CHAPTER 1
Oropharynx and Hypopharynx
INTRODUCTION
The oropharynx is the gateway to the proximal gastrointestinal tract. Although visualized daily by endoscopists, a thorough examination may not be routine. With the expanding patient base of immunocompromised patients, inspection of the oropharynx, particularly in patients with esophageal symptoms, should be part of every examination. Oropharyngeal abnormalities can suggest underlying esophageal disease in these patients, and oropharyngeal lesions may be the first manifestation of an underlying systemic disorder. Asymptomatic malignant disease may also be detected. With increasing appreciation of the extraesophageal manifestations of gastroesophageal reflux disease, hypopharyngeal examination assumes an even greater role. A thorough knowledge of hypopharyngeal anatomy is thus essential for all endoscopists.
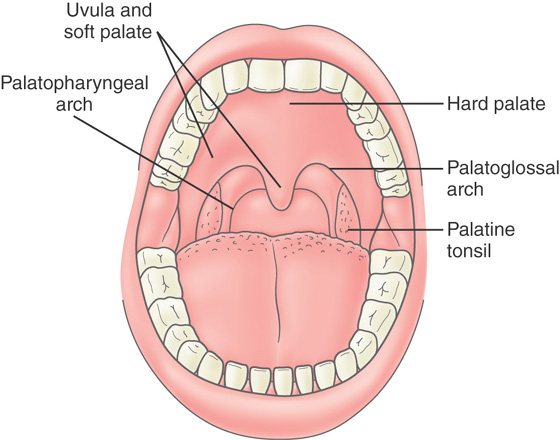
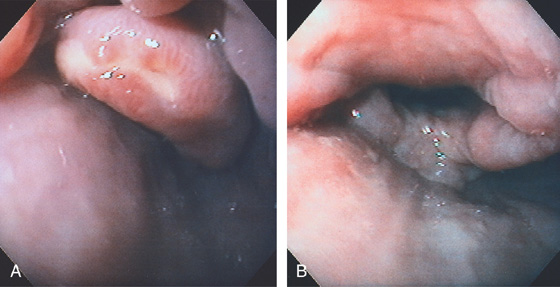
Figure 1.1 OROPHARYNX
Normal pharynx as viewed with an endoscope, demonstrating the junction of the hard and soft palate, uvula, and posterior pharynx.
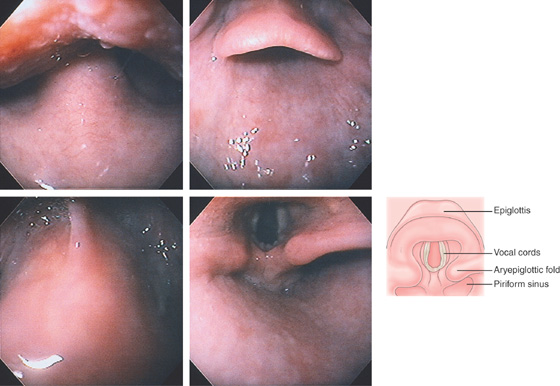
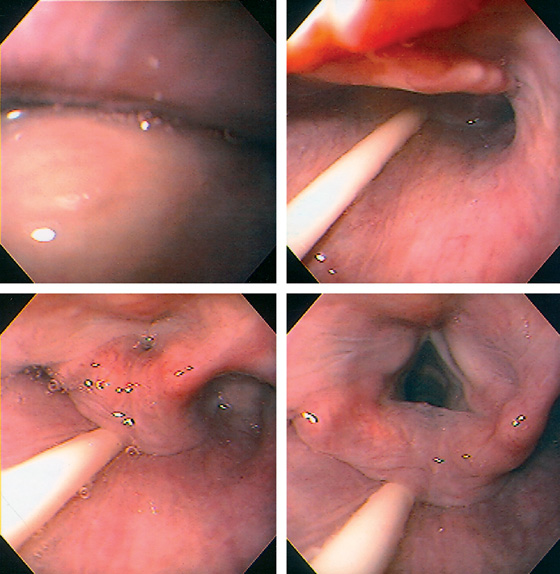
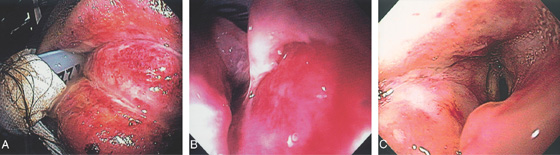
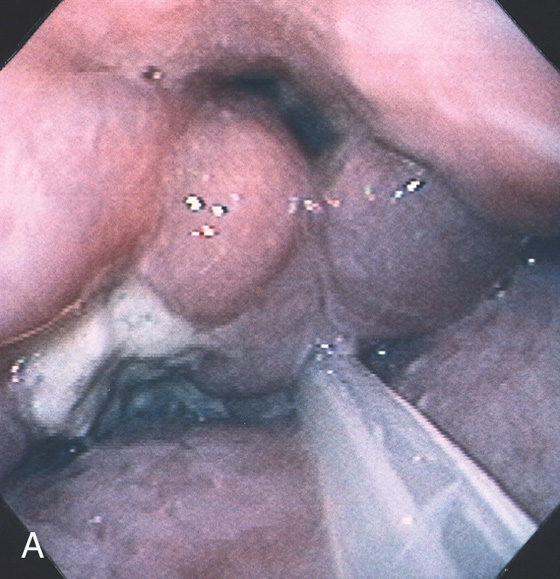
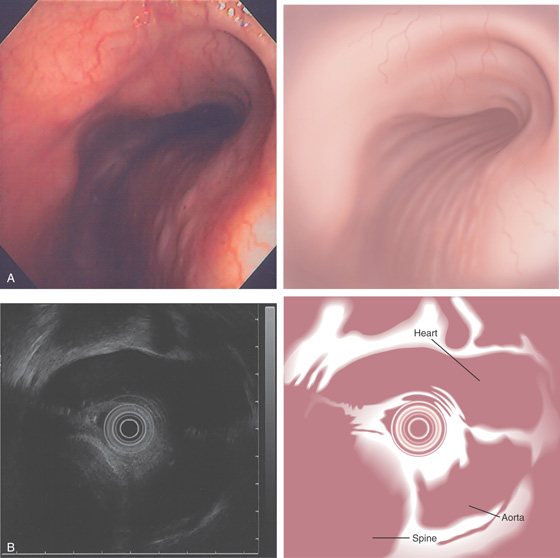
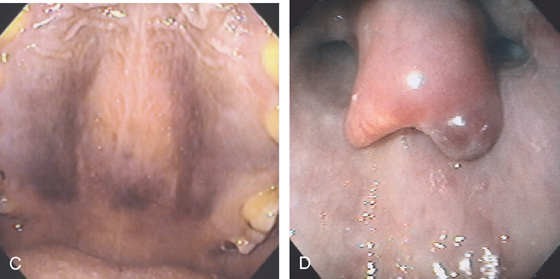
Figure 1.2 LANDMARKS OF THE OROPHARYNX AND HYPOPHARYNX
With the endoscope advanced under direct vision, the inferior portion of the uvula is seen at the base of the tongue. Notice that the image is inverted (top left). With further advancement, the superior portion of the epiglottis is identified (top right). Advancement anteriorly ends at the attachment of the epiglottis, termed the valleculae (bottom left). To enter the hypopharynx, the endoscope is advanced posteriorly behind the epiglottis into the hypopharynx (bottom right). The epiglottis appears to form a roof over the hypopharynx. The vocal cords are surrounded by the aryepiglottic folds anteriorly. In this position, the piriform recesses or sinuses are on the lateral side of the aryepiglottic folds. The cricopharyngeus and entrance to the esophagus are in the midline posteriorly.
