Chapter 3. Orthopaedic anatomy
By the end of this chapter you should:
• Be able to identify different types of joint in the body.
• Understand collagen and its function and how this relates to motion/wear.
• Understand the effect of muscles on fractures and the displacement caused.
• Be aware of neurovascular injuries and know which nerves are commonly injured and where.
Joints
Types of joint
First, remember that synovial joints are just one type of joint and that the fibrous and cartilaginous types are just as important.
Synovial joints
The shoulder, elbow, hip, knee and ankle are all synovial joints lined by synovium, which secretes synovial fluid. The articular surfaces are covered with smooth hyaline articular cartilage and movement is determined by the shape of the bones, ligaments, surrounding soft tissues and the joint capsule, which contains the proprioceptors which form the afferent segment of postural reflexes.
Synovial joints can be classified according to shape and the movement that occurs between the bones. Ball and socket joints such as the hip (Fig. 3.1) and shoulder allow movement in all planes, but a hinge joint such as the knee allows movement in one plane only. Condyloid joints such as the radiocarpal joint are elliptical and allow movement in two planes, whereas pivot, or peg, joints such as the superior radioulnar and atlantoaxial joints allow movement about one axis only (Fig. 3.2).
 |
| Fig. 3.1
A ball and socket joint. The ball of the femoral head is enclosed by the cup of the acetabulum.
|
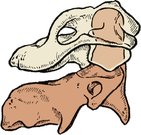 |
| Fig. 3.2
A peg joint. The atlas can pivot on the axis.
|
Some joints, such as the patellofemoral joint, have a very large range of movement (Fig. 3.3), but others have much less. The small bones of the tarsus, for example, are linked by plane joints with so little movement that groups of joints must work together to permit a useful range of motion.
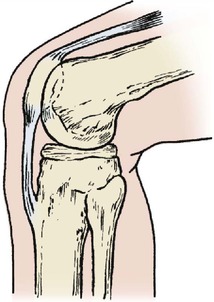 |
| Fig. 3.3
The knee is a hinge joint but the patellofemoral joint is a sliding joint.
|
The posterior intervertebral, or facet, joints are also plane joints, as is the sacroiliac joint.
Other joints are more complex and more interesting mechanically. The first carpometacarpal joint is saddle-shaped and similar to a universal joint in design (Fig. 3.4). Other joints work in pairs, including the superior and inferior radioulnar joints, which function as a single unit with two bones moving about an axis that passes through the centre of each (Fig. 3.5). The tibiofibular joints are similar; movement of the ankle produces movement at the superior tibiofibular joint (try it on your own leg). The subtalar joint also consists of two separate articulations between the same two bones, one convex upwards and the other convex downwards, but movement occurs about an oblique axis which does not pass through the articular surface of either.
 |
| Fig. 3.4
A ‘universal’ joint. The first carpometacarpal joint has two saddle-shaped joint surfaces.
|
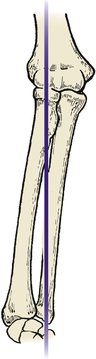 |
| Fig. 3.5
Paired joints. The axis of pronation and supination of the forearm runs through the proximal and distal radioulnar joints.
|
Cartilage joints
There are two types of cartilage joints: primary, or synchondroses, and secondary, or symphyses (Fig. 3.6). Synchondroses link immature growing bone at the epiphyses in children and have no movement. Symphyses, which are only found in the midline of the body, have a mass of fibrocartilage linking the bones instead of a synovial cavity. The pubic symphysis is the best known but the intervertebral joints with their intervertebral discs and the manubriosternal joint are also symphyses.
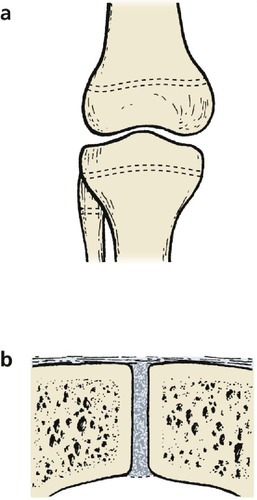 |
| Fig. 3.6
Cartilage joints. (a) Synchondroses at the growing ends of long bones; (b) a symphysis between the two halves of the pubis.
|
Fibrous joints
The flat bones of the skull are linked at the suture lines by fibrous tissue, which prevents any appreciable movement. These linkages are, strictly speaking, joints, but their function is to limit movement rather than encourage it. The inferior tibiofibular joint is the largest syndesmosis in the body and is important for the stability of the ankle (Fig. 3.7).
