Orthodontic Considerations in the Evaluation and Treatment of Dentofacial Deformities
Orthodontic Treatment Philosophy
Current issues in orthodontic therapy are, for the most part, no longer just a matter of what attachments or mechanical approaches to use.* Contemporary orthodontics focuses on accurate diagnosis and a basic philosophy of treatment to enhance facial aesthetics and to correct dysfunction. The role of orthognathic surgical interventions and coordinated comprehensive dental rehabilitation to achieve the most favorable outcome should always be considered.110
Malocclusions result from a combination of environmental influences and the patient’s morphogenetic hereditary predisposition (see Chapter 4).1,11,15,18,43,44 The dental alignment that naturally occurs in each individual is greatly influenced by the baseline jaw relationships as well as by his or her daily postural masticatory and airway function.† In the presence of a dentofacial deformity, the mere orthodontic movement of the teeth into a “better” interdigitation will not establish normal jaw relationships nor will it correct the head and neck dysfunctions that contribute to or result from the malocclusion.147,157,179–181 The observed crowding of the teeth generally reflects nature’s attempt to establish a homeostatic balance among the available space in the alveolus, the size of the teeth and the dental roots, the position and size of the jaws, and the constant molding and balancing effects of the masticatory and facial musculature with regard to daily function.6,146,147,162–165,182,183
The Biologic Basis for Orthodontic Tooth Movement
Currently, there are a plethora of appliances than can accomplish almost any desired change in the alignment of the teeth.69,72 From a purely mechanical perspective, orthodontists are trained in the techniques of tooth movement with the goals of improving dental alignment in each jaw and achieving “ideal” occlusion between the upper and lower arches. The orthodontic movement of the teeth is based on the principle that, if prolonged pressure is applied to a tooth, movement will occur as the bone around the tooth remodels. This is primarily a periodontal ligament phenomenon. In the process, bone is selectively resorbed in some areas and deposited in others. The bone that surrounds the tooth responds to the applied force through intermediate structures (periodontal ligaments), and the objective is for the tooth to move without the loss of crestal height or cortical plates while carrying its attachment apparatus along with it. The whole socket must migrate along with the tooth during this process.
When orthodontic therapy is used to move teeth outside of a biologic envelope, extended treatment time, the potential for periodontal sequelae, and a less-than-ideal long-term occlusion are the likely consequences.70,86,178 These may occur as a result of the following: (1) attempts to further compensate the position of the teeth toward the skeletal disharmony and outside of the alveolar housing; (2) dental (root) crowding within limited available alveolar bone; or (3) ongoing nasal airway obstruction with an open mouth posture and inadequate lip coverage of the incisors.4,8,9,32,73,85,193
Periodontal Ligament Structure and Function
Unless ankylosis is present, each tooth is connected to and separated from the adjacent alveolar bone by a specialized collagen supporting structure known as the periodontal ligament (PDL) (Fig. 5-1). The PDL normally occupies a space of approximately 0.5 mm around all parts of the tooth root. The PDL is comprised of a network of parallel collagenous fibers that insert into the cementum (i.e., the covering of the root surface of each tooth) and then into a dense bony plate (radiographically, this is called the lamina dura) that is adjacent to each tooth within the alveolar bone. These supporting PDL fibers are angulated between the root of the tooth and adjacent bone; they attach apically on the root and extend occlusally to the adjacent bone. Biomechanically, these angulated PDL fibers act as shock absorbers by helping to resist forces that are applied to the tooth during normal chewing function.

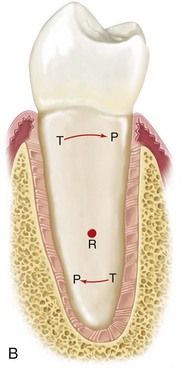
Figure 5-1 A, Principal fiber bundles of the periodontal ligament on the facial surface of a mandibular premolar (silver stain). B, Distribution of faciolingual forces (arrows) around the axis of rotation (R) in a mandibular premolar. The periodontal ligament fibers are compressed in areas of pressure (P) and taut in areas of tension (T). Part A from Glickman I: Clinical periodontology, ed 4, Philadelphia, 1972, W.B. Saunders Company, Figures 2-3 and 2-8, pp 34 and 38, respectively.
Within the periodontal ligament space, there are cellular elements (i.e., mesenchymal cells, nerve endings, and vessels) and interstitial fluid. The primary cellular elements (i.e., mesenchymal cells) are thought to differentiate to form the fibrocytes and the osteocytes. The collagenous elements of the PDL are constantly being renewed and altered, depending on the level of functional stress that they are undergoing. The remodeling and recontouring of the alveolar bone is a necessary component of orthodontic tooth movement, and it is dependent on specialized cells (Fig. 5-2). As part of the remodeling process, bone is removed by osteoclasts that are thought to be derived from the mesenchymal cells. Cementum is removed by specialized cementoclasts, which are also derived from mesenchymal cells. Nerve endings attach to the PDL and to the blood vessels that surround them. The nerve endings are effective for proprioception and for the perception of pain. The interstitial fluid found within the PDL space is derived from the vascular network. It serves as a nutrient source, and it contributes to the shock-absorbing mechanism to better withstand the physiologic forces as well as any pathologic forces that are applied directly to the teeth.
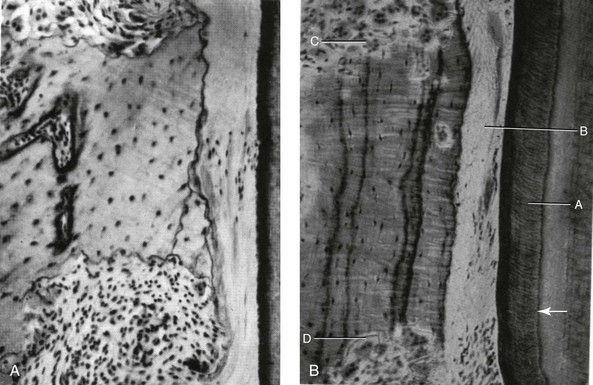
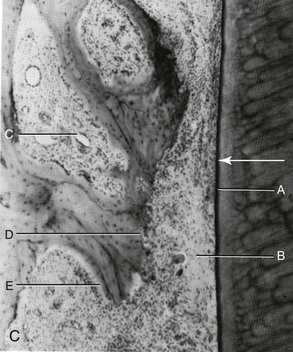
Figure 5-2 A, Undermining resorption in a 12-year-old child. This is a view from a short-rooted premolar tooth. The cementum that covers the root surface has not been broken, although the periodontal membrane is hyalinized at the area of greatest pressure. A spicule of bone is being attacked from above and below, away from the compressed PDM. B, Undermining resorption is taking place in a 39-year-old adult. No osteoclastic activity occurs in the compressed PDM, but osteoclasts are at work on bundle bone that has been laid down previously from above and below the area of greatest pressure. A, Thick cementum layer. B, Hyalinized periodontal ligament. C and D, Frontal undermining bone resorption on both sides of the cell-free area. C, Tooth movement with light forces. This image shows the pressure side during the period shortly after hyalinization. A, Root surface. B, Remnants of cell-free, formerly hyalinized tissue. C, Large marrow space in alveolar bone. D, Direct bone resorption. E, Compensatory bone formation in the marrow space as a response to bone resorption on the side of the periodontal ligament. A courtesy K. Reitan from Graber TM: Orthodontics: principles and practice, ed 3, Philadelphia, 1972, W.B. Saunders Company, Figure 10-5, p 496. B courtesy K. Reitan from Graber TM: Orthodontics: principles and practice, ed 3, Philadelphia, 1972, W.B. Saunders Company, Figure 10-5, p 496. C courtesy K. Reitan from Graber TM: Orthodontics: principles and practice, ed 3, Philadelphia, 1972, W.B. Saunders Company, Figure 10-6, p 497.
Response of the Teeth and the Periodontium to Normal Occlusal Function
During normal chewing function, the teeth are subjected to intermittent forces that are then transmitted to the periodontal structures.55,88,89,92,118,192,209 When forces are applied to a tooth, the load is dissipated by the periodontal ligament and the interstitial fluid within the tooth socket. These mechanisms allow a more limited force to then be transmitted to the cortical bone that surrounds the tooth socket (i.e., the lamina dura), which “bends” in response. The term bending is used to describe the physiologic response to normal masticatory forces. The bone bending that occurs in response to normal (chewing) function is thought to be an important stimulus to osseous regeneration and repair. This intermittent but repetitive stress loading allows for the modification of the bony architecture as an adaptation to functional demands. If pressure against the tooth is maintained (as opposed to being intermittent, as when chewing), the interstitial fluid within the tooth socket is expressed (i.e., pushed out) and the tooth itself is displaced, thereby compressing the PDL directly against the adjacent bone. This is perceived by the individual as being quite painful, and, if the force is excessive and prolonged, a different physiologic response occurs. This “trauma from occlusion” is a response in which the remodeling of the adjacent compressed bone occurs. A definition of the term traumatic occlusion was first provided by Stillman in 1917. He stated that traumatic occlusion is “a condition where injury results to the supporting structures of the teeth by the act of bringing the jaws into closed contacts.”171 The definition given by the American Association of Periodontics in 1986 is “an injury to the attachment apparatus as a result of excessive occlusal force.”171 Primary occlusal trauma involves excessive forces on a normal periodontium, and secondary occlusal trauma is considered to have occurred when normal forces are placed on a compromised periodontium (see Chapter 6).
The intentional application of these principles is how controlled orthodontic tooth movement occurs. The application of light prolonged vector-controlled forces allows for more or less predictable man-made movements of the teeth. Interestingly, nature’s application of these light prolonged forces on the teeth can also occur from maintained posturing of the muscles of the lips, cheeks, and tongue as they press against the teeth, thereby causing dental movement and remodeling of the alveolar ridge. When postural forces from the lip, cheek, or tongue are pathologic, they may contribute to the classic dental compensations that are seen with each specific pattern of developmental dentofacial deformity.* These environmental forces may then be compounded by iatrogenic orthodontic dental compensation maneuvers to further affect periodontal health. For example, consider the retroclination of the lower anterior teeth that is seen with Class III skeletal patterns (Fig. 5-3) (see Chapter 20) or the proclination of the lower incisors that is seen with skeletal Class II cases (Fig. 5-4) (see Chapter 19). In both instances, negative periodontal sequelae may occur.

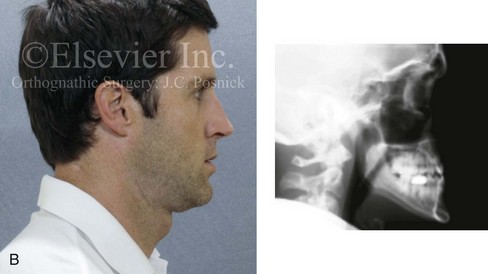

Figure 5-3 A 34-year-old man arrived for the evaluation of a long-standing jaw deformity with malocclusion, chronic obstructive nasal breathing, and periodontal issues. Since his early childhood years, he was known to have a maxillary deficiency with a relative mandibular excess growth pattern. The family elected a camouflage orthodontic approach that included four bicuspid extractions and the introduction of dental compensation in an attempt to neutralize the occlusion when he was 10 to 15 years old. He was a forced mouth breather as a result of the associated increased nasal airway resistance. He underwent septoplasty when he was 20 years old, but this did not result in significant improvement. His general dentist confirmed labial bone loss and gingival recession of the mandibular anterior and maxillary posterior dentition. He was referred to this surgeon, and a comprehensive orthognathic and dental rehabilitation approach was recommended. Consultations with a periodontist, an orthodontist, and an ear, nose, and throat specialist were carried out. The patient was confirmed to have residual deviation of the septum and enlarged inferior turbinates, which explained the continued difficulty that he had with breathing through his nose. A degree of root resorption of the anterior dentition was confirmed. The need for gingival grafting to attain improved root coverage and to generate a wider band of attachment was recommended (i.e., teeth nos. 3, 11, 14, 19, 20, 23 through 26, 29, and 30). This will be followed by the orthodontic removal of dental compensation and then orthognathic and intranasal procedures to improve long-term dental health, to enhance facial aesthetics, and to open the upper airway. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment. C, Panorex radiograph with retreatment in progress.