Figure 1.3 DIRECTION TO CRICOPHARYNGEUS
The endoscope is passed over the tongue and uvula (upper left). Once past the uvula, the epiglottis and hypopharynx are seen in the distance. A nasogastric feeding tube is now present (upper right). The arytenoids are now visible with the feeding tube seen posterior in the midline (bottom left). The arytenoids are open and the vocal cords visible. Again, the feeding tube is posterior in the midline showing the location of the cricopharyngeus (bottom right).
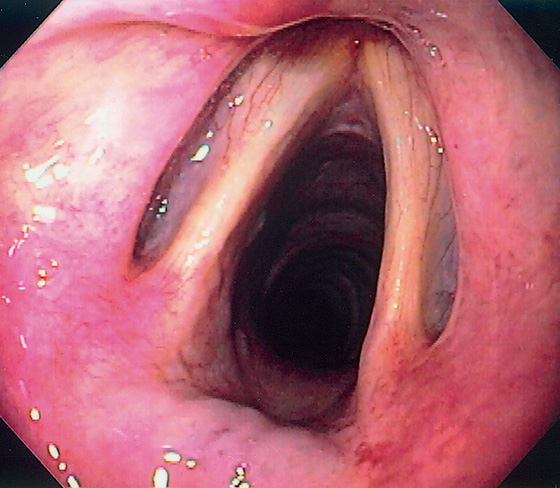
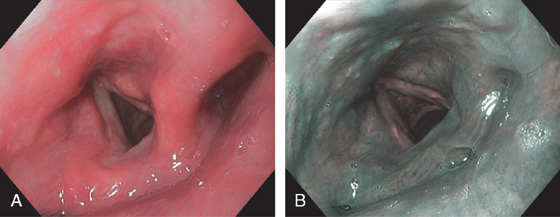
Figure 1.4 VOCAL CORDS
Normal vocal cords and surrounding structures as seen from the arytenoids.
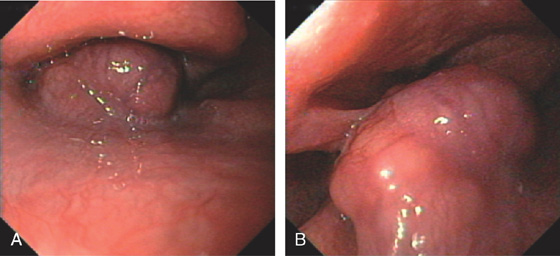
Figure 1.5 HYPOPHARYNX
A, Normal-appearing hypopharynx as seen on high-definition endoscopy. B, Narrow band imaging of the hypopharynx.
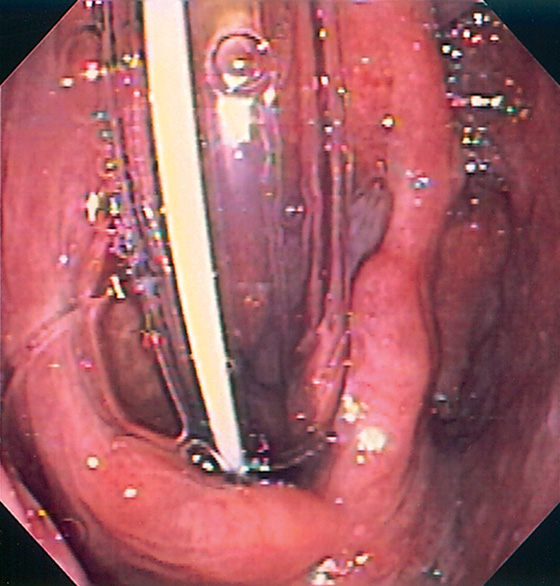
Figure 1.6 HYPOPHARYNX WITH ENDOTRACHEAL TUBE
Note the anatomy of the hypopharynx with endotracheal intubation.
