Chapter 11 Oral appliance and craniofacial problems of obstructive sleep apnea syndrome
1 INTRODUCTION
Pierre Robin (1934) used the monoblock mandible advancement appliance for the purpose of treating patients with obstructive sleep apnea for the first time.1 Following this, Boraz treated pediatric OSA patients.2 Cartwright and Samelson (1982)3 reported the effectiveness of the tongue retaining device (TRD) which retains the tongue in the bulb of the device. Meier-Ewert (1984)4 used Esmarch–Heiberg manipulation, which opens the airway of a general anesthetized patient, and developed the Esmarch appliance. The tongue retaining appliance represented by the TRD, and the mandible advancing type represented by the Esmarch, are the two main types of oral appliance. Thereafter, other oral appliances were developed such as the adjustable type, which can adjust the amount of mandible advancement. Currently, more than 55 oral appliances (OAs) are on the market.5
2 PATIENT SELECTION
In 2006, the Standards of Practice Committee of the American Academy of Sleep Medicine published the reports Oral Appliance for Snoring and Obstructive Sleep Apnea: A Review6 and Practice Parameters for the Treatment of Snoring and Obstructive Sleep Apnea with Oral Appliances: An Update for 2005.7 Oral appliances are indicated for use with patients with primary snoring and with mild to moderate OSA, who prefer them to continuous positive airway pressure (CPAP) therapy, or who do not respond to CPAP, are not appropriate candidates for CPAP, or who have failed treatment attempts with CPAP.
3 PROCEDURES FOR ORAL APPLIANCE THERAPY
The procedures for oral appliance therapy are as follows.
4 ORAL APPLIANCE VARIATIONS
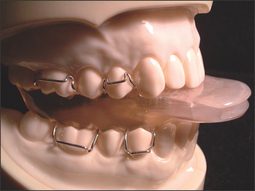
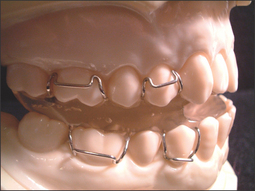
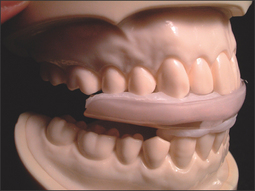
4.2 MANDIBULAR ADVANCING TYPE
4.2.1 NON-TITRATABLE TYPE
4.2.2 TITRATABLE TYPE
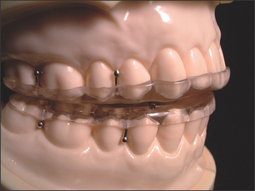
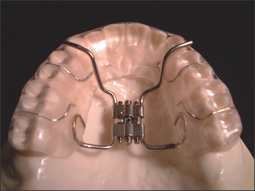
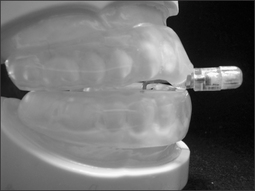
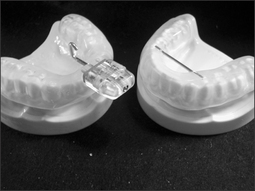
The mandibular advancing and titratable type of oral appliance is a custom-made two-piece appliance composed of two separate arches (maxillary and mandibular) containing an advancing mechanism. Examples are listed below.
5 POSTOPERATIVE MANAGEMENT AND SIDE EFFECTS OF ORAL APPLIANCE
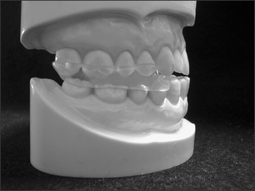
5.1 CHANGING THE OCCLUSION
Patients have to use oral appliances for long periods of time to maintain the airway patency every night. Consequently, the vigorous force applied to the teeth changes the occlusion. The occlusal change of the patient during oral appliance therapy conducted for 12 years can be seen in Figures 11.9 and 11.10. Sometimes teeth and/or prosthetic crowns can be broken by this force (Fig. 11.11). We should not only take care of the teeth, but also the occlusion and temporomandibular joint.
5.2 EFFICACY OF ORAL APPLIANCES
The Standards of Practice Committee of the American Academy of Sleep Medicine reported that the efficacy of OAs was established for controlling OSA in some but not all patients with success (defined as no more than 10 apneas or hypopneas per hour of sleep) achieved in an average of 52% of treated patients.6
5.3 ORTHODONTIC TREATMENT AND AIRWAY
Orthodontic treatment can influence the size and the function of the airway.