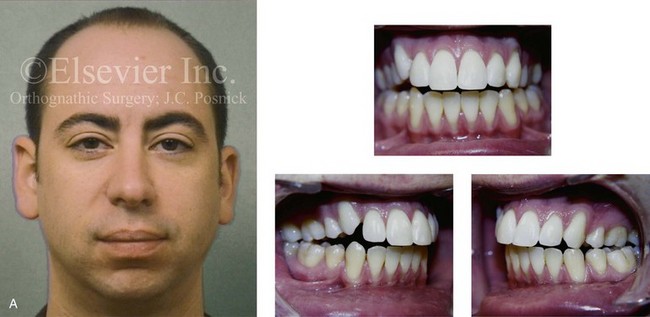
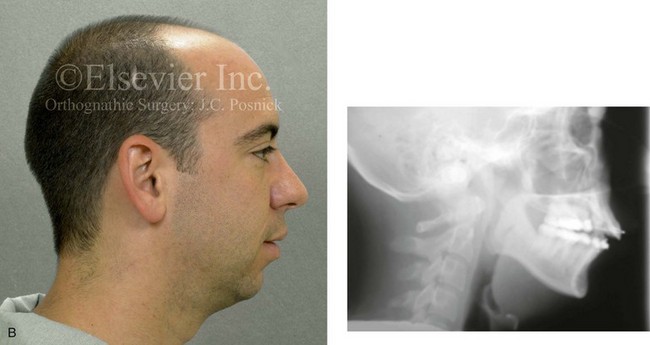
Figure 5-4 A man in his early twenties with a primary mandibular deficiency growth pattern. During his teenage years, he underwent failed growth modification attempts followed by orthodontic camouflage maneuvers that included four bicuspid extractions in an attempt to neutralize the occlusion. Deterioration of the periodontium with labial bone loss and gingiva recession along the mandibular anterior dentition is evident. The patient was referred to this surgeon, and a comprehensive orthognathic and dental rehabilitation approach was approved. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment.
Orthodontic Tooth Movement
The Periodontal Ligament and Bone Response to Sustained Orthodontic Force
The specific anatomic response to orthodontic forces is dependent on the force magnitude. “Heavy” forces often result in pain, necrosis of cellular elements within the PDL (i.e., hyalinization), and remodeling with the resorption of the alveolar bone that is being compressed (i.e., the hyalinization zone). It may also result in the resorption of the root apex, remodeling with the loss of crestal bone, and fenestrations or dehiscence through the cortical plates. When light and constant forces are applied to the tooth, there is compression without necrosis of the PDL elements and remodeling of the tooth socket without significant irreversible necrosis. As long as the tooth is being moved into adequate alveolar bone and the forces are light, the root of the tooth is less likely to resorb, and the alveolar crest height and cortical plates are for the most part preserved.30 The objective of the orthodontic movement of a tooth is to produce the desired new tooth position as quickly as can be done, with as little damage as possible to the tooth, the PDL, the alveolar bone, and the adjacent teeth.
The Amount of Orthodontic Force Applied to the Teeth
The heavier the sustained pressure, the greater the reduction in blood flow where compression is occurring in the PDL.25,166,174 When only light prolonged force is applied to a tooth, the partially compressed PDL experiences diminished blood flow, and the interstitial fluids are expressed (pushed out) from the PDL space as the tooth moves within the socket.125 Animal experiments confirm that, within a few hours, there will be increased levels of cyclic adenosine monophosphate (cAMP).175 cAMP is known for its importance in the alteration of cell functions. Within 4 hours of continued sustained low pressure, mesenchymal cell differentiation occurs. From a clinical perspective, it is known that, if orthodontic appliances are used for less than 4 to 6 hours per day, not enough sustained force will be applied, and little or no tooth movement will occur.143,148
It is known that the osteoclasts attack the compressed area of lamina dura to remove bone.184 The radiographic appearance of a widened PDL (on the tension side) in the presence of light prolonged orthodontic forces indicates that tooth movement is soon to begin.66 On the compression side, osteoclasts are removing the lamina dura. On the tension side, remodeling activity involves osteoblasts laying down new bone. The course of events is different if the prolonged force applied to the tooth is too great. If the force transmitted to the periodontal ligament totally occludes the blood vessels, thereby cutting off all blood supply to the area, generalized necrosis occurs within the compressed area. Although some avascular areas in the PDL will occur even with light forces, if the predominant forces are “heavy,” then the response is necrosis. Irreversible damage can then occur, and this includes remodeling with the loss of crestal bone, root resorption, and cortical plate dehiscence. The histologic findings within the PDL—even with light forces during the compression process—show the disappearance of cells within the vessels. The histologic appearance is descriptively said to be “hyalinized” because of its visual resemblance to hyaline connective tissue. After this hyalinization process begins, after several days of delay, the remodeling of bone that borders the sporadic necrotic areas of the PDL will occur as osteoclasts (derived from adjacent undamaged areas) arrive and do their work. The process of bone removal is called undermining resorption. This term is visually descriptive when it is viewed under the microscope, because the attack by the osteoclasts is from the underside of the lamina dura. After the hyalinization (i.e., the compression of blood flow with isolated necrosis) and the undermining resorption (i.e., the osteoclastic activity on the underside of the lamina dura) have “softened” the lamina dura, tooth movement is soon to occur. The chronology of tooth movement with frontal resorption is different than that of undermining resorption. With frontal resorption, a steady attack on the outer surface of the lamina dura results in smooth, continuous tooth movement. With undermining resorption, there will be a delay in the removal of the bone adjacent to the tooth. When heavy force (i.e., pressure) is again reinitiated, there will be a similar delay in tooth movement until a second round of undermining resorption can occur.171
The orthodontic movement of a tooth is clinically more efficient when there are only minimal areas of PDL necrosis. As a result, only limited levels of pain are experienced by the individual undergoing treatment. Unfortunately, neither aspect is completely avoidable. To date, a completely smooth progression of tooth movement with consistent light force over time has proven to be unattainable within the human biologic system. One important compounding factor is that the individual who is undergoing orthodontic tooth movement must also continue with the everyday functions of mastication, speech, swallowing, and breathing within a 24-hour cycle. These functions also place forces on the teeth, which may either conflict with or expedite the applied orthodontic forces. Another factor is the relative ineffectiveness of the appliances (i.e., the materials) used to apply sustained appropriate levels of force. To review, in clinical orthodontic practice, on one end of the spectrum, too much sustained force is detrimental to the tissues; alternatively, too little force will not produce the tooth movement that is desired.25
Medication Effects on the Rate of Orthodontic Tooth Movement
The bisphosphonates act as inhibitors of osteoclast-mediated bone resorption, which by definition have an effect on bone remodeling.5,102 There is evidence to suggest that tooth movement in patients who are receiving parenteral bisphosphonate therapy may be retarded, with a subsequent risk for osteonecrosis of the jaws.113
Bartzela and colleagues conducted a systematic review of the literature regarding the effects of medications and dietary supplements on the rate of experimental orthodontic tooth movement.23 The results of their literature search indicated the following:
• The therapeutic administration of eicosanoids results in increased tooth movement.
• Nonsteroidal anti-inflammatory drugs decreased tooth movement; however, non-nonsteroidal anti-inflammatory analgesics (e.g., Paracetamol [acetaminophen]) had no effect.
• Corticosteroid hormones, parathyroid hormone, and thyroxin have all been shown to increase tooth movement.
• Estrogens probably reduce tooth movement, although no direct evidence is available.
• Vitamin D3 stimulates tooth movement, and dietary calcium seems to reduce it.
The Role of Anchorage in the Orthodontic Movement of Teeth
The term anchorage as it applies to orthodontics refers to the nature and degree of resistance to displacement provided by an anatomic unit (e.g., molars and premolars, temporary skeletal anchorage devices, hard palate) when it is used for the purpose of effecting tooth movement.139
Reciprocal Tooth Movement
When planning orthodontic therapy, the clinician must consider not just the tooth movement that is desired but any reciprocal effects that may occur throughout the dental arches as well. Reciprocal effects must be controlled to achieve the desired repositioning of all of the teeth and to establish preferred occlusion. In a completely reciprocal situation, Newton’s theory is easy to understand. When the forces applied to similar teeth and to similar arch segments are equal, there will be an equal force distribution in each PDL with this same degree of movement. A classic clinical case analysis that is frequently used to understand the “reciprocal/nonreciprocal” concept is to consider the type of tooth movement that occurs when an elastomeric chain is placed across a first premolar extraction site in the maxilla. This pits the central incisor, the lateral incisor, and the canine in the anterior segment in opposition to the second premolar and the first molar in the posterior segment. The same total force would be felt by the three anterior teeth and the two posterior teeth as the action of the chain is equal in each segment. However, equal reciprocal movement would require the same total PDL surface area over which the force is distributed. Because the measured PDL area for the two posterior teeth is larger than the three anterior teeth, the movement will not be reciprocal. In this typical, real-life clinical setting, the anterior teeth move back into the bicuspid extraction sites more than the posterior teeth migrate forward. If it is desired that the anterior teeth move entirely into the extraction space, reinforced anchorage will be required. This may be accomplished by incorporating the second molar into the posterior unit. This changes the root surface area ratios, which results in additional retraction of the anterior teeth. Other methods of reinforcing posterior anchorage include the use of extra oral force, such as headgear, TADs, and palatal support through the use of Nance appliances or a transpalatal bar.148
Cortical Walls as Limiting Factors to Orthodontic Tooth Movement
Cortical bone is more resistant to resorption; therefore, tooth movement is slowed whenever the root to be moved contacts it. This can be problematic, for example, when there is a dense cortical layer of bone formed within the alveolar process of a previously (long-ago) extracted tooth. It can be more difficult to close an “old” extraction site, because tooth movement is slowed to a minimum when the root encounters cortical bone along the resorbing side of the alveolar ridge.118,126 Tooth movement is also greatly slowed and root resorption more likely when a tooth (or tooth root) is forced against a cortical plate (e.g., a labial plate, a lingual plate), such as may occur during attempts to correct incisor inclination.
In theory, the optimal force level for the orthodontic movement of a tooth is the lightest force (and the resulting pressure) needed to produce the near-maximum preferred response.176 Forces that are more than “optimal”—although effective for the production of tooth movement—are both unnecessary and possibly traumatic to the tooth, the periodontium, the alveolar ridge height, and the cortical plates.
Negative Sequelae of Orthodontic Forces
Effects on Root Structure
Recent research indicates that, when therapeutic orthodontic forces are applied, there is a degree of injury to the cementum. In current clinical practice, with the use of continuous light forces, this occurrence is less frequent. The repair of any limited cemental injury generally occurs. Alternatively, heavy orthodontic forces—whether continuous or intermittent—may lead to root resorption, because the cementoclasts remove not only cementum but also dentin of the root (Fig. 5-5). The permanent loss of root structure only occurs when an island of cementum and dentin becomes completely separated from the rest of the root surface. When this happens, resorption without reincorporation occurs.34,37,84,103,121 The permanent loss of root structure related to orthodontic treatment is generally seen at the root apex.