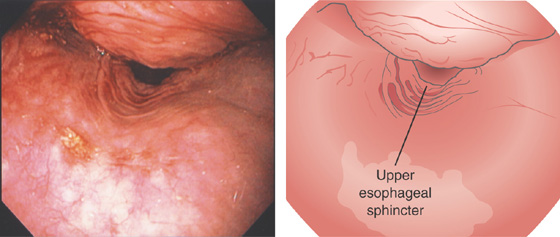
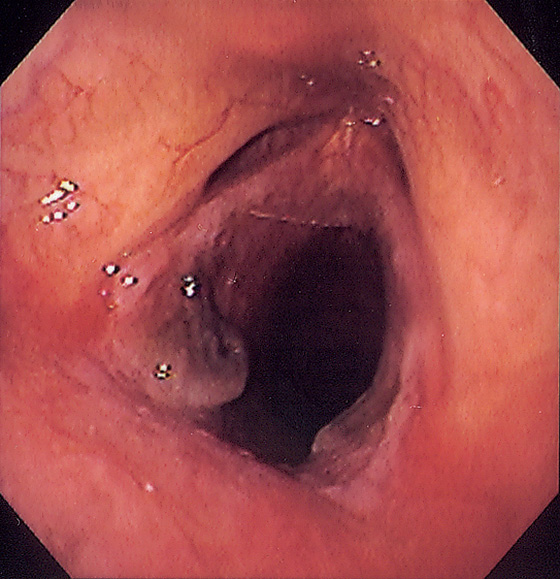
Figure 1.7 PATENT UPPER ESOPHAGEAL SPHINCTER
After endoscope removal, the upper esophageal sphincter remained patulous. Note its location relative to the cricopharyngeus, confirming the posterior location of the upper esophageal sphincter. Also note the erythema of the hypopharynx and arytenoids.
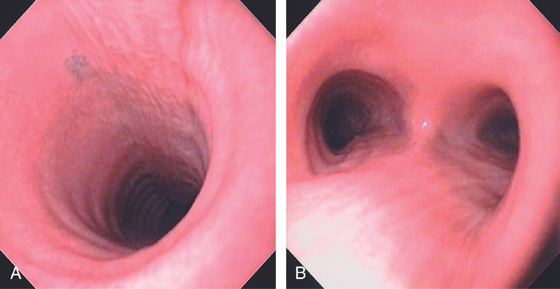
Figure 1.8 TRACHEA AND CARINA
View of the (A) trachea and (B) carina at endoscopy. Note the ringlike architecture of the trachea.
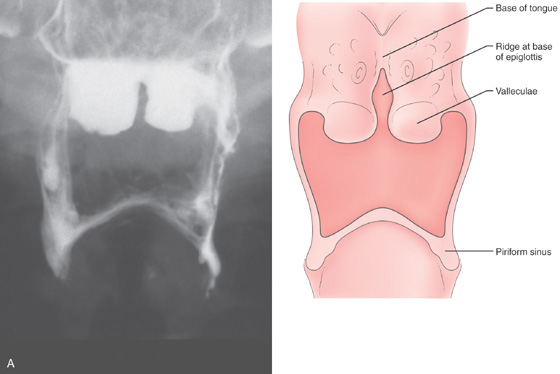
Figure 1.9 BARIUM STUDY OF HYPOPHARYNX AND ESOPHAGUS
A, Anteroposterior view demonstrates the base of the tongue, valleculae, piriform sinuses, and ridge at the base of the epiglottis.
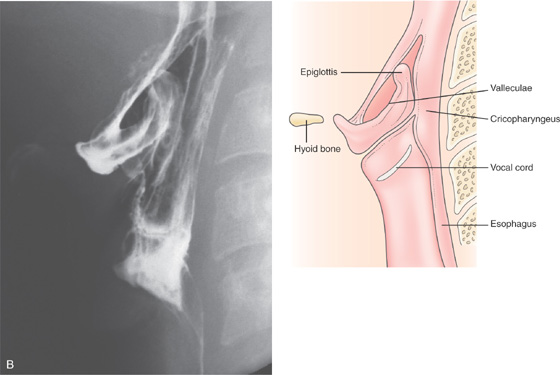
B, Lateral view demonstrates the valleculae; hypopharynx; piriform sinus; cricopharyngeus, with some contrast seen in the esophagus; and hyoid bone.
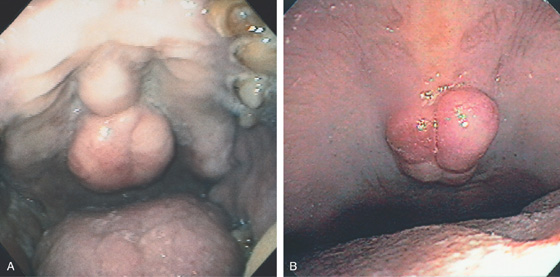
Figure 1.10 TORUS PALATINUS
A, This large, masslike abnormality on the hard palate is an exaggeration of a normal structure, resulting from a bony exostosis of the midline palatal suture. B, Nodular structure on the distal hard palate.
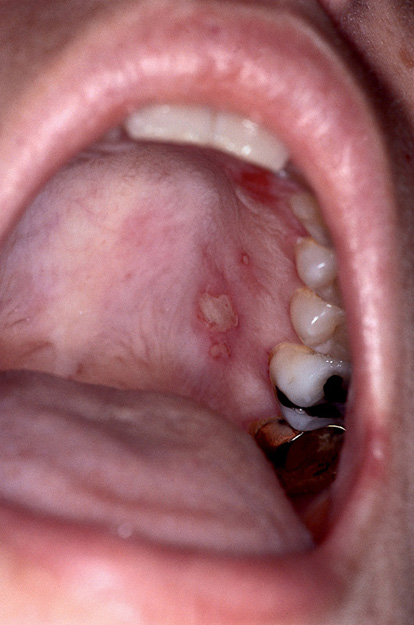
Figure 1.11 APHTHOUS ULCER
Shallow, well-circumscribed ulceration on the hard palate. This patient had active inflammatory bowel disease (see Figure 5.36).
![]() Differential Diagnosis
Differential Diagnosis
Aphthous Ulcer (Figure 1.11)
Infectious causes
Herpes simplex virus
Syphilis
Zoster
Histoplasmosis
Noninfectious causes
Systemic lupus erythematosus
T-cell disorders
Human immunodeficiency virus infection
Figure 1.12 HUMAN IMMUNODEFICIENCY VIRUS (HIV)-ASSOCIATED APHTHOUS ULCER
A, This large ulcer extends from the uvula to the soft palate. These lesions are frequent in patients with acquired immunodeficiency syndrome (AIDS) and may occur on the tongue or buccal mucosa or in the hypopharynx. They may become large, simulating an infectious or neoplastic process. B, Deep ulcer on the lateral aspect of the tongue. Note in the distance a well-circumscribed, similarappearing ulcer is present on the hard palate. C, Well-circumscribed, clean-based ulcer on the tongue. D, Multiple ulcerations on the lower lip. This patient with severe odynophagia also had a large idiopathic esophageal ulceration.