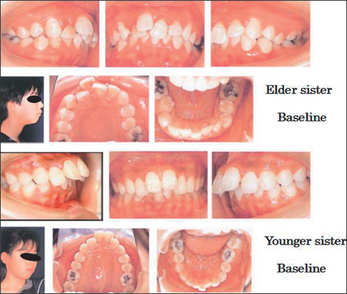
These patients were sisters aged 12 years 11 months and 11 years 9 months, so they were still growing. They complained about their maxillary protrusion. The elder sister was treated by the extraction of five teeth because she had one congenitally missing tooth and one root resorbed tooth. The younger sister, however, was treated by non-extraction with the Herbst appliance. The treatment term was 3 years 11 months for the elder sister and 3 years 2 months for the younger sister. Both sisters had a typical muscle strain on the chin when they closed the lips together (Fig. 11.12).
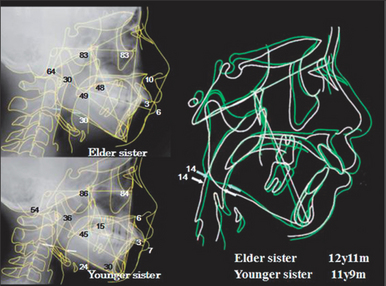
When we superimposed the cephalograms at the baseline of these sisters, there were a few differences between the sisters before treatment; for instance, the nose of the elder sister was bigger than that of the younger sister. However, the superimposition of the cephalograms of both cases revealed these sisters were almost identical. Their lower pharynx was the same width at the baseline (Fig. 11.13).
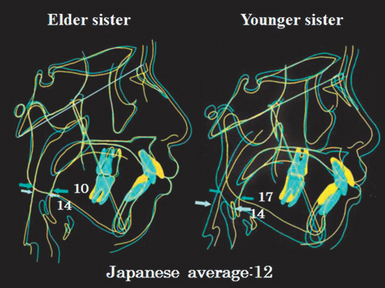
In both cases, the muscle strain on the chin disappeared after orthodontic treatment. Both sisters recovered with better facial appearance, and had a satisfactory result. There was little difference between the appearance of the sisters (Fig. 11.14).
When we superimposed the cephalograms of the baseline and the result of the elder sister, only her nose grew; the other part did not grow at all and the width of the lower pharynx was reduced from 12 mm to 10 mm. Conversely, the mandible of the younger sister grew a lot. As a consequence, the width of the lower pharynx was increased from 12 mm to 17 mm. The lower pharynxes of the sisters were the same, 12 mm before the treatment; however, the lower pharynx of elder sister reduced to 10 mm and that of younger sister increased to 17 mm. Thus, there was a total difference of 7 mm after the treatment (Fig. 11.15).
6 CRANIOFACIAL PATTERN OF OSA
The craniofacial characteristics of obstructive sleep apnea patients have been reported as follows.
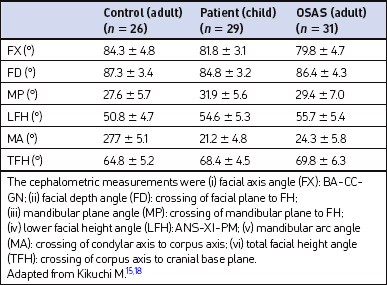
We reported that craniofacial patterns of OSA patients were: the dolichofacial pattern (increased anterior facial height) by cephalometric analysis of Ricketts’ and OSA patients having their mandible retropositioned; a long soft palate; decreased airway space; and a lowered position of the hyoid bone.15
6.1 CRANIOFACIAL PATTERN OF CHILD OSA
We also reported that the craniofacial pattern of child OSA was intermediate between adult OSA and adult control (Table 11.1).15,18 All the data showed intermediate values from the adult control to adult OSA. This may mean that the continuation of OSA makes the craniofacial pattern worsen year by year.