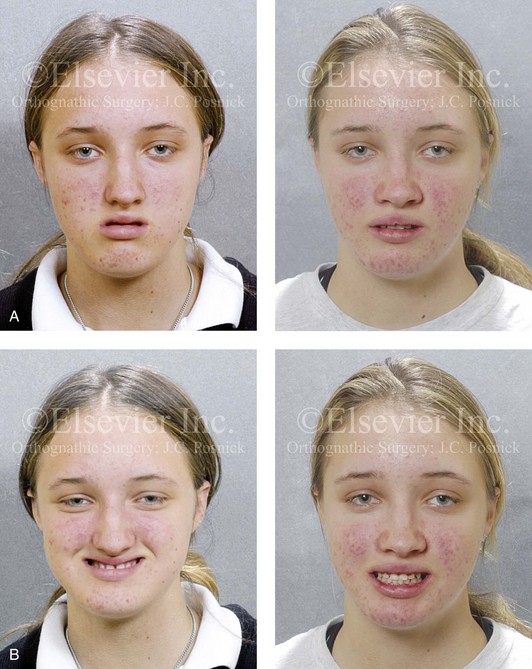

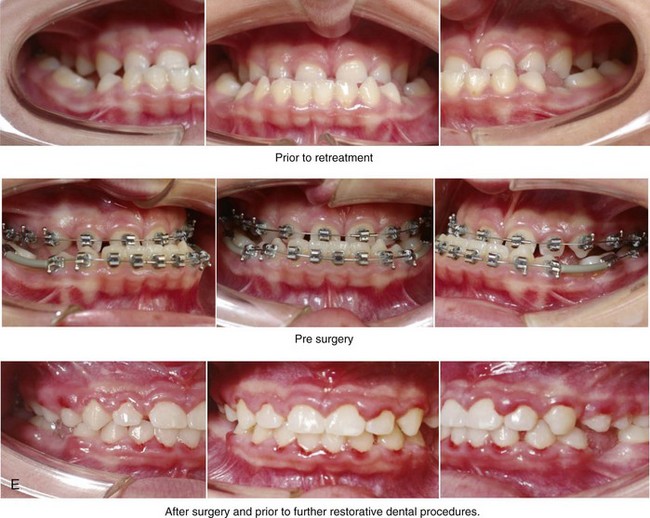
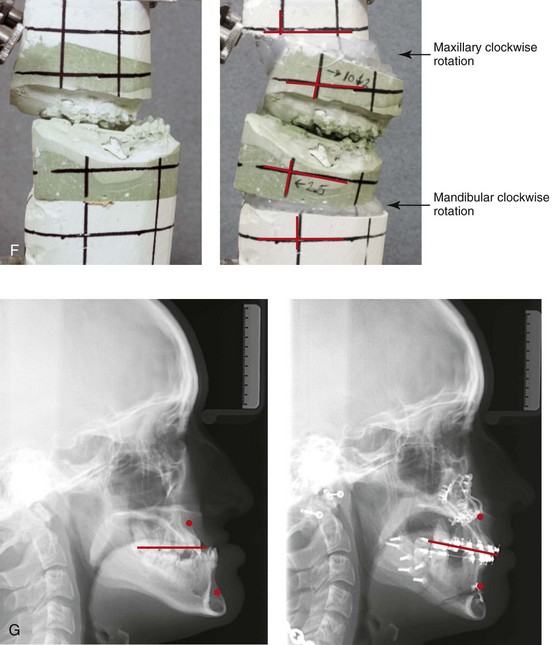
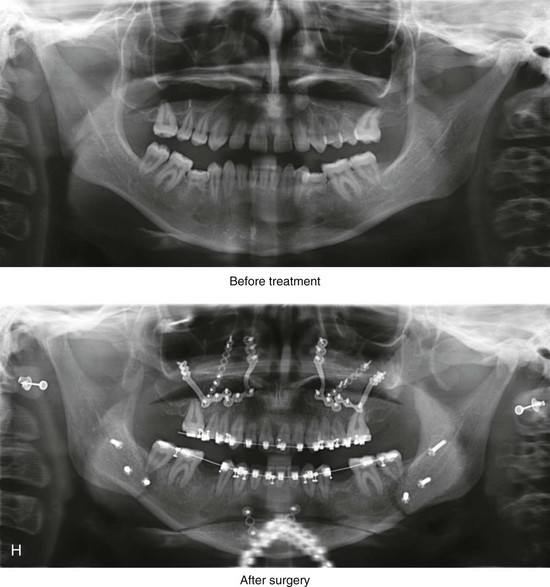
Figure 5-5 A 14-year-old girl was referred by her orthodontist for surgical evaluation. She presented with a jaw deformity and associated malocclusion characterized by maxillary deficiency in combination with asymmetrical mandibular excess. She is congenitally missing teeth (all of the third molars, the maxillary right second molar, the maxillary left second molar, the mandibular left second bicuspid, and the mandibular right second bicuspid), and she has short dental roots. At the time of arrival, she had already undergone attempts at growth modification, including a face mask followed by rapid palatal expansion. At presentation, there was an asymmetrical Angle Class III negative overjet with a bilateral posterior crossbite malocclusion. Current maxillofacial dysmorphology and dental anomalies have negative consequences on the patient’s speech, swallowing, breathing, chewing, and lip closure/posture. At this time, the patient agreed to a comprehensive facial and dental rehabilitation approach with a desire to achieve improvements in breathing, lip closure/posture, occlusion, long-term dental health, and enhanced aesthetics. After periodontal and restorative dental evaluation, limited orthodontics and then jaw and intranasal procedures were carried out. The procedures included a Le Fort I osteotomy, sagittal ramus osteotomies of the mandible, an osseous genioplasty, a septoplasty, and inferior turbinate reduction. With finishing orthodontics, restorative dentistry is planned. A, Frontal views in repose before and after surgery. B, Frontal views with smile before and after surgery. C, Oblique facial views before and after surgery. D, Profile views before and after surgery. E, Occlusal views before retreatment, with orthodontics in progress, and then after surgery but before final restorative work. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery. H, Panoramic radiographs before retreatment and after surgery.
The resorption of the tooth roots during orthodontic treatment has been documented to occur in three distinct forms: (1) moderate generalized resorption; (2) severe generalized resorption (see Figs. 5-5 and 5-6); and (3) severe localized resorption. The shortening of the root length of the maxillary incisors (i.e., severe localized resorption) is seen more often than this condition appears to occur in the other teeth (Fig. 5-7). Although some studies have shown that measurable root resorption can be identified in 90% of maxillary incisors and in more than half of all other teeth during a typical fixed orthodontic appliance treatment, the shortening is almost imperceptible, and it is clinically insignificant for most. Nevertheless, occasionally the loss of one third or one half or more of the root structure is observed in patients who underwent what was considered to be routine orthodontic treatment. When this does occur, it is either severe generalized resorption or severe localized resorption. Fortunately, severe root resorption of all orthodontically treated teeth is not common. When severe generalized resorption does occur, it is often seen without any orthodontic or other forms of active dental treatment, and it may be of an uncertain etiology. If there is evidence of root resorption before orthodontic treatment, the patient should be considered at high risk for further resorption during orthodontic treatment. Radiographs should be taken during treatment to watch for this occurrence. If resorption becomes apparent, the patient is informed, and the treatment plan altered. In contrast with severe generalized resorption, severe localized resorption is more frequently associated with specific forms of orthodontic treatment. Risk factors are likely to include heavy continuous orthodontic forces being place on the teeth and a prolonged duration of treatment. Localized resorption is more frequently seen in the maxillary incisors, when the root apices are forced against the facial cortical plate during treatment. For example, in the clinician’s attempts to compensate for a long face Class II skeletal pattern with an anterior open bite, the maxillary incisor crowns may be detorqued (resulting in a loss of proper buccolingual inclination) and vertically lengthened as the bicuspid extraction sites and the open bite are closed. This may cause the incisor roots to come into heavy contact with the labial cortical plate and thus result in so-called “round tripping.” Forces must then be reapplied to the incisors to establish adequate palatal root torque.



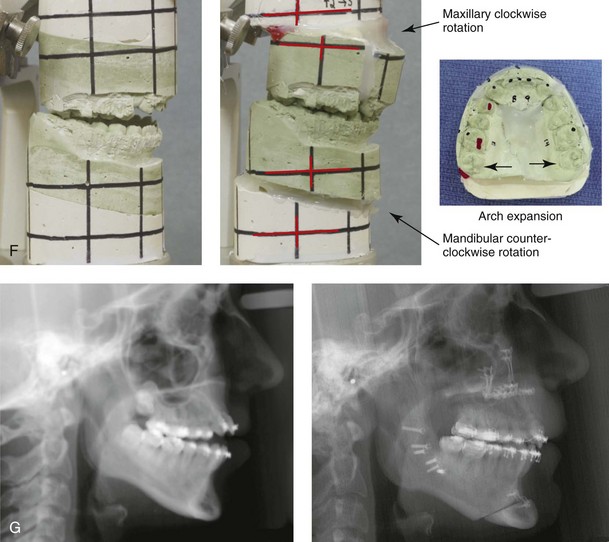
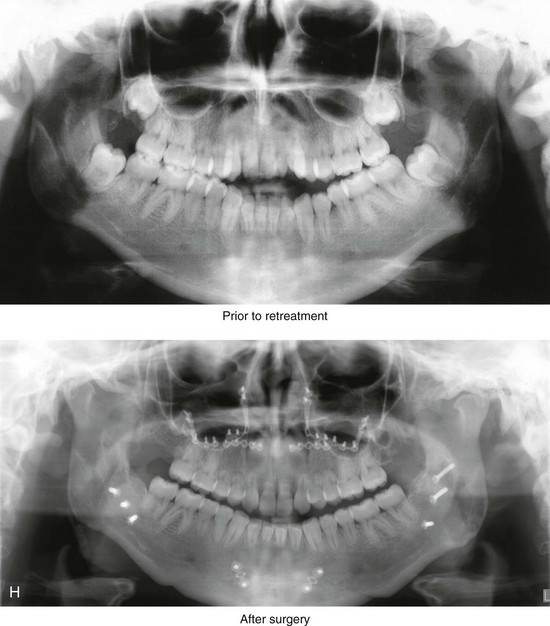
Figure 5-6 A 20-year-old woman was referred by her orthodontist for surgical evaluation. She presented with a narrow maxilla, a significant curve of Spee, and dental crowding. The mandibular arch also had dental crowding, tipping, and rotations. Both jaws lacked horizontal projection, and there was a severe anterior open bite malocclusion. The patient was a forced mouth breather with increased nasal airway resistance as a result of septal deviation, enlarged inferior turbinates, and a high nasal floor. The right maxillary lateral incisor was congenitally absent, and the left maxillary lateral incisor was hypoplastic and rudimentary. The shortness of the roots throughout the maxillary and mandibular dentition is presumed to be congenital. The patient agreed to a comprehensive facial and dental rehabilitation approach with a desire to achieve improvements in breathing, lip closure/posture, occlusion, long-term dental health, and enhanced aesthetics. She underwent periodontal treatment that included the extraction of tooth no. 10, grafting to the labial aspects of the mandibular incisors, and maxillary gingivectomy. This was followed by limited orthodontic manipulation and then jaw and intranasal surgery. The procedures included a maxillary Le Fort I osteotomy in three segments (horizontal advancement, vertical shortening, clockwise rotation, arch expansion, and the correction of the curve of Spee); bilateral sagittal split osteotomies of the mandible (horizontal advancement and counterclockwise rotation); osseous genioplasty (horizontal advancement and vertical shortening); and septoplasty/inferior turbinate reduction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before treatment, with orthodontics in progress, and after treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery. H, Sequential panoramic radiographs before retreatment and then after surgery.

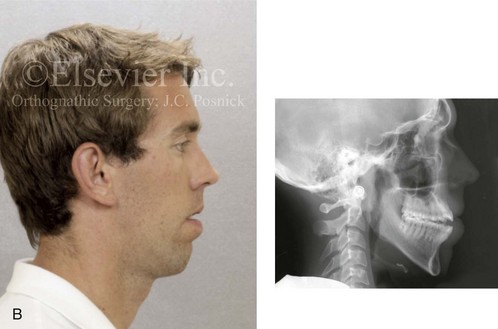
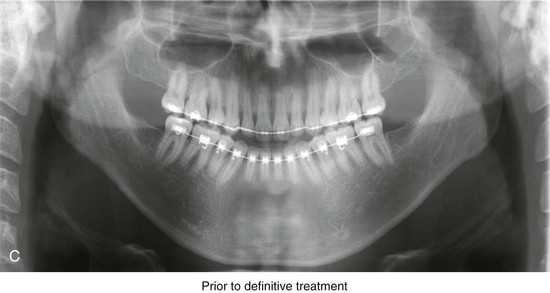
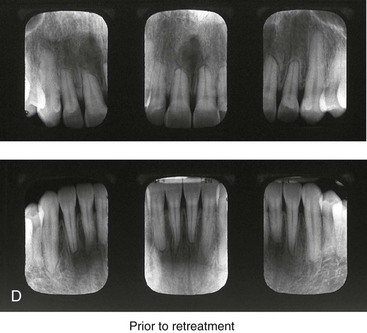
Figure 5-7 A 25-year-old man with a long face growth pattern. He underwent a first-stage surgically assisted rapid palatal expansion (SARPE) procedure to expand the maxillary arch width at another institution. There was a need for definitive orthognathic correction, which was carried out by this surgeon in conjunction with continued orthodontic treatment. A, Frontal facial view and occlusal views after SARPE procedure and before definitive orthognathic correction. B, Profile facial and cephalometric views after SARPE procedure and before further treatment. C, Panorex radiograph after SARPE. D, Periapical radiographs of anterior dentition before further treatment. A degree of root resorption of the anterior dentition had occurred after the SARPE procedure and before definitive orthognathic correction.
Effects on the Alveolar Ridge Height, the Cortical Plates, and the Gingiva
When teeth naturally erupt, they bring alveolar bone with them. It is also known that teeth may overerupt and cause excess alveolar bone height. For example, in the presence of a constant open mouth posture during growth, the hypereruption of the maxillary molars will occur (see Chapter 4). This defines the long face growth pattern (see Chapter 21).92–97 One argument for functional appliance use is to limit this molar hypereruption. The reverse effect on the alveolar process is observed at the edentulous space of a congenitally absent tooth (e.g., a retained primary molar with the congenital absence of a mandibular permanent bicuspid). The associated alveolar bone will be concave with limited vertical height (Fig. 5-8). The alveolar ridge volume deficiency at the edentulous site will also have a ripple effect, thereby preventing the full eruption of the adjacent teeth. Another example in which ridge height and volume is affected is when a maxillary canine erupts into a successfully bone-grafted alveolar cleft. Typically, the canine eruption followed by the orthodontic closure of the cleft dental gap will achieve normal vertical height and an improved arch form (see Chapters 32 and 33; Fig. 5-9).


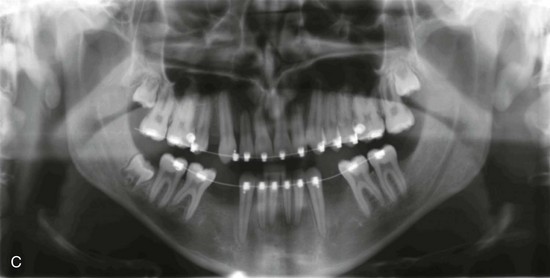
Figure 5-8 This 22-year-old man is congenitally missing the mandibular first and second bicuspids and the right maxillary first bicuspid. He has a maxillary deficiency in combination with relative mandibular excess. He underwent earlier compensating orthodontic treatment, but an Angle Class III, negative overjet, posterior crossbite malocclusion remains. With the congenital absence of the permanent lower bicuspid teeth, there is hypoplasia of the associated alveolar ridge. The congenital absence of the bicuspids causes a ripple effect on the vertical alveolar height of the adjacent teeth. A, Frontal facial view and occlusal views before definitive orthognathic correction and dental rehabilitation. B, Profile facial and cephalometric views before further treatment. C, Panorex radiograph before further treatment.