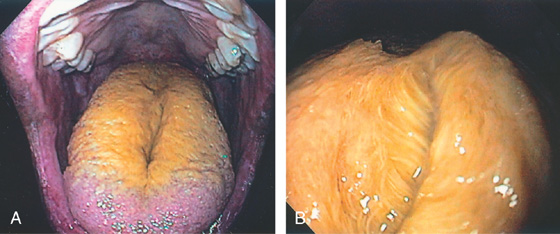
Figure 1.13 HAIRY TONGUE
A, Yellowish coating of the tongue. B, Close-up shows a furry appearance resembling hair. This disorder, of unknown etiology, is characterized by hypertrophy of the filiform papillae.
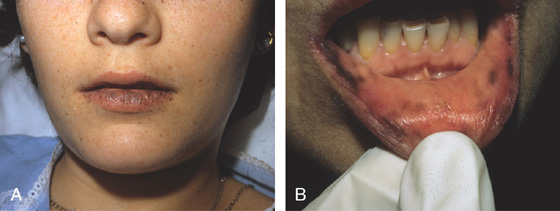
Figure 1.14 PEUTZ-JEGHERS SYNDROME
Multiple black hyperpigmented lesions of the (A) lips, (B) buccal mucosa
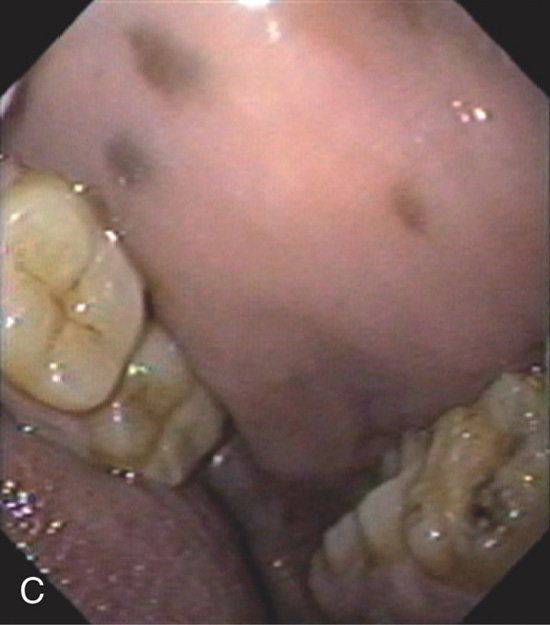
(C) hard palate.
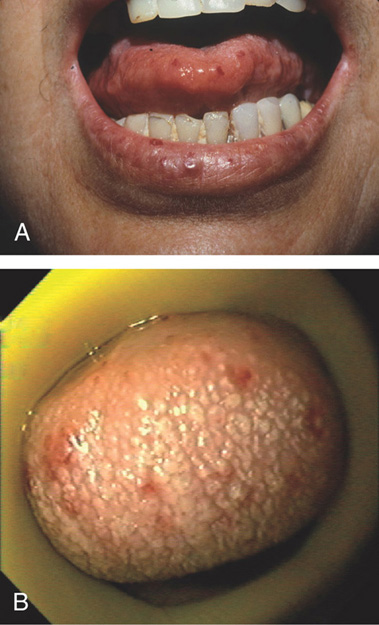
Figure 1.15 OSLER-WEBER-RENDU SYNDROME
Multiple ectasias of the (A) lips and tongue, (B) tongue
(C) palate, and (D) hypopharynx.
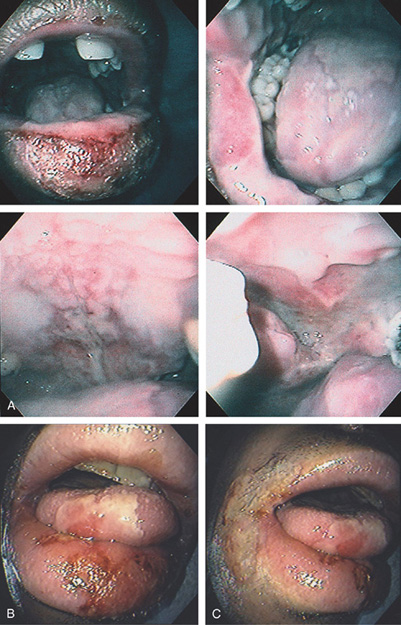
Figure 1.16 HERPES SIMPLEX VIRUS STOMATITIS
A, Characteristic lesions of herpes simplex virus stomatitis include diffuse ulceration of the lips (top left, top right), tongue (top right), hard and soft palate (bottom left), and posterior pharynx (bottom right). These lesions may also extend into the hypopharynx or to the squamous mucosa surrounding the lips or nares. B, Shallow ulceration on the lower lip, tongue, and the angle of the lips on the right (C).
Figure 1.17 HERPES SIMPLEX VIRUS STOMATITIS
A, Shallow ulceration on the hard palate associated with several small ulcerations. B, The ulceration extends to the epiglottis toward the vocal cords and aryepiglottic folds.

Figure 1.18 HERPES SIMPLEX VIRUS STOMATITIS
Shallow ulceration on the lower lip, tongue, and face extending to the nares.
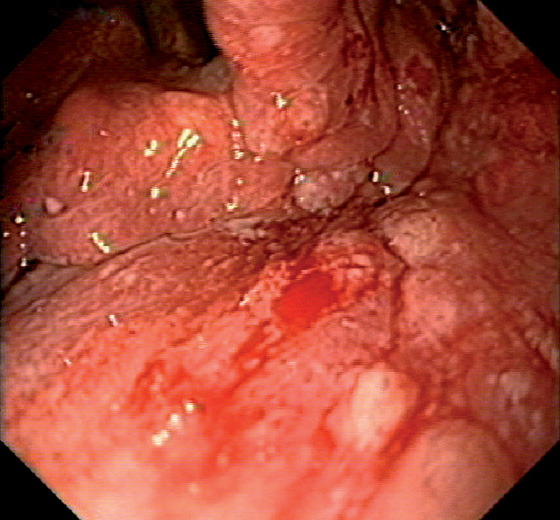
Figure 1.19 VARICELLA
Nodularity and shallow ulceration of the hypopharynx involving the arytenoid region of the larynx. Note the friability of the mucosa.