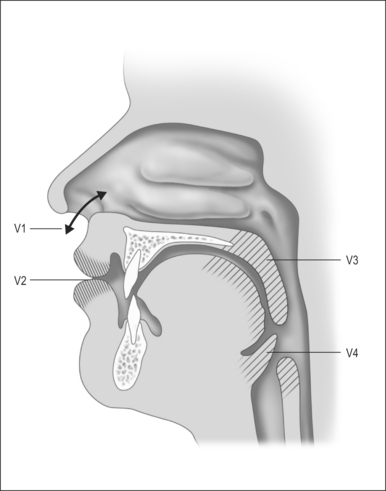
7 IMPORTANCE OF THE ORAL SEAL TOBREATHING
Frankel19 noted that the impact of the ‘space problem’ in the physiology of the orofacial complex has been emphasized by Moss.20–22 He maintains that the proper functioning of the digestive and respiratory systems depends on a functionally adequate patency of the oral and the nasopharyngeal passageways. This assumption receives significant support from the work of Bosma23 who emphasized the impact of adequate space conditions in the physiology of the orofacial complex, with particular emphasis on airway maintenance. The life-sustaining functions of breathing as well as intake and transport of food are dependent on the adequate patency of these spaces and the proper functioning of the various valves as seen in Figure 11.16.
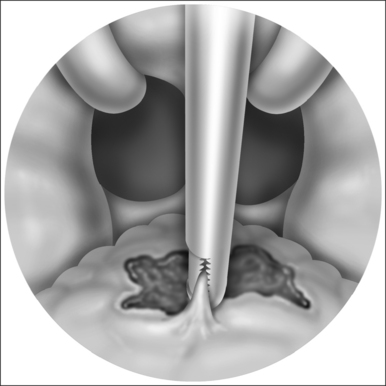
Bosma23 emphasized that the posterior soft tissue barrier formed by the soft palate and the tongue is an important factor for airway maintenance. The positional stabilization of the pharyngeal airway is the initial manifestation of the distinctive coordination of posture. The physiological relevance of the infantile performance of the stabilization of the airway is identified by its impairment in Pierre Robin syndrome. When these afflicted children are lying on their backs, the apposition of the tongue to the palate cannot take place because of the hypoplasia of the dorsal portion of the palate mostly associated with the cleft. The infantile mechanism of pharyngeal airway maintenance fails to operate, and the tongue falls downward and backward, occluding the pharynx. In a prone position, the tongue approximates the palate by the force of gravity, permitting nasal portal respiration. Bosma23 noted that mandibular retrusion in Pierre Robin syndrome may be interpreted as an appropriate component of a regional failure of a positional function which emphasizes the physiological relevance of the muscular barrier separating the oral cavity from the pharyngeal space.
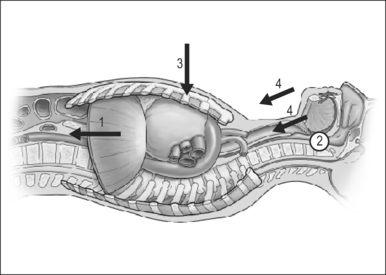
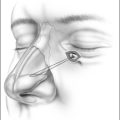
We propose the hypothesis that the mechanism of thoracic negative pressure inhibits the backward and downward growth of the mandible. When the obstruction occurs in the pharyngeal area, the patient wants to move down the diaphragm to take in air; accordingly, pressure is produced in the chest. The negative pressure produced in the chest (of the obstructive sleep apnea patient) is detected by intra-esophageal pressure monitoring. The deformity of the chest appears when the patient inhales, which is the opposite of that which occurs in breathing. The mechanism of negative pressure inhibits the growth of the mandible as follows (Fig. 11.17).
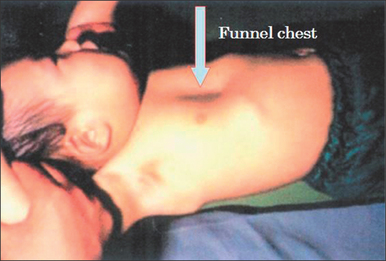
If we stand by this hypothesis and the functional matrix hypothesis, it is easier to interpret why OSA patients tend to have the dolichofacial pattern (long face) and lower positioned hyoid bone, longer soft palate and narrow airway. These may be the result of negative pressure in the chest. This negative pressure may cause funnel chest (Fig. 11.18). Castiglione25 reported that 82% of 23 children affected by chronic upper airway obstruction showed pectus excavatum and 82% showed enlarged tonsils and adenoids. If this negative pressure disappears as a result of the removal of the tonsils or adenoids, or by orthodontic treatment to improve patency of the airway, the mandible may grow normally, and we could prevent or reduce sleep apnea in the future.
