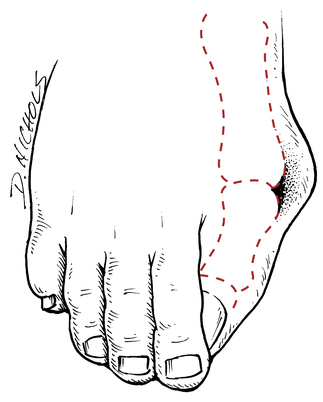
HALLUX VALGUS
Hallux valgus is a lateral or valgus deviation of the great toe with both soft tissue and bony deformity (Fig. 17-25). This condition can be exacerbated by improper footwear (narrow toe box), and often the associated pain can be relieved by modifying or changing poor footwear. Examination should include assessment of the deformity in a standing position, which often accentuates the deformity,22,79 and measurement of the hallux valgus angle (normal is <15 degrees) to determine the degree of deformity and angle of deviation. Hallux valgus is often associated with hallux rigidus. Therefore, first metatarsal phalangeal joint extension ROM should also be assessed. Further, it has been suggested that abnormal pronation is associated with the development of hallux valgus.96
LESSER TOE DEFORMITIES (HAMMER TOES, MALLET TOES, AND CLAW TOES)
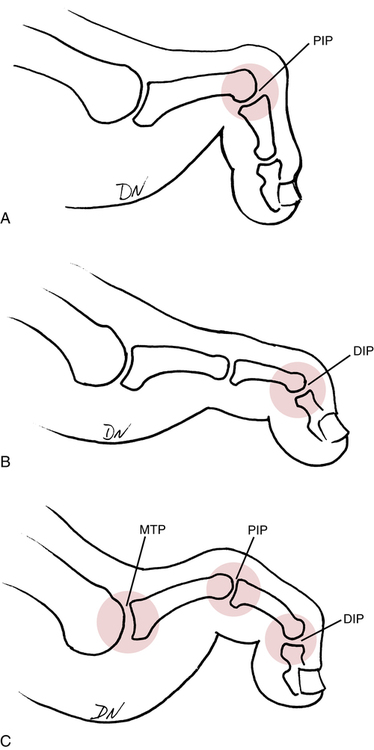
Three distinct types of lesser toe deformities are hammer toes, mallet toes, and claw toes (Fig 17-26). All three deformities are worsened by wearing improper shoes (narrow toe box).
Hammer toe (see Fig. 17-26, A) is characterized by deformity of the metatarsophalangeal (MTP) joint, proximal interphalangeal (PIP) joint, and distal interphalangeal (DIP) joint. The MTP joint is either in neutral position or extension. The PIP joint is held in flexion with the DIP joint in either flexion or extension.
Mallet toe (see Fig. 17-26, B) is characterized by a neutral MTP joint, a neutral PIP joint, and a flexed DIP joint.
Claw toes (see Fig. 17-26, C) often are associated with neuromuscular disease and are similar in appearance to hammer toes. Claw toes are distinguished by MTP hyperextension, PIP flexion, and DIP flexion. This deformity usually results from “simultaneous contraction of the extensors and flexors.”79
Intervention
Surgical repair is reserved for fixed or rigid deformities, although some flexible deformities also require operation. Typically, sutures and pins are removed about 3 weeks after surgery.22 The patient is WBAT initially, with a progression to FWB as pain allows. The affected extremity is held in a rigid-solid open-toe postsurgical boot to protect the repair from unwanted excessive flexion and extension of the toes.
Once the pins and sutures are removed at 3 weeks, physical therapy management can begin. Ultrasound, AROM, and gentle stretching and strengthening exercises (open-chain progressing to closed-chain toe curls with a towel or marbles) can be employed. The toes must be protected from unwanted stress throughout the maximum-protection phase (6 to 8 weeks after surgery) of rehabilitation. Coughlin22 recommends avoiding all running activities for 9 to 12 weeks after surgery to allow for proper healing.
COMMON MOBILIZATION TECHNIQUES FOR THE ANKLE, FOOT, AND TOES
Ankle Mobilization
Anterior and posterior glides are best performed with the patient in a supine or long-sitting position with the lower leg firmly and comfortably supported. For anterior glide of the calcaneus, the hand position, stabilization, and direction of force are similar to those for the anterior drawer test for ligament stability testing of the anterior talofibular ligament. One hand should be placed firmly on the distal anterior surface of the tibia and fibula. The application hand should be used to firmly cup the calcaneus and provide an anterior-directed force (Fig. 17-27).

The posterior glide technique is performed with the patient in the same position as the anterior glide. The distal tibia and fibula should be stabilized with the palm of one hand. The application hand should be placed on the dorsal surface of the talus to provide a posterior-directed force (Fig. 17-28).

Traction is achieved through long-axis distraction of the talus caudally from the tibia and fibula. The patient can be supine or prone with the lower leg firmly and comfortably supported. The dorsal surface of the talus should be firmly grasped with the open palm of one hand, while the other hand is used to firmly grasp and cup the calcaneus. The force should be applied simultaneously with both hands along the long axis of the tibia and fibula (Fig. 17-29), effectively distracting the talus from the mortise.

Metatarsal Mobilization
Distal metatarsal glides are performed while the patient is supine with the lower leg supported. The hand, thumb, and fingers of one hand should be used to stabilize the ray of the second metatarsal while the hand, thumb, and fingers of the application hand firmly grasp the first ray at the metatarsal head. Force should be applied in a plantar and dorsal direction (Fig. 17-30).

Proximal Interphalangeal Joint Mobilization
Long-axis distraction of the PIP joint is achieved by stabilizing the affected metatarsal ray with one hand while using the application hand to firmly grasp the affected phalanx. The thumb and fingers apply long-axis traction (distraction) (Fig. 17-31).
Plantar and dorsal PIP glides are performed with the patient supine and the lower leg supported. One hand should be used to firmly grasp the first metatarsal ray at the metatarsal head. The thumb of the stabilizing hand must be placed on the dorsal surface of the metatarsal head. The application hand should be used to grasp the proximal phalanx and apply a plantar and dorsal force while stabilizing the metatarsal head (Fig. 17-32).
GLOSSARY
Posterior tibialis tendon Rupture results in planovalgus, or flatfoot.
Syndesmosis Ligaments responsible for maintaining stability of the distal tibiofibular articulation.
Talus No muscle attachment origin or insertion. Has a tenuous blood supply.
∗For more information on these techniques, please refer to the articles found in references 5, 19, 26, 66, 75, 82, 87, 95, 116, and 122.
∗For more information on these techniques, please refer to the articles found in references 2, 15, 29, 36, 42, 45, 47, 48, 53, 55, 57, 60, 61, 69, 88, 99, 100, 102, 103, 111, and 113.
∗For more information on these techniques, please refer to the articles found in references 5, 19, 26, 66, 75, 82, 87, 95, 116, and 122.