Figure 1.20 OROPHARYNGEAL CANDIDIASIS
A, Multiple white and yellow plaques on the hard and soft palate and buccal mucosa. In this patient, the tongue appears to be spared. Occasionally, the lesions will be identified in the hypopharynx when the endoscope is passed under direct vision.
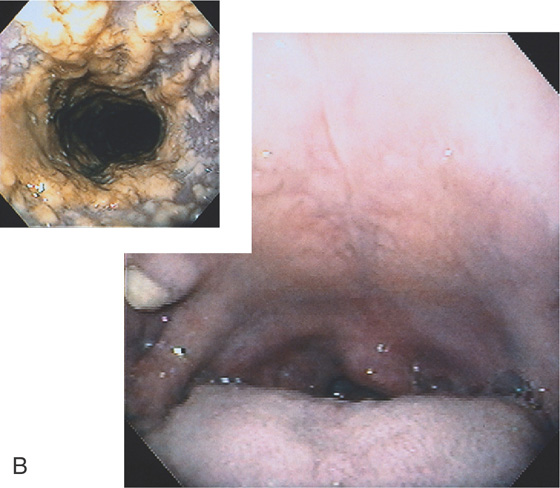
B, Normal-appearing oropharynx in a patient with Candida esophagitis (top left). This patient was not receiving antifungal therapy, highlighting the fact that thrush may be absent in patients with esophageal candidiasis.
C, Erythematous type of oropharyngeal candidiasis. Note the erythematous areas on the hard palate with minimal plaque material seen.

Figure 1.21 MUCORMYCOSIS
Necrotic-appearing hard and soft palate in this immunocompromised patient. There was also pronounced periorbital and facial swelling.
Figure 1.22 EPIGLOTTITIS
A, An ulcer is identified on the superior portion of a markedly edematous epiglottis. B, The distal portion of the epiglottis and the arytenoids are also edematous. Endoscopy was performed for dysphagia and hoarseness. After antibiotic therapy, all symptoms resolved.
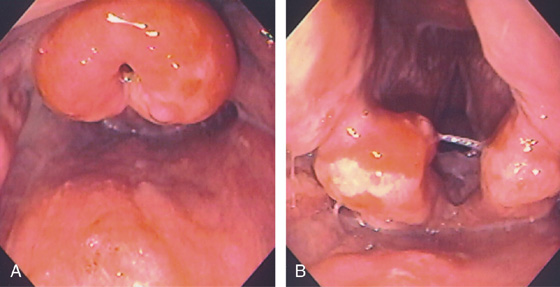
Figure 1.23 EPIGLOTTITIS
A, The epiglottis is markedly edematous with overlying erosions. B, The arytenoids are also edematous with erosive lesions.
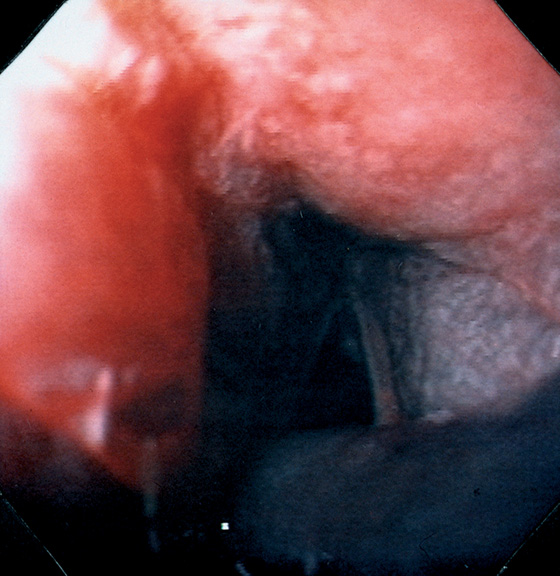
Figure 1.24 CAUSTIC INGESTION
Severe edema and hemorrhage in the hypopharynx. The vocal cords are seen in the distance. The patient had no lesions in the pharynx after ingestion of acetic acid. Further mucosal injury was seen in the esophagus and stomach (see Figure 2.157).
Figure 1.25 CAUSTIC INGESTION
Diffuse ulceration of the lips (A) and hypopharynx (B) 24 hours after caustic ingestion. The patient is intubated. C, Diffuse edema and ulceration of the hypopharynx 4 days later.
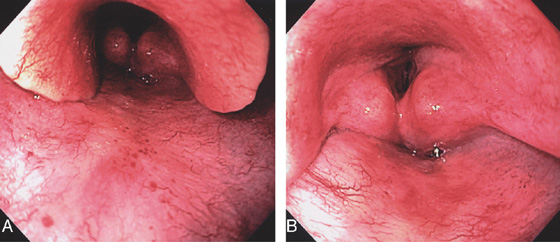
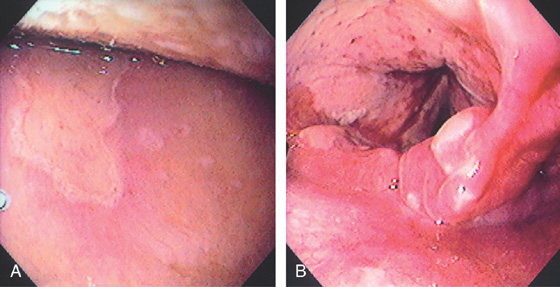
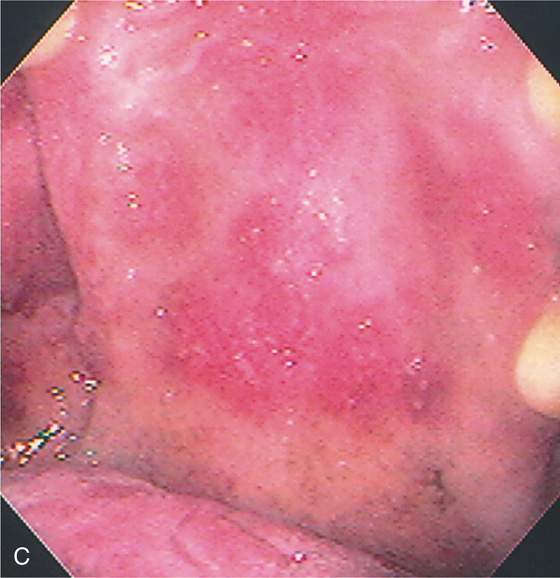
Figure 1.26 RADIATION INJURY
Diffuse erythema of the hypopharynx, epiglottis, and aryepiglottic folds. Note the pronounced neovascularization and pinpoint ectasias similar to what occurs in other areas of the gastrointestinal tract after radiation therapy (A, B).