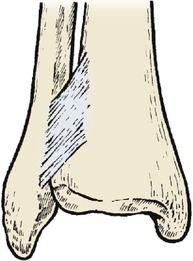 |
| Fig. 3.7
The tibiofibular syndesmosis allows a very slight, but important, degree of movement between the two bones.
|
Bones
Types of bone (Fig. 3.8)
Long bones
The epiphysis in a growing long bone is separated from the hollow shaft, or diaphysis, by the epiphyseal plate, or physis. The part of the diaphysis next to the physis is the metaphysis. Any bone arranged like this is called a long bone, even if it is quite short – the phalanges of the fingers and toes are ‘long’ bones in structure. Damage to a growing epiphysis causes deformity.
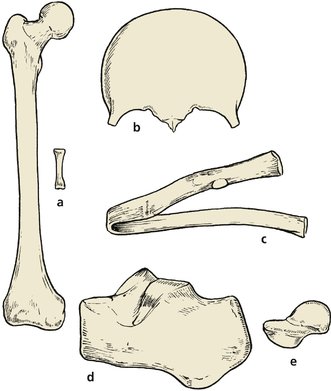 |
| Fig. 3.8
Different types of bone: (a) long bones; (b), (c) flat bones; (d), (e) short bones.
|
Flat bones
Flat bones, such as the skull, pelvis and ribs, form in condensations of fibrous tissue and are often called membrane bones. Their function is the protection of soft viscera such as the brain and lungs.
Short bones
Short square bones like those of the tarsus and carpus form in blocks of cartilage and ossify from the centre. They do not have epiphyses.
Accessory ossicles
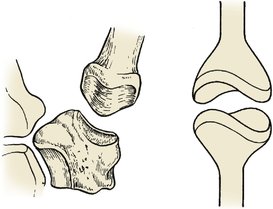
In addition to the normal bones, accessory ossicles occur as variants of normal. These are entirely innocent structures but can be mistaken for fractures and treated as such. The os trigonum behind the talus (Fig. 3.9a) and the accessory navicular (Fig. 3.9b) are among the most common.
 |
| Fig. 3.9
Accessory ossicles: (a) the os trigonum: (b) accessory navicular bone.
|
Epiphyses
Growth of bones
Long bones grow from a physis (epiphyseal plate or growth plate) at each end. Although both ends grow, one will generally grow faster than the other and different epiphyses contribute different amounts to the length of a bone.
The lower femoral and upper tibial epiphyses contribute roughly 60% of limb length, but the proximal humeral epiphysis is responsible for 80% of the length of the humerus. The exact proportions need only be remembered by orthopaedic surgeons.
If all growth is stopped at an epiphyseal plate, the limb will be straight but shorter than normal. If only one side of the plate is stopped, which can happen after a fracture through the growth plate, an unpleasant angular deformity may follow (p. 102 and p. 218). These problems do not occur in membrane or cartilage bones, which grow by getting gradually bigger in all directions.
Generalized illness in childhood can retard bone growth and leave a dense line on the radiograph that remains throughout life (growth arrest). These lines are called Harris’ lines and are of no clinical importance (Fig. 3.10).
 |
| Fig. 3.10
Harris’ lines indicating growth arrest during development. In this patient they were due to multiple operations for a congenital anomaly.
|
Apophyses
A scale of growing bone, or apophysis, is present on some bones. Unlike epiphyseal plates, apophyses do not contribute to the length of the bone. There are many apophyses but the most important are at the acromion, the olecranon, the tibial tubercle and the calcaneum. To the unwary, apophyses look like fractures and can lead to a patient being put in plaster for a fracture that does not exist.
Periosteum
The outer half of the periosteum is fibrous but the inner half contains mesenchymal cells which can differentiate into osteoblasts or osteoclasts. Periosteum, like all living tissue, must be treated gently at operation if its growth potential is to be preserved.
Blood supply
The nutrient artery supplies the bone marrow and some cortex in adult long bones but the periosteal vessels can take over if the nutrient artery is damaged by, for example, a fracture or intramedullary nailing (p. 135) (Fig. 3.11). The circulus vasculosus, the ring of vessels which surrounds most joints, contributes to the supply of the large ends of long bones.