1. Robin P. Glossoptsis due to atresia and hypotrophy of the mandible. Am J Dis Child. 1934;48:541-547.
2. Boraz R, Martin H, Michel J. Sleep apnea syndrome: report of case. J Dent Child. 1979;46:50-52.
3. Cartwright R, Samelson C. The effects of a nonsurgical treatment for obstructive sleep apnea – the tongue retaining device. JAMA. 1982;248:705-709.
4. Meir-Ewert K, Schafer H, Kloe W. Treatment of sleep apnea by a mandibular protracting device. Berichtsband 7th European Congress on Sleep Research. Munich, Germany: 1984;217.
5. Lowe A. Oral appliance for sleep breathing disorders. In: Kryger M, Roth T, Dement W, editors. Principles and Practice of Sleep Medicine. 3rd edn. Philadelphia: WB Saunders; 2000:929-939.
6. Kushida C, Morgenthaler T, Littner M. Oral appliance for snoring and obstructive sleep apnea: a review. Sleep. 2006;29(2):244-262.
7. Kushida C, Morgenthaler T, Littner M. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: an update for 2005. Sleep. 2006;29(2):240-243.
8. George PT. A new instrument for functional appliance bite registration. J Clin Orthodont. 1992;26:721-723.
9. Esaki K, Kanegae H, Uchida T, et al. Treatment of sleep apnea with a new separated type of dental appliance (mandibular advancing positioner). Kurume Med J. 1997;44:315-319.
10. Tsuiki S, Hiyama S, Ono T, et al. Effects of a titratable oral appliance on supine airway size in awake non-apneic individuals. Sleep. 2001;24(5):554-560.
11. Bacon WH, Turlot JC, Krieger J, et al. Cephalometric evaluation of pharyngeal obstructive factors in patients with sleep apneas syndrome. Angle Orthod. 1990;60(2):115-122.
12. Andersson L, Brattstrom V. Cephalometric analysis of permanently snoring patients with and without obstructive sleep apnea syndrome. Int J Oral Maxillofac Surg. 1991;20(3):159-162.
13. Jamieson A, Guilleminault C, Partinen M, et al. Obstructive sleep apneic patients have craniomandibular abnormalities. Sleep. 1986;9(4):469-477.
14. Lowe AA, Santamaria JD, Fleetham JA, et al. Facial morphology and obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1986;90(6):484-491.
15. Kikuchi M, Higurashi N, Miyazaki S, et al. Facial patterns of obstructive sleep apnea patients using Ricketts’ method. Psychiatr Clin Neurosci. 2000;54(3):336-337.
16. Tangugsorn V, Skatvedt O, Krogstad O, et al. Obstructive sleep apnoea: a cephalometric study. Part I. Cervico-craniofacial skeletal morphology. Eur J Orthod. 1995;17(1):45-56.
17. Lyberg T, Krogstad O, Djupesland G. Cephalometric analysis in patients with obstructive sleep apnoea syndrome. I. Skeletal morphology. J Laryngol Otol. 1989;103(3):287-292.
18. Kikuchi M, Higurashi N, Miyazaki S, et al. Facial pattern categories of sleep breathing disordered children using Ricketts analysis. Psychiatr Clin Neurosci. 2002;56(3):329-330.
19. Frankel R, Frankel C. Orofacial Orthopedics with the Function Regulator. Basel: Karger; 1989. pp. 19–21
20. Moss ML. Differential roles of the periosteal and capsular matrices in orofacial growth. Trans Eur Orthod Soc. 1969;45:193-206.
21. Moss ML, Rankow R. The role of the functional matrix in mandibular growth. Angle Orthod. 1968;38:95-103.
22. Moss ML, Salentijn L. The capsular matrix. Am J Orthod. 1969;55:566-577.
23. Bosma JF. Form and function in the mouth and pharynx of the human infant. In: McNamara JAJr., editor. Control Mechanism in Craniofacial Growth. Monograph 3: Craniofacial Growth Series, Center for Human Growth and Development. Ann Arbor, MI: University of Michigan, 1975.
24. Kikuchi M. Orthodontic treatment in children to prevent sleep-disordered breathing in adulthood. Sleep Breath. 2005;9:146-158.
25. Castiglione N, Eterno C, Sciuto C, et al. The diagnostic approach to and clinical study of 23 children with an obstructive sleep apnea syndrome. Pediatr Med Chir. 1992;14(5):501-506.