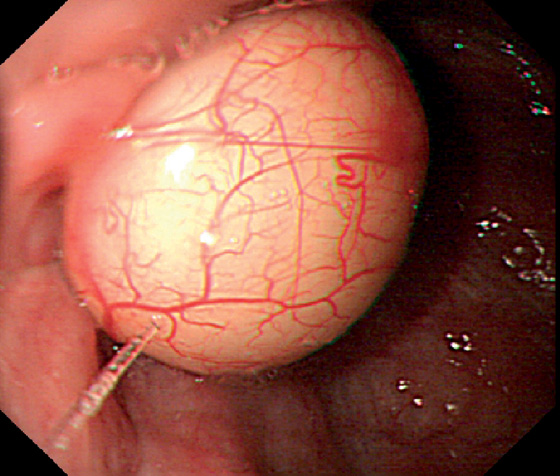
Figure 1.27 ARYTENOID CYST
Cystic structure with overlying normal vascular pattern in the hypopharynx.

Figure 1.28 CONDYLOMA
Small, whitish, verrucous-appearing lesion on the hard palate.
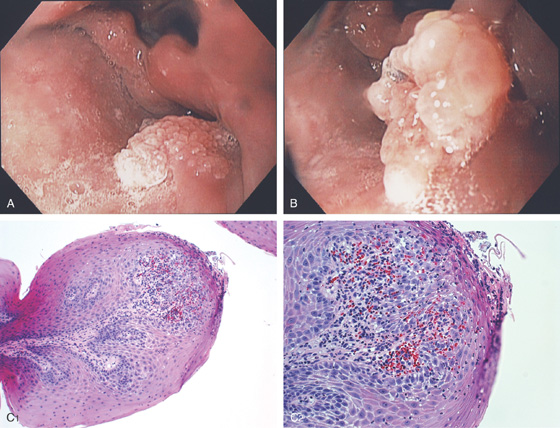
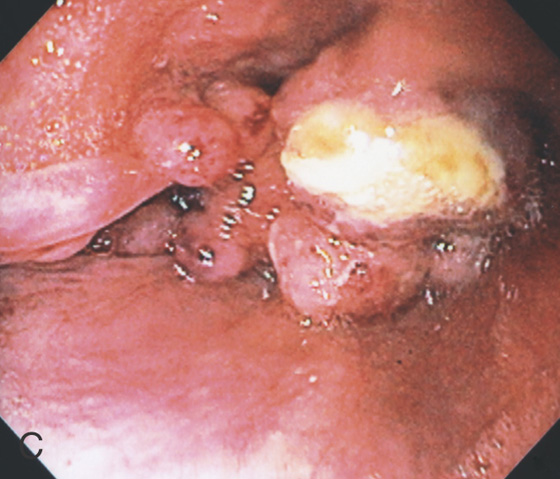
Figure 1.29 SQUAMOUS PAPILLOMA
A, B, Nodular mass lesion just proximal to the left piriform sinus with overlying verrucous appearance typical for a papilloma. C1, C2, Inflamed squamous epithelium with an edematous fibrovascular core consistent with squamous papilloma.
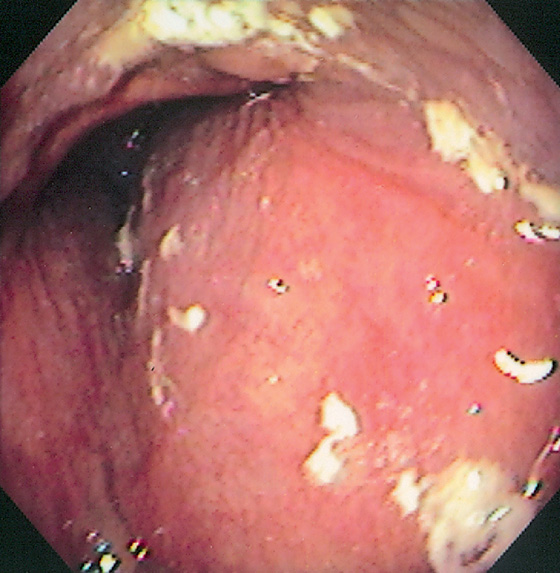
Figure 1.30 EXTRINSIC COMPRESSION
Submucosal masslike lesion causing extrinsic compression of the left hypopharynx.
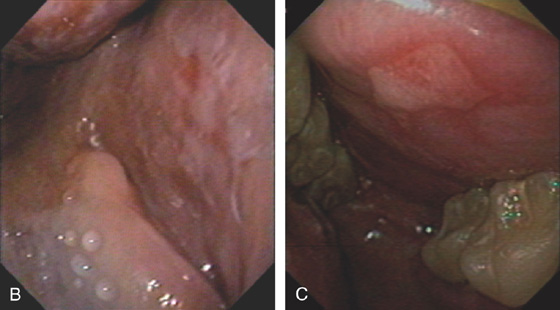
Figure 1.31 LICHEN PLANUS
Plaquelike white lesions of the buccal mucosa (A–C).