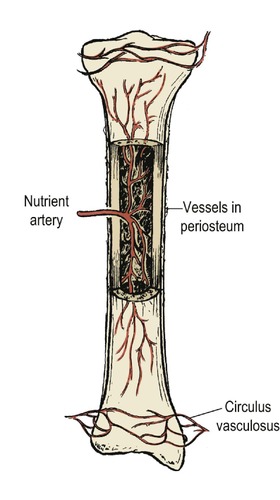 |
| Fig. 3.11
Blood supply of a long bone.
|
It is easy to forget the blood supply of bone when operating upon a limb with a tourniquet applied but the nutrient artery and periosteum must be respected or the bone may become avascular and die.
Cartilage
Types of cartilage
Hyaline cartilage
Hyaline, or articular, cartilage is highly organized tissue consisting of loops of type II collagen within a ground substance of proteoglycans produced by chondrocytes. The proteoglycans are hydrophilic and the tissue tension within the deep layers of hyaline cartilage is considerable. The structure can be compared with an inflatable building or a ‘blister’ over a tennis court: one is inflated by water drawn in by proteoglycans, and the other by air pumped in by an electric fan. In one, the pressure is contained by collagen loops, in the other by a plastic canopy (Fig. 3.12).
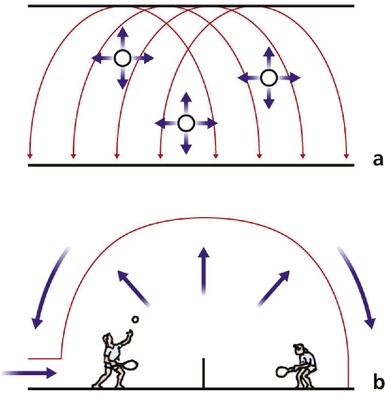 |
| Fig. 3.12
Structure of articular cartilage. The pressure generated by the chondrocytes and ground substance is contained by arches of collagen, just as the air pressure in a tennis ‘blister’ is contained by its canopy.
|
Fibrocartilage
Fibrocartilage varies from place to place according to its elasticity, which depends on the relative amounts of elastin and collagen within it. The fibrocartilage of the ear and nasal cartilages, for example, is different from that of the intervertebral discs.
Collagen
There are many types of collagen, each with different properties. Type I collagen is found in bone and type II is found in hyaline cartilage. Hyaline cartilage heals with fibrocartilage, which contains type III collagen and is less durable than true hyaline cartilage. Type IV collagen is found in flexible structures such as the ear and nose, and other types are found elsewhere.
Muscles
The ‘traditional’ anatomical teaching was that a muscle arises from bone ‘a’, is inserted on bone ‘b’ and acts on joint ‘c’. This is excellent for understanding the workings of the cadaver, but of very limited value in the management of patients. Muscles are only one part of the total motor system and the correct balancing of these muscles, both in direction and in power, is essential if a damaged limb is to work normally.
Agonists and antagonists
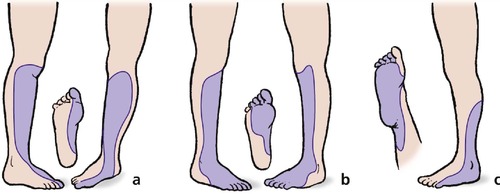
Muscles work as balanced groups which oppose each other. If the flexor muscles work more strongly than the extensors, as they do in cerebral palsy, a flexion deformity develops. If the flexors are completely denervated, an extension deformity develops, but only if the extensors are still working (Fig. 3.13).
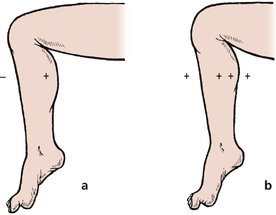 |
| Fig. 3.13
Muscle imbalance. Normal power in the ankle flexors but diminished power in the ankle extensors (a) produces an equinus deformity. Normal power in the extensors and increased power in the flexors (b) also produces a flexion deformity.
|
The agonists and antagonists work in such close harmony that no muscle can be regarded simply as an anatomical structure running between its origin and insertion. Moving an extensor to reinforce a weak flexor is no guarantee of success because the extensor has ‘learned’ to contract while the flexor is relaxing. Extensive physiotherapy is needed to re-educate the muscle to work in the opposite manner to which it is accustomed. To add to this difficulty, a transferred muscle never works quite as effectively as it did before transfer and loses at least one MRC grade of power (p. 14) when it is moved.