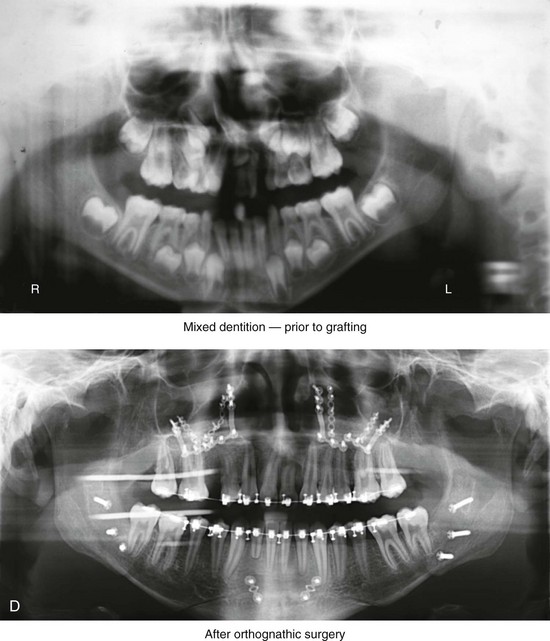
Figure 5-9 A child who was born with van der Woude syndrome, including bilateral cleft lip and palate and lower lip pits, was followed since birth by this surgeon. The child underwent lip and palate repair, including lower lip pit excisions, during childhood. He underwent successful mixed dentition grafting and fistula closure before the eruption of the canines. As a teenager, he demonstrated maxillary hypoplasia with secondary deformities of the mandible. He then underwent a comprehensive orthodontic and orthognathic/intranasal surgical approach that included a standard Le Fort I osteotomy (vertical lengthening, horizontal advancement, and clockwise rotation) with interpositional grafting; bilateral sagittal split ramus osteotomies (clockwise rotation); osseous genioplasty (horizontal advancement); and septoplasty/inferior turbinate reduction/nasal floor recontouring (see Fig 33-3). A, Frontal views with smile before and after reconstruction. B, Profile views before and after reconstruction. C, Occlusal views before mixed dentition bone grafting and fistula closure, with orthodontics in progress before orthognathic surgery, and then after the completion of reconstruction. The placement of a dental implant for the congenitally missing right maxillary bicuspid is planned for when the patient reaches 18 years of age. D, Panorex radiographs of the mixed dentition before cleft bone grafting and then after orthognathic reconstruction. With effective bone grafting of the clefts in the mixed dentition followed by orthodontic closure of the cleft dental gaps, the maxillary canines and central incisors achieved a normal alveolar ridge and periodontium.
Teeth can generally be orthodontically moved through the alveolus without significant damage being done to the bone.71,155 The essential point is to move the tooth through the alveolus rather than outside of it. An exception to this is seen in the presence of active periodontal disease or when the orthodontic forces applied are excessive.128 In this scenario, remodeling with a loss of crestal height and cortical wall dehiscence are likely negative effects to the alveolar bone. If the periodontal disease is first controlled, a normal bone response to therapeutic orthodontic mechanics should be expected (see Chapter 6).26
Before orthodontic treatment is initiated, the individual’s biotype (i.e., the biologic predisposition of the periodontium) should be considered.3,87 This includes an assessment of the adequacy of the gingiva and the alveolus. A thick attachment apparatus and a full-volume alveolus are desired. In an adult (even more so than in a teenager), the movement of teeth outside of the alveolar bone housing or without adequate attached gingiva is poorly tolerated (see Figs. 5-3 and 5-4). In addition, the extrusion of the incisors, the buccal tipping of the maxillary molars, and the labial version of the mandibular incisors should be limited. The adult dentition may also be compromised by wear abrasion facets, the presence of poorly designed and poorly fitted restorations, and the pretreatment loss of the periodontium. In addition to standard orthodontics, ideal treatment may require the following: (1) periodontal evaluation and management; (2) the completion of functional restorations; (3) the surgical correction of any existing jaw discrepancy; and (4) the management of edentulous space. Clarifying the willingness of the patient to maintain a hygiene program before the initiation of treatment is also a benchmark requirement to ensure success.
Mechanical Techniques Used in Orthodontic Force Control
Orthodontic tooth movement is best produced by light continuous force. Orthodontic appliances in clinical practice strive to use light continuous forces that are neither too great nor too variable over time.156 The use of sound mechanical principles; an understanding of the available options with regard to materials, appliance design, and anchorage control; and the prevention of a rapid decrease in the orthodontic forces are more or less achievable.
At times, it may be tempting to pursue an improved occlusion by moving teeth outside of the alveolar housing rather than coordinating treatment with either needed orthognathic procedures or with selective extractions to create necessary space40,74,98,124,137,219,235 (see Figs. 5-3 and 5-4). These two biologic treatment pitfalls contribute to many of the everyday frustrations that are experienced in clinical practice.31,41,47,60–62,67,132,133,149,168,195,212,214 The orthodontist should remain vigilant when assessing the degree of dental compensation introduced while attempting to correct the occlusion.2,24,42,65,82,169,170,194,196,206
Fixed Appliances Used in Orthodontic Treatment
Edward Angle is considered the father of modern orthodontics (see Chapter 2). His treatment was based on the development of appliances from which all contemporary orthodontics stem.15,16,138,228 Current fixed appliances in orthodontics are all variations of Angle’s edgewise appliance system.36,112,233 By the late 1800s, orthodontic fixed appliances depended on a rigid framework that was positioned on the outside circumference of the teeth.214 The teeth were then tied to the rigid framework to move them out to the desired arch form (i.e., expansion) as dictated by the appliance. Angle’s “E” arch was an innovation on earlier designs. Bands were placed on the molar teeth, and a heavy U-shaped arch wire was attached to the banded molars posteriorly. The arch wire was positioned around the labial side of the individual teeth, which were then ligated to it. The wire was gradually unscrewed at the molar location, which resulted in expansion as the arch perimeter increased. The teeth were forced to expand with the labial wire. Unfortunately, the “E” arch was only capable of tipping the teeth into the new position. In addition, it could not precisely differentially position individual teeth over the dental arch. Angle then began to band each individual tooth (not just the molars), and he refined the connection of each banded tooth to the labial arch wire. This allowed him to move each tooth toward the wire at different rates to round out the arch. This technique required ingenuity and a sophisticated mechanical understanding of the process. Accomplishing these maneuvers had a steep learning curve, and it was not easily grasped by clinicians in practice. Angle’s next appliance innovation modified the tube (band) that was placed around individual teeth to include a vertically positioned rectangular slot. The ribbon arch was made of gold wire, and it remained on the labial side of the arch.63 The gold wire was inserted into the slot (bracket) on each banded tooth and held in place with a pin. This improved the efficiency of the alignment of malpositioned teeth. Unfortunately, these appliances still did not achieve consistent bodily movement of the teeth. Tipping of the teeth continued to be problematic. To overcome the deficiencies of the ribbon arch, Angle reoriented the slot (i.e., the shape and location of the bracket on the labial side of each banded tooth) from vertical to horizontal and then inserted a rectangular labial arch wire. He also coined the term edgewise. The edgewise appliance allowed for the improved control of crown and root positioning in all three planes of space. By the early 1930s, Angle’s edgewise appliance became the mainstay of fixed orthodontic appliance therapy.222 The rectangular arch wire was tied into a rectangular slot on the labial side of each tooth with additional wire ligatures; pins were no longer used. This further improved the control of the root position (i.e., it limited tipping) during the movement of the teeth. Eyelets were added to the corners of the bands on each tooth, which could be tied into the labial arch wire as needed for rotation control. Angle was the first clinician to place attachments on each individual tooth to achieve the precise repositioning of each tooth toward a labial arch wire.
Interestingly, Angle’s edgewise appliance system was also able to provide the level of control of root position that was necessary during the process of tooth movement to close an extraction site. If Angle had known that his appliance would be used in this way, he likely would have prevented its development. Charles Tweed, who was initially an Angle disciple, adapted the edgewise appliance for this purpose.214 He did so after he observed significant relapse in many of his own non-extraction (i.e., arch expansion) cases. After he made a decision in favor of extraction, he was able to move the teeth bodily into the bicuspid extraction site with molar anchorage control. The teeth were then able to be retracted into the extraction sites with closing loops, one at a time (canines first, incisors second). In Australia, Begg adopted the ribbon arch appliance (rather than the rectangular wire) to close extraction sites.223 He felt that it provided better control of the root position. He first tipped the anterior teeth with light continuous forces and then used torquing and uprighting auxiliaries to complete tooth alignment. When this was coupled with the detorquing of the incisors, root resorption sometimes occurred.
Orthodontic appliances were further modified to allow for rotational control without the need for additional ligatures.11–14,54,107,108,111,190,191 This was accomplished by using either twin brackets or extension wings with single brackets that could contact the underside of the arch wire. Further modifications included the alteration of the bracket slot dimension, self-ligating brackets, and the addition of lingual appliances. With improvements in dental materials, bonding attachments (i.e., brackets) that were applied directly to the tooth surface (rather than the banding of teeth) became popular. Bonded attachments have no interproximal component and therefore require no separation of teeth, and they are less painful for the patient. They are more efficient for the clinician to put on and to remove, and they are more aesthetic because they are less visible to the casual observer at conversational distance. Clear and tooth-colored appliances have also been developed. An additional advantage to direct bonded brackets and tubes is improved access for oral hygiene and periodontal maintenance.
Contemporary edgewise appliances still remain an integral component of orthodontic treatment.99 Brackets or tubes are customized for each individual tooth, thereby allowing for the minimum number of bends in the arch wire that are necessary to produce an ideal arrangement of the teeth. This “straight wire” approach requires some bending of the wire to allow for a passive fit of the arch wire when the teeth are ideally aligned.
Bracket Materials and Design
Orthodontic brackets are generally made from various classes of stainless steel.99,112,140 More often than not, they are made by a metal injection molding process rather than milling. Clear brackets that are made of reinforced resin composite or alumina have become popular; this aesthetic option is often requested by the patient. Friction forces created between metal arch wires and ceramic brackets have largely been overcome by designs that incorporate a metal slot in the bracket or by reducing surface roughness within the slot. Self-ligating brackets are classified as either passive or active, depending on how the wire is held in the bracket slot. Both types of self-ligating brackets can offer low friction with a reduction in the anchorage requirements and less chair time without a loss in the quality of the results. The term prescription is used in orthodontics to describe the angulation, inclination, and offset values used in the bracket system to treat a particular patient’s malocclusion. Traditional prescriptions have been based on the systems of either Roth or Andrews, although many variations exist.12–14,190,191 Current prescriptions often use newer arch wire and bracket technology and involve claims of improved treatment efficiency. For example, SureSmile uses a variety of prescription brackets in conjunction with computer-generated, pre-bent prescription wires for faster and more accurate detailing and finishing. The Insignia system also uses a computer to mill special brackets for each tooth of each patient. The brackets are then bonded indirectly to each tooth with the use of transfer jigs. The Incognito system creates custom-made gold brackets for lingual orthodontics. This method of tooth movement has gained popularity in Europe, and it is also used in the United States. Problems with all of these prescription techniques may arise if they are improperly used by a clinician for an individual with a jaw deformity. If attempts are made to correct the malocclusion by orthodontic mechanics alone, the preset wires will result in excessive dental compensation with injury to the dentition and the surrounding periodontium as the teeth are compressed against the cortical plates and pulled out of the alveolar housing. However, when properly incorporated into a comprehensive orthodontic and orthognathic treatment plan, these newer techniques may improve results and involve reduced treatment times.
Cements and Adhesives
The spectrum of cements and adhesives used in orthodontic practice includes self-etching primers, wet bonding, fluoride release to prevent demineralization, light-cured band cements, colored cements, and curing lights.* Self-etching primers are now available for orthodontics. They are relatively moisture insensitive, but they may have reduced bond strength as compared with the conventional acid-etch technique. The wet bonding products (i.e., modified resin-filled glass ionomer adhesives) that are currently available show lower bond strengths with a higher failure rate than conventional composite, but they are generally acceptable for accomplishing needed objectives. Fixed-appliance orthodontics can lead to problems with oral hygiene, increased plaque accumulation, and altered plaque ecology, which may lead to enamel demineralization. Fluoride in the oral environment has been shown to lead to altered bacterial function, reduced enamel dissolution, and increased remineralization. Fluoride-releasing bonding cements have been shown to reduce the depth and extent of demineralization microscopically. Unfortunately, long-term success with regard to the limiting of demineralization has not been significantly demonstrated. Conventional glass ionomers are still the preferred material for use beneath molar bands to limit demineralization as compared with cements that do not release fluoride. Polyacid-modified composite cements are now available to secure bands, and they offer a light-cured snap set. These new cements appear to clinically perform as well as conventional glass ionomer cement, but, because they do not bond to enamel, they may result in greater demineralization in some patients. High-performance halogen curing lights are now available; these contain bulbs that do not degrade over time, and they have curing times of 5 to 8 seconds. Plasma arc lights are also available; these can cure adhesive in 3 to 5 seconds, but they have the disadvantage of generating much heat during the process. Currently available light-emitting diode curing lights are gaining popularity; they generate low levels of heat, and they are cordless.