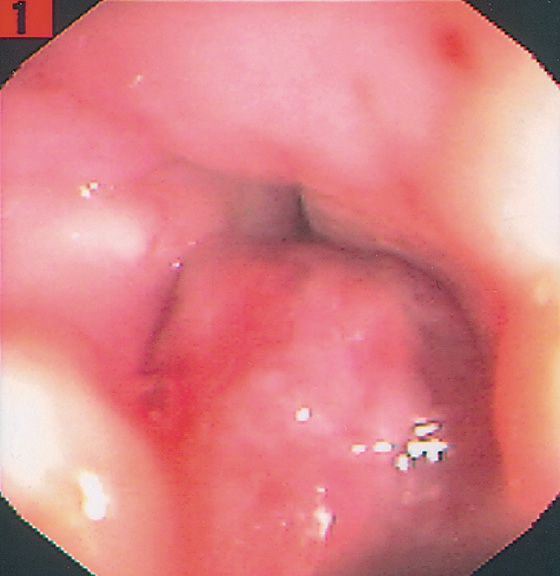
Figure 1.32 FIBROSARCOMA
Small, masslike lesion occupying the space just proximal to the vocal cords. The lesion was seen to move with respirations.
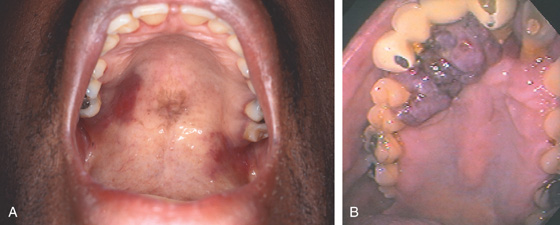
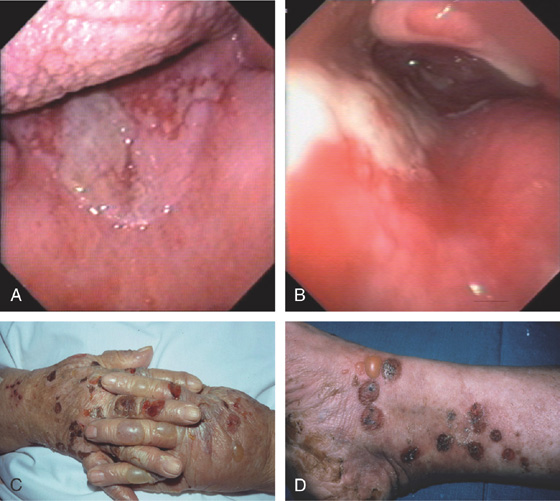
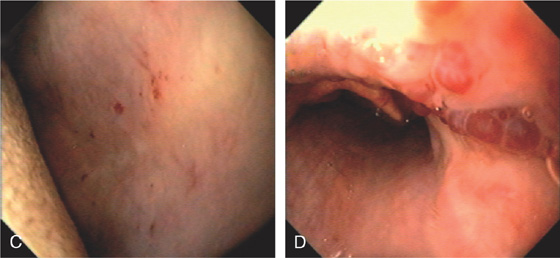
Figure 1.33 KAPOSI’S SARCOMA
A, Reddish plaquelike lesions of the hard and soft palate. B, Verrucous-appearing purple lesion on the hard palate.
C, Diffuse, flat purple lesion on both the soft and hard palate. Accompanying gastric lesions are typical (see Figure 3.156). D, Kaposi’s sarcoma lesion on the superior portion of the epiglottis. Note the associated edema, with loss of vascularity of the epiglottis.

E, Characteristic skin lesions.
Figure 1.34 SQUAMOUS CELL CARCINOMA
A, Ulcerative lesion in the right piriform sinus associated with edema and distortion of the aryepiglottic folds. A nasogastric tube can be seen entering the esophagus, demarcating the normal landmarks.
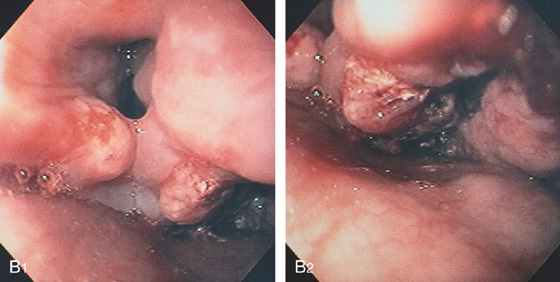
B, The arytenoids and aryepiglottic folds are distorted, with fresh blood present (B1). A necrotic ulcerated lesion is apparent in the left piriform sinus (B2). This patient underwent endoscopy for dysphagia, during which a squamous cell carcinoma of the distal esophagus was also found.
C, Ulcerated nodular lesion just proximal to the left piriform sinus involving the arytenoids.
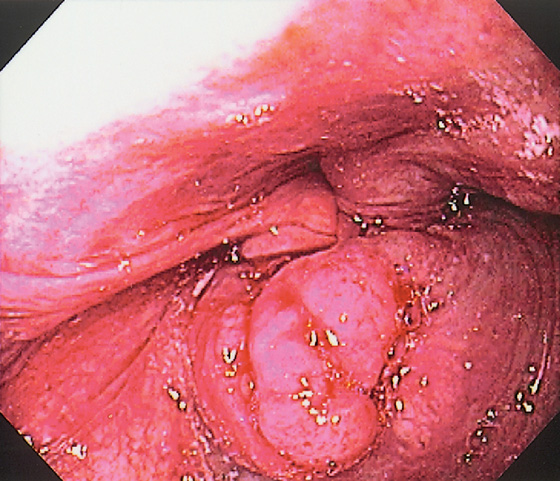
Figure 1.35 SQUAMOUS CELL CARCINOMA
Submucosal masslike lesion arising from the piriform sinus at the upper esophageal sphincter. Note the compression on the aryepiglottic folds.
Figure 1.36 MELANOMA
Submucosal mass-like lesion just proximal to the aryepiglottic folds (A, B).