Fractures separating muscle groups
The importance of the relationship between muscles is illustrated by certain fractures. A fracture of the femur at the junction of its upper and middle thirds leaves the hip abductors and most of the flexors on the upper fragment, and all the adductors and most of the extensors on the lower. The upper fragment therefore swings up into unopposed abduction and flexion while the lower fragment stays on the bed and swings into adduction (Fig. 3.14). Similarly, a fracture of the forearm separates the supinators (biceps and supinator) in the upper fragment from the pronators (pronator teres and pronator quadratus). What happens? The upper fragment supinates as far as it can and the lower fragment pronates to produce a nasty rotational deformity that prevents supination. This means that the patient cannot collect change when shopping.
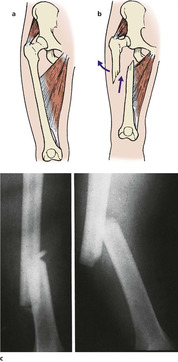 |
| Fig. 3.14
Fractures separating muscle groups. When a fractured femur separates the hip abductors from the hip adductors, the bones are pulled apart. (a) Normal. (b) Transverse fracture of the femur showing displacement of the fragments. (c) Radiograph of fractured femur.
|
A variation on the same theme is seen in fractures of the upper end of the femur. With the femur intact, the iliopsoas internally rotates the hip because it lies lateral to the axis of rotation of the joint. If the femoral neck is broken, the iliopsoas cannot act on the hip, but spins the femur about its long axis to produce the characteristic external rotation deformity of a fracture at the upper end of the femur.
Fractures which separate the mechanical linkage between muscle groups are difficult to hold without internal fixation devices.
Compartments
Muscles are contained within fascial compartments (Fig. 3.15). The fascia prevents the damaged tissue swelling and the pressure within the compartment can rise so much that its contents become ischaemic and die. Ischaemic muscle is replaced by fibrous tissue, which contracts. Nerves also perish and a serious disability ensues.
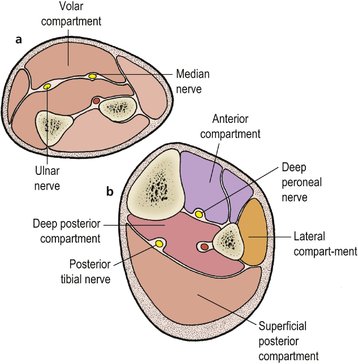 |
| Fig. 3.15
Fascial compartments in (a) the forearm and (b) the calf.
|
Forearm
There are two compartments in the forearm, ventral (flexor) and dorsal (extensor).
Ventral compartment. The ventral compartment includes the median and ulnar nerves, and the radial and ulnar arteries. Compression of these structures within the fascial sheath can have disastrous consequences.
Dorsal compartment. The extensor compartment is less often damaged than the ventral and includes the posterior interosseous nerve but no major vessels. The consequences of a dorsal compartment syndrome are less serious than ventral compartment compression, partly because it contains fewer important structures and partly because its fascia is less dense.
Lower limb
In the leg there are four compartments and all can cause serious problems (Fig. 3.16).
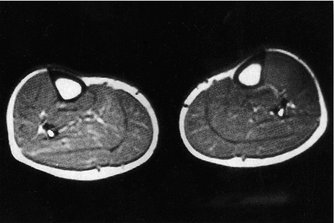 |
| Fig. 3.16
MRI scan showing the compartments in the calf.
By kind permission of the MRIS Unit, Addenbrooke’s Hospital, Cambridge.
|
Anterior tibial compartment. The anterior tibial compartment contains the anterior tibial artery and deep peroneal nerve after it has left the peroneal compartment.
Superficial posterior compartment. There are no important vessels or nerves in the superficial posterior compartment, which includes gastrocnemius and soleus only.
Lateral (peroneal) compartment. The lateral compartment contains the superficial peroneal nerve but it is seldom affected by compression.
Muscle length
Muscles only work correctly over a very small range of movement. If a bone is fractured and unites a centimetre shorter than it was before, the first centimetre of muscle contraction has no effect on the position of the limb and power is reduced (Fig. 3.17). The correct relationship between the length of the muscle and tendon and the length of bone should be maintained whenever possible, but if this cannot be achieved the muscle will eventually adapt to its new length.