Arch Wire (Materials and Design)
Before the 1950s, precious metal alloys were the commonly used materials for orthodontic arch wires. Stainless steel alloys surpassed gold as the preferred arch wire materials during the 1940s to reduce costs, to provide higher-yield strength and stiffness, and to result in higher elastic modulus and flexibility with improved properties to orthodontically close dental space. These alloys generally included platinum and palladium, which were often mixed with gold and copper. During the 1970s, NASA developed a nickel-titanium alloy that was easily deformed at low temperatures but that was able to memorize its original shape with warming (i.e., the thermal dynamic shape memory effect). The term active has been coined to describe this phenomenon. Nitinol was then developed as a cheaper, stabilizing “passive” version of this material, and it has been found to be useful as an orthodontic wire, because it still possessed low stiffness and good recovery when it was used as an aligning or intermediate arch wire. Currently, two active nickel-titanium alloy forms of this material are used in orthodontic practice, because they both possess excellent elastic properties. This includes the strength-induced superelastic wires and the thermally induced superelastic wires. The term superelastic refers to a material that can undergo martensite-austenite phase transformations, which are generated by either mechanical stress or heat. The crystal structure of the wire changes with mechanical deformation, which results in a unique non-linear stress–strain curve in which stress is independent of applied strain. In theory, the force levels that are used to deform the wire to ligate it into the bracket are less than those created by the wire as it attempts to return to its original shape. This offers the advantage of low continuous forces applied to the teeth through the entire reforming process, despite the wire being tied into teeth that are severely displaced. The thermally induced superelastic wire undergoes phase change as the temperature changes from the ambient temperature to an individual’s body temperature. The temperature at which the transformation takes place can be specifically controlled during the manufacturing process to match the intraoral temperature requirements. When using thermally induced superelastic wires, the wire is ligated in place during its low-stiffness phase; then, with the heat of the oral cavity, transformation is induced, thereby returning it to its predetermined austenitic form. The theoretical advantage of both of these superelastic wire types is that they are able to provide a physiologic low and continuous force that can be used for leveling and aligning the teeth. Although individual practitioners are advocates of these wires as compared with the more traditional nickel titanium or multi-strand stainless steel wires, significant differences in the speed of alignment between the wire types has yet to be proven.42
Intra-Oral Auxiliaries to Brackets and Arch Wires
The definition of friction is the resistive force between surfaces that oppose motion. In orthodontic tooth movement, friction results from the interaction of an arch wire with the walls of an orthodontic bracket or a ligature. It is now known that friction is only a small part of the resistance to movement as a bracket slides along in arch wire.19,39,64,122,208 In orthodontics, tooth and bracket movements have major interactions that involve the teeth, the PDLs, the alveolar bone, and the forces of mastication. For a bracket that is attached to a tooth to move relative to a wire in the bracket slot, the tooth must move. The tooth’s resistance to being moved contributes to its resistance to sliding. This is particularly true when bodily movement rather than tipping is desired. Binding and notching will occur in the clinical setting but not in laboratory simulations, where only brackets and wires are involved. In review, clinical studies and the analysis of laboratory findings support the view that, in orthodontic practice, resistance to sliding has little to do with friction and instead is largely a binding-and-release phenomenon. Interestingly, resistance to sliding is about the same with both conventional and self-ligating brackets.39
Removable Appliances Used in Orthodontic Treatment
Functional appliances represent a second category of removable design (although they may also be fixed). They are constructed primarily with the hope of changing the position of the mandible (i.e., to hold the lower jaw open and to posture it forward) as well as to limit or enhance the eruption of maxillary molars. The history of functional appliances can be traced back to the mid 1800s, when Norman Kingsley introduced the “bite-jump” appliance (1879).114 The “monobloc,” which was developed by Robin in the United States during the early 1900s, was followed by the “activator,” which was developed in Norway by Andresen during the 1920s; both of these devices became widely accepted. Harvold reintroduced removable functional appliances to North American orthodontists during the 1960s, around the same time that the use of fixed appliances finally began to catch on throughout Europe. Harvold’s animal model studies confirmed that mandibular posture did in fact affect maxillomandibular growth92–97 (see Chapter 4). This led to a belief that functional appliances could be used to “alter back” abnormal jaw growth tendencies. During the 1970s, the Frankel regulator by Rolf Frankel of East Germany popularized the concept of a tissue-borne functional appliance. By the 1980s, William Clark of Scotland introduced the Twin Block, which is a two-piece, tooth-borne appliance. The Twin Block was easier to wear than the Frankel regulator, and it was designed to accomplish the same objectives. Pancherz then popularized the Herbst fixed functional appliance during the 1980s, because it circumvented the problem of patient compliance. This appliance was originally developed by Emil Herbst at the beginning of the 20th century. Proffit has stated that, despite continued strong advocates of functional appliances, “the results of human clinical trials and retrospective analysis have not confirmed sufficient success with the use of functional appliances to make them mainstay treatment.”210 Although there is limited evidence-based research to support functional appliances, their continued use in everyday orthodontic practice remains a reality.
Siara-Olds and colleagues recently completed a prospective, randomized, controlled clinical study to assess the early and long-term treatment outcomes of tooth-borne functional appliances.201 They tested the use of four different functional appliances in a treatment group, and they also followed a group of untreated control subjects with Class II malocclusions. The treatment group (n = 80) was subdivided evenly into four subgroups in accordance with the type of functional appliance being used: the Bionator (n = 20); the Herbst fixed functional appliance (n = 20); the Twin Block (n = 20); and the mandibular anterior repositioning appliance (n = 20). The functional appliance treatment was carried out on individuals with Class II malocclusions who were between the ages of 8 and 12 years. Each randomized Class II malocclusion subject received comprehensive orthodontic treatment with bands and brackets to complete their treatment after the use of the specific functional appliance. The investigators compared lateral cephalometric radiographs that were taken at standard intervals (i.e., before treatment, after functional appliance therapy, and after the completion of comprehensive orthodontics). The four subgroups were also compared with an untreated control group who had similar Class II malocclusions who were not treated with functional appliances, bands, or brackets. The results of the study confirmed that the use of the functional appliances did not alter long-term mandibular growth patterns as compared with the results seen among the control subjects with Class II malocclusions. Interestingly, the use of a functional appliance in combination with bands and brackets did demonstrate effects, including the following: (1) the restriction of maxillary horizontal growth; (2) the creation of a steeper occlusal plane (with the Herbst and mandibular anterior repositioning appliances); and (3) the steepening of the mandibular plane angle (i.e., clockwise rotation) with the labial version of the mandibular incisors with the Twin Block appliance.201 In review, the study by Siara-Olds, et al. confirms that functional appliances for the purpose of correcting micrognathia have negligible impact on the growth potential of the mandible long term.
A third category of removable appliances are used for the retention of the achieved orthodontic results. A spectrum of retention appliance designs are used in everyday orthodontic practice. With regard to the issue of retention, Melsen stated the following: “We [orthodontists] deliver the product, but the final result, as when you buy a car, depends on life-long retention and life-long maintenance. Other than diamonds, everything has to be maintained; true stability only occurs post mortem.”142
Accelerated Osteogenic Orthodontics
Finding a technique that enhances the speed of orthodontic tooth movement without causing damage has been an objective of clinicians for more than 100 years. Attempts to modify the balance between resorption and deposition and to bypass the waiting time for the alveolar cortex to resorb and thus move the teeth faster without causing irreversible damage to the periodontium has been the focus of much research over the years.28,29,49,78,79,81,90,101,200,217,218,234 Corticotomy, which is the intentional injury of the cortical bone, was described in the mid 1800s as a surgical approach to correct malocclusion. Osteotomies into the cortical alveolar bone were made, and then the teeth were splinted into new positions. This concept received renewed attention when Kole published a series of clinical articles describing a different approach to the treatment of orthodontic patients.116,117 In 1975, Duker used a dog model to demonstrate rapid segmental alveolar movement after corticotomy.68 In 1986, Anholm and colleagues also described corticotomy-facilitated orthodontics in clinical practice.17 William and Thomas Wilcko further modified the protocol for corticotomy-facilitated orthodontics; they trademarked their technique in 1998.230,231 That same year, the Wilcko brothers received an endorsement for their technique from the American Academy of Periodontics. Their technique involves elevating a full-thickness mucosal flap off of the alveolar plate (either labial or lingual/palatal) directly over the teeth to be moved. They then place corticotomies (perforations) through the alveolar bone adjacent to the teeth to be moved with the use of a burr on a handpiece. The Wilckos also recommend placing bone graft material over the surgical perforations in the cortical plate to improve alveolar volume. They then replace the mucosal flap into its anatomic location with sutures. They further claim that the technique enhances difficult tooth movement (i.e., molar intrusion) and that it can provide relative anchorage (i.e., a corticotomy limited to the anterior region will provide relative anchorage from the posterior teeth). The theory behind this technique is that injury to the bone (i.e., the cortical perforations) creates a “regional acceleratory phenomenon.”230As a result, the body rapidly sends cells to the site to heal the injured bone. This surge in cellular healing activity is thought to promote faster tooth movement. The Wilckos called their technique accelerated osteogenic orthodontics.230
The animal research by Lino and colleagues130 and the experimental study completed by Sebaoun and colleagues197 describe a plausible biologic explanation for the greater speed of tooth movement that is seen with these techniques. Lino’s group used adult beagle dogs (n = 12). The mandibular right and left first premolars were to be moved mesially with the use of a calibrated spring that attached to the mandibular canines. On one side of each mandible, a flap was elevated, and holes were placed in the alveolar bone (corticotomies) to create a regional acceleratory phenomenon. No corticotomy was performed on the opposite (control) side. The PDL on the mesial (compression) side of each premolar was evaluated histologically at weeks 1, 2, 4, and 8. In addition, the amount of mesial bicuspid tooth movement on each side (i.e., the experimental side versus the control side) was compared at the 8-week interval. Histologic comparisons of the two sides showed very distinct differences. At 1 week, bicuspid tooth compression produced a typical hyalinization of the PDL on both sides. “Hyaline formation” within the PDL, which is referred to as a “sterile necrosis,” occurs in response to compressive forces. This is the expected response when significant compressive forces are produced in the PDL. It is known that this sterile necrosis interferes with bone resorption; thus, at the 1-week interval, no tooth movement was experienced on either side. At 2 weeks, hyaline was still present on the control side, so no bone resorption of the tooth socket wall had yet occurred; however, root resorption was evident. At 2 weeks, on the experimental (corticotomy) side, the hyaline had already been removed from the PDL. Presumably, macrophages (the presence of which had been stimulated by the regional acceleratory phenomenon) were in place very early to perform this removal and thus, in the process, no root resorption occurred. At 4 and 8 weeks after the initiation of treatment on the control (non-corticotomy) side, the hyaline had finally been removed and the alveolar bone resorption had begun, thereby allowing mesial bicuspid tooth movement to proceed. During this waiting period, extensive root resorption had occurred on the control side. Interestingly, at the 4- and 8-week post-treatment intervals on the experimental (corticotomy) side, there was no hyaline present in the periodontium, the socket wall had appropriately resorbed, and the bicuspid tooth was able to move mesially without root resorption.
In the rat model, Sebaoun and colleagues studied the alveolar response to corticotomy as a function of time and proximity to the surgical injury.197 Maxillary buccal and palatal cortical plates were injured (corticotomy) in healthy adult rats (n = 36) adjacent to the upper left first molars. Twenty-four of the animals were euthanized at 3, 7, and 11 weeks after injury.
In review, it appears that the completion of a corticotomy of the alveolar process immediately brings macrophages into the field of bony injury.116 The macrophages are then able to remove the hyaline (necrotic material) from the periodontium more quickly than occurs in a non-corticotomy setting. The early presence of macrophages can explain the rapid degree of bone resorption and minimal root resorption during orthodontic tooth movement that was documented by Lino and colleagues. When Lino’s group compared the amount of tooth movement in their experimental and control groups, the teeth on the corticotomy side moved twice as fast as the teeth on the control side. The enhanced tooth movement after corticotomy should continue as long as the surgical site healing remains in progress (only approximately 2 to 3 months). The potential for morbidity to the teeth and periodontium that is associated with the surgical procedure, must be considered in light of any advantage of reduced time to reach treatment objectives.