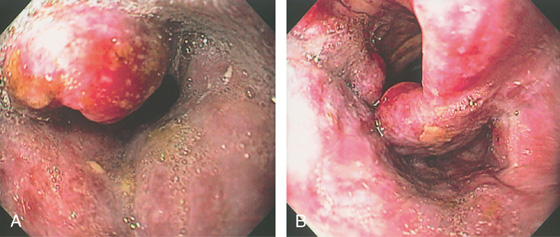
Figure 1.37 LEUKEMIA
Diffuse edema and exudate of epiglottis (A) and hypopharynx with erosion on the left aryepiglottic fold (B). This patient had leukemic infiltrates throughout the gastrointestinal tract (see Figures 2.74 and 5.207).
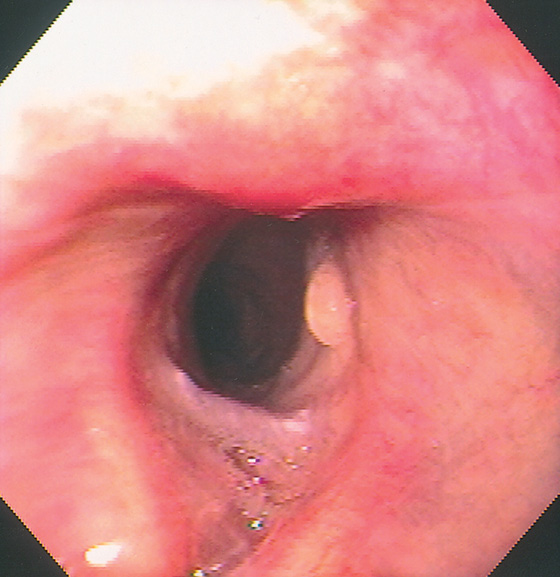
Figure 1.38 VOCAL CORD GRANULOMA
A small, benign-appearing lesion on the left true vocal cord diagnostic for a granuloma. There is no overlying epithelium on the lesion.
![]() Differential Diagnosis
Differential Diagnosis
Vocal Cord Granuloma (Figure 1.38)
Differential diagnosis of vocal cord nodules
Nodules typically are bilateral
Polyps
Gastroesophageal reflux disease
Allergies
Neoplasm
Figure 1.39 VOCAL CORD INJURY WITH INTUBATION
The vocal cords are edematous with a dark area representing trauma. Note the flame hemorrhages emanating from the cords typical for reflux of acid associated with intubation.
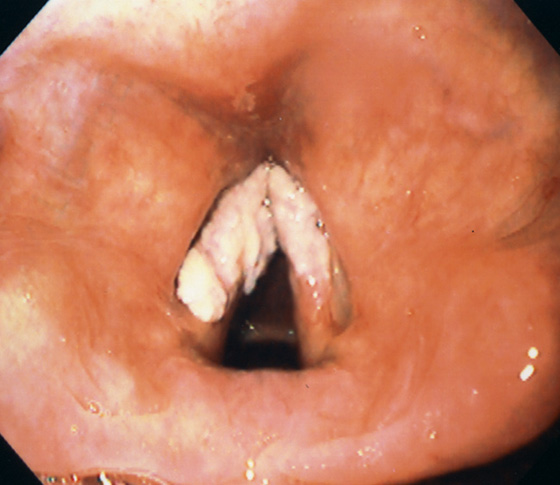
Figure 1.40 VOCAL CORD LEUKOPLAKIA
White, plaquelike lesion involving the true vocal cords.
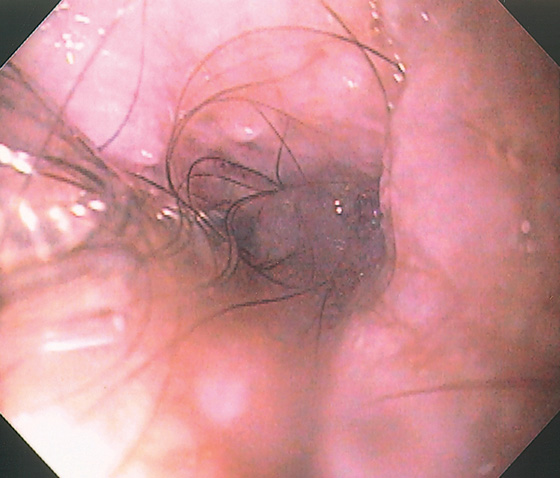
Figure 1.41 HYPOPHARYNGEAL RECONSTRUCTION
Note the color of the mucosa and associated hair. This patient had hypopharyngeal surgery with a skin flap. This was the area of the upper esophageal sphincter.
Figure 1.42 LATERAL PHARYNGOTOMY WITH FLAP
In the left pharynx, suture material is seen (A). More distally, note the distinction in color between the right and left pharynx (B). Resection was performed and a forearm flap used in this dark skinned individual.
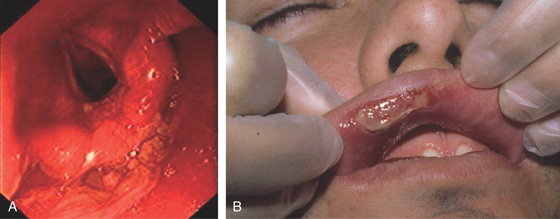
Figure 1.43 PEMPHIGUS VULGARIS
A, Marked erythema, exudates, and whitish mucosal changes of the hypopharynx involving the arytenoids. B, Shallow ulcer of the lip. (B courtesy P. Redondo, MD, Pamplona, Spain.)
Figure 1.44 BULLOUS PEMPHIGOID
A, Erosive lesion at the junction of hard and soft palate. B, The erosive lesion extends to the right hypopharynx involving the epiglottis. Bullous lesions of the (C) hands and (D) feet. (C, D courtesy P. Redondo, MD, Pamplona, Spain.)

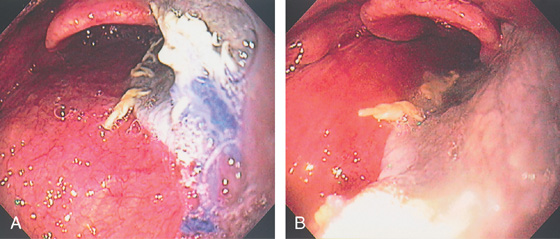
Figure 1.45 TRACHEAL BLEEDING
A, B, Fresh blood is seen to emanate from the vocal cords. C, Active bleeding from the tracheostomy site.