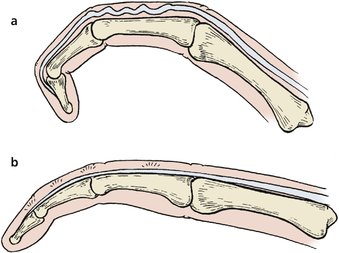 |
| Fig. 3.17
A finger with an excessively long extensor tendon (a) cannot be fully extended. (b) A finger with an excessively short extensor tendon cannot be fully flexed.
|
Tendons
The direction in which a muscle acts depends upon the direction of its tendon, which can change as it runs through loops, as at the wrist, or around corners, as in the fingers. Tendons do not tolerate friction well and are protected at such points by bursae, synovial sheaths, or the sesamoid bones, such as the patella and the fabella in the gastrocnemius tendon at the back of the knee.
Nerves
The orthopaedic surgeon sees many neurological lesions: root lesions caused by prolapsed discs or spinal injury, peripheral nerve lesions caused by trauma, ulnar neuritis, median nerve compression, brachial plexus injuries, spinal stenosis, peroneal muscle atrophy and many others. A few patients are seen with other neurological disorders, particularly if they cause muscle weakness or mimic a disc lesion. These must be recognized and referred to the neurologists.
Orthopaedic surgeons are therefore particularly interested in dermatomes and the root value of peripheral nerves. A knowledge of the root innervation of muscles is also needed to interpret the MRC grading of muscle power. If a muscle is innervated by several nerve roots, one root can be completely divided with only a partial loss of power, but dividing one root will cause a complete loss of power if the muscle is supplied by a single root only.
Dermatomes and root values
The dermatomes in the upper and lower limbs determine the distribution of sensory symptoms arising from pressure on the nerve roots, and must be known in detail (Fig. 3.18).
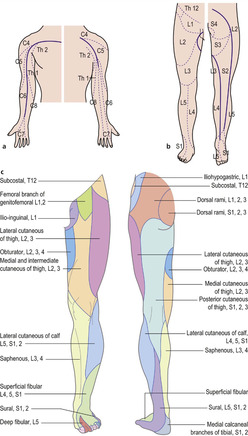 |
| Fig. 3.18
Dermatomes in (a) the upper limb and (b) the lower limb. Nerve distribution in the lower limb (c).
|
The distribution of the L4, L5 and S1 roots is specially important because they are involved in 90% of lumbar disc prolapses (Fig. 3.19).
 |
| Fig. 3.19
Dermatomes. The area of skin supplied by (a) L4, (b) L5 and (c) S1.
|
Peripheral nerves
Damage to the median nerve at the wrist and the ulnar nerve at the elbow (p. 203 and p. 221) are common problems and provide a good example of the importance of clinical anatomy.
Median nerve
Patients with persistent paraesthesia in the distribution of the median nerve are likely to have compression of the median nerve at the wrist (Fig. 3.20) (p. 387). The fluid retention of pregnancy is one cause but repetitive movements of the flexor tendons of the hand and wrist also lead to a localized flexor tenosynovitis, which in turn causes soft tissue swelling and compression of the median nerve as it enters the hand through the carpal tunnel.
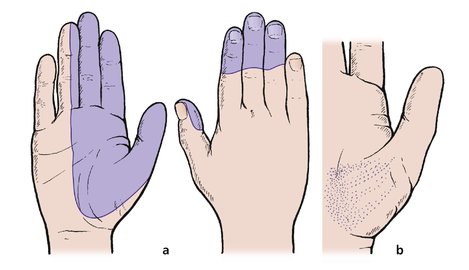 |
| Fig. 3.20
Distribution of the median nerve. Damage to the median nerve produces (a) diminished sensibility in the palm; (b) weakness and wasting of the thenar eminence. Note: If the nerve is compressed in the carpal tunnel the palm is spared.
|
As the median nerve is compressed, sensory symptoms are felt in thumb, index and middle fingers, half the ring finger on the palmar surface and on the back of the fingers. The palm itself is spared because the palmar branch arises before the nerve enters the carpal tunnel.
Variations in the distribution of the median nerve are common.