Temporary Skeletal Anchorage in Orthodontics
TADs that are made of titanium and temporarily fixed into alveolar bone have been shown to provide effective supplemental or “maximum” anchorage for the movement of teeth while avoiding unwanted negative reciprocal responses in the dentition.* Retromolar titanium (dental) implants simply for the purpose of temporary skeletal anchorage to facilitate orthodontic movement of the teeth were first placed by Roberts and colleagues in 1989.185–187 Wehrbein and Merz placed titanium implants directly into the hard palate and then tied the molar teeth to them.224,225 The purpose of the temporary hard-palate implants was to prevent the movement of the molar teeth that were to be used as direct anchorage for the distal movement of anterior teeth into bicuspid extraction sites. Standard titanium bone fixation plates (i.e., mini-plates) were next used as TADs. The mini-plates were fixed to the zygomatic buttress with titanium screws. The end of the titanium plate then perforated through the oral mucosa to provide a point of attachment for orthodontic wires, springs, coils, and elastics.
• The retraction and realignment of the anterior teeth without the need for posterior support (anchorage)
• The closing of edentulous spaces after extraction
• The correction of the midline in patients with missing posterior teeth
• The reestablishment of proper molar positions (i.e., uprighting tipped teeth) for use as abutments
• The intrusion and extrusion of teeth (e.g., to intrude maxillary molars in an attempt to close anterior open bites)
• The protraction and retraction of teeth
• The stabilization of teeth that have reduced alveolar bone support
• The application of orthopedic traction to the maxilla or mandible in the growing individual in an attempts to alter jaw growth
References
1. Ackerman, H, Proffit, WR. The characteristics of malocclusion: a modern approach to classification and diagnosis. Am J Orthod. 1969; 56:443–454.
2. Ackerman, JL, Proffit, WR. Communication in orthodontic treatment planning: bioethical and informed consent issues. Angle Orthod. 1995; 65:253.
3. Ackerman, JL, Proffit, WR. Soft tissue limitations in orthodontic treatment. Angle Orthod. 1997; 67:327–336.
4. Ackerman, M. Evidence-based orthodontics for the 21st century. J Am Dent Assoc. 2004; 135:162–167.
5. Adachi, H, Igarashi, K, Mitani, H, Shinoda, H. Effects of topical administration of a bisphosphonate (risedronate) on orthodontic tooth movements in rats. J Dent Res. 1994; 73:1478–1484.
6. Adamides, IP, Spyropoulos, MN. The effects of lymphadenoid hypertrophy on the position of the tongue, the mandible and the hyoid bone. Eur J Orthod. 1983; 5:287–294.
7. Adell, R, Hansson, BO, Brånemark, PI, Breine, U. Intra-osseous anchorage of dental prostheses. II. Review of clinical approaches. Scand J Plast Reconstr Surg. 1970; 4:19–34.
8. Al Yami, EA, Kuijpers-Jagtman, AM, Van’t Hof, MA. Stability of orthodontic treatment outcome: Follow-up until 10 years post-retention. Am J Orthod Dentofacial Orthop. 1999; 115:300–304.
9. Albino, JE, Lewis, EA, Slakter, MJ. Examiner reliability for two methods of assessing malocclusion. Angle Orthod. 1978; 48:297–302.
10. Al-Munajed, MK, Gordon, PH, McCabe, JF. The use of a cyanoacrylate adhesive for bonding orthodontic brackets: an ex-vivo study. J Orthod. 2000; 27:255–260.
11. Andrews, LF. The six keys to normal occlusion. Am J Orthod. 1972; 63:296–309.
12. Andrews, LF. The straight-wire appliance, origin, controversy, commentary. J Clin Orthod. 1976; 10:99–114.
13. Andrews, LF. The straight-wire appliance: extraction brackets and classification of treatment. J Clin Orthod. 1976; 10:360–379.
14. Andrews, LF. Straight wire: the concept and appliance, San Diego. LA Wells Co. 2003.
15. Angle, EH. Treatment of malocclusion of the teeth, ed 7. Philadelphia: SS White; 1907.
16. Angle, EH. The latest and best in orthodontic mechanism. Dent Cosmos. 1928; 70:1143–1158.
17. Anholm, JM, Crites, DA, Hoff, R, Rathbun, WE. Corticotomy-facilitated orthodontics. CDA J. 1986; 14:7–11.
18. Aronowitz, HI. Orthodontics and occlusion: a historical perspective. J Calif Dent Assoc. 1996; 24:16–18.
19. Articolo, LC, Kusy, RP. Influence of angulation on the resistance to sliding in fixed appliances. Am J Orthod Dentofacial Orthop. 1999; 115:39–51.
20. Asbell, MB. A brief history of orthodontics. Am J Orthod Dentofacial Orthop. 1990; 98:176–183.
21. Bae, SM, Park, HS, Kyung, HM, et al. Clinical application of micro-implant anchorage. J Clin Orthod. 2002; 36:298–302.
22. Baker, CR. Orthodontic profiles. Am J Orthod. 1957; 43:210–218.
23. Bartzela, T, Turp, J, Motschall, E, Maltha, J. Medication effect on the rate of orthodontic tooth movement: a systematic literature. Am J Orthod Dentofacial Orthop. 2009; 135:16–26.
24. Baumrind, S, Korn, EL, Boyd, RL, Maxwell, R. The decision to extract: Part 1–Interclinican agreement. Am J Orthod Dentofacial Orthop. 1996; 109:297–309.
25. Begg, PR, Kesling, PC. The differential force method of orthodontic treatment. Am J Orthod. 1977; 71:1–39.
26. Bibb, CA. Occlusal evaluation and therapy in the management of periodontal disease. In: Newman MG, Takei HH, Carranza FA, eds. Carranza’s clinical periodontology. ed 9. Philadelphia: W. B. Saunders Company; 2002:698–701.
27. Block, MS, Hoffman, DR. A new device for absolute anchorage for orthodontics. Am J Orthod Dentofacial Orthop. 1995; 107:251–258.
28. Bogoch, E, Gschwend, N, Rahn, B, et al. Healing of cancellous bone osteotomy in rabbits–Part I: Regulation of bone volume and the regional acceleratory phenomenon in normal bone. J Orthop Res. 1993; 11:285–291.
29. Bogoch, E, Gschwend, N, Rahn, B, et al. Healing of cancellous bone osteotomy in rabbits–Part II: Local reversal of arthritis-induced osteopenia after osteotomy. J Orthop Res. 1993; 11:292–298.
30. Bohl, MV, Maltha, JC, Von den Hoff, JW, Kuijpers-Jagtman, AM. Focal hyalinization during experimental tooth movement in beagle dogs. Am J Orthod Dentofacial Orthop. 2004; 125:615–623.
31. Bolton, WA. Disharmony in tooth size and its relation to the analysis and treatment of malocclusion. Angle Orthod. 1958; 28:113–130.
32. Bowman, J. One-stage versus two-stage treatment: are two really necessary? Am J Orthod Dentofacial Orthop. 1998; 113:111–116.
33. Brånemark, PI, Adell, R, Breine, U, et al. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969; 3:81–100.
34. Brezniak, N, Wasserstein, A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J Orthod Dentofac Orthop. 1993; 103:138–146.
35. Brodie, AG. Orthodontic history and what it teaches. Angle Orthod. 1934; 4:85–97.
36. Brodie, AG. Orthodontic concepts prior to the death of Edward H Angle. Angle Orthod. 1956; 26:144–154.
37. Brudvik, P, Rygh, P. The initial phase of orthodontic root resorption incident to local compression of periodontal ligament. Eur J Orthod. 1993; 15:249–263.
38. Buonocore, MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955; 34:849–853.
39. Burrow, JS. Friction and resistance to sliding in orthodontics: a critical review. Am J Orthod Dentofacial Orthop. 2009; 135:442–447.
40. Cain, KK, Rugh, JD, Hatch, JP, et al. Readiness for orthognathic surgery: a survey of practitioner opinion. Int J Adult Orthodon Orthognath Surg. 2002; 17:7–11.
41. Carey, CW. Lower arch dimension and tooth size. Am J Orthod. 1949; 35:762–775.
42. Carranza, FA. Bone loss and patterns of bone destructions. In: Newman MG, Takei HH, Carranza FA, eds. Carranza’s clinical periodontology. ed 9. Philadelphia: W. B. Saunders Company; 2002:362.
43. Case, CS. Principles of occlusion and dentofacial relations. Dent Items Int. 1905; 27:489.
44. Case, CS. A practical treatise on the techniques and principles of dental orthopedia and prosthetic correction of cleft palate, ed 2. Chicago: CS Case; 1922.
45. Casto, FM. The trend of orthodontic treatment. Int J Orthod Oral Surg Rad. 1930; 16:1078–1092.
46. Casto, FM. A historical sketch of orthodontia. Dent Cosmos. 1934; 76:111–135.
47. Cetlin, NM, Ten Hoeve, AJ. Nonextraction treatment. J Clin Orthod. 1983; 17:396–413.
48. Chapman, H. Orthodontics: fifty years in retrospect. Am J Orthod. 1955; 41:421–442.
49. Chung, KR, Oh, MY, Ko, SJ. Corticotomy-assisted orthodontics. J Clin Orthod. 2001; 35:331–339.
50. Cleall, JF. Deglutition: a study of form and function. Am J Orthod. 1965; 51:161–182.
51. Cooper, RB, Gross, M, Hamula, W. Direct bonding with light cured adhesive precoated brackets. J Clin Orthod. 1992; 26:477–479.
52. Costa, A, Raffaini, M, Melsen, B. Microscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998; 13:201–209.
53. Creekmore, TD, Ecklund, MK. The possibilities of skeletal anchorage. J Clin Orthod. 1983; 17:266–269.
54. Creekmore, TD, Kunik, RL. Straight wire: the next generation. Am J Orthod Dentofacial Orthop. 1993; 104:8–20.
55. Cryer, M. Typical and atypical occlusion of teeth. Dent Cosmos. 1904; 46:713.
56. Cueto, HI. A little bit of history: the first direct bonding in orthodontia. Am J Orthod Dentofacial Orthop. 1990; 98:276–277.
57. Deguchi, T, Takano-Yamamoto, T, Kanomi, R, et al. The use of small titanium screws for orthodontic anchorage. J Dent Res. 2003; 82:377–381.
58. Delaire, J. Considerations on facial growth (particularly of the maxilla): therapeutic deductions. Rev Stomatol Chir Maxillofac. 1971; 72:57–76.
59. Delaire, J. La croissance maxillaire: deductions therapeutiques. Trans Eur Orthod Soc. 1971; 81–102.
60. Dewel, BF. Second premolar extraction in orthodontics: principles, procedures, and case analysis. Am J Orthod. 1955; 441:107–120.
61. Dewel, BF. The Case-Dewey-Cryer extraction debate. Am J Orthod. 1964; 50:862–865.
62. Dewel, BF. Editorial: Orthodontosie, orthodontics, or dentofacial orthopedics. Am J Orthod. 1976; 70:328.
63. Dewel, BF. The ribbon arch: its influence in the development of orthodontic appliances. Angle Orthod. 1981; 51:263–268.
64. DiBiase, AT, Nasr, IH, Scott, P, Cobourne, MT. Duration of treatment and occlusal outcome using Damon3 self-ligated and conventional orthodontic bracket systems in extraction patients: a prospective randomized clinical trial. Am J Orthod Dentofacial Orthop. 2011; 139:e111–e116.
65. Dowling, P, Espeland, L, Krogstad, O, et al. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:146–152.
66. Driel, WD, Leeuwen, EJ, Hoff, JW, et al. Time-dependent mechanical behavior of the periodontal ligament. Proc Inst Mech Eng H. 2000; 214:497–504.
67. Drobocky, OB, Smith, RJ. Changes in facial profile during orthodontic treatment with extraction of four first premolars. Am J Orthod Dentofacial Orthop. 1989; 95(5):220–230.
68. Düker, J. Experimental animal research into segmental alveolar movement after corticotomy. J Maxillofac Surg. 1975; 3:81–84.
69. Eby, JD. Clinical approach to orthodontic therapy. Am J Orthod. 1949; 35:407–424.
70. Edler, RJ. Problems in the orthodontic management of orthognathic cases. Eur J Orthod. 1990; 12:420–437.
71. Engström, C, Granström, G, Thilander, B. Effect of orthodontic force on periodontal tissue metabolism: a histologic and biochemical study in normal and hypocalcemic young rats. Am J Orthod Dentofacial Orthop. 1988; 93:486–495.
72. Fastlicht, S. Evolution of the universal appliance. Am J Orthod. 1950; 36:433–444.
73. Ferguson, J. Comment on two-phase treatment. Am J Orthod Dentofacial Orthop. 1996; 110:14–15.
74. Fink, DF, Smith, RJ. The duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992; 102:45–51.
75. Freng, A, Kvam, E. Facial sagittal growth following partial basal resection of the nasal septum: a retrospective study in man. Eur J Orthod. 1979; 1:89–96.
76. Freng, A. Dentofacial development in the long-lasting nasal stenosis. Scand J Dent Res. 1979; 87:260–267.
77. Freudenthaler, JW, Bantleon, H-P, Haas, R. Bicortical titanium screws for critical orthodontic anchorage in the mandible: a preliminary report on clinical applications. Clin Oral Implants Res. 2001; 12:358–363.