Ulnar nerve
The ulnar nerve may be irritated at the elbow as it runs behind the medial epicondyle. The nerve can be damaged by trauma, osteoarthrosis, deformity from malunion (tardy ulnar palsy, p. 387), or even pressure on the medial side of the elbow as the arm rests on an operating table. The patient will experience paraesthesiae or numbness in the little finger and the ulnar half of the ring finger, weakness of the hand, or sometimes clumsiness due to weakness of the intrinsic muscles supplied by the ulnar nerve (Fig. 3.21).
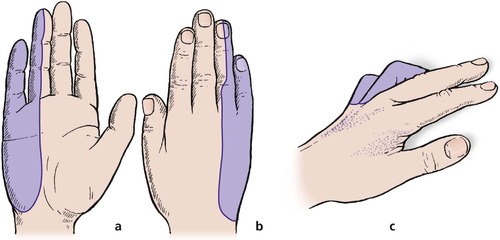 |
| Fig. 3.21
Distribution of the ulnar nerve. Damage to the nerve produces diminished sensibility in: (a) the palm; (b) the dorsum of the hand; and (c) a claw deformity in the little and ring fingers because of damage to their interossei and lumbrical muscles.
|
Radial nerve
The radial nerve is safe in the forearm but vulnerable in the upper arm. Pressure on the radial nerve from old-fashioned axillary crutches can lead to a troublesome drop wrist but few sensory symptoms (Fig. 3.22). Other causes, now almost historical, are the ‘Saturday night palsy’ of inebriated patients who fall asleep with their arms over the back of a chair and, in more recent and healthier days, pressure on the medial side of the upper arm from prolonged pressure on the back of a cinema seat.
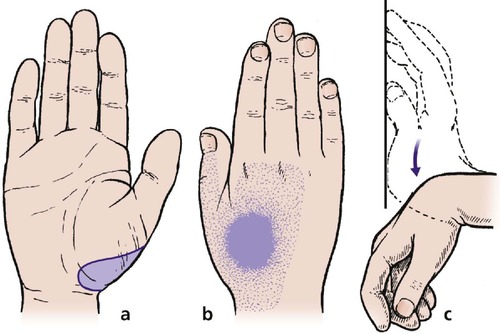 |
| Fig. 3.22
Distribution of the radial nerve. Damage to the radial nerve produces no loss of sensibility in the palm (a) but there may be a small area of diminished sensibility on the dorsum (b) and there will be paralysis of the wrist extensors (wrist drop) (c).
|
Sciatic nerve
In the lower limb, the commonest peripheral nerve lesion is damage to the lateral half of the sciatic nerve from posterior dislocation of the hip (Fig. 3.23) (p. 182).
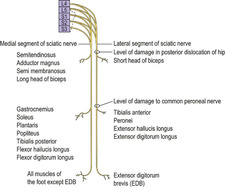 |
| Fig. 3.23
Roots of the medial and lateral components of the sciatic nerve, which become the popliteal and common peroneal nerves behind the knee.
|
Common peroneal nerve
A similar but not identical clinical picture is produced by a lesion of the common peroneal nerve as it passes around the fibular neck.
Vulnerable peripheral nerves (Fig. 3.24)
Upper limb
• Median nerve – hand through glass window.
• Ulnar nerve at elbow – pressure during operation, trauma from fracture.
• Radial nerve – cuts around the elbow, pressure from crutches, etc.
• Digital nerves – cuts around the fingers.
• Brachial plexus – upper cord, downward pressure on the shoulder as when falling off a motorcycle; lower cord, dragging of the arm upwards during road trauma and catching onto things while falling, e.g. scaffolding.
• Cervical nerve roots – prolapsed intervertebral disc.
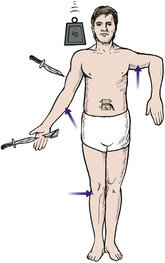 |
| Fig. 3.24
Common sites of peripheral nerve injury include abduction injuries of the brachial plexus, lacerations of the radial nerve, compression of the ulnar nerve, lacerations of the median nerve at the wrist and digital nerves in the fingers, pressure on the radial nerve in the upper arm, root entrapment in the lumbar spine and pressure on the common peroneal nerve at the knee.
|
Lower limb
• Common peroneal nerve – damage at the neck of the fibula through trauma.
• Lumbar nerve roots – prolapsed intervertebral disc.
• Sciatic nerve – damage from dislocation of the hip.