78. Frost, HM. The biology of fracture healing: an overview for clinicians. Part I. Clin Orthop Related Res. 1989; 248:283–293.
79. Frost, HM. The biology of fracture healing: an overview for clinicians. Part II. Clin Orthop Relat Res. 1989; 248:294–309.
80. Gainsforth, BL, Higley, LB. A study of orthodontic anchorage possibilities in basal bone. Am J Orthod Oral Surg. 1945; 31:406–417.
81. Gantes, B, Rathbun, E, Anholm, M. Effects on the periodontium following corticotomy-facilitated orthodontics: case reports. J Periodontol. 1990; 61:234–238.
82. Generson, RM, Porter, JM, Zell, A, Stratigos, GT. Combined surgical and orthodontic management of anterior open bite using corticotomy. J Oral Surg. 1978; 36:216–219.
83. Gianelly, A. One-phase versus two-phase treatment. Am J Orthod Dentofacial Orthop. 1995; 108:556–559.
84. Goldie, RS, King, GJ. Root resorption and tooth movement in orthodontically treated, calcium-deficient, and lactating rats. Am J Orthod. 1984; 85:424–430.
85. Goldstein, A. The clinical testing of orthodontic results. Am J Orthod. 1965; 51:723–755.
86. Gottlieb, EL. Orthodontics in the year 2000. J Clin Orthod. 2000; 34:9–10.
87. Graber, TM, Vanarsdall, RL. Orthodontics: current principles and techniques. St. Louis: Mosby; 2000.
88. Graf, H, Grassl, J, Aeberhard, H. A method for measurement of occlusal force in three directions. Helv Odontol Acta. 1974; 18:7–11.
89. Guilford, SH. Orthodontia: malposition of human teeth. Philadelphia: Spangler & Davis; 1889.
90. Hajji, SS. The influence of accelerated osteogenic response on mandibular decrowding (thesis). St. Louis: St. Louis University; 2000.
91. Hannuksela, A. The effect of moderate and severe atopy on the facial skeleton. Eur J Orthod. 1981; 3:187–193.
92. Harvold, EP. The role of function in the etiology and treatment of malocclusion. Am J Orthod. 1968; 54:883–898.
93. Harvold, EP, Chierici, G, Vargervik, K. Experiments on the development of dental malocclusions. Am J Orthod. 1972; 61:38–44.
94. Harvold, EP, Vargervik, K, Chierici, G. Primate experiments on oral sensation and dental malocclusion. Am J Orthod Dentofacial Orthop. 1973; 63:494–508.
95. Harvold, EP. Centric relation: a study of pressure and tension systems in bone modeling and mandibular positioning. Dent Clin North Am. 1975; 19:473–484.
96. Harvold, EP, Chierici, G, Vargervik, K. Primate experiments on oral sensation and dental malocclusions. Am J Orthod. 1981; 79:359–372.
97. Harvold EP, Chierici G, Vargervik K, eds. Treatment of hemifacial microsomia. New York: Alan R. Liss, 1983.
98. Hernández-Alfaro, F, Guijarro-Martínez, R, Molina-Coral, A, Badía-Escriche, C. “Surgery first” in bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 2011; 69:e201–e207.
99. Holdaway, RA. Bracket angulation as applied to the edgewise appliance. Angle Orthod. 1952; 22:227–236.
100. Hsieh, TJ, Pinskaya, Y, Roberts, WE. Assessment of orthodontic treatment outcomes: early treatment versus late treatment. Angle Orthod. 2005; 75:162–170.
101. Hwang, HS, Lee, KH. Intrusion of overerupted molars by corticotomy and magnets. Am J Orthod Dentofacial Orthop. 2001; 120:209–215.
102. Igarashi, K, Mitani, H, Adachi, H, Shinoda, H. Anchorage and retentive effects of a bisphosphate (AHBuBP) on tooth movements in rats. Am J Orthod Dentofacial Orthop. 1994; 106:279–289.
103. Igarashi, K, Adachi, H, Mitani, H, Shinoda, H. Inhibitory effect of the topical administration on root resorption incident to orthodontic tooth movement in rats. J Dent Res. 1996; 75:1644–1649.
104. Ismail, SFH, Johal, AS. The role of implants in orthodontics. J Orthod. 2002; 29:239–245.
105. Itoh, T, Matsuo, N, Fukushima, T, et al. Effect of contamination and etching on enamel bond strength of a new light-cured glass ionomer cement. Angle Orthod. 1999; 69:450–456.
106. Janssens, F, Swennen, G, Dujardin, T, et al. Use of an onplant as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2002; 122:566–570.
107. Jarabak, JR, Fizzell, JA. Technique and treatment with the light-wire appliances: light, differential forces in orthodontics. St. Louis: Mosby; 1963.
108. Johnson, JE. A new orthodontic mechanism: the twinwire automatic appliance. J Am Dent Assoc. 1932; 19:997–1011.
109. Kanomi, R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997; 31:763–767.
110. Kapila, S, Conley, RS, Harrell, WE, Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011; 40:24–34.
111. Kesling, PC. Dynamics of the tip-edge bracket. Am J Orthod Dentofacial Orthop. 1989; 96:16–25.
112. Kesling, PC. The edgewise slot: Angle’s orthodontic albatross. World J Orthod. 2000; 1:142–151.
113. Kim, TW, Yoshida, Y, Yokoya, K, Sasaki, T. An ultrastructural study of the effects of bisphosphonate administration on osteoclastic bone resorption during relapse of experimentally moved rat molars. Am J Orthod Dentofacial Orthop. 1999; 115:645–653.
114. Kingsley, NW. A treatise on oral deformities (as a branch of mechanical surgery). New York: Appleton & Company; 1880.
115. Kloehn, SJ. Mixed dentition treatment. Angle Orthod. 1950; 20:75–96.
116. Kole, H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959; 12:515–529.
117. Korkhaus, G. Handbuch de Zahnheilkunde. Munchen: J. F. Bergmann; 1939.
118. Kraus, BS, Jordan, RE, Abrams, L. Dental anatomy and occlusion. Baltimore: Williams & Wilkins Company; 1969.
119. Kreiborg, S, Jensen, BL, Møller, E, Björk, A. Craniofacial growth in a case of congenital muscular dystrophy. Am J Orthod. 1978; 74:207–215.
120. Krishnan, PH, Gupta, DS, Sharma, VP. Application of cyanoacrylate in orthodontics. J Polymer Materials. 1994; 11:299–300.
121. Kurol, J, Owman-Moll, P. Hyalinization and root resorption during early orthodontic tooth movement in adolescents. Angle Orthod. 1998; 68:161–165.
122. Kusy, RP, Whitley, JQ. Influence of archwire and bracket dimensions on sliding mechanics: derivations and determinations of the critical contact angles for binding. Eur J Orthod. 1999; 21:199–208.
123. Lee, JS, Park, HS, Kyung, HM. Micro-implant anchorage for lingual treatment of a skeletal class II malocclusion. J Clin Orthod. 2001; 35:643–647.
124. Lee, RT. The benefits of post-surgical orthodontic treatment. Br J Orthod. 1994; 21:265–274.
125. Leeuwen, EJ, Maltha, JC, Kuijpers-Jagtman, AM. Tooth movement with light continuous and discontinuous forces in beagle dogs. Eur J Oral Sci. 1999; 107:468–474.
126. Lewis, PD. Space closure in extraction cases. Am J Orthod. 1950; 36:172–191.
127. Linder-Aronson, S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. A biometric, rhino-manometric and cephalometro-radiography study on children with and without adenoids. Acta Otolaryngol Suppl. 1970; 265:1–132.
128. Lindskog, S, Lilja, E. Scanning electron microscopic study of orthodontically induced injuries to the periodontal membrane. Scand J Dent Res. 1984; 92:334–343.
129. Linkow, LI. The endosseous blade implant and its use in orthodontics. Int J Orthod. 1969; 18:149–154.
130. Lino, S, Sakoda, S, Ito, G, et al. Acceleration of orthodontic tooth movement by alveolar corticotomy in the dog. Am J Orthod Dentofacial Orthop. 2007; 131:448. e1–448. e8.
131. Liou, EJW, Pai, BCJ, Lin, JCY. Do miniscrews remain stationary under orthodontic forces? Am J Orthod Dentofacial Orthop. 2004; 126:42–47.
132. Livieratos, FA, Johnston, LE, Jr. A comparison of one-stage and two-stage nonextraction alternatives in matched Class II samples. Am J Orthod Dentofacial Orthop. 1995; 108:118–131.
133. Logan, LR. Second premolar extraction in Class I and Class II. Am J Orthod. 1973; 63:115–147.
134. Lundström, A, The importance of genetic and non-genetic factors in the facial skeleton studied in 100 pairs of twins. The Hague: European Orthodontic Society. 1954:92–102.
135. Lundström, A, Woodside, DG. Individual variation in growth directions expressed at the chin and the midface. Eur J Orthod. 1980; 2:65–79.
136. Lundström, A. Nature versus nurture in dento-facial variation. Eur J Orthod. 1984; 6:77–91.
137. Luther, F, Morris, DO, Hart, C. Orthodontic preparation for orthognathic surgery: how long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 2003; 41:401–406.
138. Matasa, CG, Graber, TM. Angle, the innovator, mechanical genius, and clinician. Am J Orthod Dentofacial Orthop. 2000; 117:444–452.
139. McLaughlin, RP, Bennett, JC. Anchorage leveling and aligning with a preadjusted appliance system. J Clin Orthod. 1991; 25:687–696.
140. McManaman, JE, Woodside, DG. Evolution of orthodontic bracket design. Alpha Omegan. 2000; 93:55–65.
141. Meikle, MC. Remodeling the dentofacial skeleton: the biological basis of orthodontics and dentofacial orthopedics. J Dent Res. 2007; 86:12–24.
142. Melsen, B, Petersen, JK, Costa, A. Zygoma ligatures: an alternative form of maxillary anchorage. J Clin Orthod. 1998; 32:154–158.
143. Midgett, RJ, Shaye, R, Fruge, JF, Jr. The effect of altered bone metabolism on orthodontic tooth movement. Am J Orthod. 1981; 80:256–262.
144. Mitchell, DL. The first direct bonding in orthodontia, revisited [viewpoint]. Am J Orthod Dentofacial Orthop. 1992; 101:187–189.
145. Miura, F, Nakagawa, K, Masuhara, E. New direct bonding system for plastic brackets. Am J Orthod. 1971; 59:350–361.
146. Monson, GS. Occlusion as applied to crown and bridge work. J Am Dent Assoc. 1920; 7:399–413.
147. Moyers, R. Handbook of orthodontics, ed 4. Chicago: Year Book; 1988.
148. Nance, HN. The limitations of orthodontic treatment. Am J Orthod. 1947; 33:177–223.
149. Nance, HN. The removal of second premolars in orthodontic treatment. Am J Orthod. 1949; 35:685–695.
150. Nanda, R. Protraction of maxilla in rhesus monkeys by controlled extraoral forces. Am J Orthod. 1978; 74:121–141.
151. Nanda, R. Biomechanical and clinical considerations of a modified protraction headgear. Am J Orthod. 1980; 78:125–139.
152. Nanda, R, Goldin, B. Biomechanical approaches to the study of alterations of facial morphology. Am J Orthod. 1980; 78:213–226.
153. Newman, GV. First direct bonding in orthodontics. Am J Orthod Dentofacial Orthop. 1992; 101:190–191.
154. Newman, GV, Newman, RA, Sun, BI, et al. Adhesion promoters, their effect on the bond strength of metal brackets. Am J Orthod Dentofacial Orthop. 1995; 108:237–241.
155. Noxon, SJ, King, GJ, Gu, G, Huang, G. Osteoclast clearance from periodontal tissues during orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2001; 120:466–476.
156. Nyman, S, Karring, T, Bergenholtz, G. Bone regeneration in alveolar bone dehiscences produced by jiggling forces. J Periodontal Res. 1982; 17:316–322.
157. Otuyemi, OD, Jones, SP. Long-term evaluation of treated Class II division 1 malocclusions utilizing the PAR index. Br J Orthod. 1995; 22:171–178.
158. Paladin P, ed. Orthodontic history: braced for a century. St. Louis: American Association of Orthodontics, 2005.
159. Park, HS. The skeletal cortical anchorage using titanium microscrew implants. Korea J Orthod. 1999; 29:699–706.
160. Park, HS, Bae, SM, Kyung, HM, Sung, JH. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J Clin Orthod. 2001; 35:417–422.
161. Park, HS, Kyung, HM, Sung, JH. Simple method of molar uprighting with micro-implant anchorage. J Clin Orthod. 2002; 36:592–596.
162. Parker, WS. Review of the D’Amico concept of cuspid function and its relationship to orthodontic treatment. Bull Pac Coast Soc Orthod. 1967; 42:11–14.
163. Pascal, M, Gallucci, G, Belser, U. Anatomic crown/width ratios of unworn and worn maxillary teeth in white subjects. J Prosthet Dent. 2003; 89:453–461.
164. Peck, H, Peck, S. An index for assessing tooth-shape deviations as applied to the mandibular incisors. Am J Orthod. 1972; 61:384–401.
165. Peterson, HW. Some observations on the progress of orthodontics during the past fifty years. Am J Orthod. 1953; 39:289–290.
166. Pilion, JJGM, Kuijpers-Jagtman, AM, Maltha, JC. Magnitude of orthodontic forces and rate of bodily tooth movement: an experimental study in beagle dogs. Am J Orthod Dentofacial Orthop. 1996; 110:16–23.
167. Proffit, WR, Gamble, JW, Christiansen, RL. Generalized muscular weakness with severe anterior open bite. Am J Orthod. 1968; 54:104–110.
168. Proffit, WR. Forty-year review of extraction frequencies at a university orthodontic clinic. Angle Orthod. 1994; 64:407–414.
169. Proffit, WR, Miguel, JA. The duration and sequencing of surgical orthodontic treatment. Int J Adult Orthod Orthognath Surg. 1995; 10:35–42.
170. Proffit, WR, White, RP, Sarver, DM. Contemporary treatment of dentofacial deformity. St. Louis: Mosby; 2003.
171. Proffit WR, Fields HW, Sarver DM, eds. Contemporary orthodontics, ed 5, St. Louis: Mosby/Elsevier, 2012.
172. Pus, MD, Way, DC. Enamel loss due to orthodontic bonding with filled and unfilled resins using various clean-up techniques. Am J Orthod. 1980; 77:269–283.
173. Redd, TB, Shivapuja, PK. Debonding ceramic brackets: effects on enamel. J Clin Orthod. 1991; 25:475–481.
174. Reitan, K. Continuous bodily tooth movement and its histological significance. Acta Odontol Scand. 1947; 6:115–144.
175. Ren, Y, Maltha, JC, Bohl, MV, et al. Cytokine levels in crevicular fluid are less responsive to orthodontic force in adults than in juveniles. J Clin Periodontol. 2002; 29:757–762.
176. Ren, Y, Maltha, JC, Von den Hoff, JW, Kuijpers-Jagtman, AM. Age effect on orthodontic tooth movement in rats. J Dent Res. 2003; 82:38–42.
177. Retief, DH, Dreyer, CJ, Gavron, G. The direct bonding of orthodontic attachments to teeth by means of an epoxy resin adhesive. Am J Orthod. 1970; 58:21–40.
178. Richmond, S, Shaw, WC, Roberts, CT, Andrews, M. The PAR index (Peer Assessment Rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod. 1992; 14:180–187.
179. Ricketts, RM. Keystone triad: Part 2. Am J Orthod. 1964; 50:728–750.
180. Ricketts, RM. A detailed consideration of the line of occlusion. Angle Orthod. 1978; 48:274–282.
181. Ricketts, RM. The wisdom of the bioprogressive philosophy. Semin Orthod. 1998; 4:201–209.
182. Rinchuse, DJ, Kandasamy, S. Articulators in orthodontics: an evidence-based perspective. Am J Orthod Dentofacial Orthop. 2006; 129:299–308.
183. Rinchuse, DJ, Kandasamy, S. Centric relation: a historical and contemporary orthodontic perspective. J Am Dent Assoc. 2006; 137:494–501.
184. Roberts, WE, Goodwin, WC, Jr., Heiner, SR. Cellular response to orthodontic force. Dent Clin North Am. 1981; 25:3–17.
185. Roberts, WE, Smith, RK, Zilberman, Y, et al. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984; 86:95–111.
186. Roberts, WE, Helm, FR, Marshal, KJ, Gongloff, RK. Rigid endosseous implants for orthodontic and orthopaedic anchorage. Angle Orthod. 1989; 59:247–256.
187. Roberts, WE, Marshall, KJ, Mozsary, PG. Rigid endosseous implant utilized as anchorage to protract molars and close an atrophic extraction site. Angle Orthod. 1990; 60:135–151.
188. Roberts, WE, Arbuckle, GR, Analoui, M. Rate of mesial translation of mandibular molars using implant anchored mechanics. Angle Orthod. 1996; 66:331–338.
189. Roberts, WE, Huja, S, Roberts, JA. Bone modeling: biomechanics, molecular mechanisms, and clinical perspectives. Semin Orthod. 2004; 10:123–161.
190. Roth, RH. Five-year clinical evaluation of the Andrews straightwire appliance. J Clin Orthod. 1976; 10:836–850.
191. Roth, RH. The straight-wire appliance 17 years later. J Clin Orthod. 1987; 21:632–642.
192. Roth, RH. Gnathological considerations for orthodontic therapy. In: McNeill C, ed. Science and practice of occlusion. Chicago: Quintessence; 1997:502–514.
193. Sabri, R. Orthodontic objectives in orthognathic surgery: state of the art today. World J Orthod. 2006; 7:177–191.
194. Sato, S, Kaneko, M, Sasaguri, K, et al. Different mechanics for orthodontic correction of Class II openbite and Class III openbite malocclusions. Bulletin of Kanagawa Dental College. 2007; 35(1):65–77.
195. Schoppe, RJ. An analysis of second premolar extraction procedures. Angle Orthod. 1964; 34:292–302.
196. Schubert, P, Bailey, LJ, White, RP, Proffit, WR. Long-term cephalometric changes in untreated adults compared to those treated with orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:91–99.
197. Sebaoun, JD, Kantarci, A, Turner, JW, et al. Modeling of trabecular bone and lamina dura following selective alveolar decortication in rats. J Periodontol. 2008; 79(9):1679–1688.
198. Shankland, WM. The American Association of Orthodontists: the biography of a specialty organization. St. Louis: The American Association of Orthodontists; 1971.
199. Shapiro, PA, Kokich, VG. Uses of implants in orthodontics. Dent Clin North Am. 1988; 32:539–540.
200. Shih, MS, Norrdin, RW. Regional acceleration of remodeling during healing of bone defects in beagles of various ages. Bone. 1985; 5:377–379.
201. Siara-Olds, NJ, Pangrazio-Kulbersh, V, Berger, J, Bayirli, B. Long-term dentoskeletal changes with the Bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthod. 2010; 80:18–29.
202. Silverman, E, Cohen, M, Gianelly, AA, Dietz, VS. A universal direct bonding system for both metal and plastic brackets. Am J Orthod. 1972; 62:236–244.
203. Siomka, LV, Powers, JM. In vitro bond strength of treated direct-bonding metal bases. Am J Orthod. 1985; 88:133–136.
204. Sirirungrojying, S, Saito, K, Hayakawa, T, Kasai, K. Efficacy of using self-etching primer with a 4-META/MMA-TBB resin cement in bonding orthodontic brackets to human enamel and effect of saliva contamination on shear bond strength. Angle Orthod. 2004; 4:251–258.
205. Southard, TE, Buckley, MJ, Spivey, JD, et al. Intrusion anchorage potential of teeth versus rigid endosseous implants: a clinical and radiographic evaluation. Am J Orthod Dentofacial Orthop. 1995; 107:115–120.
206. Squire, D, Best, AM, Lindauer, SJ, Laskin, DM. Determining the limits of orthodontic treatment of overbite, overjet, and transverse discrepancy: a pilot study. Am J Orthod Dentofacial Orthop. 2006; 129:804–808.
207. Strang, RH. Highlights of sixty-four years in orthodontics. Angle Orthod. 1974; 44:101–112.
208. Swartz, LS. Fact or fiction: the clinical relevance of in vitro steady state friction studies. J Clin Orthod. 2007; 8:427–432.
209. Thompson, JR, Craddock, FW. Functional analysis of occlusion. J Am Dent Assoc. 1949; 33:404–406.
210. Tulloch, C, Phillips, C, Proffit, W. Benefit of early Class II treatment: progress report of a two-phase randomized clinical trial. Am J Orthod Dentofacial Orthop. 1998; 113:62–71.
211. Turley, PK, Kean, C, Schur, J, et al. Orthodontic force application to titanium endosseous implants. Angle Orthod. 1988; 58:151–162.
212. Tweed, CH. Indications for extraction of teeth in orthodontic procedure. Am J Orthod Oral Surg. 1944; 30:405–428.
213. Tweed, CH. Pre-orthodontic guidance procedure: classification of facial growth trends; treatment and timing. In: Kraus BS, Riedel RA, eds. Vistas in orthodontics. Philadelphia: Lea & Febiger; 1962:359–389.
214. Tweed, CH. Clinical orthodontics. St. Louis: Mosby; 1966.
215. Umemori, M, Sugawara, J, Mitani, H, et al. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofacial Orthop. 1999; 115:166–174.
216. Vargervik, K, Miller, AJ, Chierici, G, et al. Morphologic response to changes in neuromuscular patterns experimentally induced by altered mode of respiration. Am J Orthod. 1984; 85:115–124.
217. Verna, C, Dalstra, M, Melsen, B. The rate and the type of orthodontic tooth movement is influenced by bone turnover in a rat model. Eur J Orthod. 2000; 22:343–352.
218. Verna, C, Melsen, B. Tissue reaction to orthodontic tooth movement in different bone turnover conditions. Orthod Craniofac Res. 2003; 6:155–163.
219. Vig, PS, Weintraub, JA, Brown, C, Kowalski, CJ. The duration of orthodontic treatment with and without extractions: a pilot study of five selected practices. Am J Orthod Dentofacial Orthop. 1990; 97:45–51.
220. Wahl, N. Orthodontics in 3 millennia. Chapter 1: Antiquity to the mid-19th century. Am J Orthod Dentofacial Orthop. 2005; 127:255–259.
221. Wahl, N. Orthodontics in 3 millennia. Chapter 2: Entering the modern era. Am J Orthod Dentofacial Orthop. 2005; 127:510–515.
222. Wahl, N. Orthodontics in 3 millennia. Chapter 5: The American Board of Orthodontics, Albert Ketcham, and early 20th-century appliances. Am J Orthod Dentofacial Orthop. 2005; 128:535–540.
223. Wahl, N. Orthodontics in 3 millennia. Chapter 6: More early 20th-century appliances and the extraction controversy. Am J Orthod Dentofacial Orthop. 2005; 128:795–800.
224. Wehrbein, H, Merz, BR, Diedrich, P, Glatzmaier, J. The use of palatal implants for orthodontic anchorage. Clin Oral Implants Res. 1996; 7:410–417.
225. Wehrbein, H, Merz, BR. Aspects of the use of endosseous palatal implants in orthodontic therapy. J Esthet Dent. 1998; 10:315–324.
226. Weinberger, BW. Orthodontics: a historical review of its origin and evolution, including an extensive bibliography of orthodontic literature up to the time of specialization. St. Louis: The CV Mosby Company; 1926.
227. Weinberger, BW. Historical résumé of the evolution and growth of orthodontia. J Am Dent Assoc. 1934; 21:2001–2021.
228. Weinberger, BW. Dr Edward Hartley Angle: his influence on orthodontics. Am J Orthod. 1950; 36:596–607.
229. Wenzel, A, Henriksen, J, Melsen, B. Nasal respiratory resistance and head posture: effect of intra-nasal corticosteroid (Budesonide) in children with asthma and perennial rhinitis. Am J Orthod. 1983; 84:422–426.
230. Wilcko, WM, Wilcko, MT, Bouquot, JE, Ferguson, DJ. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001; 21:9–19.
231. Wilcko, WM, Ferguson, DJ, Bouguot, JE, Wilcko, MT. Rapid orthodontic decrowding with alveolar augmentation: case report. World J Orthod. 2003; 4:197–205.
232. Wilson, AD, Kent, BE. A new translucent cement for dentistry. The glass ionomer cement. Br Dent J. 1972; 132:133–135.
233. Wright, CF. Status of orthodontic education prior to 1930. Angle Orthod. 1947; 17:92–96.
234. Yaffe, A, Fine, N, Binderman, I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994; 65:79–83.
235. Yaqoob, O, Patel, A, O’Neill, J. Active postsurgical orthodontic treatment: how long does it take? Br Orthod Soc Clin Effect Bull. 2006; 19:12.
236. Zachrisson, BU, Årtun, J. Enamel surface after various debonding techniques. Am J Orthod. 1979; 75:121–127.
*References 20, 22, 35, 45, 46, 48, 83, 87, 100, 115, 158, 171, 198, 207, 220–223, 226–228
†References 50, 58, 59, 75, 76, 91, 93–97, 119, 127, 134–136, 141, 150–152, 167, 213, 216, 229
*References 50, 58, 75, 76, 91, 93–97, 119, 127, 134–136, 141, 150–152, 167, 213, 216, 229
*References 10, 38, 51, 56, 105, 120, 144, 145, 153, 154, 172, 173, 177, 202–204, 232, 236
*References 7, 21, 27, 33, 52, 53, 57, 62, 77, 80, 104, 106, 109, 123, 129, 131, 142, 159–161, 188, 189, 199, 205, 211, 215



